A Comparison of Black and White Women With Binge Eating Disorder
Abstract
OBJECTIVE: Binge eating disorder was introduced in DSM-IV as a psychiatric disorder needing further study. This community-based study describes the relationship between race and clinical functioning in black and white women with and without binge eating disorder. METHOD: A group of 150 women with binge eating disorder (52 black, 98 white) and a race-matched group of 150 healthy comparison subjects were recruited from the community. Eating and psychiatric symptoms were assessed through interviews and self-report. RESULTS: Black and white women with binge eating disorder differed significantly on numerous eating disorder features, including binge frequency, restraint, history of other eating disorders, treatment-seeking behavior, and concerns with eating, weight, and shape. Black and white healthy comparison subjects differed significantly in obesity rates. CONCLUSIONS: For both black and white women, binge eating disorder was associated with significant impairment in clinical functioning. Yet, racial differences in clinical presentation underscore the importance of considering race in psychopathology research.
In DSM-IV, binge eating disorder was introduced as a psychiatric disorder needing further study. The mission of the present study was twofold: to describe the clinical functioning of a community cohort of women with binge eating disorder and to examine the relationship between race and clinical functioning among women with binge eating disorder. To this end, this investigation provides, to our knowledge, the first interview assessment of a community cohort of black and white American women with binge eating disorder.
The clinical literature notes high rates of psychiatric comorbidity and elevated rates of obesity associated with binge eating disorder (1–3). In contrast, data from a previous community-based study (4) found lower rates of psychiatric comorbidity associated with binge eating disorder compared to findings from clinical studies. However, that study did not directly compare community and clinical studies and did not address the role of race in the presentation of binge eating disorder. By directly comparing a community cohort of black and white women with binge eating disorder and a race-matched group of healthy comparison subjects, this study enhances our understanding of binge eating disorder and the role of race in the presentation of binge eating disorder in several important ways. First, until recently, it was widely believed that eating disorders afflicted only individuals who were white, female, and affluent; the well-established literature on the sociocultural influences associated with etiology of eating disorders explains theoretically the limited racial diversity among individuals with eating disorders (5, 6). However, because binge eating disorder appears more common among diverse ethnic groups, we must revisit some of these assumptions. Second, because most of the existing data on binge eating disorder derive from individuals in treatment, a community study will broaden our understanding of the implications of binge eating disorder for a wider spectrum of individuals.
Consistent with current population demographics, it was hypothesized that black women would have higher body mass indexes than white women, regardless of case status (7). Regarding specific eating pathology, it was hypothesized that black women would report lower rates of weight and shape concerns, regardless of case status, given the greater acceptance of higher weight among black women (8). By extension, it was hypothesized that black women with binge eating disorder would be comparable to white women with binge eating disorder in terms of the defining behavioral disturbances but report less weight and shape dissatisfaction.
This study used data collected as part of the New England Women’s Health Project, a community-based study of the risk factors for binge eating disorder (9).
Method
Subjects
The participants included 150 women whose primary diagnosis was binge eating disorder (98 white, 52 black) and a matched group of 150 healthy comparison subjects. The first group met DSM-IV criteria for current binge eating disorder, operationalized as follows: minimum average frequency of binge eating episodes of twice a week for 6 consecutive months, distress over binge eating, presence of three behavioral indicators of loss of control over binge eating, and absence of regular extreme compensatory behaviors. Extreme compensatory behaviors included vomiting; use of laxatives, diuretics, or other drugs for weight control; fasting (eating nothing for 24 hours or more); and excessive exercise (exercising despite pain, against a physician’s advice, or so much that it interferes with responsibilities). Women who reported engaging in extreme compensatory behaviors once a month or more often were excluded from the binge eating disorder group. For this study, binge eating disorder was considered the primary condition for individuals in this group even when comorbid psychiatric conditions were present.
The matched group of healthy comparison subjects were women who did not meet current axis I criteria for any psychiatric disorder and who did not have a history of binge eating or compensatory behaviors once a month or more often or a history of extreme dieting for weight control for 3 or more consecutive months. Comparison subjects were individually matched to patients by race, age, and education.
Recruitment and Procedure
Participants were recruited as part of the New England Women’s Health Project, a community-based study of risk factors for binge eating disorder with project offices in Middletown, Conn., Boston, New York, and Los Angeles. Recruitment began in January 1995 and ended in December 1999. Eligibility criteria for the New England Women’s Health Project included being female, white or black, born in the United States, 18 to 40 years of age, and within driving distance of a project office.
The New England Women’s Health Project used two recruitment strategies. Approximately 10,000 potential participants were contacted through a consumer information database. Individuals were also recruited through posters, newspaper ads, and radio and television announcements for participation in a study of women’s health. There were no racial differences in percentages of women recruited through the consumer information database (white women: 52.0% [N=102 of 196]; black women: 51.9% [N=54 of 104]) or through the advertising campaign (white women: 48.0% [N=94]; black women: 48.1% [N=50]). Most of the women with binge eating disorder were recruited through the advertising campaign (76.7%, N=115), whereas most healthy comparison subjects were recruited from the consumer information database (80.7%, N=121).
Staff phoned all potential participants and determined eligibility for the study by using a 15-minute screening interview developed for the New England Women’s Health Project. Exclusion criteria were age over 40 or under 18 years, physical conditions known to influence eating habits or weight, current pregnancy, presence of psychotic disorder, not being white or black, or not being born in the United States. Women who remained eligible after the telephone screening interview were then interviewed in person and completed several self-report questionnaires. Participants were ensured confidentiality of their responses and were paid for their time. Height and weight were measured and recorded at the end of this interview session. Only instruments used in the present report are described here. This study was reviewed and approved by the institutional review boards at Wesleyan University and Columbia University. Informed consent was obtained in two separate steps. For the telephone screening interview, after a complete description of the study, verbal informed consent was obtained from all participants. For the full interview, after a complete description of the study, written informed consent was obtained from all participants.
Clinical Information
During the telephone screening interview, participants provided their race, age, and educational attainment. In data analyses, three educational levels were used: high school or less, some college, and college graduate or more. The question about race was asked toward the end of the screening call to reduce the possibility of interviewer bias in ascertaining potential cases of binge eating disorder. Hispanic women were excluded from this study because there were insufficient resources to recruit an adequate sample to study Hispanic women as a distinct group.
The Structured Clinical Interview for DSM-IV Axis I Disorders (SCID) (10) was used to determine current and lifetime psychiatric status. The reliability and validity of the SCID have been well documented (11). Staff participated in an initial 60-hour training workshop. Training was continued until individual supervision found 100% agreement between staff ratings and master trainer ratings of three consecutive SCID interviews. Staff participated in ongoing monthly supervision meetings and annual 2-day refresher workshops to avoid interviewer drift.
Participants who met SCID criteria for an eating disorder were interviewed further with the Eating Disorder Examination (12). The Eating Disorder Examination is a semistructured, investigator-based interview that generates operational eating disorder diagnoses based on DSM-IV criteria. The reliability and validity of this interview are well established (12). The section that assesses history of binge eating was modified so that the Eating Disorder Examination could be used to confirm eating disorder diagnoses (current and lifetime) and to identify the onset age for eating disorder symptoms and syndromes. Onset age for an eating disorder was defined as the age at which the participant first met all diagnostic criteria. Questions also were added to the Eating Disorder Examination to assess history of treatment for an eating or weight problem. Staff participated in a 40-hour initial training workshop and continued training individually until the master trainer was in 100% agreement with the staff regarding the ratings of three consecutive Eating Disorder Examination interviews. Staff reviewed Eating Disorder Examination tapes in weekly supervision meetings and participated in annual 2-day refresher workshops.
For a continuous assessment of eating disorder symptoms, the Eating Disorder Examination Questionnaire (13) was used. Derived from the Eating Disorder Examination, this self-report questionnaire focuses on the past 28 days and assesses shape concerns, weight concerns, eating concerns, and dietary restraint. The Eating Disorder Examination Questionnaire has documented reliability and validity (13–15).
The Brief Symptom Inventory (16) is a 53-item instrument that indicates the degree to which an individual has been troubled by specific symptoms during the past 7 days. Items are rated on a 5-point scale ranging from 0 (not at all) to 4 (extremely). A Global Severity Index score is calculated by summing across items.
Height (in meters) and weight (in kilograms) were used to calculate body mass index (kg/m2). Obesity was defined as body mass index of 30 or higher (17).
Results
Women with binge eating disorder and comparison subjects did not differ significantly in education (χ2=0.44, df=2, p=0.81) or age (F=0.97, df=1, 298, p=0.33). White and black women did not differ in age (F=0.02, df=1, 298, p=0.89) but differed somewhat in education (χ2=6.18, df=2, p<0.05).Slightly more white women than black women reported having completed college (Table 1).
In all, 67 cases of bulimia nervosa (53 purging subtype and 14 nonpurging subtype) and 70 cases of eating disorder not otherwise specified (53 of which were subthreshold binge eating disorder and 10 of which were subthreshold bulimia nervosa) were identified. No current cases of anorexia nervosa were confirmed, since women who reported a body mass index of less than 18 achieved by their intentional efforts were excluded from the study during the screening phase. A comparison of individuals with bulimia nervosa and binge eating disorder has been published elsewhere (18); however, because the bulimia nervosa group was not of sufficient size to conduct racial comparisons, it was not included in this report.
Severity of Weight Problems and Eating Pathology Associated With Binge Eating Disorder
Body weight
Women with binge eating disorder were significantly heavier (mean body mass index=34.17 kg/m2, SD=9.24) than comparison subjects (mean body mass index=25.81 kg/m2, SD=7.05) (F=69.69, df=1, 296, p<0.0001). As seen in Table 1, black women were significantly heavier than white women (Table 1). The race-by-group interaction effect was not significant (F=0.74, df=1, 298, p=0.39).
Obesity
Women with binge eating disorder were significantly more likely to be obese (65.3%, N=98) than healthy comparison women (20.7%, N=31) (χ2=61.05, df=1, p<0.0001). Obesity also was significantly more common among black women (58.7%, N=61) than white women (34.7%, N=68) (χ2=15.92, df=1, p<0.0001). This significant difference in obesity rates between black and white women held true for the binge eating disorder group (black obese: 82.7% [N=43], white obese: 56.1% [N=55]) (χ2=10.59, df=1, p<0.001; odds ratio=3.74, 95% confidence interval [CI]=1.64–8.50) and for healthy comparison subjects (black obese: 34.6% [N=18], white obese: 13.3% [N=13]) (χ2=9.45, df=1, p<0.002; odds ratio=3.46, 95% CI=1.53–7.83).
Eating disorder symptoms
Multivariate analysis of variance comparing the groups on the subscale scores of the Eating Disorder Examination Questionnaire revealed significant main effects for group status (binge eating disorder versus comparison group: omnibus F=128.61, df=4, 271, p<0.0001) and race (omnibus F=7.48, df=4, 271, p<0.0001) and a significant group-by-race interaction effect (omnibus F=4.27, df=4, 271, p<0.002). As shown in Figure 1, the significant interaction between race and case status indicated that, among women with binge eating disorder, black women had significantly lower scores than white women on eating concern (ε2=0.029), dietary restraint (ε2=0.033), shape concern (ε2=0.025), and weight concern (ε2=0.041). (In analysis of variance, ε2 represents the effect size [19].) Among healthy comparison subjects, no racial differences were found on the Eating Disorder Examination Questionnaire subscale scores.
Race and the Clinical Presentation of Binge Eating Disorder
All women with binge eating disorder met the diagnostic criterion of binge eating a minimum of two times per week for the past 6 months. A more in-depth examination of the number of binge eating episodes experienced over the past 3 months showed that white and black women differed significantly in mean number of binge episodes per week (Table 1).
History of eating disorders
Black and white women with binge eating disorder did not differ in the age they first met criteria for an eating disorder (F=2.78, df=1, 148, p=0.10). None of the black women and only one white woman met criteria for a history of anorexia nervosa (restricting type) (χ2=0.53, df=1, p=1.00). However, as seen in Table 1, white women were more than eight times more likely than black women (relative risk ratio=8.6) to meet criteria for a history of bulimia nervosa (odds ratio=6.52, 95% CI=0.96–44.18).
Treatment for a weight or eating problem
Black women with binge eating disorder were as likely as white binge eating disorder women to have been treated for a weight problem (28.8% [N=15] and 30.6% [N=30], respectively; χ2=0.05, df=1, p=0.86). However, black women with binge eating disorder were significantly less likely than white binge eating disorder women to have been treated for an eating problem (7.7% [N=4] versus 22.4% [N=22]; χ2=5.16, df=1, p<0.03) (odds ratio=2.52, 95% CI=0.99–6.34; relative risk ratio=2.9).
Given the discrepancy between receiving treatment for eating and weight disorders, we conducted an unplanned, post hoc test of the hypothesis that the higher rate of receiving treatment for an eating problem reported by the white women was related to their more likely history of bulimia nervosa. Of the 22 white women who had received treatment for an eating problem, nine had a history of bulimia nervosa; none of the four black women who had received such treatment had a history of bulimia nervosa. When the women who had a history of bulimia nervosa were dropped from the analysis, the rates of receiving treatment for an eating problem for black (N=4) and white (N=13) women were no longer significantly different (χ2=1.81, df=1, p=0.18). However, the odds ratio of 1.72 (95% CI=0.71–4.17) indicates that white women still were more likely than black women to report having received treatment for an eating problem. Thus, the failure to obtain significance in this result could be an artifact of the small group size.
Psychiatric distress and comorbidity
White women with binge eating disorder reported significantly higher levels of psychiatric distress on the Brief Symptom Inventory than black women with binge eating disorder (mean=1.04 [SD=0.70] versus 0.72 [SD=0.57], respectively; F=6.57, df=1, 129, p<0.02; ε2=0.05). White and black women with binge eating disorder were equally likely to have at least one current axis I disorder (43.9% [N=43] and 42.3% [N=22]; χ2=0.03, df=1, p=0.86). However, white women with binge eating disorder were more than twice as likely as black binge eating disorder women (relative risk ratio=2.8) to meet criteria for multiple current axis I disorders (21.4% [N=21] versus 7.7% [N=4]; χ2=4.62, df=1, p<0.04) (odds ratio=2.40, 95% CI=0.95–6.05). As indicated in Table 1, two of the four most common current comorbid diagnoses were consistent across race: major depressive disorder and social phobia. Panic disorder was more common among white women with binge eating disorder, and dysthymic disorder was more common among black binge eating disorder women.
White and black women with binge eating disorder were equally likely to have met criteria for at least one comorbid axis I disorder during their lifetime (81.6% [N=80] and 80.8% [N=42], respectively; χ2=0.02, df=1, p<0.90). Similarly, white and black women with binge eating disorder were equally likely to have met criteria for multiple comorbid axis I disorders during their lifetime (67.3% [N=66] and 57.7% [N=30]; χ2=1.37, df=1, p=0.24). However, significantly more white women than black women with binge eating disorder reported a lifetime history of alcohol abuse or dependence (40.8% [N=40] versus 23.1% [N=12]; χ2=4.72, df=1, p<0.03) and drug abuse or dependence (41.8% [N=41] versus 21.2% [N=11]; χ2=6.42, df=1, p<0.02).
Discussion
The results from this study offer a broad picture of clinical functioning related to binge eating disorder among white and black American women in the community. The findings are provocative in that the black and white women with binge eating disorder differed significantly on all associated eating disorder features, including binge frequency, restraint, and concern with eating, weight, and shape. They also differed significantly in terms of history of other eating disorders and seeking treatment for their eating disturbances. These differences occurred despite the fact that all these women met DSM-IV criteria for binge eating disorder according to structured clinical interviews that were further confirmed by the Eating Disorder Examination.
Even though their Eating Disorder Examination Questionnaire scores fell within pathological ranges and were significantly greater than those of matched healthy comparison subjects, black women with binge eating disorder reported less concern about body weight, shape, and eating than white women with binge eating disorder. Coupled with higher weight and more frequent binge eating, the clinical binge eating disorder picture for black women is quite different from that of white women. It is of note that the Eating Disorder Examination Questionnaire scales did not differentiate between black and white healthy comparison subjects, suggesting that racial differences emerge only at the pathological end of the spectrum of weight, shape, and eating concerns. Given that black culture tends to be more accepting of larger body shapes and less preoccupied with dietary restraint (6), it appears that black women may be less likely to experience or acknowledge the same degree of attitudinal concern despite significant behavioral symptoms.
The positive relationship of binge eating disorder to body weight and obesity is consistent with results of other studies and underscores the adverse health implications of binge eating disorder. Our results agree with other studies that have documented that black women are heavier than white women whether or not they have an eating disorder (7). Black and white women with binge eating disorder were equally likely to report having received treatment for a weight problem, but significantly fewer black women with binge eating disorder reported having received treatment for an eating problem. Given the role that binge eating disorder may play in contributing to or maintaining obesity, the fact that black women may be less likely to receive treatment for binge eating disorder presents a significant public health concern.
In our study, only a subset of the women with binge eating disorder reported a history of bulimia nervosa, and such a history was significantly more common in white women. The hallmark feature distinguishing bulimia nervosa and binge eating disorder is inappropriate compensatory behavior subsequent to binge eating. These data are compatible with the idea that black women are as much at risk as white women for developing binge eating disorder but, because of cultural differences in concerns about weight and shape, are at less risk than white women for developing bulimia nervosa.
The significant rates of comorbidity associated with binge eating disorder for both black and white women in the community are consistent with clinic data that have suggested that binge eating disorder is a syndrome often linked to affective and anxiety disorders. Black and white women with binge eating disorder reported comparable rates of one current comorbid axis I diagnosis; however, white women were significantly more likely to meet criteria for multiple current axis I disorders and to report higher levels of subjective distress. More research is needed to reconcile the difference in current and lifetime comorbidity. The finding of greater lifetime alcohol and substance abuse among white women than in black women replicates that of larger studies (20).
The findings from this study have important implications for treatment providers across a range of specialties. Given the apparent relationship between obesity and binge eating disorder (1), screening for binge eating disorder in obese patients may be indicated. Additionally, although black and white women with binge eating disorder may be equally likely to seek treatment for weight problems, black women in our study were less likely to receive treatment for their eating disorder. This parallels data that indicate, across the entire range of psychiatric disturbances, that the likelihood of receiving mental health care is low for racial minority groups (18, 21). This low usage of treatment may reflect a cultural bias within the black community regarding mental health care, or there may be other barriers to securing such care. Future studies examining the influence of race on treatment seeking and health care delivery are warranted.
To our knowledge this is the first community-based interview study to assess a cohort of black women with binge eating disorder. It illuminates significant ways in which race plays a role in the clinical presentation of binge eating disorder. One limitation is that, because of the relatively low base rate of the disorder in the population, we were not able to find equal numbers of black and white women with binge eating disorder. These low base rates are a challenge for any community-based study of eating disorders and make investigations of racial differences particularly difficult given the lower proportion of minorities in the broader population. Given these sampling limitations, conclusions drawn from this study should be viewed as tentative until further replication.
The two recruitment strategies revealed important information for future community studies of eating disorders. More cases of binge eating disorder were self-identified through direct recruitment strategies (e.g., advertising campaign) than through the national consumer information database. This likely is a function of the low base rate of binge eating disorder, but it may also reflect some resistance to participating in phone survey research. Women with binge eating disorder may have denied their symptoms or refused to participate in the study when contact was initiated through the consumer database list.
Other interesting issues to explore further are the relationship between race, degree of acculturation, socioeconomic status, and eating disorders. Within a racial minority group, vulnerability to developing an eating disorder may, in part, be a function of socioeconomic status and degree of acculturation. Given the extreme idealization of thinness within white culture, higher socioeconomic status and greater assimilation into white culture in the United States may render black women more vulnerable to developing certain eating and weight disorders (8). However, drive for thinness may be less central to the etiology of binge eating disorder, and, therefore, socioeconomic status and cultural assimilation as they correlate with binge eating disorder will be important to explore in future studies.
The differences between black and white women with binge eating disorder suggest that distinct racial/ethnic influences need to be considered in studying eating disorder psychopathology. For example, the disturbance pattern for Hispanic women, although generally similar to that of white women, differs in some ways (e.g., increased diuretic use [22]). Future studies elucidating additional racial/ethnic contributions to the presentation of eating disorders are warranted.
A particular strength of this study is the fact that, to date, it is the largest community interviewer-based investigation of binge eating disorder in North America. Another strength is that we included a healthy comparison group matched by race, age, and education. The comparison allowed us to show that despite racial variation in severity of eating symptoms, both black and white women with binge eating disorder could be differentiated from the healthy comparison subjects. Our data support the notion that binge eating disorder is a clinically significant syndrome in both black and white women. The racial differences in this study suggest the need for research aimed at further elucidating the impact of race on clinical course, health care utilization, and treatment response.
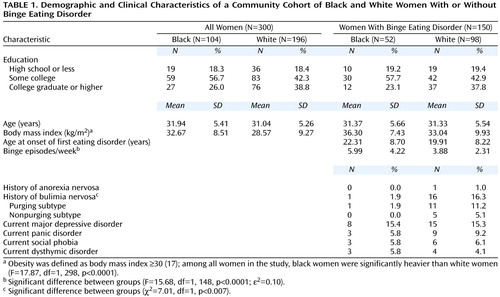 |
Received Oct. 15, 1999; revisions received Oct. 12, 2000, and Jan. 31, 2001; accepted Feb. 21, 2001. From the New England Women’s Health Project. Address reprint requests to Dr. Striegel-Moore, Department of Psychology, Wesleyan University, 207 High St., Middletown, CT 06459; [email protected] (e-mail). Supported by NIMH grant MH-52348 and a supplemental grant from the NIH Office for Research on Women’s Health (Dr. Striegel-Moore) and a Principal Fellowship from the Wellcome Trust (Dr. Fairburn).
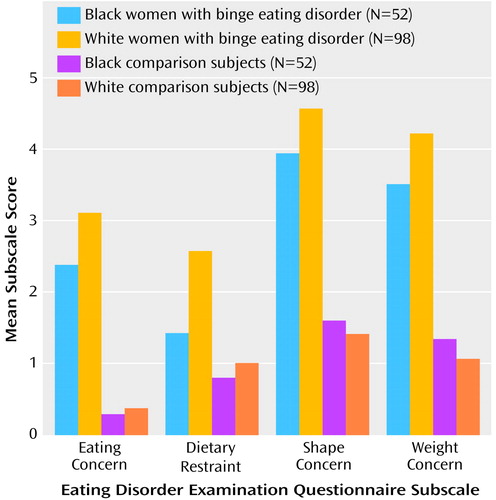
Figure 1. Scores on Subscales of the Eating Disorder Examination Questionnaire of a Community Cohort of Black and White Women With or Without Binge Eating Disordera
aAmong the women with binge eating disorder, black women had significantly lower scores than white women on each of the four questionnaire subscales (eating concern: F=8.11, df=1, 274, p<0.005; dietary restraint: F=9.21, df=1, 274, p<0.003; shape concern: F=7.07, df=1, 274, p<0.008; and weight concern: F=11.71, df=1, 274, p<0.001).
1. Spitzer RL, Devlin M, Walsh BT, Hasin D, Wing R, Marcus M, Stunkard A, Wadden T, Yanovski S, Agras S, Mitchell J, Nonas C: Binge eating disorder: a multisite field trail of the diagnostic criteria. Int J Eat Disord 1992; 11:191-204Crossref, Google Scholar
2. Telch CF, Agras WS: Obesity, binge eating and psychopathology: are they related? Int J Eat Disord 1994; 15:53-61Crossref, Medline, Google Scholar
3. Yanovski SZ, Nelson JE, Dubbert BK, Spitzer RL: Association of binge eating disorder and psychiatric comorbidity in obese subjects. Am J Psychiatry 1993; 150:1472-1479; correction, 150:1910Google Scholar
4. Telch CF, Stice E: Psychiatric comorbidity in women with binge eating disorder: prevalence rates from a non-treatment-seeking sample. J Consult Clin Psychol 1998; 66:768-776Crossref, Medline, Google Scholar
5. Pike KM, Walsh BT: Ethnicity and eating disorders: implications for incidence and treatment. Psychopharmacol Bull 1996; 32:265-273Medline, Google Scholar
6. Striegel-Moore RH, Smolak L: The influence of ethnicity on eating disorders in women, in Handbook of Gender, Culture, and Health. Edited by Eisler RM, Hersen M. Mahwah, NJ, Lawrence Erlbaum Associates, 2000, pp 227-254Google Scholar
7. Kuczmarski RJ, Flegal KM, Campbell SM, Johnson CL: Increasing prevalence of overweight among adults: the National Health and Nutrition Examination Surveys, 1960-1991. JAMA 1994; 272:205-211Crossref, Medline, Google Scholar
8. Wilfley DE, Schreiber GB, Pike KM, Striegel-Moore RH: Eating disturbance and body image: a comparison of a community sample of adult black and white women. Int J Eat Disord 1996; 20:377-387Crossref, Medline, Google Scholar
9. Striegel-Moore RH, Wilfley DE, Pike KM, Dohm FA, Fairburn CG: Recurrent binge eating in black American women. Arch Fam Med 2000; 9:83-87Crossref, Medline, Google Scholar
10. First MB, Spitzer RL, Gibbon M, Williams JBW: Structured Clinical Interview for DSM-IV Axis I Disorders (SCID). New York, New York State Psychiatric Institute, Biometrics Research, 1995Google Scholar
11. Segal DL, Hersen M, Van Hasselt VB: Reliability of the structured clinical interview for DSM-III-R: an evaluative review. Compr Psychiatry 1994; 35:316-327Crossref, Medline, Google Scholar
12. Fairburn CG, Cooper Z: The Eating Disorder Examination, 12th ed, in Binge Eating: Nature, Assessment and Treatment. Edited by Fairburn CG, Wilson GT. New York, Guilford Press, 1993, pp 317-360Google Scholar
13. Fairburn CG, Beglin SJ: Assessment of eating disorder pathology: interview or self-report questionnaire. Int J Eat Disord 1994; 16:363-370Medline, Google Scholar
14. Black CMD, Wilson GT: Assessment of eating disorders: interview versus questionnaire. Int J Eat Disord 1996; 20:43-50Crossref, Medline, Google Scholar
15. Wilfley DE, Schwartz MB, Spurell EB, Fairburn CG: Assessing the specific psychopathology of binge eating disorder patients: interview or self-report? Behav Res Ther 1997; 35:1151-1159Google Scholar
16. Derogatis LR: Brief Symptom Inventory. Baltimore, Clinical Psychometric Research, 1975Google Scholar
17. NHLBI Obesity Task Force: Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults—the evidence report. Obes Res 1998; 6(suppl 2):51S-209SGoogle Scholar
18. Kessler RC, Zhao S, Katz SJ, Kouzis AC, Frank RG, Edlund M, Leaf P: Past-year use of outpatient services for psychiatric problems in the National Comorbidity Survey. Am J Psychiatry 1999; 156:115-123Link, Google Scholar
19. Kirk RE: Experimental Design: Procedures for the Behavioral Sciences, 2nd ed. Pacific Grove, Calif, Brooks/Cole, 1982Google Scholar
20. National Household Survey on Drug Abuse. Rockville, Md, Substance Abuse and Mental Health Services Administration, US Department of Health and Human Services, 1999Google Scholar
21. Olfson M, Pincus HA: Outpatient psychotherapy in the United States, I: volume, costs, and user characteristics. Am J Psychiatry 1994; 151:1281-1288Google Scholar
22. Cachelin FM, Veisel C, Barzegarnazari E, Striegel-Moore RH: Disordered eating, acculturation, and treatment-seeking in a community sample of Hispanic, Asian, Black, and White women. Psychol of Women Quarterly 2000; 24:244-253Crossref, Google Scholar



