Combining Molecular and Neuroimaging Measures to Understand Psychopathology and Inform New Treatment Development
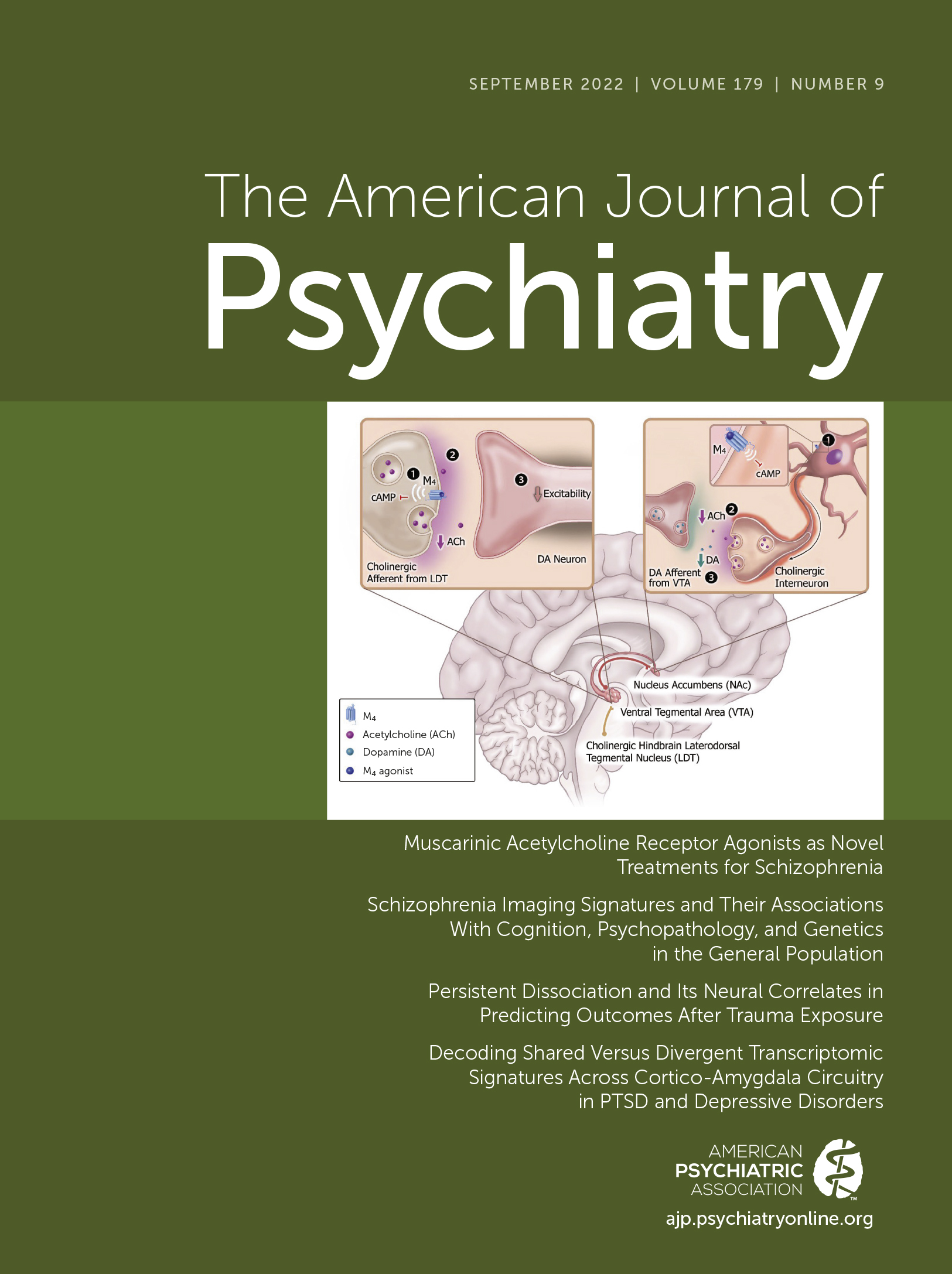
This issue of the Journal brings together very interesting papers that provide new insights into understanding and informing treatment approaches for schizophrenia, posttraumatic stress disorder (PTSD), depression, and anxiety disorders. Regarding new treatments for schizophrenia, Paul and colleagues (1) contribute a review paper focused on muscarinic acetylcholine agonists that provides evidence to support their potential utility in reducing both the positive and negative symptoms of schizophrenia. This review provides the basics relevant to muscarinic receptor pharmacology, and also presents encouraging preclinical and clinical data suggesting that the M1 and M4 receptor subtypes are viable drug targets. Elsewhere in this issue, a study addresses the extent to which psychotic experiences in children of schizophrenia spectrum disorder and bipolar parents confer risk to develop psychopathology. An additional study focused on schizophrenia that used machine learning with neuroimaging data to confirm a previous finding that identified patterns of structural brain alterations that are useful in subtyping schizophrenia. The researchers also determine the prevalence of these neural phenotypes in at-risk youth and in a large nonaffected sample of adults.
The remaining papers in this issue of the Journal focus on anxiety disorders, depression, and PTSD. In one of these papers, an adoption study design is employed to characterize how rearing and genetic influences contribute to the intergenerational transmission of anxiety and depression. Two papers in this issue are focused on PTSD. One explores the prognostic value of persistent dissociative symptoms and their associated functional brain alterations that occur after an acute traumatic event. The other, aimed at understanding the molecular underpinnings of PTSD, uses postmortem brain tissue to characterize patterns of gene expression in cortical-amygdala circuits that are shared with, and specific to, PTSD and depression.
The Predictive Value of Psychotic Experiences in Children From Parents With Schizophrenia and Bipolar Disorder
Psychotic experiences are relatively common during childhood and are associated with an increased risk to develop psychopathology. To better understand psychotic experiences in children as they relate to schizophrenia and bipolar disorder, Gregersen and colleagues (2) longitudinally assessed psychotic experiences and axis I disorders in children at 7 and 11 years of age who were at a familial high risk to develop schizophrenia (N=170) or bipolar disorder (N=103) as well as a population-based control group (N=174). The study sample was drawn from the Danish High Risk and Resilience Study, with high familial risk defined as having at least one parent with either a schizophrenia spectrum disorder or bipolar disorder. Children at high risk for schizophrenia, and not bipolar disorder, were significantly more likely to report psychotic experiences compared with children in the control group (31.8% vs. 18.4%, respectively). Regardless of parental status, 30.7% of the children that reported psychotic experiences at the 7 years of age assessment also reported persistent psychotic experiences that occurred between 7 years and 11 years of age. Of children who reported psychotic experience during early childhood, 46.6% met criteria for various types of axis I disorders (internalizing, externalizing, and other) during middle childhood as compared to an axis I prevalence of 28.3% in children without psychotic experiences during early childhood. Persistent psychotic experiences were more common in the schizophrenia high-risk children (36.1%) than in bipolar risk children (26.7%) or the control group (26.2%). Irrespective of risk category, children with persistent psychotic experiences had the greatest likelihood of developing psychopathology during middle childhood (odds ratio: 4.1), and the type of psychopathology that the children developed did not differ in relation to their risk group status. Along with colleagues from RCSI University of Medicine and Health Sciences and Queen’s University in Belfast, Dr. Mary Cannon provides an editorial (3) commenting on the findings from this study and another study in this issue in which risk for psychosis is assessed using measures derived from structural brain imaging and polygenic risk scores. The editorialists conclude with a suggestion that additional factors should be included in the determination of childhood risk with the hope of identifying a greater number of individuals that would seek out and benefit from early interventions.
Brain Structural Alterations and Genetic Risk for Developing Schizophrenia Assessed in At-Risk Youth and a Normative Sample
To understand the utility of neuroimaging data and polygenic risk scores in predicting the risk to develop schizophrenia, Chand and colleagues (4) first performed studies in a sample of individuals with schizophrenia (N=149) and control subjects (N=198), and then explored the extent to which the identified schizophrenia-associated brain alterations were present in population-based samples. The population-based samples included a community sample, the Philadelphia Neurodevelopmental Cohort, which was constituted of youth with psychosis spectrum symptoms (N=181; 47 individuals had “full psychotic symptoms”) and control subjects (N=178), and adult participants from the UK Biobank, none of whom had schizophrenia (N=836). First, in the schizophrenia sample, machine learning techniques were used to replicate a result that previously identified two neural signatures associated with schizophrenia. In this sample, 58% of individuals had a pattern of structural alterations characterized by reductions in white matter and gray matter volume across the brain (signature 1: predominant volumetric reductions in thalamus, nucleus accumbens, and medial temporal, prefrontal, frontal, and insular cortices), and 42% of individuals were characterized by increased striatal and internal capsule volumes (signature 2). Next, the researchers determined that approximately 40% of youth with psychosis spectrum symptoms had a signature 1 pattern of structural alterations, which was significantly greater than that observed in 23% of the control subjects. The groups did not significantly differ in relation to the prevalence of signature 2, or in having both signatures, or none of the signatures. When assessed across both psychosis spectrum youth and control subjects, individuals with the signature 1 pattern were found to have reductions in cognitive performance efficiency, whereas signature 2 was associated with increased cognitive performance efficiency. In the normative UK Biobank sample, the signature 1 pattern was present in 24.3% of participants, whereas 20.3% had signature 2, 9.6% had both signatures, and 45.8% had neither of the signatures. Similar to the youth cohort, the presence of the signature 1 pattern was associated with decreased cognitive performance. Polygenic risk scores for schizophrenia were available from the UK Biobank sample and did not significantly differ between signature 1 and signature 2 individuals. However, the polygenic risk scores were significantly higher when individuals with the signature 1 pattern were compared with individuals who did not have either signature 1 or signature 2. In summary, the researchers found that the signature 1 pattern is enriched in youth with psychotic symptoms who are at risk to develop schizophrenia, and that both signature 1 and signature 2 are not exclusive to at-risk individuals or those with schizophrenia. Additionally, the genetic risk to develop schizophrenia is associated with the neural phenotype characterized by broad white matter and gray matter volumetric reductions. These findings further the understanding of the neural phenotypes that are relevant to schizophrenia, the risk to develop this illness, and the prevalence of these patterns of brain alterations in the general population.
Genetic and Rearing Influences on the Parent-Child Transmission of Anxiety Disorders
Anxiety disorders are among the most common psychiatric disorders, with lifetime prevalence rates in the United States estimated to be 31.1% (5). Kendler and colleagues (6) use an adoptive design with a very large database from a Swedish national sample to characterize the extent to which genes and rearing contribute to the intergenerational risk to develop anxiety disorders and comorbid depression. Using data from over 2 million offspring, the authors categorized individuals into six different family configurations in which the children were raised (i.e., intact family, not living with mother or father, living with stepfather or stepmother, or fully adoptive). These different parental configurations provided the researchers with the opportunity to estimate the relative influences of genes and rearing on the intergenerational transmission of anxiety disorders. Consistent with the increased incidence of anxiety disorders in women that occurs during their reproductive years, the researchers found a higher prevalence of anxiety disorders in mothers and daughters compared with fathers and their sons. The highest incidence of anxiety disorders in parents and offspring was observed in the families without mothers as well as in those with step-parents, whereas the lowest incidence of anxiety disorders occurred in the intact families. Overall findings for anxiety disorders demonstrate a correlation of 0.16 between parents and children, with 70% of this effect estimated to be due to genetics and 30% rearing. Also, similar effects were determined for the relation between parent anxiety disorders and children’s depression, as well as for parent depression and children’s anxiety disorders. Additional analyses revealed shared genetic and rearing factors underlying the risk to develop anxiety and depression. When more specifically assessing panic disorder and generalized anxiety disorder, the results demonstrated a higher genetic correlation between generalized anxiety disorder and depression as compared to that for panic disorder and depression. In her editorial, Dr. Francis Rice from Cardiff University (7) discusses the value of adoption designs in affording the capacity to disentangle genetic from rearing effects and emphasizes the strengths of this paper, one of which is the use of data from fathers that enables analyses of paternal-offspring relations.
Persistent Trauma-Related Derealization and Associated Ventromedial Prefrontal Cortex Function 2 Weeks after Trauma Predicts Longer-Term Symptoms
Unfortunately, trauma is ubiquitous in our society and in numerous individuals results in marked dysfunction, which when severe manifests as PTSD and its associated comorbidities such as depression, anxiety, and substance abuse. In an attempt to better predict long-term outcomes in traumatized individuals, Lebois et al. (8) use a large sample to assess how dissociative symptoms resulting from a traumatic experience, and their neural correlates, relate to long-term psychological outcomes. Based on earlier work, the researchers specifically focused on derealization, a sense of detachment from one’s world or environment, and ventromedial prefrontal cortical (vmPFC) activity. The hypothesis that was explored was that persistent derealization symptoms and increased vmPFC activity would predict worse trauma-related outcomes. Importantly, the researchers examined the extent to which these psychological symptoms and neural alterations predicted outcomes when controlling for other related factors such as prior history of trauma and other current posttraumatic symptoms. This multisite effort, as part of the AURORA study, involved recruiting participants from 22 emergency rooms using self-report data from 1,464 participants and fMRI data from a subset of 145 individuals. Approximately 2 weeks after the traumatic event, participants rated their dissociative symptoms and also were scanned to assess task-based and resting-state neural activity. Three months posttrauma, assessments of dissociative symptoms as well as other psychiatric symptoms and measures of functional capacity were obtained. Persistent derealization occurring during the first 2 weeks after their traumatic experience was reported in 55% of participants. As hypothesized, increased levels of derealization were significantly associated with increased vmPFC activity when viewing fearful faces and also with measures of resting-state functional connectivity (i.e., connectivity between the vmPFC and a region of the cerebellum, as well as between vmPFC and a region within the right orbitofrontal cortex). Importantly, individual differences in levels of derealization occurring during the 2-week posttrauma period, even when controlling for factors such as childhood maltreatment and PTSD symptoms at 2 weeks, predicted the development of PTSD and depression at 3 months posttrauma. Emotion-related vmPFC activity assessed 2 weeks posttrauma also predicted PTSD and depression at 3 months but not as strongly as the derealization symptoms. In her editorial (9), Dr. Lisa Shin from Tufts University discusses these findings in relation to their potential clinical utility, underscoring the value of the imaging data in pointing to neural circuits that could serve as treatment targets.
Shared and Distinct Patterns of Prefrontal and Amygdala Gene Expression in PTSD and Depression
PTSD and depression are highly comorbid, and Jaffe and colleagues (10) use RNA sequencing data from postmortem brains to understand alterations in gene expression that are associated with these illnesses and also shared by them. Measuring RNA is of value because RNA levels reflect an interaction between heritable genetic structural variation and environmentally mediated epigenetic effects, and, via translation and mRNA, direct protein formation. The postmortem brains that were used in this study included those from control subjects (N=109), major depression without comorbid PTSD (N=109), and PTSD with some individuals with comorbid depression, bipolar disorder, or substance use disorder (N=107; 62.6% with comorbid major depression; 27% with comorbid bipolar disorder; 77.6% with comorbid substance use disorder). Because of data linking alterations in prefrontal/frontal-amygdala circuitry to depression and other stress-related psychopathology, RNA sequencing was performed from tissue dissected from two cortical regions (dorsolateral PFC and midcingulate cortex) and two amygdala regions (basolateral region and medial amygdala nucleus). When combining the cortical regions, the investigators found 41 genes that were differentially expressed when PTSD and control subjects were compared. Among the differentially expressed genes, CORT expression was decreased. This is of interest because CORT encodes for precorticostatin, a protein that is processed to corticostatin-17, which is found in inhibitory GABA cortical neurons. Furthermore, the structure of corticostatin is very similar to that of somatostatin, and also binds to somatostatin receptors. When combining the RNA data from the amygdala regions and using multiple comparison corrections, only one differentially expressed gene was detected (i.e., reduced expression of CRHBP). This is of interest since CRHBP encodes for the corticotropin-releasing hormone binding protein, which functions to modulate the synaptic availability of the anxiogenic neuropeptide, corticotropin-releasing hormone. Additional differential analyses were performed for the two cortical and two amygdala subregions, and findings revealed that the most prominent cortical effects were detectable in the midcingulate cortex. When controlling for other potentially important variables, such as the use of antidepressants and the presence of opioids in the blood, the overall findings were generally conserved, suggesting that the detected effects are specific to PTSD and not due to comorbid depression or substance abuse. Other analyses revealed that the differentially expressed genes were found to be in pathways related to immune function, microglia, and GABA-inhibitory neurons. In relation to major depression, when combining the RNA data from the two cortical and two amygdala regions, the researchers found 182 genes in the cortex and none in the amygdala that were differentially expressed when compared with control subjects. Further analyses of the amygdala data revealed 16 genes that were differentially expressed in the medial amygdala nucleus and none in the basolateral region. Overall, when using liberal significance criteria, there was a considerable amount of overlap in the genes that were differentially expressed between PTSD and major depression. Consistent with this, only a few genes were found to be differentially expressed when comparing PTSD to major depression. Taken together, this study suggests shared and distinct alterations in gene expression patterns in PTSD and major depression, highlighting pathways involving immune-related alterations, GABA-inhibitory neurons, and the corticotropin-releasing hormone binding protein. In their editorial, Drs. Sarah Rudzinskas and David Goldman from NIMH (11) discuss the importance of the findings and also discuss issues relevant to interpreting transcriptomic studies from postmortem brain tissue.
Conclusion
This issue of the Journal emphasizes the value of combining phenotypic measures at different levels of analysis (i.e., behavioral, neural-circuit, molecular, and genetic) to better understand mechanisms underlying psychopathology. New findings derived from these approaches that are reported in this issue include: 1) the possibility of using M1 and M4 agonists as new treatments for the positive and negative symptoms of schizophrenia; 2) that children with persistent psychotic experiences are at a fourfold risk for developing psychopathology during middle childhood; 3) the genetic risk to develop schizophrenia is associated with a neural phenotype characterized by broad white matter and gray matter volumetric reductions; 4) the intergenerational transmission of anxiety disorders appears to be 70% due to genetics and 30% to rearing, and these components for anxiety disorders are also highly correlated with those for the transmission of depression; 5) persistent derealization symptoms and associated vmPFC functional alterations predict negative outcomes after acute trauma; and 6) cortical and amygdala gene expression patterns in PTSD and major depression highlight shared alterations in molecular pathways (e.g., immune-related) and distinct PTSD-associated alterations in GABA-inhibitory neurons. By further elucidating factors and mechanisms underlying schizophrenia, PTSD, major depression and anxiety disorders, the papers in this issue of the Journal bring us closer to developing sound scientific rationales for the development of early intervention strategies that target altered neural circuits and their underlying molecular substrates.
1. : Muscarinic acetylcholine receptor agonists as novel treatments for schizophrenia. Am J Psychiatry 2022; 179:611–627Link, Google Scholar
2. : Developmental pathways and clinical outcomes of early childhood psychotic experiences in preadolescent children at familial high risk of schizophrenia or bipolar disorder: a prospective, longitudinal cohort study - the Danish High Risk and Resilience Study, VIA 11. Am J Psychiatry 2022; 179:628–639Abstract, Google Scholar
3. : Broadening the parameters of clinical high risk for psychosis. Am J Psychiatry 2022; 179:593–595Abstract, Google Scholar
4. : Schizophrenia imaging signatures and their associations with cognition, psychopathology, and genetics in the general population. Am J Psychiatry 2022; 179:650–660Abstract, Google Scholar
5. : National Comorbidity Survey, data table 1: Lifetime prevalence DSM-IV/WMH-CIDI disorders by sex and cohort. https://www.hcp.med.harvard.edu/ncs/ftpdir/table_ncsr_LTprevgenderxage.pdf Google Scholar
6. : An extended Swedish adoption study of anxiety disorder and its cross-generational familial relationship with major depression. Am J Psychiatry 2022; 179:640–649Abstract, Google Scholar
7. : The intergenerational transmission of anxiety disorders and major depression. Am J Psychiatry 2022; 179:596–598Link, Google Scholar
8. : Persistent dissociation and its neural correlates in predicting outcomes after trauma exposure. Am J Psychiatry 2022; 179:661–672Link, Google Scholar
9. : Looking through a fog: what persistent derealization can teach us about PTSD. Am J Psychiatry 2022; 179:599–600Abstract, Google Scholar
10. : Decoding shared versus divergent transcriptomic signatures across cortico-amygdala circuitry in PTSD and depressive disorders. Am J Psychiatry 2022; 179:673–686Link, Google Scholar
11. : Transcriptomic decoding of shared and unshared molecular etiologies in psychiatric disorders. Am J Psychiatry 2022; 179:601–603Abstract, Google Scholar