Muscarinic Acetylcholine Receptor Agonists as Novel Treatments for Schizophrenia
Abstract
Schizophrenia remains a challenging disease to treat effectively with current antipsychotic medications due to their limited efficacy across the entire spectrum of core symptoms as well as their often burdensome side-effect profiles and poor tolerability. An unmet need remains for novel, mechanistically unique, and better tolerated therapeutic agents for treating schizophrenia, especially those that treat not only positive symptoms but also the negative and cognitive symptoms of the disease. Almost 25 years ago, the muscarinic acetylcholine receptor (mAChR) agonist xanomeline was reported to reduce psychotic symptoms and improve cognition in patients with Alzheimer’s disease. The antipsychotic and procognitive properties of xanomeline were subsequently confirmed in a small study of acutely psychotic patients with chronic schizophrenia. These unexpected clinical findings have prompted considerable efforts across academia and industry to target mAChRs as a new approach to potentially treat schizophrenia and other psychotic disorders. The authors discuss recent advances in mAChR biology and pharmacology and the current understanding of the relative roles of the various mAChR subtypes, their downstream cellular effectors, and key neural circuits mediating the reduction in the core symptoms of schizophrenia in patients treated with xanomeline. They also provide an update on the status of novel mAChR agonists currently in development for potential treatment of schizophrenia and other neuropsychiatric disorders.
Schizophrenia is a common and complex psychiatric syndrome consisting of three primary symptom domains: positive symptoms (e.g., hallucinations, delusions, disordered thinking and speech), negative symptoms (e.g., lack of motivation, lack of emotional expression or flat affect, social withdrawal), and cognitive symptoms (e.g., impaired attention, concentration, memory, and executive functions) (1). Demographically, schizophrenia affects approximately 0.5%–1.0% of the population worldwide (2) and usually manifests by one’s late teens or early adulthood. Although the natural progression of schizophrenia is highly variable, many patients remain disabled their entire lives (3). In fact, schizophrenia remains one of the top 10 causes of disability worldwide (3).
The very first commonly used antipsychotic drug, chlorpromazine, was discovered serendipitously by Laborit, Delay, and Deniker and was introduced in the United States in the 1950s (4). Many chemically unique first- and second-generation antipsychotic drugs have subsequently been developed; however, with the possible exception of clozapine, they all have relatively similar efficacy across the symptom domains of schizophrenia while differing in their side-effect profiles (5). This is not surprising, since all currently approved antipsychotics are either antagonists or partial agonists/antagonists of dopamine (DA) D2 receptors (6). Whereas other neurotransmitter systems may contribute to their overall efficacy and/or side effects, DA D2 receptors are believed to predominantly mediate their beneficial therapeutic effects by reducing positive symptoms of schizophrenia (7, 8).
Despite the effects of current antipsychotic medications on positive symptoms, many patients with schizophrenia continue to experience residual positive symptoms, and a significant percentage of patients remain treatment resistant (9). Moreover, there is currently no approved medication for the treatment of negative or cognitive symptoms (10) (the “dementia” of dementia praecox). Antipsychotic drugs are also associated with undesirable adverse events, including extrapyramidal side effects, akathisia, weight gain, metabolic disturbances, excessive sedation, hyperprolactinemia, and a risk of developing tardive dyskinesia (5, 11). More efficacious treatments based on new or unique mechanistic targets are desperately needed, especially if they are shown to be effective across all three symptom domains and/or possess better safety and tolerability profiles (12). Here, we review a considerable body of historical and recent preclinical and clinical evidence suggesting that muscarinic acetylcholine receptors, a small family of G protein–coupled receptors (GPCRs), may represent novel targets for treating the core symptom domains of schizophrenia.
For more than six decades, muscarinic acetylcholine receptors (mAChRs) have been implicated in the pathophysiology of schizophrenia, based on the observation that brain-penetrant mAChR antagonists can either induce or exacerbate cognitive impairment (13, 14) as well as psychosis (15, 16). Almost 65 years ago, Pfeiffer and Jenney (17) reported that the natural mAChR agonist arecoline (Figure 1A) exhibited antipsychotic “activity” in a preclinical model of psychosis (i.e., conditioned avoidance responding) and produced what were described as “lucid intervals” in patients with schizophrenia. Although these lucid intervals were of relatively short duration, and despite the obvious limitations of this small, open-label, unblinded study, this was the first evidence that an mAChR agonist might reduce some of the symptoms of schizophrenia. Arecoline is also the most abundant psychoactive alkaloid in the betel nut, which is commonly chewed as a cultural practice in the south of Asia and Asia Pacific (18). Several small follow-on studies have again reported that betel nut chewing is associated with less severe positive and negative symptoms of schizophrenia (19, 20).
FIGURE 1. The chemical structure of the natural pan-muscarinic acetylcholine receptor (mAChR) agonist alkaloid arecoline and the synthetic M1/M4-preferring mAChR agonist xanomeline
In the 1980s, the development of mAChR agonists as potential procognitive drugs became of interest to the pharmaceutical industry. Xanomeline, a potent synthetic mAChR agonist derivative of arecoline (21) (Figure 1B), was evaluated for its ability to improve cognition in a large placebo-controlled phase 2 study in patients with Alzheimer’s disease. Bodick and colleagues (22) reported that xanomeline improved cognition in patients with Alzheimer’s disease, but also reported the surprising and unexpected finding that xanomeline rapidly and dose-dependently reduced psychotic symptoms in patients manifesting these symptoms at baseline and prevented or delayed their onset compared with placebo during the 6-month trial. The antipsychotic properties of xanomeline in dementia-related psychosis were completely unanticipated and in many patients were quite dramatic.
Subsequently, Shekhar and colleagues (23) reported that xanomeline treatment led to rapid and robust antipsychotic and procognitive effects in a small double-blind placebo-controlled trial in inpatients with treatment-resistant schizophrenia. Treatment with xanomeline in both trials (22, 23), although not associated with the common side effects of first- and second-generation antipsychotics (e.g., weight gain, extrapyramidal side effects, and sedation), resulted in substantial peripheral “cholinergic” adverse events (e.g., nausea and vomiting) that precluded xanomeline’s further development. Nonetheless, these clinical studies (22, 23) and related preclinical work (24, 25) with xanomeline strongly suggested that mAChR agonists can reduce psychotic symptoms without directly antagonizing DA D2 receptors (26).
Over the ensuing two decades, much has been learned about the molecular, cellular, and neural circuit-based mechanisms of mAChR agonist–based antipsychotics. These findings and their application may lead to the discovery of potentially more effective treatments for managing the positive, negative, and cognitive symptoms of schizophrenia.
Muscarinic Receptor Pharmacology
The discovery of mAChRs emerged from early Nobel Prize–winning discoveries on the regulation of frog heart contractility by Loewi and Dale and their seminal finding of the first neurotransmitter, acetylcholine (ACh), in 1921 (27). Cholinergic neurons are now known to form an intricate brain-wide network to modulate microcircuits through actions at both nicotine-sensitive (ionotropic) ion channels and muscarine-sensitive (metabotropic) mAChRs (28). The mAChR family is composed of five distinct subtypes (M1–M5) belonging to the superfamily of GPCRs, which, as transmembrane proteins, transmit external neurotransmitter signals via intracellular transducer proteins and second messengers (29). Although G protein–mediated signaling of GPCRs was the first signaling process associated with this superfamily of proteins, it is now well known that their signal transduction activities include complex combinations of G protein–dependent and –independent signaling pathways (see references 30, 31 for reviews). Historically, the mAChRs are subdivided into two distinct functional classes based on their propensity to couple to one of two primary G protein–dependent second messenger and signal transduction pathways (Figure 2A) (29, 32). The first class consists of the M1, M3, and M5 receptor subtypes, which couple primarily through the Gq subtype of G protein to stimulate phospholipase C and the subsequent release of the intracellular second messenger, inositol 1,4,5-trisphosphate (IP3), leading to increased intracellular calcium (Ca2+) levels and facilitation of excitatory postsynaptic currents. The second class is composed of M2 and M4 receptors, which couple primarily through the Gi/o subtype of G proteins that inhibit adenylate cyclase, leading to a reduction in the second messenger cAMP to generally suppress excitation.
FIGURE 2. Signaling selectivity among muscarinic acetylcholine receptors (mAChRs)a
aAs shown in panel A, the muscarinic receptor family consists of five members (M1–M5), which mediate the physiological effects of the neurotransmitter acetylcholine (ACh). The M1, M3, and M5 receptors are stimulatory and couple primarily to the generation of intracellular Gq alpha subunit to stimulate phospholipase C (via inositol 1,4,5-trisphosphate [IP3]), resulting in the mobilization of intracellular calcium (Ca2+). The M2 and M4 receptors are inhibitory and negatively modulate adenylyl cyclase (AC) via Gi/o alpha subunit to reduce cytoplasmic concentrations of cyclic adenosine monophosphate (cAMP). Panel B shows the crystal structure of the active state of the M2 receptor with allosteric and orthosteric binding pockets simultaneously occupied by the mAChR orthosteric agonist iperoxo and the M4/M2 positive allosteric modulator LY2119620. Created with BioRender.com.
All five mAChRs are broadly expressed throughout the body, supporting both peripheral autonomic functions and CNS control of arousal, attention, memory, and motivation (Figure 3A). The M1 and M4 receptors have their highest expression in the CNS, whereas the M2 and M3 receptors are more highly expressed in the periphery. The M5 receptor is relatively discretely expressed in DA-rich midbrain regions. The M1 receptor is expressed predominantly postsynaptically, with high levels of expression in the cerebral cortex and hippocampus, and is primarily associated with modulating excitatory synapses (33). The M2 receptor subtype primarily functions as a presynaptic neuromodulator, often acting as an autoreceptor on ACh-producing neurons (34) or as a heteroreceptor on neurons that release non-ACh neurotransmitters (e.g., glutamate, gamma-aminobutyric acid [GABA], and DA) to reduce their release (35). The M2 receptor is also highly expressed in the brainstem and thalamus and is expressed at low levels in cortical regions (33). The M3 receptor has a similar distribution pattern to the M1 receptor’s, but with a much lower level of expression in brain (33). The M4 receptor is particularly abundant as either pre- or postsynaptic auto- or heteroreceptors in the basal ganglia, limbic system, hippocampus, and cortex (36, 37). In contrast to its other family members, the M5 receptor has a more discrete localization in brain, primarily in midbrain DA neurons (38) (see references 39, 40 for mAChR distribution).
FIGURE 3. Quantification of muscarinic acetylcholine receptor (mAChR) mRNAs in central and peripheral human tissues using RNA sequencinga
aRelative expression of the five mAChR subtypes across key brain regions (panel A) and peripheral organs (panel B) associated with efficacy and tolerability of mAChR agonists. (Data used for the relative expression analysis described in this figure were obtained from the Genotype-Tissue Expression [GTEx] Portal on March 29, 2021. The GTEx Project was supported by the Common Fund of the Office of the Director of the National Institutes of Health and by the National Cancer Institute, the National Human Genome Research Institute, the National Heart, Lung, and Blood Institute, the National Institute on Drug Abuse, the National Institute of Mental Health, and the National Institute of Neurological Disorders and Stroke.)
Early CNS drug development efforts resulted in agonists with only modest mAChR subtype selectivity and were associated with poor tolerability due to peripheral side effects that precluded clinical development (41). Further complicating the discovery of mAChR subtype–selective agonists was the experimentally observed difference in selectivity based on receptor binding potencies versus functional activity (42). Upon cloning and sequencing of the mAChRs (43), along with recent observations of their three-dimensional crystal and cryo-electron-microscopic structures (44–46), it became clear that the mAChR family is one of the most highly conserved with respect to protein sequence and structure, making it exceedingly challenging to develop subtype-selective orthosteric ligands (31). Lack of mAChR subtype–selective ligands has also confounded attempts to fully attribute the desired in vitro and in vivo pharmacology to one or more mAChR subtypes (47). In mice, this challenge has in part been addressed by the use of global tissue-specific and cell-type-specific transgenic mice, in which each of the mAChR subtypes has been genetically deleted to better define their physiological and behavioral roles as well as to characterize the pharmacology of mAChR ligands (48–50).
The first highly selective mAChR agonists were developed relatively recently by targeting ligand-binding pockets or sites outside of the ACh (orthosteric) binding pocket itself (51). Receptor subtype–specific amino acid residues residing in these unique allosteric binding pockets have enabled the discovery of allosteric ligands with highly receptor-selective modulatory properties (51) (Figure 2B). These modulatory properties can either enhance or reduce receptor activation by the endogenous neurotransmitter ACh and maintain the temporal and spatial signaling of natural cholinergic neurotransmission in the brain (52, 53).
Modulators are classified as either positive allosteric modulators (PAMs) or negative allosteric modulators (NAMs) (51). However, these designations should be interpreted with caution as they are highly contextual, being dependent on the exact receptor being studied, the choice of orthosteric ligand, and the signaling assay employed (31). For example, the M1 receptor–selective modulator benzylquinolone carboxylic acid (BQCA) acts solely as a PAM when assayed in a cell line with low M1 receptor expression (54) but acts as both a full allosteric agonist and as a PAM in a system with high M1 receptor reserve (55). Moreover, recent research on mAChRs and other GPCRs has revealed several additional and unexpected complexities, including receptor-receptor interactions (56, 57), the formation of homomeric versus heteromeric receptor complexes (58, 59), ligand-dependent biased signaling (47), and species specificity (60).
Notwithstanding these drug development challenges, both mAChR PAMs and NAMs remain a focus of investigation due to their potential to achieve receptor subtype selectivity and to maintain spatial and temporal signaling that are better aligned with natural cholinergic neurotransmission in the brain (52, 53). The ability of allosteric modulators to maintain temporal signaling compared to orthosteric agents could have potential advantages if persistent, full receptor activation is undesirable (i.e., due to potential side effects or receptor desensitization) (61).
However, the advantages ascribed to PAMs could, in some cases, be disadvantageous. For example, a PAM’s reliance on cooperativity with the endogenous neurotransmitter, in this case ACh, could render such treatments less effective, especially in diseases where ACh levels decrease due to the progressive degeneration of cholinergic neurons, such as in Alzheimer’s disease and Parkinson’s disease (62, 63). Allosteric modulators are designed to regulate the affinity and efficacy of the natural ligand based on prevailing cholinergic tone, which may turn out to be therapeutic in one context but insufficient or even detrimental in another pathophysiologic state (64). The potential advantages or disadvantages of the selectivity afforded by allosteric mAChR agonists, however, will likely need to be determined in clinical studies to compare their relative efficacy and safety with direct-acting orthosteric agonists (see below).
Development of Muscarinic Receptor Agonists to Treat Schizophrenia
The initial development of mAChR-based therapies for CNS disorders focused primarily on treating Alzheimer’s disease–associated cognitive impairment, which results, at least in part, from loss of cholinergic innervation from forebrain regions such as the nucleus basalis and longitudinal band projecting to the hippocampus, afferents important for cognition and memory (65, 66). This prompted drug developers to create direct-acting ACh-mimetic agonist drugs based on the structure of arecoline, a well-characterized ACh-mimetic agonist for mAChRs (41, 67, 68). The result was the development of a number of mAChR agonists, several of which were taken into clinical trials, such as RS-86, milameline, cevimeline, tazomeline, talsaclidine, alvameline, sabcomeline, and xanomeline, with the intent of stimulating postsynaptic M1 receptors and thus circumventing the loss of ACh in Alzheimer’s disease (41, 69). Although these agents were developed as M1 receptor–targeted compounds, in practice they displayed only modest pharmacological selectivity across all five mAChRs (70).
Some of these M1 receptor–targeted compounds demonstrated detectable, although modest, improvements in cognition; however, parasympathetically mediated adverse events, including nausea and vomiting, increased gastrointestinal motility, salivation, and sweating, prevented their further clinical development (41, 71). For example, cevimeline initially yielded positive results on both the Alzheimer’s Disease Assessment Scale–Cognitive Subscale (ADAS-Cog) and caregiver impression scales (72). However, in a larger follow-up study, cevimeline subsequently failed to improve these same prespecified primary endpoints (73). Similarly, initial results from a clinical trial of sabcomeline in patients with Alzheimer’s disease indicated that it, too, improved ADAS-Cog scores (74), but it failed to meet its primary cognitive endpoint in a phase 3 trial (75). In a phase 2 study in patients with schizophrenia, sabcomeline was also reported to have no effect on Positive and Negative Syndrome Scale (PANSS) scores compared with placebo; however, trends in improved cognitive function were reported (76).
Overall, the often-cited reasons for discontinuation of these first-generation full or partial M1 receptor–targeted orthosteric agonists were the lack of efficacy and/or poor tolerability. The trials did not include any CNS assessment of activity, such as CNS muscarinic receptor occupancy, which is not surprising given the lack of reliable positron emission tomography ligands when these trials were conducted. Thus, it is difficult to conclude whether these trials failed owing to suboptimal dosing caused by dose-limiting peripheral mAChR adverse events or a lack of therapeutic activity for any given compound. At the time, the poor tolerability of these compounds was believed to be primarily due to their M2 and M3 receptor activity (48), but further work (see below) with mAChR subtype–selective ligands suggested that M1 and M4 receptors also likely played a role in the peripherally mediated adverse events observed with this first generation of mAChR-targeted drug candidates.
Although initially developed to specifically treat the cognitive symptoms of Alzheimer’s disease, the mAChR agonist xanomeline, as briefly discussed above, significantly reduced and prevented the emergence of behavioral, including psychotic, disturbances in patients with Alzheimer’s disease and resulted in modestly improved cognitive impairment as measured by the ADAS-Cog (22). These promising clinical data in patients with Alzheimer’s disease encouraged a considerable number of preclinical studies across academia and industry (discussed in detail below) to substantiate the neurobiological underpinnings of these surprising clinical results. Moreover, these findings also prompted a small (N=20), proof-of-concept, phase 2 follow-up trial in acutely psychotic patients with chronic schizophrenia (23). In that trial, when compared with placebo, treatment with xanomeline resulted in significant improvements in total Brief Psychiatric Rating Scale and PANSS scores as well as improvement in several cognitive domains, specifically in measures of verbal learning and short-term memory function. These rather compelling results obtained in patients with either Alzheimer’s disease (22) or schizophrenia (23) stimulated further research on the potential utility of mAChR agonists for treating a variety of neuropsychiatric disorders. Also evident from these early studies, however, was the need for improved tolerability, primarily with respect to limiting peripheral mAChR stimulation.
Following these early encouraging clinical data with xanomeline, the field set out to develop “mAChR-targeted” agents that would maintain the clinical benefits associated with xanomeline while reducing the associated mAChR-mediated adverse events. To accomplish this, two different approaches have been pursued. The predominant approach has been to develop compounds that more selectively target M1 and/or M4 receptors, the two mAChRs believed to be most associated with the benefits of xanomeline, via their allosteric (63) rather than orthosteric binding sites.
The other approach is a strategy recently adopted for reducing the peripheral side effects of xanomeline while maintaining its therapeutic benefits in the CNS: coadministration of xanomeline with a peripherally restricted mAChR antagonist (77). By blocking peripheral mAChRs with trospium (a U.S. Food and Drug Administration–approved, non–brain-penetrant, pan-mAChR antagonist) (78) while simultaneously activating central mAChRs with xanomeline, tolerability was markedly improved while maintaining xanomeline’s centrally mediated therapeutic benefits. The high brain-to-plasma ratio (>10:1) of xanomeline also likely favors CNS-mediated therapeutic activity observed across these clinical trials (79–81).
The results from a recently completed placebo-controlled phase 2 trial in patients with schizophrenia experiencing acute psychotic symptoms (82) demonstrated that treatment with the investigational drug combination of xanomeline and trospium (KarXT) resulted in a significant reduction in PANSS total score as well as a number of secondary endpoints (e.g., PANSS positive subscale, PANSS negative subscale, and Clinical Global Impressions severity scale) compared with placebo (Figure 4). Additionally, an exploratory post hoc analysis (83) suggests that KarXT treatment was also associated with greater improvement in cognitive performance compared with placebo in patients who were cognitively impaired at baseline. However, additional prospective studies will be needed to confirm the potential procognitive benefits of KarXT. KarXT was associated with mild to moderate cholinergic and anticholinergic adverse events that were generally transient and did not lead to discontinuation from the trial. Treatment with KarXT was not associated with extrapyramidal side effects, weight gain, or sedation (82). Although these phase 2 data are encouraging, phase 3 studies will be required to confirm the efficacy and safety profile observed in phase 2. Several phase 3 studies are currently under way (NCT04659161, NCT04738123, NCT04659174, NCT04820309, NCT05145413).
FIGURE 4. Treatment with the muscarinic acetylcholine receptor (mAChR) M1/M4-preferring agonist xanomeline in combination with the peripherally restricted mAChR antagonist trospiuma
aTreatment with xanomeline-trospium was superior to placebo on symptom improvement as assessed by the Positive and Negative Syndrome Scale (PANSS) at week 5 (panel A). Secondary efficacy endpoints, the PANSS positive symptom subscore (panel B) and negative symptom subscore (panel C), were also statistically significant compared with placebo at week 5. (From Brannan SK et al., Muscarinic cholinergic receptor agonist and peripheral antagonist for schizophrenia, New England Journal of Medicine, vol. 384, pp. 717–726. Copyright © 2021 Massachusetts Medical Society. Reprinted with permission.)
These results, which replicate the earlier phase 2 trials with xanomeline (22, 23), strongly suggest that mAChRs are compelling drug targets to potentially modulate neural circuits disrupted in patients with schizophrenia. Still to be explained, however, is whether one or more mAChR subtypes contribute to xanomeline’s antipsychotic and procognitive activity and how mAChR agonists may impact neural circuits likely responsible for their potential benefits in treating the core symptoms of schizophrenia.
Role of Specific Muscarinic Receptor Subtypes
Xanomeline has been reported to bind with relatively equal affinity to all five mAChRs, as determined by the displacement of the nonselective radiolabeled mAChR antagonist [3H]-N-methyl scopolamine (84, 85), and has been reported in some (86) but not all (26, 85) studies to bind to several serotonin (5-HT) receptors with low to high nanomolar affinity. Historically, radioligand binding assays with receptor-containing isolated whole-cell or synaptic membranes were used to rapidly screen compounds that target GPCRs, but these simple binding assays do not adequately establish whether a given compound of interest is an agonist or an antagonist or, importantly, whether it has functional activity as either a full or partial agonist or antagonist (42). Efforts have been made to develop signaling-dependent cell-based functional assays to provide more accurate and comprehensive data sets of compounds targeting GPCRs. Based on several cellular and in vivo functional assays, xanomeline appears to be selective for M1 and M4 receptors, and at pharmacologically relevant concentrations, it does not have significant functional activity at other GPCRs (85, 87, 88), including DA or 5-HT receptors.
Recent studies using X-ray crystal or cryo-electron-microscopy–solved structures of mAChRs at the <3.0-angstrom level, along with in silico molecular dynamic simulations, have allowed more detailed descriptions of both the static and kinetic interactions of mAChR ligands, such as xanomeline, at each of the mAChR subtypes (89). Based on these studies, xanomeline has been found to have unique and unexpected binding properties and pharmacology, including functional selectivity for M1 and M4 receptors (24, 90) and some level of persistent or “wash-resistant” binding that suggests pseudo-irreversible binding properties (91–93), which may contribute to its potentially unique functional pharmacology. Data generated from pharmacological models (94), paired with genetic deletion of mAChRs in mice (49), have provided considerable insight into which receptor subtypes are responsible for xanomeline’s behavioral pharmacology.
Xanomeline exhibits robust “antipsychotic drug–like” activity in animals treated with psychostimulant drugs that increase DA neurotransmission (e.g., amphetamine or apomorphine) (25, 26, 90, 95–97) or that block N-methyl-d-aspartate (NMDA) receptors (e.g., phencyclidine [PCP], dizocilpine [MK-801], or ketamine) (98, 99). The ability of xanomeline to decrease the functional effects of dopaminergic and glutamatergic psychostimulants is consistent with the putative antipsychotic actions of this compound, findings that have been replicated across numerous preclinical behavioral models of “psychosis” (24, 25, 90, 95, 97, 98, 100) and in recent pharmacological MRI studies (101, 102). Moreover, xanomeline’s antipsychotic activity is fully blocked by a centrally penetrant but not peripherally restricted pan-muscarinic-subtype antagonist, indicating that activation of one or more central mAChRs is sufficient to elicit antipsychotic-like activity (103) and likely to regulate neurotransmitter systems and neural circuits implicated in the pathophysiology of schizophrenia. Evidence for which mAChR subtypes are involved in the behavioral actions of xanomeline has only recently been made possible with the development of mice bearing genetic deletions of one or more mAChR subtypes as well as by using mAChR subtype–selective agonists.
Role of M4 Receptors
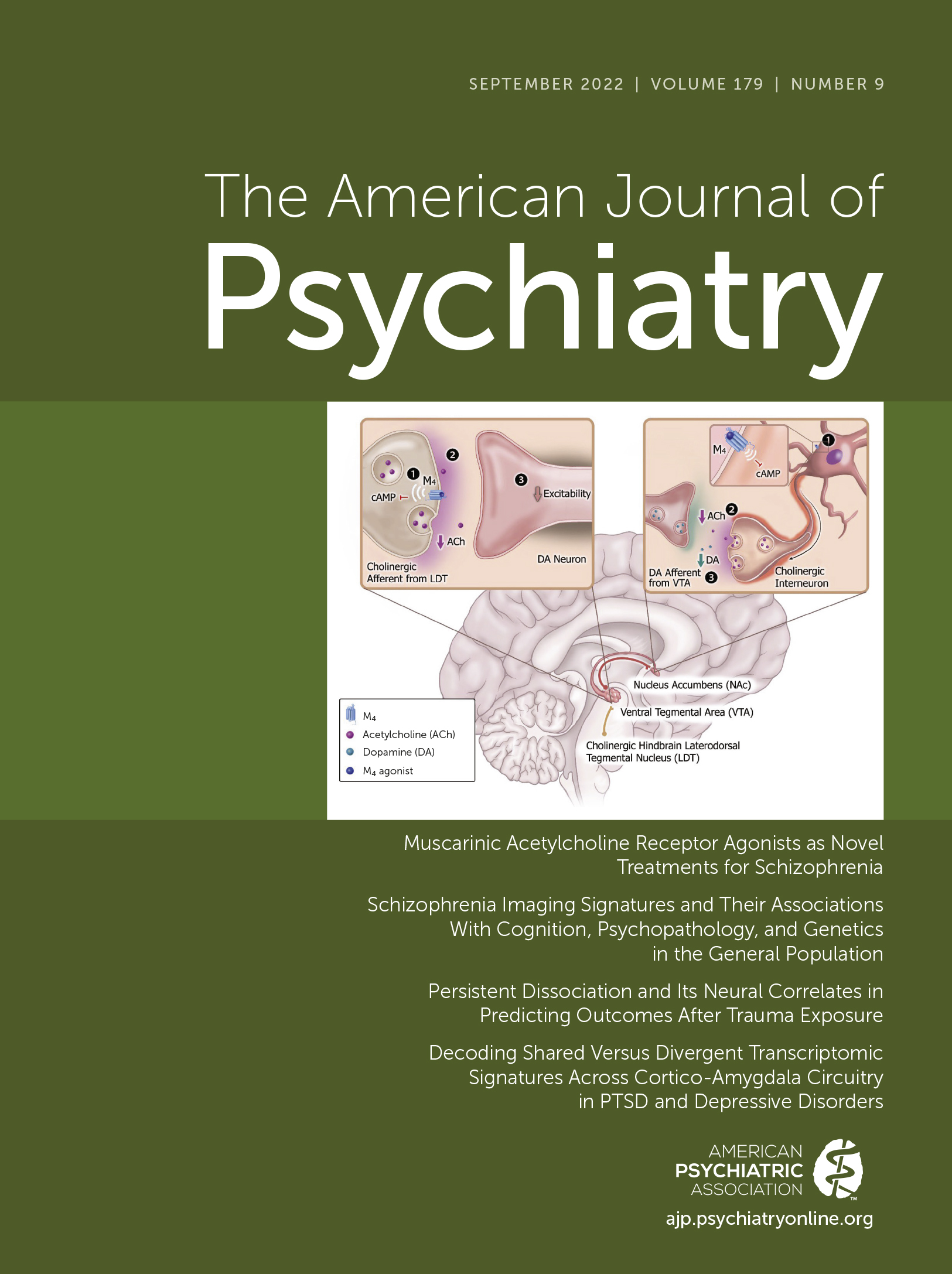
The onset of psychotic (i.e., positive) symptoms is believed to be associated with neural network dysfunction that includes a variety of brain regions and neurotransmitters, including increased activity of ventral tegmental area (VTA) DA neurons and heightened terminal DA release (104). Although the exact mechanism of how antipsychotic drugs achieve their therapeutic activity is still not completely understood, it has been postulated, with considerable experimental support, that most, if not all, antipsychotic drugs induce “depolarization block” or inactivation of DA neurons in both the VTA (“mesolimbic DA circuit”) and the substantia nigra (SN; “motor DA circuit”); this phenomenon takes place over a period of time that parallels the delay in the onset of clinical improvement (105). Based on the “depolarization block” hypothesis, antipsychotic drugs with more selective actions on VTA DA neurons consistently show a lower motor symptom liability (i.e., low extrapyramidal side effects), whereas high liability to extrapyramidal side effects is associated with antipsychotic drugs that more markedly reduce the activity of DA neurons in the SN, which is involved in the control of the extrapyramidal motor control system (106, 107). Importantly and often overlooked is that the activity of midbrain VTA DA neurons is modulated by cholinergic input from hindbrain structures (108), particularly the laterodorsal tegmental nucleus (LDT), where M4 receptors are abundantly expressed and function as autoreceptors (49, 109). M4 receptors play a key role in blunting the stimulatory effects of ACh on DA neurons, making them less active and thereby reducing downstream DA release in brain regions implicated in psychosis, such as the nucleus accumbens and ventral striatum (Figure 5A) (49, 109).
FIGURE 5. Activation of M4 receptors modulates cholinergic tone within midbrain dopamine (DA) centers to regulate terminal DA releasea
aThe M4 receptor is an autoreceptor on cholinergic afferents (point 1 in panel A) that project into the ventral tegmental area (VTA). Upon activation, M4 receptors reduce acetylcholine (ACh) release onto VTA DA neurons (point 2 in panel A) and subsequently decrease neuron firing activity due to reduced activation of ACh receptors located on DA cell bodies (point 3 in panel A). This leads to a downstream reduction of DA release within the nucleus accumbens (NAc). Locally, within the NAc, M4 receptors are located on cholinergic interneurons (ChIs) (point 1 in panel B). Upon activation, M4 receptors decrease ChI spontaneous activity, and thus decrease cholinergic release from these neurons (point 2 in panel B). Reduced local cholinergic tone will also decrease stimulation (i.e., activation) of DA terminals (point 3 in panel B).
Interestingly, xanomeline has been shown to selectively and rapidly reduce VTA DA neuron firing rates but not SN DA neuron activity (24), an effect now believed to be mediated by selective activation of LDT afferents (110, 111). This very rapid reduction in VTA DA neuron activity observed following acute administration of xanomeline (24) contrasts with the slow, time-dependent depolarization block of these same DA neurons that occurs following treatment with second-generation antipsychotics (105, 112, 113). The DA D2 receptor–independent modulation of DA microcircuits may also explain the relatively rapid antipsychotic effects of xanomeline reported in patients with Alzheimer’s disease (22) or schizophrenia (23). Also consistent with xanomeline’s selective action on mesolimbic VTA DA neurons is the lack of overt motor effects (e.g., catalepsy) observed in preclinical models (24, 90) or its lack of effect in inducing immediate early gene expression (e.g., cFos) in brain regions associated with extrapyramidal side effects (114). This highly selective regulation of DA-containing neural circuits seen with xanomeline may therefore account for the lack of observed extrapyramidal side effects in multiple clinical trials (22, 23, 82) and a much lower, if not absent, risk of developing tardive dyskinesia.
In addition to their ability to regulate midbrain VTA DA neuron activity, M4 receptors are expressed in cholinergic interneurons that reside locally in the nucleus accumbens and modulate terminal DA release (115, 116). Within the nucleus accumbens, activation of M4 autoreceptors on cholinergic interneurons decreases spontaneous activity, which reduces ACh release to dampen nicotinic receptor feed-forward stimulation on DA terminals (Figure 5B) (116, 117). It should be noted, however, that there are other postulated mechanisms by which M4 receptor–mediated inhibition of local DA release may occur, such as activation of M4 receptors coexpressed in D1 receptor–expressing medium spiny neurons (MSNs) of the dorsolateral striatum (118, 119). In support of this hypothesis, selective deletion of M4 receptors from D1 MSNs increases DA-dependent behavioral phenotypes (119) and blunts M4 receptor–mediated inhibition of DA release in preclinical models (120), an effect likely mediated through competition of convergent second messenger systems (56), recruitment of endocannabinoids (120), interactions with Gq-coupled receptors (121), or direct actions on enhanced Ca2+ currents via Cav1 channels (122). Genetically eliminating M4 receptors from D1 MSNs also markedly reduces the inhibitory effects of xanomeline on amphetamine-stimulated locomotor activity (118).
More recent studies using highly selective M4 receptor PAMs support the important role that these receptors play in mediating antipsychotic drug–like behavioral activity, as numerous chemical scaffolds that modulate M4 receptors display antipsychotic activity (60, 120, 123–125). In addition to modulating classical neural circuits implicated in psychosis, M4 receptor PAMs have been shown to enhance attentional and memory network function in preclinical rodent models (126). M4 receptor agonists can reduce elevated CA1 pyramidal neuron activity, which may partially contribute to their procognitive effects (85), as changes in CA1 excitability have been postulated to contribute to the cognitive deficits in schizophrenia (27). However, additional detailed studies are needed to fully understand the multinodal mechanisms by which M4 receptors impact local subcortical microcircuits within the dorsal (i.e., associative striatum) and ventral striatum to inhibit DA neurotransmission (for a review, see reference 9).
Although M4 receptor regulation of DA microcircuits appears to be important in the central mechanism of action of xanomeline, glutamatergic microcircuits may also contribute to its antipsychotic activity. In rodents, acute administration of NMDA receptor antagonists, such as PCP or MK-801, produces behavioral hyperactivity and cognitive deficits that correlate with a disinhibition of pyramidal cell firing in the prefrontal cortex and increased DA and glutamate levels (127, 128). Administration of xanomeline or a selective M4 receptor PAM can attenuate PCP- or MK-801-evoked locomotor activity, an effect that is absent in global M4 receptor knockout mice (123). M4 receptor–mediated regulation of MK-801-induced hyperactivity may involve actions at corticostriatal terminals to normalize the function of overactive excitatory glutamatergic projections to the striatum (129) or via a dampening of thalamocortical synapses (130). This “top-down” control of cortical glutamatergic projections has important implications, as these projections indirectly modulate phasic DA release (118). In addition, activation of M4 receptors attenuates MK-801-induced disruptions in learning and memory (123) and elevations of high-frequency gamma power as well as state-dependent alterations in sleep architecture and arousal similar to the effects observed with atypical antipsychotics in preclinical models (131). Taken together, these findings suggest an important role for M4 receptors in modulating neural circuits involved in the psychotic, motivational, cognitive, and executive functions disrupted in schizophrenia via glutamatergic microcircuits.
These behavioral studies describing an important role for M4 receptors in animal models of psychosis have led to further studies exploring the potential role of M4 receptors in the pathophysiology of schizophrenia. In postmortem studies, M4 receptor expression has been reported to be decreased in striatal and hippocampal brain regions of patients with schizophrenia compared with those of healthy control subjects (132). Other studies using modestly selective mAChR antagonist radioligands also suggest that M4 receptors are decreased in the frontal cortex, hippocampus, and striatum of patients with schizophrenia compared with those of control subjects (133, 134). In tandem with the apparent decreases in M4 receptor expression, these morphometric changes could also contribute to decreased regional brain volumes and cortical thickness. Genetic markers (single-nucleotide polymorphisms) in a region on chromosome 11 have been reported to be associated with schizophrenia (135), and this region contains several candidate genes, including CHRM4, the gene encoding the M4 receptor. Two genomic variants of the M4 receptor, rs2067482 and rs72910092, have also been reported to be associated with an increased risk of schizophrenia (136). It should be noted, however, that these allelic associations have not been consistently replicated across studies (137), which may be due to differences in the patient populations sampled and diagnostic subtyping.
Importantly, recent clinical results were released from a phase 1b placebo-controlled trial of emraclidine (CVL-231), an M4 receptor PAM, in patients with schizophrenia (138). In an exploratory analysis, treatment with CVL-231 was associated with reduced psychotic symptoms compared with placebo after 6 weeks of treatment (138). Rates of gastrointestinal adverse events were minimal compared to those in historical mAChR agonist trials (41, 69). These data provide additional evidence that M4 receptors play key roles in mediating the antipsychotic properties of mAChR agonists (138) and preliminary clinical validation for drugs that target allosteric binding pockets of mAChR receptors (in this case M4 receptors). Although encouraging, these data have yet to be peer reviewed, and further placebo-controlled trials of CVL-231 will be necessary to establish its efficacy and safety profile in patients with schizophrenia.
Role of M1 Receptors
Although an important role for M4 receptors in mediating the antipsychotic effects of xanomeline is quite likely (see above) there is also substantial evidence that M1 receptors regulate neural circuits underlying psychosis as well as learning and memory (especially working memory). Xanomeline’s “antipsychotic” activity as measured by amphetamine-induced hyperactivity was abolished in mice lacking M4 receptors but also was partially attenuated in mice lacking M1 receptors, suggesting that M4 receptors and, to a certain degree, M1 receptors may both contribute to xanomeline’s efficacy in treating the positive symptoms of schizophrenia (97). As xanomeline is a “dual” M1 and M4 receptor agonist, M1 receptors may also contribute to its reported antipsychotic and procognitive activity.
Several hypotheses have emerged regarding how M1 receptors may modulate neural circuits implicated in psychosis, including regulation of top-down circuits that synapse onto VTA DA neurons (Figure 6) (139, 140). For example, activation of M1 receptors facilitates excitability of cortical GABAergic interneurons that synapse onto pyramidal neurons (139), causing a decrease in excitability of principal cortical output neurons. However, there are additional hypotheses regarding how M1 receptor activators may exhibit antipsychotic activity, including augmentation of corticostriatal plasticity (141), modulation of MSN excitability (142), and enhanced communication between MSNs (e.g., via nucleus accumbens output neurons) (143). Additional studies have demonstrated a “psychosis-like” phenotype in global M1 receptor knockout mice (144) as well as antipsychotic drug–like activities in various preclinical models following administration of selective M1 receptor PAMs (145, 146). M1 receptor PAMs have also been reported to reverse excessive spontaneous locomotor activity in NMDA receptor NR1-subunit knockdown mice that display an NMDA receptor–mediated hypofunction phenotype (147).
FIGURE 6. Activation of M1 receptors in the frontal cortex exerts top-down control onto midbrain dopamine (DA) circuitsa
aAs illustrated in panel A, activation of M1 receptors expressed on layer II/III inhibitory GABAergic interneurons (pink) facilitates inhibitory drive onto excitatory output neurons (i.e., pyramidal neurons; green). In panel B, enhanced inhibitory drive onto pyramidal neurons decreases glutamatergic input to the ventral tegmental area (VTA). A reduction of excitatory input leads to a decrease in VTA dopamine (DA; red) neuron activity and reduced terminal DA release.
As summarized above, significant effort has been made to develop M1 receptor agonists to treat the cognitive impairment associated with various neuropsychiatric and neurodegenerative disorders (64, 70). In memory circuits, M1 receptor activators have been shown to enhance synaptic plasticity (85, 148), increase neuronal excitability (149), and facilitate learning and improve cognition in aged animals (150) and in a variety of NMDA receptor hypofunction models of impaired learning and memory (147, 149, 151, 152). Previous studies have shown that M1 receptors are physically and functionally coupled to NMDA receptors and that activation of M1 receptors potentiates NMDA receptor currents in cortical and hippocampal pyramidal neurons (54, 153, 154). Conversely, global M1 receptor knockout mice have impaired performance in prefrontal cortex–dependent cognitive tasks (155, 156) and reduced hippocampal long-term potentiation (157). Administration of an M1 receptor potentiator in genetic models of NMDA receptor hypofunction restored plasticity deficits and improved impaired learning and memory in these mice (147). Moreover, M1 receptor PAMs have been shown to modulate sleep-wake architecture in rodents and nonhuman primates (150), suggesting that activation of M1 receptors may participate in restorative sleep–mediated plasticity, which has been postulated to be dysregulated in patients with schizophrenia (158). Beyond cognition, M1 receptor PAMs have been reported to reverse behavioral and electrophysiological deficits in chronic PCP rodent models, which are thought to recapitulate the “deficit state” or negative symptoms of schizophrenia (149). Recently it was shown that M1 receptor PAMs can reverse PCP-induced disruption of mAChR-stimulated long-term depression (149), a plasticity measure that is important for adapting neural networks to physiological activity. These studies support the idea that M1 receptor activation may, by itself, contribute to improvements in the cognitive, negative, and even positive symptom domains of schizophrenia, and thus a dual M1/M4-preferring mAChR agonist may be particularly effective in treating schizophrenia.
As mentioned earlier, clozapine appears to be unique among the drugs used to treat schizophrenia, as it appears to be more effective in treating positive and negative symptoms in patients with treatment-resistant illness (159). Moreover, some (160) but not all (161) studies have reported that clozapine can improve cognition and especially working memory performance in patients with schizophrenia. Interestingly, although clozapine itself is a potent mAChR antagonist (162), its major metabolite, N-desmethylclozapine (NDMC), is a potent partial M1 receptor agonist (163). Recently, it has been reported by several groups that lower clozapine-to-NDMC ratios are associated with improvements in working memory and executive function, whereas higher ratios are associated with cognitive deficits (164–167). These findings raise the intriguing possibility that the M1 receptor activity of NDMC contributes to clozapine’s unique clinical profile, including its reported procognitive benefits (160). Several lines of evidence suggest that M1 receptors may also play a key role in the ability of clozapine to modulate schizophrenia-related circuity in rodents (168–170). Sub-efficacious doses of clozapine can reverse MK-801-induced deficits in sensorimotor gating, and this is potentiated by coadministration of an M1 receptor PAM (151). From a circuit-level perspective, local administration of NDMC can alter DA release in brain regions implicated in psychosis, an effect that is opposite to that of clozapine (171).
However, in preclinical models (172), and in marked contrast to clozapine, NDMC did not display antipsychotic activity, and a subsequent phase 2 clinical trial in patients with schizophrenia confirmed its lack of efficacy in treating positive symptoms (173). Although NDMC shares many of clozapine’s pharmacological properties beyond mAChR activity, it does not occupy or block DA D2 receptors (174); this may account for its lack of efficacy in treating positive symptoms. However, it is quite possible that NDMC accounts for the procognitive effects of clozapine and possibly its beneficial effects on negative symptoms. NDMC could also be responsible for some of the peripheral adverse effects observed with clozapine (175), such as hypersalivation. Moreover, the peripheral gastrointestinal adverse events reported for xanomeline are almost certainly due to stimulation of peripheral mAChRs. Nonetheless, these data fit with the hypothesis that M1 receptor activation could be a key mechanism through which clozapine exerts its unique clinical profile (175).
Previous studies have also suggested a role for M1 receptors in the pathophysiology of schizophrenia. For instance, using [123I]quinuclidinyl benzilate, mAChR availability was found to be reduced in unmedicated patients with schizophrenia (21), a finding similar to that in the postmortem studies. Several postmortem studies using the mAChR antagonist [3H]-pirenzepine have demonstrated decreased M1 receptor expression in cortical and subcortical regions in patients with schizophrenia (62, 176, 177). The authors refer to these patients as having “mAChR deficit” schizophrenia. Interestingly, whereas there is a pronounced loss of M1 receptors in the mAChR deficit schizophrenia subtype, the residual M1 population has increased receptor–G protein coupling efficiency, suggesting an adaptive change to compensate for reduced receptor expression (178). Importantly, these changes in M1 receptor expression appear to be specific to schizophrenia and may represent a distinguishable endophenotype (177). Additional evidence that M1 receptors may contribute to the pathophysiology of schizophrenia include recent reports that homozygous carriers of CHRM1 C267A nucleotide polymorphisms exhibit pronounced perseveration errors and poor performance on tests of executive functioning (179, 180). More recently, elevated serum titers of anti–M1 receptor antibodies have been reported in up to one-third of people diagnosed with schizophrenia (181, 182), and their presence was correlated with the severity of negative symptoms (181).
In actual practice, it is likely that many patients with schizophrenia will be treated simultaneously with conventional antipsychotic drugs and novel therapies to improve overall efficacy before they are switched to monotherapy with a novel drug (183). This concept is supported by preclinical data showing that treatment with the M1 PAM BQCA in combination with atypical antipsychotics (i.e., aripiprazole and clozapine) provided synergistic procognitive activity in deficit states induced by the NMDA receptor antagonist MK-801 (151). Although additional studies are needed to fully understand the underlying neural circuits involved in mediating the procognitive effects of BQCA, they likely involve modulation of hippocampal synaptic plasticity (184, 185).
In the context of psychosis, subeffective doses of the M4 PAM PGM039678 in combination with subeffective doses of the atypical antipsychotics olanzapine or risperidone significantly augmented conditioned avoidance responding in rats (186). Recently, it was also reported that subeffective doses of xanomeline augmented the activity of aripiprazole and risperidone in the conditioned avoidance response assay in mice (103). In the same study, subthreshold doses of xanomeline and risperidone administered together significantly attenuated MK-801-induced hyperactivity (103). These results raise the intriguing possibility that M1 receptor, M4 receptor, or dual M1/M4 receptor agonists may represent adjunctive treatments, when used together with currently prescribed first- or second-generation antipsychotics, to improve the core symptoms of schizophrenia, especially in patients with treatment-resistant illness.
Role of M2, M3, and M5 Receptors
Pharmacological studies using M2 receptor–preferring antagonists have produced contradictory results regarding their potential role in cognition. Whereas some studies suggest that blockade of central M2 receptors enhances learning and memory in various experimental settings (187), other studies arrived at the opposite conclusion (188). M2 receptor global knockout mice display deficits in behavioral flexibility, working memory, and passive avoidance learning (189). However, M2 receptors are apparently not required for stimulus-reward learning. Reduced expression of subcortical (190, 191) but not cortical (192) M2 receptors has also been found in patients with schizophrenia. In preclinical models, the antipsychotic-like activity of BuTAC, an M2 receptor–preferring orthosteric agonist and a partial M1/M4 receptor agonist, is lost in global M2/M4 double-knockout mice (193). From a microcircuit perspective, there appears to be a functional interplay between M2 and M4 receptors to regulate DA release in striatal regions (116), suggesting that M2 receptor activation may play an important role in M4-mediated suppression of DA release. Additional studies are needed to understand the therapeutic potential of dual M2-M4 receptor agonists or whether M2-M4 heterodimers play a role in psychosis.
The M3 receptor is expressed widely in the CNS, including in the hippocampus (194), and may play an important role in learning and memory. M3 receptor knockout mice have severe deficits in hippocampus-dependent memory, suggesting that selective M3 receptor activators may be beneficial for cognition (195). Recently, it has been reported that M3 receptors regulate feed-forward inhibition, which may facilitate memory consolidation by reducing interference signals (196). Detailed biochemical studies support an important role for M3 receptor signaling through phosphorylation events as contributing to these procognitive effects (195) and raise the possibility that M3 receptor–biased ligands that increase β-arrestin-dependent (non–G protein) signaling might promote cholinergic-mediated learning and memory (197).
Finally, M5 receptors may also be a promising drug target for schizophrenia given their expression in and control of midbrain DA neurons (198). M5 receptor global knockout mice display reduced striatal DA release and blunted responses in preclinical models of psychosis (199). Activation of M5 receptors increases the activity of midbrain DA neurons (200) to facilitate terminal DA release (201), suggesting that therapeutic agents that inhibit the M5 receptor will decrease elevated DA levels reported in various forebrain regions in schizophrenia. More recent preclinical evidence suggests that M5 receptor agonists or PAMs may also be effective for treating negative symptoms (202) and cognitive deficits (203). Continued efforts are needed to develop CNS-penetrant compounds with appreciable M5 receptor agonist or antagonist selectivity to further elucidate their potential benefits (204, 205). In this regard, xanomeline has been shown to be an M5 receptor partial agonist (206) and thus is likely to have a predominant M5 receptor antagonist pharmacological profile (206). The contribution, if any, of xanomeline’s M5 receptor activity, along with its M1 and M4 receptor pharmacology, to its reported clinical (antipsychotic and procognitive) activity in patients with schizophrenia is unclear but cannot be excluded.
Summary and Conclusions
Current treatments for schizophrenia include a wide array of antipsychotic drugs that are chemically distinct, but all target the DA D2 receptor, just like the very first antipsychotic drug, chlorpromazine, which was introduced in the United States 70 years ago (4, 207). With the exception of clozapine, all current antipsychotics have relatively similar efficacy profiles. These drugs work primarily to reduce the positive symptoms of schizophrenia, with little beneficial impact on either negative or cognitive symptoms (9). Currently approved antipsychotic drugs are all believed to work by initially binding to (and occupying) DA D2 receptors, where they behave as either antagonists or partial agonists/antagonists, leading to downstream adaptive neurochemical and neurophysiological changes in neural circuits underlying psychotic symptoms, which may also account for the time-dependent lag of several weeks for a maximal antipsychotic response (208). Due to their conserved pharmacology, these drugs all share many of the undesirable side effects and longer-term adverse events associated with their use, including extrapyramidal side effects, akathisia, sedation, weight gain, hyperprolactinemia, and a risk of developing tardive dyskinesia (5, 209), among others.
The need for new and mechanistically unique antipsychotic drugs that can treat not only the positive but also negative and cognitive symptoms of schizophrenia cannot be overstated (9). Based on the clinical observations of the antipsychotic properties of the M1/M4-preferring mAChR agonist xanomeline (22) and other mAChR agonists, it appears that mAChRs may represent viable non-DA D2 receptor drug targets for discovering mechanistically unique treatments for the core symptoms of schizophrenia. Preclinical and clinical data support the role of both the M1 and M4 mAChRs (as well as potentially other mAChRs) in mediating the antipsychotic and procognitive effects of xanomeline, as well as potentially other orthosteric and allosteric mAChR modulators. The evidence suggests that these drugs can rather rapidly and selectively impact the cellular and neural circuits that may underlie their novel antipsychotic and procognitive properties. mAChR agonists represent a promising new class of medication with the potential to treat the core symptoms of schizophrenia, including positive, negative, and cognitive symptoms, while not being associated with the long-term side effects of DA-based antipsychotics.
1 : Schizophrenia: an overview. JAMA Psychiatry 2020; 77:201–210Crossref, Medline, Google Scholar
2 : A systematic review of the prevalence of schizophrenia. PLoS Med 2005; 2:e141Crossref, Medline, Google Scholar
3 : Size of burden of schizophrenia and psychotic disorders. Eur Neuropsychopharmacol 2005; 15:399–409Crossref, Medline, Google Scholar
4 : Classics in chemical neuroscience: chlorpromazine. ACS Chem Neurosci 2019; 10:79–88Crossref, Medline, Google Scholar
5 : Comparative efficacy and tolerability of 32 oral antipsychotics for the acute treatment of adults with multi-episode schizophrenia: a systematic review and network meta-analysis. Focus (Am Psychiatr Publ) 2020; 18:443–455Medline, Google Scholar
6 : Dopamine targeting drugs for the treatment of schizophrenia: past, present, and future. Curr Top Med Chem 2016; 16:3385–3403Crossref, Medline, Google Scholar
7 : Glutamate and dopamine in schizophrenia: an update for the 21st century. J Psychopharmacol 2015; 29:97–115Crossref, Medline, Google Scholar
8 : Mechanisms underlying psychosis and antipsychotic treatment response in schizophrenia: insights from PET and SPECT imaging. Curr Pharm Des 2009; 15:2550–2559Crossref, Medline, Google Scholar
9 : Schizophrenia: overview and treatment options. P T 2014; 39:638–645Medline, Google Scholar
10 : Thinking and acting beyond the positive: the role of the cognitive and negative symptoms in schizophrenia. CNS Spectr 2014; 19:38–52Crossref, Medline, Google Scholar
11 : Management of common adverse effects of antipsychotic medications. World Psychiatry 2018; 17:341–356Crossref, Medline, Google Scholar
12 : Molecules and circuits implicated in schizophrenia provide leads for novel treatments. Am J Psychiatry 2020; 177:1099–1102Link, Google Scholar
13 : Review of cognitive impairment with antimuscarinic agents in elderly patients with overactive bladder. Int J Clin Pract 2010; 64:1279–1286Crossref, Medline, Google Scholar
14 : Muscarinic receptor occupancy and cognitive impairment: a PET study with [11C](+)3-MPB and scopolamine in conscious monkeys. Neuropsychopharmacology 2011; 36:1455–1465Crossref, Medline, Google Scholar
15 : Toxic psychoses from atropine and scopolamine. Fortschr Neurol Psychiatr 1998; 66:289–295Medline, Google Scholar
16 : Transdermal scopolamine-induced psychosis. Postgrad Med 1988; 84:73–76Crossref, Medline, Google Scholar
17 : The inhibition of the conditioned response and the counteraction of schizophrenia by muscarinic stimulation of the brain. Ann N Y Acad Sci 1957; 66:753–764Crossref, Medline, Google Scholar
18 : Global epidemiology of areca nut usage. Addict Biol 2002; 7:77–83Crossref, Medline, Google Scholar
19 : Potential action of betel alkaloids on positive and negative symptoms of schizophrenia: a review. Nord J Psychiatry 2012; 66:73–78Crossref, Medline, Google Scholar
20 : Effects of chewing betel nut (Areca catechu) on the symptoms of people with schizophrenia in Palau, Micronesia. Br J Psychiatry 2000; 177:174–178Crossref, Medline, Google Scholar
21 : Towards a muscarinic hypothesis of schizophrenia. Mol Psychiatry 2007; 12:232–246Crossref, Medline, Google Scholar
22 : Effects of xanomeline, a selective muscarinic receptor agonist, on cognitive function and behavioral symptoms in Alzheimer disease. Arch Neurol 1997; 54:465–473Crossref, Medline, Google Scholar
23 : Selective muscarinic receptor agonist xanomeline as a novel treatment approach for schizophrenia. Am J Psychiatry 2008; 165:1033–1039Link, Google Scholar
24 : Xanomeline, an M1/M4 preferring muscarinic cholinergic receptor agonist, produces antipsychotic-like activity in rats and mice. Schizophr Res 2000; 42:249–259Crossref, Medline, Google Scholar
25 : The muscarinic receptor agonist xanomeline has an antipsychotic-like profile in the rat. J Pharmacol Exp Ther 2001; 299:782–792Medline, Google Scholar
26 : Xanomeline: a novel muscarinic receptor agonist with functional selectivity for M1 receptors. J Pharmacol Exp Ther 1994; 269:271–281Medline, Google Scholar
27 : Henry Dale and the discovery of acetylcholine. C R Biol 2006; 329:419–425Crossref, Medline, Google Scholar
28 : Acetylcholine as a neuromodulator: cholinergic signaling shapes nervous system function and behavior. Neuron 2012; 76:116–129Crossref, Medline, Google Scholar
29 : Muscarinic acetylcholine receptors: signal transduction through multiple effectors. FASEB J 1995; 9:619–625Crossref, Medline, Google Scholar
30 : GPCR signaling regulation: the role of GRKs and arrestins. Front Pharmacol 2019; 10:125Crossref, Medline, Google Scholar
31 : Muscarinic acetylcholine receptors: novel opportunities for drug development. Nat Rev Drug Discov 2014; 13:549–560Crossref, Medline, Google Scholar
32 : Muscarinic receptors: characterization, coupling, and function. Pharmacol Ther 1993; 58:319–379Crossref, Medline, Google Scholar
33 : Identification and localization of muscarinic acetylcholine receptor proteins in brain with subtype-specific antibodies. J Neurosci 1991; 11:3218–3226Crossref, Medline, Google Scholar
34 : Characterization of central inhibitory muscarinic autoreceptors by the use of muscarinic acetylcholine receptor knock-out mice. J Neurosci 2002; 22:1709–1717Crossref, Medline, Google Scholar
35 : Association of M1 and M2 muscarinic receptor proteins with asymmetric synapses in the primate cerebral cortex: morphological evidence for cholinergic modulation of excitatory neurotransmission. Proc Natl Acad Sci USA 1993; 90:5194–5198Crossref, Medline, Google Scholar
36 : Coordinated expression of muscarinic receptor messenger RNAs in striatal medium spiny neurons. Neuroscience 2001; 103:1017–1024Crossref, Medline, Google Scholar
37 : Differential regulation of molecular subtypes of muscarinic receptors in Alzheimer’s disease. J Neurochem 1995; 64:1888–1891Crossref, Medline, Google Scholar
38 : Localization of M5 muscarinic receptor mRNA in rat brain examined by in situ hybridization histochemistry. Neurosci Lett 1990; 114:154–159Crossref, Medline, Google Scholar
39 : The use of chemogenetic approaches to study the physiological roles of muscarinic acetylcholine receptors in the central nervous system. Neuropharmacology 2018; 136:421–426Crossref, Medline, Google Scholar
40 : Muscarinic receptor subtype distribution in the central nervous system and relevance to aging and Alzheimer’s disease. Neuropharmacology 2018; 136:362–373Crossref, Medline, Google Scholar
41 : Cognitive effects of muscarinic M1 functional agonists in non-human primates and clinical trials. Curr Opin Investig Drugs 2010; 11:740–760Medline, Google Scholar
42 : Tools for GPCR drug discovery. Acta Pharmacol Sin 2012; 33:372–384Crossref, Medline, Google Scholar
43 : Muscarinic acetylcholine receptors: typical G-coupled receptors. Symp Soc Exp Biol 1990; 44:39–54Medline, Google Scholar
44 : Cryptic pocket formation underlies allosteric modulator selectivity at muscarinic GPCRs. Nat Commun 2019; 10:3289Crossref, Medline, Google Scholar
45 : Structures of the M1 and M2 muscarinic acetylcholine receptor/G-protein complexes. Science 2019; 364:552–557Crossref, Medline, Google Scholar
46 : Crystal structures of the M1 and M4 muscarinic acetylcholine receptors. Nature 2016; 531:335–340Crossref, Medline, Google Scholar
47 : Fine tuning muscarinic acetylcholine receptor signaling through allostery and bias. Front Pharmacol 2021; 11:606656Crossref, Medline, Google Scholar
48 : Use of M1–M5 muscarinic receptor knockout mice as novel tools to delineate the physiological roles of the muscarinic cholinergic system. Neurochem Res 2003; 28:437–442Crossref, Medline, Google Scholar
49 : Muscarinic acetylcholine receptors: mutant mice provide new insights for drug development. Nat Rev Drug Discov 2007; 6:721–733Crossref, Medline, Google Scholar
50 : Physiological roles of CNS muscarinic receptors gained from knockout mice. Neuropharmacology 2018; 136:411–420Crossref, Medline, Google Scholar
51 : Allosteric modulators of GPCRs: a novel approach for the treatment of CNS disorders. Nat Rev Drug Discov 2009; 8:41–54Crossref, Medline, Google Scholar
52 : GPCR drug discovery: moving beyond the orthosteric to the allosteric domain. Adv Pharmacol 2019; 86:1–20Crossref, Medline, Google Scholar
53 : Current advances in allosteric modulation of muscarinic receptors. Biomolecules 2020; 10:325Crossref, Google Scholar
54 : A selective allosteric potentiator of the M1 muscarinic acetylcholine receptor increases activity of medial prefrontal cortical neurons and restores impairments in reversal learning. J Neurosci 2009; 29:14271–14286Crossref, Medline, Google Scholar
55 : A Monod-Wyman-Changeux mechanism can explain G protein-coupled receptor (GPCR) allosteric modulation. J Biol Chem 2012; 287:650–659Crossref, Medline, Google Scholar
56 : M4 muscarinic receptor signaling ameliorates striatal plasticity deficits in models of l-DOPA-induced dyskinesia. Neuron 2016; 90:1139Crossref, Medline, Google Scholar
57 : Direct interaction of GABAB receptors with M2 muscarinic receptors enhances muscarinic signaling. J Neurosci 2009; 29:15796–15809Crossref, Medline, Google Scholar
58 : Quantitative analysis of muscarinic acetylcholine receptor homo- and heterodimerization in live cells: regulation of receptor down-regulation by heterodimerization. J Biol Chem 2006; 281:5416–5425Crossref, Medline, Google Scholar
59 : Pharmacological evidence of muscarinic receptor heterodimerization. Pharm Acta Helv 2000; 74:315–326Crossref, Medline, Google Scholar
60 : Allosteric modulation of the muscarinic M4 receptor as an approach to treating schizophrenia. Proc Natl Acad Sci USA 2008; 105:10978–10983Crossref, Medline, Google Scholar
61 : Allosteric modulation of GPCRs: new insights and potential utility for treatment of schizophrenia and other CNS disorders. Neuron 2017; 94:431–446Crossref, Medline, Google Scholar
62 : Widespread changes in positive allosteric modulation of the muscarinic M1 receptor in some participants with schizophrenia. Int J Neuropsychopharmacol 2019; 22:640–650Crossref, Medline, Google Scholar
63 : Muscarinic acetylcholine receptor subtypes as potential drug targets for the treatment of schizophrenia, drug abuse, and Parkinson’s disease. ACS Chem Neurosci 2012; 3:80–89Crossref, Medline, Google Scholar
64 : M1 muscarinic acetylcholine receptors: a therapeutic strategy for symptomatic and disease-modifying effects in Alzheimer’s disease? Adv Pharmacol 2020; 88:277–310Crossref, Medline, Google Scholar
65 : M1 muscarinic agonists target major hallmarks of Alzheimer’s disease: an update. Curr Alzheimer Res 2007; 4:577–580Crossref, Medline, Google Scholar
66 : Potential role of muscarinic agonists in Alzheimer’s disease. Drugs Aging 1997; 11:450–459Crossref, Medline, Google Scholar
67 : Design, synthesis, and neurochemical evaluation of 2-amino-5-(alkoxycarbonyl)-3,4,5,6-tetrahydropyridines and 2-amino-5-(alkoxycarbonyl)-1,4,5,6-tetrahydropyrimidines as M1 muscarinic receptor agonists. J Med Chem 1994; 37:2774–2782Crossref, Medline, Google Scholar
68 : Design and development of selective muscarinic agonists for the treatment of Alzheimer’s disease: characterization of tetrahydropyrimidine derivatives and development of new approaches for improved affinity and selectivity for M1 receptors. Pharm Acta Helv 2000; 74:135–140Crossref, Medline, Google Scholar
69 : M1 muscarinic agonists target major hallmarks of Alzheimer’s disease: the pivotal role of brain M1 receptors. Neurodegener Dis 2008; 5:237–240Crossref, Medline, Google Scholar
70 : Current status of muscarinic M1 and M4 receptors as drug targets for neurodegenerative diseases. Neuropharmacology 2018; 136:449–458Crossref, Medline, Google Scholar
71 : Muscarinic and nicotinic acetylcholine receptor agonists: current scenario in Alzheimer’s disease therapy. J Pharm Pharmacol 2018; 70:985–993Crossref, Medline, Google Scholar
72 : M1 agonists for the treatment of Alzheimer’s disease: novel properties and clinical update. Ann NY Acad Sci 1996; 777:189–196Crossref, Medline, Google Scholar
73 : Failure of muscarinic agonists in the treatment of dementia of the Alzheimer type. Neurology 1999; 52:A398Medline, Google Scholar
74 : Efficacy and safety of SB 202026 as a symptomatic treatment for Alzheimer’s disease. Neurobiol Aging 1996; 17(suppl 1):S161Crossref, Google Scholar
75 : Cholinergic receptors and neurodegenerative diseases. Pharm Acta Helv 2000; 74:85–89Crossref, Medline, Google Scholar
76 Sharpe PC, Blower PR, Rasmussen JG, inventors; Minster Research Ltd, assignee: Mono and Combination Therapy with a M1/M4 Muscarinic Agonist (Sabcomeline) for Treatment of Cognitive Disorders in Schizophrenia. United States patent application US 12/226,431. 2009Google Scholar
77 : Xanomeline plus trospium: a novel strategy to enhance pro-muscarinic efficacy and mitigate peripheral side effects. Presented at the
78 : Trospium chloride: a quaternary amine with unique pharmacologic properties. Curr Urol Rep 2003; 4:436–440Crossref, Medline, Google Scholar
79 : Xanomeline and the antipsychotic potential of muscarinic receptor subtype selective agonists. CNS Drug Rev 2003; 9:159–186Crossref, Medline, Google Scholar
80 : Determination of xanomeline and active metabolite, N-desmethylxanomeline, in human plasma by liquid chromatography-atmospheric pressure chemical ionization mass spectrometry. J Chromatogr B Biomed Appl 1995; 668:273–280Crossref, Medline, Google Scholar
81 : PET study of the M1-agonists [11C]xanomeline and [11C]butylthio-TZTP in monkey and man. Dementia 1996; 7:187–195Medline, Google Scholar
82 : Muscarinic cholinergic receptor agonist and peripheral antagonist for schizophrenia. N Engl J Med 2021; 384:717–726Crossref, Medline, Google Scholar
83 : P.0794: KarXT treatment improves cognitive performance in cognitively impaired patients with schizophrenia: a post-hoc analysis of the phase 2 EMERGENT-1 study. Eur Neuropsychopharmacol 2021; 53:S580–S581Crossref, Google Scholar
84 : Functional comparison of muscarinic partial agonists at muscarinic receptor subtypes hM1, hM2, hM3, hM4, and hM5 using microphysiometry. Br J Pharmacol 1999; 126:1620–1624Crossref, Medline, Google Scholar
85 : Effects of M1 and M4 activation on excitatory synaptic transmission in CA1. Hippocampus 2017; 27:794–810Crossref, Medline, Google Scholar
86 : Functional effects of the muscarinic receptor agonist, xanomeline, at 5-HT1 and 5-HT2 receptors. Br J Pharmacol 1998; 125:1413–1420Crossref, Medline, Google Scholar
87 : Pharmacological comparison of muscarinic ligands: historical versus more recent muscarinic M1-preferring receptor agonists. Eur J Pharmacol 2009; 605:53–56Crossref, Medline, Google Scholar
88 : Antipsychotic-like effect of the muscarinic acetylcholine receptor agonist BuTAC in non-human primates. PLoS One 2015; 10:e0122722Crossref, Medline, Google Scholar
89 : Activation and allosteric modulation of a muscarinic acetylcholine receptor. Nature 2013; 504:101–106Crossref, Medline, Google Scholar
90 : The muscarinic M1/M4 receptor agonist xanomeline exhibits antipsychotic-like activity in Cebus apella monkeys. Neuropsychopharmacology 2003; 28:1168–1175Crossref, Medline, Google Scholar
91 : Wash-resistantly bound xanomeline inhibits acetylcholine release by persistent activation of presynaptic M(2) and M(4) muscarinic receptors in rat brain. J Pharmacol Exp Ther 2007; 322:316–323Crossref, Medline, Google Scholar
92 : Long-term wash-resistant effects of brief interaction of xanomeline at the M1 muscarinic receptor. Neurosci Lett 2006; 410:11–14Crossref, Medline, Google Scholar
93 : Novel persistent activation of muscarinic M1 receptors by xanomeline. Eur J Pharmacol 1997; 334:R3–R4Crossref, Medline, Google Scholar
94 : Molecular mechanism of antipsychotic xanomeline’s selectivity at muscarinic receptors. Presented at the
95 : Pharmacologic interactions between the muscarinic cholinergic and dopaminergic systems in the modulation of prepulse inhibition in rats. J Pharmacol Exp Ther 2005; 312:1055–1063Crossref, Medline, Google Scholar
96 : Acute and chronic effects of the M1/M4-preferring muscarinic agonist xanomeline on cocaine vs food choice in rats. Psychopharmacology (Berl) 2014; 231:469–479Crossref, Medline, Google Scholar
97 : Attenuation of amphetamine-induced activity by the non-selective muscarinic receptor agonist, xanomeline, is absent in muscarinic M4 receptor knockout mice and attenuated in muscarinic M1 receptor knockout mice. Eur J Pharmacol 2009; 603:147–149Crossref, Medline, Google Scholar
98 : The M1/M4 preferring agonist xanomeline reverses amphetamine-, MK801-, and scopolamine-induced abnormalities of latent inhibition: putative efficacy against positive, negative, and cognitive symptoms in schizophrenia. Int J Neuropsychopharmacol 2011; 14:1233–1246Crossref, Medline, Google Scholar
99 : In vivo pharmacological comparison of TAK-071, a positive allosteric modulator of muscarinic M1 receptor, and xanomeline, an agonist of muscarinic M1/M4 receptor, in rodents. Neuroscience 2019; 414:60–76Crossref, Medline, Google Scholar
100 : Muscarinic receptor agonists, like dopamine receptor antagonist antipsychotics, inhibit conditioned avoidance response in rats. J Pharmacol Exp Ther 1999; 290:901–907Medline, Google Scholar
101 : Xanomeline modulation of the blood oxygenation level-dependent signal in awake rats: development of pharmacological magnetic resonance imaging as a translatable pharmacodynamic biomarker for central activity and dose selection. J Pharmacol Exp Ther 2012; 341:263–273Crossref, Medline, Google Scholar
102 : The M1/M4 preferring muscarinic agonist xanomeline modulates functional connectivity and NMDAR antagonist-induced changes in the mouse brain. Neuropsychopharmacology, 2021; 46:1194–1206Crossref, Medline, Google Scholar
103 : P0837. Xanomeline’s activity in rodent models of psychosis: role of central muscarinic receptors and augmentation by risperidone and aripiprazole. Presented at the
104 : The role of dopamine in schizophrenia from a neurobiological and evolutionary perspective: old fashioned, but still in vogue. Front Psychiatry 2014; 5:47Medline, Google Scholar
105 : Dopamine-cell depolarization block as a model for the therapeutic actions of antipsychotic drugs. Trends Neurosci 1997; 20:31–37Crossref, Medline, Google Scholar
106 : Typical and atypical neuroleptics: differential effects of chronic administration on the activity of A9 and A10 midbrain dopaminergic neurons. J Neurosci 1983; 3:1607–1619Crossref, Medline, Google Scholar
107 : Antipsychotic drugs rapidly induce dopamine neuron depolarization block in a developmental rat model of schizophrenia. J Neurosci 2011; 31:12330–12338Crossref, Medline, Google Scholar
108 : Cholinergic modulation of mesolimbic dopamine function and reward. Physiol Behav 2011; 104:76–81Crossref, Medline, Google Scholar
109 : M4 muscarinic receptors regulate the dynamics of cholinergic and dopaminergic neurotransmission: relevance to the pathophysiology and treatment of related CNS pathologies. FASEB J 2004; 18:1410–1412Crossref, Medline, Google Scholar
110 : Cholinergic modulation of midbrain dopaminergic systems. Brain Res Rev 2008; 58:265–271Crossref, Medline, Google Scholar
111 : Cholinergic mesopontine signals govern locomotion and reward through dissociable midbrain pathways. Neuron 2016; 90:333–347Crossref, Medline, Google Scholar
112 : The depolarization block hypothesis of neuroleptic action: implications for the etiology and treatment of schizophrenia. J Neural Transm Suppl 1992; 36:91–131Medline, Google Scholar
113 : Induction of depolarization block in midbrain dopamine neurons by repeated administration of haloperidol: analysis using in vivo intracellular recording. J Pharmacol Exp Ther 1986; 238:1092–1100Medline, Google Scholar
114 : The muscarinic agonist xanomeline increases monoamine release and immediate early gene expression in the rat prefrontal cortex. Biol Psychiatry 2001; 49:716–725Crossref, Medline, Google Scholar
115 : Striatal dopamine release is triggered by synchronized activity in cholinergic interneurons. Neuron 2012; 75:58–64Crossref, Medline, Google Scholar
116 : Dopamine signaling in dorsal versus ventral striatum: the dynamic role of cholinergic interneurons. Front Syst Neurosci 2011; 5:11Crossref, Medline, Google Scholar
117 : Striatal muscarinic receptors promote activity dependence of dopamine transmission via distinct receptor subtypes on cholinergic interneurons in ventral versus dorsal striatum. J Neurosci 2010; 30:3398–3408Crossref, Medline, Google Scholar
118 : Involvement of a subpopulation of neuronal M4 muscarinic acetylcholine receptors in the antipsychotic-like effects of the M1/M4 preferring muscarinic receptor agonist xanomeline. J Neurosci 2011; 31:5905–5908Crossref, Medline, Google Scholar
119 : A subpopulation of neuronal M4 muscarinic acetylcholine receptors plays a critical role in modulating dopamine-dependent behaviors. J Neurosci 2010; 30:2396–2405Crossref, Medline, Google Scholar
120 : Antipsychotic-like effects of M4 positive allosteric modulators are mediated by CB2 receptor-dependent inhibition of dopamine release. Neuron 2016; 91:1244–1252Crossref, Medline, Google Scholar
121 : Activation of the mGlu1 metabotropic glutamate receptor has antipsychotic-like effects and is required for efficacy of M4 muscarinic receptor allosteric modulators. Mol Psychiatry 2020; 25:2786–2799Crossref, Medline, Google Scholar
122 : Modulation of direct pathway striatal projection neurons by muscarinic M4-type receptors. Neuropharmacology 2015; 89:232–244Crossref, Medline, Google Scholar
123 : Selective activation of M4 muscarinic acetylcholine receptors reverses MK-801-induced behavioral impairments and enhances associative learning in rodents. ACS Chem Neurosci 2014; 5:920–942Crossref, Medline, Google Scholar
124 : Muscarinic and nicotinic acetylcholine receptor agonists and allosteric modulators for the treatment of schizophrenia. Neuropsychopharmacology 2012; 37:16–42Crossref, Medline, Google Scholar
125 : State-dependent alterations in sleep/wake architecture elicited by the M4 PAM VU0467154: relation to antipsychotic-like drug effects. Neuropharmacology 2016; 102:244–253Crossref, Medline, Google Scholar
126 : Positive allosteric modulation of M1 and M4 muscarinic receptors as potential therapeutic treatments for schizophrenia. Neuropharmacology 2018; 136:438–448Crossref, Medline, Google Scholar
127 : NMDAR hypofunction animal models of schizophrenia. Front Mol Neurosci 2019; 12:185Crossref, Medline, Google Scholar
128 : Fifty years of research on schizophrenia: the ascendance of the glutamatergic synapse. Am J Psychiatry 2020; 177:1119–1128Link, Google Scholar
129 : M4 mAChR-mediated modulation of glutamatergic transmission at corticostriatal synapses. ACS Chem Neurosci 2014; 5:318–324Crossref, Medline, Google Scholar
130 : Evaluating novel muscarinic acetylcholine receptor potentiators for the treatment of cognitive deficits in schizophrenia. Vanderbilt University, 2017. PhD thesis. https://ir.vanderbilt.edu/handle/1803/14700?show=fullGoogle Scholar
131 : Cognitive enhancement and antipsychotic-like activity following repeated dosing with the selective M4 PAM VU0467154. Neuropharmacology 2018; 128:492–502Crossref, Medline, Google Scholar
132 : Altered hippocampal muscarinic M4, but not M1, receptor expression from subjects with schizophrenia. Biol Psychiatry 2007; 61:1161–1170Crossref, Medline, Google Scholar
133 : Investigation of M1/M4 muscarinic receptors in the anterior cingulate cortex in schizophrenia, bipolar disorder, and major depression disorder. Neuropsychopharmacology 2004; 29:619–625Crossref, Medline, Google Scholar
134 : Possible involvement of muscarinic receptors in psychiatric disorders: a focus on schizophrenia and mood disorders. Curr Mol Med 2015; 15:253–264Crossref, Medline, Google Scholar
135 : Association between genetic variation in a region on chromosome 11 and schizophrenia in large samples from Europe. Mol Psychiatry 2012; 17:906–917Crossref, Medline, Google Scholar
136 : Cholinergic muscarinic M4 receptor gene polymorphisms: a potential risk factor and pharmacogenomic marker for schizophrenia. Schizophrenia Res 2013; 146:279–284Crossref, Medline, Google Scholar
137 : Association of cholinergic muscarinic M4 receptor gene polymorphism with schizophrenia. Appl Clin Genet 2020; 13:97–105Crossref, Medline, Google Scholar
138 : Press release: Cerevel therapeutics announces positive topline results for CVL-231 in phase 1b clinical trial in patients with schizophrenia. June 29, 2021. https://investors.cerevel.com/news-releases/news-release-details/cerevel-therapeutics-announces-positive-topline-results-cvl-231Google Scholar
139 : Direct excitation of parvalbumin-positive interneurons by M1 muscarinic acetylcholine receptors: roles in cellular excitability, inhibitory transmission, and cognition. J Physiol 2014; 592:3463–3494Crossref, Medline, Google Scholar
140 : Immunolocalization of muscarinic M1 receptor in the rat medial prefrontal cortex. J Comp Neurol 2018; 526:1329–1350Crossref, Medline, Google Scholar
141 : Muscarinic M1 receptor modulation of synaptic plasticity in nucleus accumbens of wild-type and fragile X mice. ACS Chem Neurosci 2018; 9:2233–2240Crossref, Medline, Google Scholar
142 : M1 muscarinic activation induces long-lasting increase in intrinsic excitability of striatal projection neurons. Neuropharmacology 2017; 118:209–222Crossref, Medline, Google Scholar
143 : High-frequency activation of nucleus accumbens D1-MSNs drives excitatory potentiation on D2-MSNs. Neuron 2019; 103:432–444.e3Crossref, Medline, Google Scholar
144 : Hyperactivity, elevated dopaminergic transmission, and response to amphetamine in M1 muscarinic acetylcholine receptor-deficient mice. Proc Natl Acad Sci USA 2001; 98:15312–15317Crossref, Medline, Google Scholar
145 : Novel selective allosteric activator of the M1 muscarinic acetylcholine receptor regulates amyloid processing and produces antipsychotic-like activity in rats. J Neurosci 2008; 28:10422–10433Crossref, Medline, Google Scholar
146 : Design and optimization of selective azaindole amide M1 positive allosteric modulators. Bioorg Med Chem Lett 2016; 26:650–655Crossref, Medline, Google Scholar
147 : Prefrontal cortex-mediated impairments in a genetic model of NMDA receptor hypofunction are reversed by the novel M1 PAM VU6004256. ACS Chem Neurosci 2016; 7:1706–1716Crossref, Medline, Google Scholar
148 : M1 and M4 receptors modulate hippocampal pyramidal neurons. J Neurophysiol 2011; 105:779–792Crossref, Medline, Google Scholar
149 : Potentiation of M1 muscarinic receptor reverses plasticity deficits and negative and cognitive symptoms in a schizophrenia mouse model. Neuropsychopharmacology 2016; 41:598–610Crossref, Medline, Google Scholar
150 : Modulation of arousal and sleep/wake architecture by M1 PAM VU0453595 across young and aged rodents and nonhuman primates. Neuropsychopharmacology 2020; 45:2219–2228Crossref, Medline, Google Scholar
151 : Positive allosteric modulation of the muscarinic M1 receptor improves efficacy of antipsychotics in mouse glutamatergic deficit models of behavior. J Pharmacol Exp Ther 2016; 359:354–365Crossref, Medline, Google Scholar
152 : Muscarinic M1 receptors modulate working memory performance and activity via KCNQ potassium channels in the primate prefrontal cortex. Neuron 2020; 106:649–661.e4Crossref, Medline, Google Scholar
153 : Activation of the genetically defined m1 muscarinic receptor potentiates N-methyl-d-aspartate (NMDA) receptor currents in hippocampal pyramidal cells. Proc Natl Acad Sci USA 1998; 95:11465–11470Crossref, Medline, Google Scholar
154 : Muscarinic receptor stimulation reduces NMDA responses in CA3 hippocampal pyramidal cells via Ca2+-dependent activation of tyrosine phosphatase. Neuropharmacology 2005; 49:328–337Crossref, Medline, Google Scholar
155 : Selective cognitive dysfunction in acetylcholine M1 muscarinic receptor mutant mice. Nat Neurosci 2003; 6:51–58Crossref, Medline, Google Scholar
156 : Role for the M1 muscarinic acetylcholine receptor in top-down cognitive processing using a touchscreen visual discrimination task in mice. ACS Chem Neurosci 2015; 6:1683–1695Crossref, Medline, Google Scholar
157 : Facilitation of long-term potentiation by muscarinic M(1) receptors is mediated by inhibition of SK channels. Neuron 2010; 68:948–963Crossref, Medline, Google Scholar
158 : Disrupted sleep and circadian rhythms in schizophrenia and their interaction with dopamine signaling. Front Neurosci 2020; 14:636Crossref, Medline, Google Scholar
159 : Heterogeneity and efficacy of antipsychotic treatment for schizophrenia with or without treatment resistance: a meta-analysis. Neuropsychopharmacology 2020; 45:622–631Crossref, Medline, Google Scholar
160 : Improvement in cognitive functions and psychiatric symptoms in treatment-refractory schizophrenic patients receiving clozapine. Biol Psychiatry 1993; 34:702–712Crossref, Medline, Google Scholar
161 : Second-generation antipsychotic effect on cognition in patients with schizophrenia: a meta-analysis of randomized clinical trials. Acta Psychiatr Scand 2015; 131:185–196Crossref, Medline, Google Scholar
162 : Antischizophrenic drugs and brain cholinergic receptors: affinity for muscarinic sites predicts extrapyramidal effects. Arch Gen Psychiatry 1974; 31:58–61Crossref, Medline, Google Scholar
163 : The highly efficacious actions of N-desmethylclozapine at muscarinic receptors are unique and not a common property of either typical or atypical antipsychotic drugs: is M1 agonism a pre-requisite for mimicking clozapine’s actions? Psychopharmacology (Berl) 2005; 178:451–460Crossref, Medline, Google Scholar
164 : Associations between plasma clozapine/N-desmethylclozapine ratio, insulin resistance, and cognitive performance in patients with co-morbid obesity and ultra-treatment resistant schizophrenia. Sci Rep 2021; 11:2004Crossref, Medline, Google Scholar
165 : Plasma ratio of clozapine to N-desmethylclozapine can predict cognitive performance in treatment-resistant psychotic patients. Psychiatry Res 2017; 258:153–157Crossref, Medline, Google Scholar
166 : Relationship of change in plasma clozapine/N-desmethylclozapine ratio with cognitive performance in patients with schizophrenia. Psychiatry Investig 2020; 17:1158–1165Crossref, Medline, Google Scholar
167 : Prediction of working memory performance in schizophrenia by plasma ratio of clozapine to N-desmethylclozapine. Am J Psychiatry 2015; 172:579–585Link, Google Scholar
168 : Muscarinic receptor signaling contributes to atypical antipsychotic drug reversal of the phencyclidine-induced deficit in novel object recognition in rats. J Psychopharmacol 2017; 31:1588–1604Crossref, Medline, Google Scholar
169 : The role of M1 muscarinic cholinergic receptors in the discriminative stimulus properties of N-desmethylclozapine and the atypical antipsychotic drug clozapine in rats. Psychopharmacology (Berl) 2009; 203:295–301Crossref, Medline, Google Scholar
170 : N-desmethylclozapine, an allosteric agonist at muscarinic 1 receptor, potentiates N-methyl-d-aspartate receptor activity. Proc Natl Acad Sci USA 2003; 100:13674–13679Crossref, Medline, Google Scholar
171 : N-desmethylclozapine, a major metabolite of clozapine, increases cortical acetylcholine and dopamine release in vivo via stimulation of M1 muscarinic receptors. Neuropsychopharmacology 2005; 30:1986–1995Crossref, Medline, Google Scholar
172 : Evaluation of N-desmethylclozapine as a potential antipsychotic: preclinical studies. Neuropsychopharmacology 2007; 32:1540–1549Crossref, Medline, Google Scholar
173 : ACADIA pharmaceuticals announces results from ACP-104 phase IIb schizophrenia trial. June 16, 2008. https://ir.acadia-pharm.com/news-releases/news-release-details/acadia-pharmaceuticals-announces-results-acp-104-phase-iib?fie ld_nir_news_date_value%5Bmin%5D=Google Scholar
174 : The role of M1 muscarinic receptor agonism of N-desmethylclozapine in the unique clinical effects of clozapine. Psychopharmacology (Berl) 2004; 177:207–216Crossref, Medline, Google Scholar
175 : A novel antipsychotic agent. N Engl J Med 1991; 324:746–754Crossref, Medline, Google Scholar
176 : Decreased cortical muscarinic M1 receptors in schizophrenia are associated with changes in gene promoter methylation, mRNA, and gene targeting microRNA. Transl Psychiatry 2013; 3:e230Crossref, Medline, Google Scholar
177 : Low levels of muscarinic M1 receptor-positive neurons in cortical layers III and V in Brodmann areas 9 and 17 from individuals with schizophrenia. J Psychiatry Neurosci 2018; 43:338–346Crossref, Medline, Google Scholar
178 : Altered M(1) muscarinic acetylcholine receptor (CHRM1)-Galpha(q/11) coupling in a schizophrenia endophenotype. Neuropsychopharmacology 2009; 34:2156–2166Crossref, Medline, Google Scholar
179 : The effect of a muscarinic receptor 1 gene variant on grey matter volume in schizophrenia. Psychiatry Res 2015; 234:182–187Crossref, Medline, Google Scholar
180 : Association of muscarinic M1 receptor genetic polymorphisms with psychiatric symptoms and cognitive function in schizophrenic patients. Neuropsychobiology 2003; 48:72–76Crossref, Medline, Google Scholar
181 : Elevated levels of autoantibodies targeting the M1 muscarinic acetylcholine receptor and neurofilament medium in sera from subgroups of patients with schizophrenia. J Neuroimmunol 2014; 269:68–75Crossref, Medline, Google Scholar
182 : Autoantibodies against four kinds of neurotransmitter receptors in psychiatric disorders. J Neuroimmunol 2003; 141:155–164Crossref, Medline, Google Scholar
183 : Antipsychotic combinations vs monotherapy in schizophrenia: a meta-analysis of randomized controlled trials. Schizophr Bull 2009; 35:443–457Crossref, Medline, Google Scholar
184 : Effects of selective M1 muscarinic receptor activation on hippocampal spatial representations and neuronal oscillations. ACS Chem Neurosci 2016; 7:1393–1405Crossref, Medline, Google Scholar
185 : Selective activation of the M1 muscarinic acetylcholine receptor achieved by allosteric potentiation. Proc Natl Acad Sci USA 2009; 106:15950–15955Crossref, Medline, Google Scholar
186 : Characterization of PGM039678, a positive allosteric modulator of the muscarinic M4 receptor, in animal models of schizophrenia. Presented at the
187 : Facilitation of acetylcholine release and cognitive performance by an M(2)-muscarinic receptor antagonist in aged memory-impaired. J Neurosci 1995; 15:1455–1462Crossref, Medline, Google Scholar
188 : Intrahippocampal injections of gallamine impair learning of a memory task. Neurosci Lett 1988; 89:367–372Crossref, Medline, Google Scholar
189 : M2 muscarinic acetylcholine receptor knock-out mice show deficits in behavioral flexibility, working memory, and hippocampal plasticity. J Neurosci 2004; 24:10117–10127Crossref, Medline, Google Scholar
190 : The binding of [3H]AF-DX 384 is reduced in the caudate-putamen of subjects with schizophrenia. Life Sci 1999; 64:1761–1771Crossref, Medline, Google Scholar
191 : M2/M4 muscarinic receptor binding in the anterior cingulate cortex in schizophrenia and mood disorders. Brain Res Bull 2005; 65:397–403Crossref, Medline, Google Scholar
192 : No change in cortical muscarinic M2, M3 receptors or [35S]GTPgammaS binding in schizophrenia. Life Sci 2006; 78:1231–1237Crossref, Medline, Google Scholar
193 : The muscarinic acetylcholine receptor agonist BuTAC mediates antipsychotic-like effects via the M4 subtype. Neuropsychopharmacology 2013; 38:2717–2726Crossref, Medline, Google Scholar
194 : Expression of M1–M4 muscarinic acetylcholine receptor proteins in rat hippocampus and regulation by cholinergic innervation. J Neurosci 1995; 15:4077–4092Crossref, Medline, Google Scholar
195 : The M3-muscarinic receptor regulates learning and memory in a receptor phosphorylation/arrestin-dependent manner. Proc Natl Acad Sci USA 2010; 107:9440–9445Crossref, Medline, Google Scholar
196 : Acetylcholine prioritises direct synaptic inputs from entorhinal cortex to CA1 by differential modulation of feedforward inhibitory circuits. Nat Commun 2021; 12:5475Crossref, Medline, Google Scholar
197 : Therapeutic potential of beta-arrestin- and G protein-biased agonists. Trends Mol Med 2011; 17:126–139Crossref, Medline, Google Scholar
198 : Expression of muscarinic acetylcholine and dopamine receptor mRNAs in rat basal ganglia. Proc Natl Acad Sci USA 1990; 87:7050–7054Crossref, Medline, Google Scholar
199 : Emerging approaches for treatment of schizophrenia: modulation of cholinergic signaling. Discov Med 2012; 14:413–420Medline, Google Scholar
200 : M5 receptor activation produces opposing physiological outcomes in dopamine neurons depending on the receptor’s location. J Neurosci 2014; 34:3253–3262Crossref, Medline, Google Scholar
201 : Muscarinic regulation of dopamine and glutamate transmission in the nucleus accumbens. Proc Natl Acad Sci USA 2015; 112:8124–8129Crossref, Medline, Google Scholar
202 : Examining the role of muscarinic M5 receptors in VTA cholinergic modulation of depressive-like and anxiety-related behaviors in rats. Neuropharmacology 2020; 171:108089Crossref, Medline, Google Scholar
203 : Loss of M5 muscarinic acetylcholine receptors leads to cerebrovascular and neuronal abnormalities and cognitive deficits in mice. Neurobiol Dis 2006; 24:334–344Crossref, Medline, Google Scholar
204 : Discovery and optimization of potent and CNS penetrant M5-preferring positive allosteric modulators derived from a novel, chiral N-(indanyl)piperidine amide scaffold. ACS Chem Neurosci 2018; 9:1572–1581Crossref, Medline, Google Scholar
205 : Development of the first CNS penetrant M5 positive allosteric modulator (PAM) based on a novel, non-isatin core; in Probe Reports From the NIH Molecular Libraries Program. Bethesda, Md, National Center for Biotechnology Information (US), 2010Google Scholar
206 : Persistent binding and functional antagonism by xanomeline at the muscarinic M5 receptor. J Pharmacol Exp Ther 2005; 315:313–319Crossref, Medline, Google Scholar
207 : Schizophrenia. N Engl J Med 2019; 381:1753–1761Crossref, Medline, Google Scholar
208 : Time course of the antipsychotic effect and the underlying behavioral mechanisms. Neuropsychopharmacology 2007; 32:263–272Crossref, Medline, Google Scholar
209 : Adverse effects of antipsychotic medications. Am Fam Physician 2010; 81:617–622Medline, Google Scholar