Eating Disorders in White and Black Women
Abstract
OBJECTIVE: Epidemiological studies of eating disorders in the United States have focused on white women and girls, and the prevalence of eating disorders in ethnic minority groups is unknown. This study examined the prevalence of anorexia nervosa, bulimia nervosa, and binge eating disorder in a geographically and economically diverse community sample of young white and black women who previously participated in the 10-year National Heart, Lung, and Blood Institute (NHLBI) Growth and Health Study. METHOD: All NHLBI Growth and Health Study participants were recruited for this study. A two-stage case finding method was used, consisting of a telephone screening (sensitivity=0.90, specificity=0.98) and an in-person confirmatory diagnostic interview. RESULTS: A total of 86.0% of the original NHLBI Growth and Health Study cohort participated, including 985 white women (mean age=21.3) and 1,061 black women (mean age=21.5). Fifteen white (1.5%) and no black women met lifetime criteria for anorexia nervosa; more white women (N=23, 2.3%) than black women (N=4, 0.4%) met criteria for bulimia nervosa; binge eating disorder also was more common among white women (N=27, 2.7%) than black women (N=15, 1.4%). Few women (white: N=16, 28.1%; black: N=1, 5.3%) ever had received treatment for an eating disorder. CONCLUSIONS: Results suggest that eating disorders, especially anorexia nervosa and bulimia nervosa, are more common among white women than among black women. The low treatment rates in both groups suggest that health professionals need to be more alert to the possibility of eating disorders in women.
Eating disorders pose a considerable threat to young adult women’s health and adjustment because they are associated with significant psychosocial impairment and adverse health outcomes, such as loss of bone mass, infertility, and high rates of suicide or death, resulting from complications of starvation (1). To date in the United States, epidemiological studies of anorexia nervosa and bulimia nervosa have focused on white women and girls, and information about the prevalence of eating disorders in ethnic minority groups is unknown (2). Several studies have examined rates of behavioral symptoms of eating disorders in ethnic minority populations in which black women have been studied the most. Results suggest that black women are less likely than white women to report dieting and vomiting but equally or more likely to report binge eating (3). The lower rates of dieting and vomiting have been thought to reflect a lower risk for black women of developing anorexia nervosa or bulimia nervosa, disorders in which inappropriate methods of weight control represent core clinical features (DSM-IV). The similar (4, 5) or slightly higher (6) rates of binge eating in white and black women have been thought to reflect comparable risk for developing binge eating disorder, a disorder characterized by recurrent binge eating and the absence of inappropriate weight-control efforts. Most of these studies used self-report questionnaires, a method associated with high false positive identification of eating disorders symptoms, especially binge eating (7–9), or have relied on samples of convenience and provided incomplete information about participation rates, raising concerns about the generalizability of results.
The introduction of binge eating disorder into DSM-IV as a disorder in need of further study has prompted efforts to diversify eating disorders study populations because field studies, unexpectedly, reported comparable rates of binge eating disorder in white and black women (10, 11). Moreover, subsequent studies found a strong association between binge eating disorder and obesity (12). Given the high rates of obesity in ethnic minority populations, experts have hypothesized that binge eating disorder is a significant problem among these groups (3). This study examined the prevalence of eating disorders, including binge eating disorder, in a geographically diverse community sample of young adult white and black women who had participated in a 10-year longitudinal study with an exceptional retention rate (89%) and who were assessed by using a state-of-the-art case-finding method.
Method
Sample
Participants were recruited from a cohort of young women who had taken part in a previous 10-year longitudinal study (involving annual assessments) of risk factors for cardiovascular disease, the National Heart, Lung, and Blood Institute (NHLBI) Growth and Health Study (13). The NHLBI Growth and Health Study recruited 2,379 white and black girls who were 9 or 10 years old at study entry at three clinical centers: the University of California at Berkeley, the University of Cincinnati/Cincinnati Children’s Hospital Medical Center, and Westat, Inc./Group Health near Washington, D.C. The University of California at Berkeley recruited participants from public and parochial schools in the Richmond Unified School District. The area was chosen on the basis of census tract data showing approximately equal percentages of white and black children with the least degree of income disparity between ethnic groups. The University of Cincinnati/Cincinnati Children’s Hospital Medical Center recruited girls from all public and parochial schools in greater Cincinnati in order to have ethnic and socioeconomic representation for Hamilton County (which includes inner-city, urban residential, and suburban areas). The Westat, Inc./Group Health cohort was randomly drawn from a membership listing of families who were enrolled in a large Washington, D.C., area health maintenance organization, and because the membership did not include a sufficient number of white families with age-eligible girls, others were chosen from several local Girl Scout troops in the same geographic area. Eligible participants identified themselves from census categories for race/ethnicity as “black” or “white,” non-Hispanic, and with ethnically concordant parents or guardians. All girls who entered the NHLBI Growth and Health Study assented and their parents consented to their participation.
For this study, all girls who entered the NHLBI Growth and Health Study at baseline were recruited over a period of 3 years, commencing 1 year after the final 10-year NHLBI Growth and Health Study assessment.
Instruments and Procedure
A self-report questionnaire was used to obtain demographic information. Because of the young age of the participants, many were still in the process of obtaining a college education. Therefore, educational attainment was coded as high school diploma or equivalence (no/yes).
To determine the rate of eating disorders, a two-stage assessment protocol was implemented, each requiring informed consent. All participants were interviewed by telephone with the Screening Interview for Eating Disorders (6), which includes questions about health services use in the previous 12 months, current height and weight, behavioral symptom items from the Eating Disorder Examination (14), and screening questions from the Structured Clinical Interview for DSM-IV (SCID) (15). Height and weight had been measured annually by trained female health examiners during the NHLBI Growth and Health Study. To verify history of low weight, this information was retrieved for all participants with anorexia nervosa for the period of time when the participant was presumed to have experienced this illness.
To verify eating disorders and obtain information regarding age of onset and history of treatment for the eating disorders, all women identified in the Screening Interview for Eating Disorders as having experienced current or past symptoms of an eating disorders were recruited for an in-person interview with the complete SCID (15) and the Eating Disorder Examination (14). Also, a random sample of 10% of the remaining participants was interviewed to determine sensitivity and specificity of the Screening Interview for Eating Disorders. All assessments were administered by female interviewers who had attended an initial 3-day training seminar, reached 90% diagnostic agreement, and participated in monthly study-wide conference calls with the first author (R.H.S.-M.) to review interviews and discuss staff questions. With the participants’ written permission, in-person interviews were audiotaped; a master Eating Disorder Examination trainer reviewed the written records for the Screening Interview for Eating Disorders regarding all episodes of overeating and all audiotapes to determine completeness and accuracy of the in-person diagnostic interview. Diagnostic information was summarized by a master trainer on a coding sheet for final review by two clinical psychologists (R.H.S.-M. and F.A.D.) who were blind to the participants’ ethnicity. An eating disorder diagnosis was given only when available information indicated that all required diagnostic criteria were present. The sensitivity of the Screening Interview for Eating Disorders was 0.90, and the specificity was 0.98.
The participants were compensated for their time and transportation expenses. The study protocol was approved by and in compliance with the ethical guidelines of the institutional review boards of all participating institutions.
Statistical Analysis
All analyses were performed by using linear models with site, ethnicity, and the interaction of site by ethnicity as independent variables. For binary outcome measures, chi-square analysis with Breslow-Day tests for homogeneity (16) and Mantel-Haenszel tests for independence (17) were used. The Breslow-Day test (16) assesses the homogeneity of odds ratios for ethnicity across sites, and a significant value indicates a site-by-ethnicity interaction effect. When no significant interaction effect was detected, the main effect for ethnicity across sites was tested with the Mantel-Haenszel test (17). A p=0.05 two-tailed significance level was used. The odds ratio was used as an effect size for binary measures. For survival analysis, Cox proportional hazards analysis (18) was used.
Results
The sample included 2,046 women, representing 86.0% of the initial NHLBI Growth and Health Study cohort (California: 92.4%, N=820; Ohio: 77.5%, N=675; District of Columbia: 88.7%, N=551). Of the 1,166 white girls and 1,213 black girls enrolled in the first year of the NHLBI Growth and Health Study, 985 white women (84.5%) and 1,061 black women (87.5%) consented to participate in the present study. Most of the nonparticipants had been lost to follow-up before this study. Of the women included in NHLBI Growth and Health Study year 10, 98.3% (2,046 of 2,082) participated in the present study. By design, the NHLBI Growth and Health Study had enrolled two specific age cohorts, ages 9 and 10. For budgetary reasons, the present study collected data over 3 years, with participants’ ages ranging from 19 to 24 years. The average age was 21.3 years (SD=0.7) for the white women and 21.5 years (SD=0.7) for the black women.
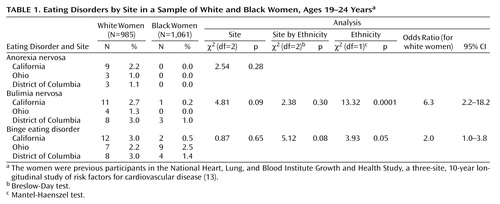
A total of 76 women (57 white, 19 black) met lifetime criteria for at least one eating disorder (Table 1). Of the women with an eating disorder, 15 women (1.5%) met the criteria for anorexia nervosa (all were white), 27 (1.3%) for bulimia nervosa (23 white, 2.3%, four black, 0.4%), and 42 (2.1%) for binge eating disorder (27 white, 2.7%, 15 black, 1.4%). No participant met the criteria for all three disorders; six women met the criteria for anorexia nervosa and bulimia nervosa, and two met the criteria for bulimia nervosa and binge eating disorder (not concurrent).
As previously reported (13), on average the black households had lower family incomes and lower educational levels than the white households. Nevertheless, in each ethnic group, wide ranges of income (less than $10,000 to $75,000 or more) and educational levels (less than a high school diploma to a graduate degree) were represented. White women with an eating disorder did not differ significantly from white women without an eating disorder on parental education (eating disorder: 8.8% had high school or less; 29.8% had some college; 61.4% had a college degree; no eating disorder: 19.1% had high school or less; 31.0% had some college; 49.9% had a college degree) (χ2=4.52, df=2, p=0.11) or family income (eating disorder: 5.4% made less than $10,000; 7.1% made $10,000 to <$20,000; 32.1% made $20,000 to <$40,000; 55.4% made $40,000 or more; no eating disorder: 7.1% made less than $10,000; 9.0% made $10,000 to <$20,000; 31.5% made $20,000 to <$40,000; 52.3% made $40,000 or more) (χ2=0.54, df=3, p=0.91).
Black women with an eating disorder did not differ significantly from black women without an eating disorder on parental education (eating disorder: 36.8% had high school or less; 47.4% had some college; 15.8% had a college degree; no eating disorder: 30.4% had high school or less; 47.5% had some college; 22.2% had a college degree) (χ2=0.60, df=2, p=0.74) or family income (eating disorder: 5.9% made less than $10,000; 41.2% made $10,000 to <$20,000; 29.4% made $20,000 to <$40,000; 23.5% made $40,000 or more; no eating disorder: 27.0% made less than $10,000; 19.7% made $10,000 to <$20,000; 29.7% made $20,000 to <$40,000; 23.6% made $40,000 or more) (χ2=6.67, df=3, p=0.08).
Black women (47.8%, N=507) were significantly more likely than white women (34.2%, N=337) to have ever been obese (χ2=38.82, df=1, p<0.0001, odds ratio=1.8, [confidence interval] CI=1.5–2.1). Black women (28.7%, N=304) were also significantly more likely than white women (12.0%, N=118) to be currently obese (χ2=86.73, df=1, p<0.0001, odds ratio=3.0, CI=2.3–3.7). We further examined the rates of current obesity among white and black women with and without a diagnosis of binge eating disorder. Results were nonsignificant (Mantel-Haenszel χ2=2.76, df=1, p=0.10), but they showed more women who met the criteria for binge eating disorder than those without being classified as currently obese.
The interaction term for ethnicity-by-eating-disorder status was not significant (Breslow-Day χ2=0.01, df=1, p=0.72). Specifically, more white women who ever had binge eating disorder were currently obese (22.2%, 6 of 27) than the white women without a history of binge eating disorder (11.6%, 111 of 958), but this difference only approached statistical significance (χ2=2.80, df=1, p=0.09). The rate of current obesity among black women with binge eating disorder (40%, 6 of 15) was not significantly elevated compared to obesity in black women without binge eating disorder (28.4%, 297 of 1,046) (χ2=0.97, df=1, p=0.32).
Analyses testing for ethnicity, site, and ethnicity-by-site interaction effects were conducted for bulimia nervosa and binge eating disorder; because all participants with anorexia nervosa were white (N=15, 1.5%) and it was self-evident that there was an ethnic difference in the rate of this disorder, only site effects were examined (the odds ratio estimated by assigning a value of 0.5 for black women with anorexia nervosa was 32.8). No significant site differences in the rate of anorexia nervosa were detected. White women (2.3%) were significantly more likely than black women (0.4%) to meet the lifetime criteria for bulimia nervosa (pooled odds ratio=6.3, CI=2.2–18.2); no site differences or site-by-ethnicity interaction effects were detected. White women (2.7%) were more likely than black women (1.4%) to meet the lifetime criteria for binge eating disorder (odds ratio=2.0, CI=1.0–3.8); no significant site or site-by-ethnicity effects were found.
For descriptive purposes, separate survival curves were generated for the white and black women with bulimia nervosa and binge eating disorder and for the white women with anorexia nervosa, as shown in Figure 1. For anorexia nervosa, the average age at onset was 15.4 years (SD=3.4); for bulimia nervosa, it was 16.6 years (SD=2.4) for white women and 17.3 (SD=1.3) for black women; for binge eating disorder, the average age of onset was 16.4 years (SD=2.7) in white women and 17.3 years (SD=2.9) in black women. Of the 76 women who ever had an eating disorder, 16 (28.1%) of the white women and one (5.3%) of the black women reported having received treatment for an eating disorder. When we excluded the 15 white women with anorexia nervosa, the eating disorder with the highest reported rates of treatment (19), 11 (26.2%) of 42 white women reported that they had received treatment.
Discussion
Consistent with epidemiological studies in North America, Europe, and Australia (2), our results suggest that all eating disorders are relatively uncommon and that anorexia nervosa is the least common, while binge eating disorder is the most common of the three eating disorders. The prevalence and ages of onset of anorexia nervosa and bulimia nervosa observed in our sample of white women were well within the ranges reported in other studies of white women in the United States and Canada (20–24). For example, the number of white women with anorexia nervosa and bulimia nervosa observed in this study (15 and 23 of about 1,000 women, respectively) was comparable to the lifetime prevalence rates (1.4% and 2.5%) in a community sample of similar ages recruited in Oregon (22). Research has shown that late adolescence is the period of greatest risk for the onset of anorexia nervosa and bulimia nervosa and that onset after age 21 is rare (20–24). Nevertheless, in our sample of more than 1,000 black women (ages 19–24), no case of anorexia nervosa was detected, and the odds of detecting bulimia nervosa were six-fold greater for white women than for black women. We caution that our results need to be replicated by an independent research team before further conclusions can be drawn about differential risks for these eating disorders.
Previous studies of adult women have reported similar (4) or even higher (5, 6) rates of binge eating in black women than in white women. For example, the Coronary Artery Risk Development in Young Adults study (4) reported that in a representative sample of women ages 18 to 30, 2.0% of white women and 2.2% of black women were identified by a questionnaire method as having binge eating disorder. In this study, significantly fewer black women (1.4%) than white women (2.7%) met the criteria for binge eating disorder, although the odds ratio of 2.0 suggested that this was only a small effect. Compared to anorexia nervosa and bulimia nervosa, the onset of binge eating disorder has been reported to occur later, with onsets observed later than the age of 21 years in a considerable subset of women (25). Our sample was younger than those included in previous studies that examined ethnic differences in rates of binge eating or binge eating disorder. Future studies are needed to address the question of whether with increasing age black women “catch up” with white women in terms of actual rates of binge eating disorder.
Consistent with other studies, we found significant ethnic differences in lifetime and current rates of obesity. Although the rates of current obesity clearly were elevated among white and black women with binge eating disorder compared to women without binge eating disorder, these differences failed to reach statistical significance. Our sample was quite small for examining the association between a diagnosis of binge eating disorder and obesity that had been found in patient samples (1) and in some (4)—but not all—(26) community-based studies of binge eating disorder. Moreover, our sample was relatively young, and the possible adverse effects of binge eating disorder on body weight may become more pronounced with increasing age (27).
Few women reported a history of treatment for their eating disorders, and black women with eating disorders were particularly unlikely to have received treatment. Our results add to a growing literature that documents low treatment rates in general and marked ethnic differences in seeking and receiving treatment for an eating disorder (28, 29). These differences do not appear to be a function of ethnic differences in the symptom severity of eating disorders (25). The reasons for ethnic differences in mental health services use are complex (30). Given that eating disorders are uncommon, it is plausible that health care providers are unfamiliar with eating disorders in ethnic minority groups and are therefore less likely to assess patients for the presence of an eating disorder. Several studies have shown that binge eating disorder is associated with obesity and psychiatric impairment (10–12), regardless of ethnicity (25). Effective treatments have been developed (31), and efforts are needed to increase the identification of and treatment rates for eating disorders.
Several limitations of this study need to be noted. Our study recruited participants who had been involved in a previous study that, by design, included only white and black girls. Consequently, the important question of prevalence of eating disorders in ethnic minority groups such as Asian American, Latina, or Native American women could not be addressed. Because of the small number of participants with eating disorders, we did not test whether the differences in ethnic groups observed in demographic variables contributed to the ethnic group differences in risk for an eating disorder. We noted that within ethnic groups, neither parental education nor family income was significantly associated with eating disorder status. The role of socioeconomic variables as possible risk factors for the development of an eating disorder is a matter of considerable debate (32), and conclusive answers have been elusive because of the challenges involved in establishing community-based samples with adequate power.
Several strengths of the study also need to be acknowledged. We included a geographically and socioeconomically diverse sample of black and white women and achieved excellent participation over a long time period. Two major sources of potential bias regarding ethnic group differences in eating disorders can likely be ruled out. One, the uniformly high participation rate suggests that the present study did not favor differential detection of an eating disorder in either group. Two, diagnoses were based on operationalized criteria and measured with reliable interviews that were administered by highly trained staff.
Results of this epidemiological study suggest that, among young adults, black women are less likely than white women to have experienced an eating disorder. These differences were more pronounced for anorexia nervosa and bulimia nervosa than for binge eating disorder. Reported rates of treatment were low in both groups, but black women were particularly unlikely to have received treatment specifically for an eating disorder. Health professionals need to be alert to the possibility of eating disorders in adolescent girls, and research is needed to identify barriers to accessing treatment. Given the association of obesity and binge eating disorder, screening for binge eating disorder in white and black girls and women could lead to timely identification and prevention of the development of obesity.
 |
Received May 6, 2002; revision received Nov. 15, 2002; accepted Nov. 26, 2002. From the Department of Psychology, Wesleyan University; the Graduate School of Education and Allied Professions, Fairfield University, Fairfield, Conn.; the Department of Psychiatry, Stanford University School of Medicine, Stanford, Calif.; the Department for Cardiology, Cincinnati Children’s Hospital, Cincinnati; the School of Public Health, University of California at Berkeley, Berkeley, Calif.; and Westat, Inc., Rockville, Md. Address reprint requests to Dr. Striegel-Moore, Department of Psychology, Wesleyan University, 207 High St., Middletown, CT 06459; [email protected] (e-mail). Supported by a grant (MH-52348) funded jointly by NIMH and the National Institute of Diabetes and Digestive and Kidney Diseases. The authors thank the participants in the National Heart, Lung, and Blood Institute (NHLBI) Growth and Health Study for their cooperation during the NHLBI Growth and Health Study and the present study, the NHLBI Growth and Health Study Steering Committee for the design, execution, and cohort retention of the NHLBI Growth and Health Study (Bruce A. Barton, Ph.D., Frank M. Biro, M.D., Frank Falkner, M.D., Sue Y.S. Kimm, M.D., Robert P. McMahon, Ph.D., John A. Morrison, Ph.D., Eva Obarzanek, Ph.D., R.D., Gerald Payne, M.D., Dennis L. Sprecher, M.D., and Zak Zabry, Ph.D.), and Miriam Gibbon, M.S.W., and Michael First, M.D., for providing staff training in the administration of the Structured Clinical Interview for DSM-IV diagnoses.
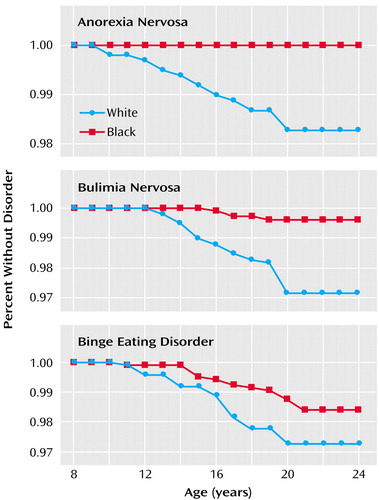
Figure 1. Survival Curves Showing Time to Onset of Anorexia Nervosa, Bulimia Nervosa, and Binge Eating Disorder for 2,046 White and Black Women, Ages 19–24 Years, Who Ever Met the DSM-IV Criteria for Each Eating Disordera
aNo black women in the sample ever met the criteria for anorexia nervosa.
1. Agras WS: The consequences and costs of the eating disorders. Psychiatr Clin North Am 2001; 24:371-379Crossref, Medline, Google Scholar
2. Nielsen S: Epidemiology and mortality of eating disorders. Psychiatr Clin North Am 2001; 24:201-214Crossref, Medline, Google Scholar
3. Striegel-Moore RH, Smolak L: The influence of ethnicity on eating disorders in women, in Handbook of Gender, Culture, and Health. Edited by Eisler RM, Hersen M. Mahwah, NJ, Lawrence Erlbaum Associates, 2000, pp 227-254Google Scholar
4. Smith DE, Marcus MD, Lewis CE, Fitzgibbon M, Schreiner P: Prevalence of binge eating disorder, obesity, and depression in a biracial cohort of young adults. Ann Behav Med 1998; 20:227-232Crossref, Medline, Google Scholar
5. Pemberton AR, Vernon SW, Lee ES: Prevalence and correlates of bulimia nervosa and bulimic behaviors in a racially diverse sample of undergraduate students in two universities in southeast Texas. Am J Epidemiol 1996; 144:450-455Crossref, Medline, Google Scholar
6. Striegel-Moore RH, Wilfley DE, Pike KM, Dohm FA, Fairburn CG: Recurrent binge eating in black American women. Arch Fam Med 2000; 9:83-87Crossref, Medline, Google Scholar
7. Carter JC, Aime AA, Mills JS: Assessment of bulimia nervosa: a comparison of interview and self-report questionnaire methods. Int J Eat Disord 2001; 30:187-192Crossref, Medline, Google Scholar
8. Grilo CM, Masheb RM, Wilson GT: Different methods for assessing the features of eating disorders in patients with binge eating disorder: a replication. Obes Res 2001; 9:418-422Crossref, Medline, Google Scholar
9. Wilfley DE, Schwartz MB, Spurell EB, Fairburn CG: Assessing the specific psychopathology of binge eating disorder patients: interview or self-report? Behav Res Ther 1997; 35:1151-1159Crossref, Medline, Google Scholar
10. Spitzer RL, Devlin M, Walsh BT, Hasin D, Wing R, Marcus M, Stunkard A, Wadden T, Yanovski S, Agras S, Mitchell J, Nonas C: Binge eating disorder: a multisite field trail of the diagnostic criteria. Int J Eat Disord 1992; 11:191-204Crossref, Google Scholar
11. Spitzer RL, Yanovski SZ, Wadden T, Wing R, Marcus M, Stunkard A, Devlin M, Mitchell J, Hasin D, Horne R: Binge eating disorder: its further validation in a multisite study. Int J Eat Disord 1993; 13:137-153Crossref, Medline, Google Scholar
12. de Zwaan M: Binge eating disorder and obesity. Int J Obes Relat Metab Disord Suppl 2001; 1:S51-S55Google Scholar
13. National Heart, Lung, and Blood Institute Growth and Health Study Research Group: Obesity and cardiovascular disease risk factors in black and white girls: the NHLBI Growth and Health Study. Am J Public Health 1992; 82:1613-1621Crossref, Medline, Google Scholar
14. Fairburn CG, Cooper Z: The Eating Disorder Examination, 12th ed, in Binge Eating: Nature, Assessment and Treatment. Edited by Fairburn CG, Wilson GT. New York, Guilford, 1993, pp 317-360Google Scholar
15. First MB, Spitzer RL, Gibbon M, Williams JB: Structured Clinical Interview for DSM-IV Axis I Disorders—Non-Patient Edition (SCID-I/NP), version 2.0. New York, New York State Psychiatric Institute, Biometrics Research, 1996Google Scholar
16. Breslow NE, Day NE: Statistical Methods in Cancer Research, vol II: The Design and Analysis of Cohort Studies. Lyon, France, International Agency for Research on Cancer, 1987Google Scholar
17. Mantel N, Haenszel W: Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst 1959; 22:719-748Medline, Google Scholar
18. Cox DR: Regression models and life tables. J R Stat Soc 1972; 34:187-202Google Scholar
19. Striegel-Moore RH, Leslie D, Petrill SA, Garvin V, Rosenheck RA: One-year use and cost of inpatient and outpatient services among female and male patients with an eating disorder: evidence from a national database of health insurance claims. Int J Eat Disord 2000; 27:301-389Google Scholar
20. Garfinkel PE, Lin E, Goering P, Spegg C, Goldbloom D, Kennedy S, Kaplan AS, Woodside DB: Should amenorrhea be necessary for the diagnosis of anorexia nervosa? Br J Psychiatry 1996; 168:500-506Crossref, Medline, Google Scholar
21. Garfinkel PE, Lin E, Goering P, Spegg C, Goldbloom DS, Kennedy S, Kaplan AS, Woodside DB: Bulimia nervosa in a Canadian community sample: prevalence and comparison of subgroups. Am J Psychiatry 1995; 152:1052-1058Link, Google Scholar
22. Lewinsohn PM, Striegel-Moore RH, Seeley JP: The epidemiology and natural course of eating disorders in young women from adolescence to young adulthood. J Am Acad Child Adolesc Psychiatry 2000; 39:1284-1292Crossref, Medline, Google Scholar
23. Walters EE, Kendler KS: Anorexia nervosa and anorexic-like syndromes in a population-based female twin sample. Am J Psychiatry 1995; 152:64-71Link, Google Scholar
24. Kendler KS, MacLean C, Neale M, Kessler R, Heath A, Eaves L: The genetic epidemiology of bulimia nervosa. Am J Psychiatry 1991; 148:1627-1637Link, Google Scholar
25. Pike KM, Dohm FA, Striegel-Moore RH, Wilfley DE, Fairburn CG: A comparison of black and white women with binge eating disorder. Am J Psychiatry 2001; 158:1455-1460Link, Google Scholar
26. Hay P: The epidemiology of eating disorder behavior. Int J Eat Disord 1998; 23:371-382Crossref, Medline, Google Scholar
27. Fairburn CG, Cooper Z, Doll HA, Norman P, O’Connor M: The natural course of bulimia nervosa and binge eating disorder in young women. Arch Gen Psychiatry 2000; 57:659-665Crossref, Medline, Google Scholar
28. Cachelin FM, Rebeck R, Veisel C, Striegel-Moore RH: Treatment seeking for eating disorders among ethnically diverse women. Int J Eat Disord 2001; 30:269-278Crossref, Medline, Google Scholar
29. Wilfley DE, Pike KM, Dohm FA, Striegel-Moore RH, Fairburn CG: Bias in binge eating disorder: how representative are recruited clinic samples? J Consult Clin Psychol 2001; 69:383-388Crossref, Medline, Google Scholar
30. Kessler RC, Zhao S, Katz SJ, Kouzis AC, Frank RG, Edlund M, Leaf P: Past-year use of outpatient services for psychiatric problems in the National Comorbidity Survey. Am J Psychiatry 1999; 156:115-123Link, Google Scholar
31. Whittal ML, Agras WS, Gould RA: Bulimia nervosa: a meta-analysis of psychosocial and pharmacological treatments. Behav Ther 1999; 30:117-135Crossref, Google Scholar
32. McClelland L, Crisp A: Anorexia nervosa and social class. Int J Eat Disord 2001; 29:150-156Crossref, Medline, Google Scholar



