Past-Year Use of Outpatient Services for Psychiatric Problems in the National Comorbidity Survey
Abstract
OBJECTIVE: The authors present nationally representative descriptive data on 12-month use of outpatient services for psychiatric problems. They focused on the relationship between DSM-III-R disorders and service use in four broadly defined service sectors as well as the distribution of service use in multiple service sectors. METHOD: Data from the National Comorbidity Survey were examined. RESULTS: Summary measures of the seriousness and complexity of illness were significantly related to probability of use, number of sectors used, mean number of visits, and specialty treatment. One-fourth of the people in outpatient treatment were seen in multiple service sectors, but no evidence was found of multisector offset in number of visits. CONCLUSIONS: Use of outpatient services for psychiatric problems appears to have increased over the decade between the early 1980s and early 1990s, especially in the self-help sector. Aggregate allocation of treatment resources was related to need, highlighting the importance of making provisions for specialty care in the triage systems currently evolving as part of managed care.
It has been nearly two decades since the President’s Commission on Mental Health (1) called for improved data on use of services for psychiatric disorders in the United States, and it has been more than a decade since the Epidemiologic Catchment Area (ECA) study (2, 3) produced the first national data of this sort. The purpose of the present report is to provide more recent and representative data on 12-month use of outpatient services for psychiatric problems in the United States. The data come from the National Comorbidity Survey (4), a nationally representative household survey of prevalence and correlates of DSM-III-R disorders.
The focus of the current study was on basic descriptive issues. We began by examining the proportion of respondents in the total sample and in subsamples defined by 12-month disorders who obtained outpatient treatment for psychiatric problems during the year before the interview in each of four broadly defined service sectors. We were particularly interested in determining whether a higher proportion of people were in treatment than had been a decade earlier according to ECA study results (2) or whether there were differences in allocation of treatment across these different sectors.
We also examined whether, consistent with previous research (2, 3, 5), both probability of outpatient treatment and mean number of visits were highest for disorders defined a priori as most serious and complex. We would expect that such patterns would be found if allocation of treatment resources was related to need. In addition, we examined whether more serious disorders had a higher relative probability of treatment in the specialty sector than other treatment sectors. If this was true, it would imply that caution is needed in managed care efforts to substitute primary care for specialty treatment.
Finally, we examined the distribution of service use in multiple service sectors. We hypothesized that use of multiple service sectors was common and occurred most often among patients with serious disorders and comorbidity. We also examined whether the number of visits in any one sector varied depending on the number of visits in other sectors. We were especially interested in the possibility that participation in a self-help group among respondents who received professional treatment was associated with a decrease in the mean number of visits to a professional.
METHOD
Sample
The National Comorbidity Survey is based on a stratified, multistage, area probability sample of individuals 15 to 54 years old in the noninstitutionalized civilian population of the coterminous United States. Fieldwork was carried out between September 1990 and February 1992. The response rate was 82.4%, with 8,098 completed interviews. Informed consent was obtained from all respondents and from the parents of respondents who were 15–17 years old. Face-to-face interviews were carried out in two parts. Part 1 included the core diagnostic questions, and part 2 included risk factors and service use questions administered to a probability subsample of 5,877 respondents (all those with a lifetime disorder, all those 15–24 years old, and a random subsample of other respondents). The results reported in this paper are based on the subsample of part 2. These data were weighted for differential probabilities of selection and differential nonresponse. A weight was also included to adjust the sample to approximate the cross-classification of the population distribution on a range of sociodemographic characteristics. These weights are described in more detail elsewhere (4, 6).
Diagnostic Assessment
The 14 DSM-III-R diagnoses included in the present report were mood disorders (major depressive episode, dysthymia, mania), anxiety disorders (panic disorder, generalized anxiety disorder, simple phobia, social phobia, agoraphobia with or without panic, posttraumatic stress disorder), addictive disorders (alcohol and drug abuse and dependence), and nonaffective psychosis. The diagnoses were generated from a modified version of the fully structured Composite International Diagnostic Interview (7). World Health Organization field trials (8) and National Comorbidity Survey clinical reappraisal studies (9–13) have documented acceptable reliability and validity of all the Composite International Diagnostic Interview diagnoses considered here with two exceptions: 1) A National Comorbidity Survey clinical reappraisal study (14) found that the manic symptom profile characterized by euphoria, grandiosity, and decreased need for sleep is the only one validly assessed in the Composite International Diagnostic Interview, so the present report considers only that type of mania. 2) A National Comorbidity Survey clinical reappraisal study (15) also found that the Composite International Diagnostic Interview substantially overestimates the prevalence of nonaffective psychosis, so the present report defines nonaffective psychosis on the basis of clinical reinterviews administered to 454 National Comorbidity Survey respondents who screened positive for at least one psychotic symptom in the Composite International Diagnostic Interview.
To define an a priori gradient of presumed average seriousness of disorders in order to test hypotheses regarding between-disorder differences in patterns of service use, we assumed that nonaffective psychosis would be treated more often than other disorders, mania more often than other mood disorders, panic more often than other anxiety disorders, and substance dependence more often than substance abuse. To create a small number of subgroups that define a global gradient of psychiatric illness complexity as indicated by comorbidity, respondents were classified into four groups: those with two or more 12-month disorders, one 12-month disorder, no 12-month disorder but a lifetime history of one or more disorders, and no lifetime disorder.
Use of Outpatient Services
The first outpatient service use question was whether respondents ever in their lifetime went to see any of the professionals on a list (e.g., psychiatrist, psychologist, family doctor, minister) “for problems with your emotions or nerves or your use of alcohol or drugs.” Probe questions were then asked about recency of contact and number of visits during the past 12 months to each type of professional. A separate list was then presented describing different treatment settings (e.g., hospital emergency room, community mental health center, doctor’s private office), and probe questions were asked about recency of contact and number of visits during the past 12 months to each of these settings.
Respondents’ answers were grouped into three main service categories: health care, human services, and self-help, and a combination of questions probed each category. The health care category was broken down further into specialty and general medical. Specialty service contact was defined as either 1) seeing a psychiatrist or psychologist regardless of place, 2) seeing a social worker or counselor in either an emergency room, a psychiatric outpatient clinic, a drug or alcohol outpatient clinic, a doctor’s office, or a drop-in center or program for people with emotional problems or problems with drugs or alcohol, or 3) seeing a nurse in either a psychiatric outpatient clinic, a drug or alcohol outpatient clinic, or a drop-in center or program for people with emotional problems or problems with drugs or alcohol.
General medical service contact was defined as either 1) seeing a physician other than a psychiatrist regardless of place or 2) seeing a nurse, occupational therapist, or other allied health professional in either a hospital emergency department or a doctor’s private office. Together, specialty and general medical service contact were combined into a category of health care contact. Human service contact was defined as seeing either 1) a counselor, social worker, or nurse in a social service agency, 2) a minister, priest, or rabbi in any setting, 3) other types of nonmedical professionals (such as school counselors), or 4) using a hotline.
Use of the self-help sector was assessed by asking respondents if they had ever gone “to a self-help group for problems with your emotions or nerves or your use of alcohol or drugs.” Positive responses were followed with questions assessing recency of attendance and number of meetings attended in the past 12 months.
Analysis Procedures
The descriptive statistics reported here consist entirely of prevalences, means, and the standard errors of these estimates. Standard errors of estimates based on conventional estimation procedures are biased in the National Comorbidity Survey because of geographic clustering of the sample and use of weights. Therefore, standard errors were computed by using the method of jackknife repeated replications (16) in 42 design-based subsample replicates. A SAS macro (17) was written to operationalize the jackknife repeated replication procedure.
RESULTS
Probability of 12-Month Outpatient Service Use
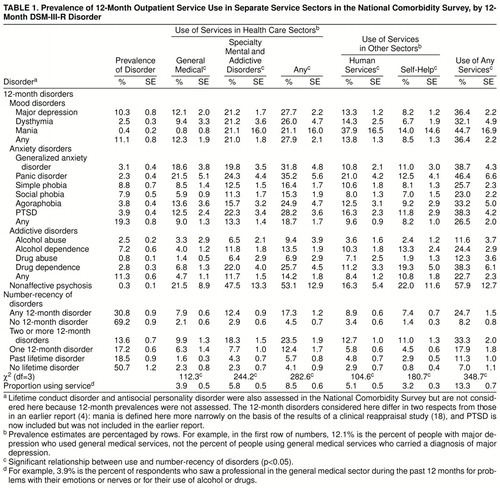
A previous report of National Comorbidity Survey data (18) found that 13.3% of respondents used some type of outpatient service for a psychiatric problem in the past 12 months—3.9% accessed the general medical sector, 5.8% the specialty sector, 5.1% the human services sector, and 3.2% the self-help sector. The detailed disorder-specific data in table 1 demonstrate that prevalence of outpatient use was highest among those with nonaffective psychosis. In addition, use was higher among those with mania than other mood disorders, among those with panic disorder than other anxiety disorders, and among those with drug dependence than other addictive disorders. As reported previously (18), there is a generally positive ordinal relationship between the summary measure of number-recency of disorders and prevalence of service use; the gradient of this relationship is most steep in the specialty sector. The number-recency measure is based on a more comprehensive set of disorders than those in a previous comparison of service use in the United States and Ontario (18), which explains differences between the results shown here for this summary measure and the results in the previous report.
The majority of patients (63.8% of those who used outpatient services) were seen in the health care sectors, and a higher proportion were seen in the specialty (43.7%) than in the general medical (29.2%) sector. Substantial proportions were also seen in the human services (38.6%) and self-help (24.3%) sectors. Proportional use of the specialty sector (43.7% of outpatients in the total sample) was highest for nonaffective psychosis (82.0%) and strongly related to number-recency of disorders.
Mean Number of Visits
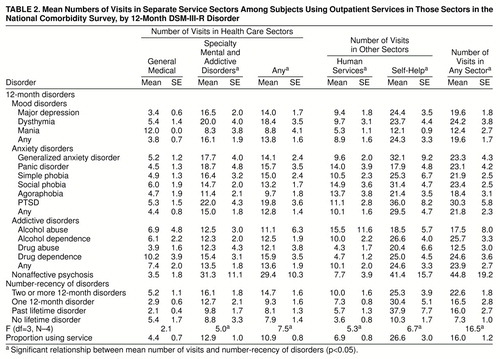
A previous report of National Comorbidity Survey data (18) showed that the average person in outpatient treatment made 16 visits in the last 12 months. table 2 shows that there are substantial differences in this mean across sectors, from a high of 26.6 visits in the self-help sector to a low of 4.4 visits in the general medical sector. With the exception of very high means among patients with nonaffective psychosis, there is little variation in either sector-specific or total means across classes of disorder. However, as reported previously (18), there is a generally significant and positive ordinal relationship between number-recency of disorders and mean number of visits. The only exception is in the general medical sector, where this relationship was not statistically significant.
Use of Multiple Sectors
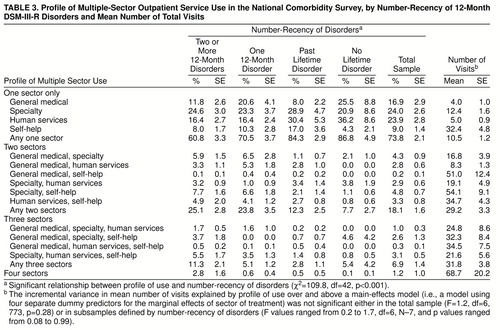
As shown in table 3, 73.8% of the respondents in outpatient treatment were seen in only one sector, 18.1% were seen in two, 6.9% were seen in three, and 1.2% were seen in all four sectors. The proportion of patients seen in multiple sectors was positively related to number-recency of disorders. Among those seen in only one sector, the specialty sector was used by the largest proportion of respondents with one or more 12-month disorders, but the human services sector was used by the largest proportion of respondents with none of the 12-month disorders. Among the respondents seen in multiple sectors, the combination of specialty and self-help was used by the largest proportion of patients with either one or more 12-month disorders, the combination of specialty and human services was used by the largest proportion of those with a past lifetime disorder, and the combination of specialty and general medical sectors was used by the largest proportion of those with no lifetime disorder. A significantly higher proportion of those in self-help (63.2% of 188 respondents) than other sectors (37.8%–45.2% of 229–341 respondents) were seen in multiple sectors (z=3.2–4.5, p=0.02–0.001). In addition, a significantly higher proportion of those seen in the self-help sector (48.0% of 188 respondents) than either the general medical sector (20.6% of 229 respondents) (z=4.7, p<0.001) or the human services sector (21.2% of 300 respondents) (z=5.1, p <0.001) were also seen in the specialty sector.
The results in the last column of table 3 show, as one would expect, that the overall number of visits increased with the number of service sectors. A more interesting finding is that this increase was roughly additive; that is, the mean numbers of visits for respondents seen in multiple sectors were similar in magnitude to the sum of the means for the one-sector respondents in these same sectors. This implies that the mean number of visits to, say, the general medical sector was not less among respondents who were in both the general medical and specialty sectors than among those who were only in the general medical sector. Deviation from this additivity was not statistically significant either in the sample as a whole (F=1.2, df=10, 769, p=0.29) or in subsamples defined by number-recency of disorders (analysis of variance results ranged from F=0.2, df=10, 193, p=0.12, in the subsample of respondents with no lifetime disorder to F=1.6, df=10, 246, p=0.12, in the subsample of respondents with two or more 12-month disorders).
DISCUSSION
Limitations
The results reported here are limited in a number of respects—they rely on 12-month recall, they exclude people living outside the sampling frame (i.e., the homeless and residents of institutional settings), and the large number of significance tests carried out creates an excessive chance of false significance of at least some results. The results should be interpreted with these limitations in mind.
Probability of Outpatient Service Use
The figure of 13.3% of National Comorbidity Survey respondents who used outpatient services is slightly higher than the 12.3% found a decade earlier in the ECA study (excluding the ECA respondents who were counted as receiving “services” in the ECA only because of talking to family or friends) (2), which superficially suggests that there was no change in probability of outpatient service use over that time interval. There are many differences in the two surveys, however, that confound any attempt to make rigorous comparisons (for example, an unrestricted age range in the ECA but not the National Comorbidity Survey, local sampling in the ECA versus national sampling in the National Comorbidity Survey, DSM-III diagnoses in the ECA versus DSM-III-R diagnoses in the National Comorbidity Survey).
Three aspects of the ECA study design created higher estimates of outpatient service use than we found in the National Comorbidity Survey. First, the ECA study was carried out largely in urban areas. Second, the ECA had a more inclusive definition of general medical use than the National Comorbidity Survey. Third, the ECA 12-month service use estimate was based on a combination of data from three interviews (a baseline interview that asked about service use during the previous 6 months, a reinterview 6 months later that asked about service use since baseline, and a second reinterview 12 months after baseline that asked about current service use). This would be expected to reduce recall failure compared with a single interview using 12-month recall. The fact that the 13.3% National Comorbidity Survey estimate is slightly higher than the 12.3% ECA estimate, despite these three differences, implies that a comparison using the same definitions of use and same sampling frame would probably show a clear increase between the early 1980s and early 1990s.
Two other sector-specific differences between the National Comorbidity Survey and the ECA are also worthy of note. First, general medical use was much lower in the National Comorbidity Survey (3.9%) than the ECA (6.4%). The ECA estimate implies that the general medical sector was the most common point of contact for outpatient psychiatric help-seeking (53% of all people in treatment seen in this sector), but the National Comorbidity Survey estimate implies that the rate of use of the general medical sector for psychiatric help was much lower (29%). This difference could be due to the three-wave ECA design having an especially strong effect in reducing recall failure of general medical visits. Or it could be because the question about general medical use was broader in the ECA than the National Comorbidity Survey. ECA respondents were asked whether they “talked to” a general medical provider “about” psychiatric problems, and they were asked whether they “went to” other providers “for help with” these problems. The National Comorbidity Survey asked the more narrow question of whether they went for psychiatric help to each of the providers in a comprehensive list that included, among others, both general medical providers and mental health specialists.
The National Comorbidity Survey presumably underestimated general medical use, in view of the fact that many people with emotional problems seek help in the general medical sector for primary somatic complaints (19, 20) and might not have gone “for help with” emotional problems even though these problems are mentioned as secondary complaints. However, if their physicians treated the emotional problems, the patients would be told to come back for a follow-up visit 2–4 weeks after starting their psychotropic medications to check on side effects and treatment response. These follow-up visits would be “for help with” emotional problems and would, therefore, be picked up in the National Comorbidity Survey question. This means that the only patients missed because of the wording of the National Comorbidity Survey question would be those who initially presented primary somatic problems and either were not treated for their secondary emotional problems or failed to make follow-up visits for treatment of their emotional problem. Exclusion of these patients is probably appropriate because it is difficult to think of them as truly having been in treatment for their emotional problems.
The ECA, in comparison, counted patients as being in treatment for their emotional problems if they told their doctor about these problems. As noted by Mechanic (21), this leads to substantial overestimation of general medical treatment of emotional problems because many of the patients who told their doctors about these problems did not receive treatment. Given the importance of primary care physicians as gatekeepers in managed care, future surveys need to resolve this uncertainty by combining the ECA and National Comorbidity Survey approaches to learn if respondents talked to a general medical doctor about psychiatric problems, whether this was the primary purpose of their visit, and whether they received treatment from the doctor for these problems. It is also important that future studies address the fact that primary care doctors sometimes prescribe psychotropics for patients they diagnose as somatizers without telling the patients they might have emotional problems. This hidden treatment of emotional problems might be very common (22, 23). If so, not only the National Comorbidity Survey but also the ECA could have substantially underestimated the true extent of general medical treatment of emotional problems.
A second difference between the National Comorbidity Survey and the ECA in sector-specific outpatient service use concerns self-help. Although 3.2% of National Comorbidity Survey respondents (accounting for more than 40% of all visits) reported participation in self-help groups, only 0.7% of ECA respondents did so (19% of all visits) (2, 3). The possibility has been raised that this difference could be due to the broader wording of the question about self-help use in the National Comorbidity Survey than the ECA. The National Comorbidity Survey asked respondents whether they went to a self-help group “for problems with your emotions or nerves or your use of alcohol or drugs,” while the ECA asked respondents if they went to “someone at a self-help group like Alcoholics Anonymous, etc.” It is conceivable that the ECA respondents interpreted this question narrowly to be asking exclusively about use of self-help groups for substance problems. If so, there might not have been any real change in self-help group use in the United States in the decade between the times the ECA and the National Comorbidity Survey were carried out.
We suspect, however, that the dramatically higher prevalence of reported self-help use in the National Comorbidity Survey than the ECA is due to more than a difference in the question wording. There are two reasons for this suspicion. The first is that the ECA question about self-help use was part of a larger series of questions introduced with the statement, “Now I’m going to read you a list of different kinds of places and people where someone might get help for problems with emotions, nerves, drugs, alcohol, or their mental health.” Questions in the series repeatedly asked respondents whether they saw various types of providers “for help with any of these problems” and intermittently repeated the entire stem by asking about seeing various types of providers “for help with problems with your emotions, nerves, drugs, alcohol, or your mental health.” The self-help question happened to be one of the questions in which this phrase was missing. However, we believe that it is likely, especially in the light of the fact that self-help participants reported attending a mean of 25 meetings a year, that such participants would think to report that they attend such a group for emotional problems, even though the only example given in the question was Alcoholics Anonymous.
The other reason we believe that the much higher prevalence of self-help use in the National Comorbidity Survey than the ECA is due to more than differences in question wording is that this higher prevalence estimate is consistent with a number of independent data sources. These include the observations of clinicians of a great increase in patients who seek help in self-help groups (24), an increase in self-help clearinghouses to handle the growth of self-help groups beginning in the 1980s (25–27), and the fact that a recent national survey (28) carried out after the National Comorbidity Survey found evidence based on synthetic cohort analysis of an enormous increase in self-help group participation in cohorts born after World War II.
The Relationship Between Need and Outpatient Service Use
Only a minority of the National Comorbidity Survey respondents who met criteria for a disorder in the 12 months before interview reported any 12-month outpatient treatment. This is consistent with findings of previous studies (2, 5), as is the finding that nearly half of the people who received treatment did not carry any of the disorders assessed in the National Comorbidity Survey (2). Earlier similar results raised concerns that a high proportion of mental health services might be going to people with low need (2, 3).
The debate about the relationship between diagnosis and need for treatment is complex and goes well beyond the focus of this report (29–31). However, two points are worth noting in response to the concern that treatment of many patients who fail to carry a DSM diagnosis is indicative of inappropriate treatment of people with low need. The first is that neither the National Comorbidity Survey nor earlier studies assessed the full range of DSM disorders. The second is that despite the fact that the National Comorbidity Survey assessed only a small proportion of all DSM disorders, nearly three-fourths of the visits reported in the National Comorbidity Survey were made by people who met criteria for one or more of the 12-month disorders and that close to 90% were made by people with at least one lifetime disorder.
We have no way of knowing which, if any, of the DSM disorders assessed in the National Comorbidity Survey were the primary reason for seeking treatment. Nonetheless, the findings that seriousness and comorbidity of disorders are strongly related both to probability of service use and to number of visits are consistent with findings in the ECA study (2, 3) and the RAND Health Insurance Experiment (5). However, there is one important exception to this general pattern—no statistically significant relationship was found between number-recency of disorders and duration of treatment in the general medical sector (table 3). This is identical to a result found in the RAND Health Insurance Experiment (5). Moreover, a related National Comorbidity Survey finding demonstrated that the gradient of the relationship between number-recency of disorders and probability of use was much less steep in the general medical sector than the specialty sector (ratios of 4.3 and 8.0, respectively, for probabilities of use in the highest versus lowest number-recency categories).
This last result could be due, at least in part, to the fact that the National Comorbidity Survey underestimated general medical use in the way described above. Furthermore, the fact that “diagnosis” is not the same as “need for treatment” means that we cannot conclude from these results that allocation of resources is less closely tied to need in the general medical sector than other sectors. Nor can we legitimately make inferences from these cross-sectional naturalistic data about the driving force behind the observed patterns. Nonetheless, these results do raise a question for future research regarding differences in the determinants of variation in treatment intensity across treatment sectors.
A related finding is the statistically significant relationship in the treatment subsample, as shown in table 1, between complexity of disorder (as indicated by a diagnosis of nonaffective psychosis or comorbidity) and treatment in the specialty versus nonspecialty sectors. This pattern is far from consistent, however, as indicated by the fact that the relative prevalences of treatment in the general medical and specialty sectors are greater for panic disorder than social phobia despite the fact that the impairment associated with panic is almost certainty greater than that associated with social phobia. The finding that the disorders of the patients seen by specialists are, in the aggregate, more complex than those seen in other service sectors contradicts some previous studies that have found only weak differences in the seriousness and complexity of cases seen in general medical versus specialty settings (2, 5) but is consistent with other studies (32–35). The documentation of this association in a nationally representative general population survey that includes service use in both the medical and nonmedical sectors highlights the importance of making provisions for specialty care in the triage systems currently evolving as part of managed care.
Use of Multiple Sectors
Over one-fourth of all outpatients and nearly 40% of outpatients with comorbid disorders were seen in more than one service sector. The self-help sector was most likely to be used in conjunction with some other sector rather than alone—63% of those in self-help were also in some other sector, compared with 42%–50% of those in other sectors. We have no way of determining from the National Comorbidity Survey data how often this use of multiple sectors was coordinated (e.g., a primary care doctor and psychologist working together to provide joint pharmacotherapy and talk therapy) versus uncoordinated or sequential.
The question naturally arises as to whether there is some sort of offset effect associated with use of multiple sectors. This would be much easier to study if data on coordination of treatment were available. To the extent that we can get a glimpse of this issue with the available data, there appears to be no offset effect. This conclusion is based on the finding that total visits were an additive function of the number and types of sectors used.
This said, it is important to realize that those who use multiple health care sectors are likely to have greater need and/or greater motivation to pursue treatment than those who use only one sector. This means that unmeasured aspects of demand for services might exist that confound any attempt to make causal inferences from the National Comorbidity Survey data concerning the offset effect of multiple sector use. A more fine-grained descriptive analysis or an experimental analysis might find that systematic adjunctive use of self-help as part of a comprehensive specialty treatment package could reduce the number of visits to specialists. Given the enormous popularity of self-help groups in the United States today and the existence of emerging models for combined use of professional and self-help services (36), it would seem to be an area warranting more systematic investigation.
ACKNOWLEDGMENTS
The National Comorbidity Survey is a collaborative epidemiologic investigation of the prevalences, causes, and consequences of psychiatric morbidity and comorbidity in the United States supported by the National Institute of Mental Health (grants MH-46376, MH-49098, and MH-52861) with supplemental support from the National Institute of Drug Abuse (through a supplement to grant MH-46376) and the W.T. Grant Foundation (grant 90135190), Ronald C. Kessler, principal investigator. Preparation for this report was also supported by a Research Scientist Award to Dr. Kessler (MH-00507).
Collaborating National Comorbidity Survey sites and investigators are as follows: the Addiction Research Foundation (Robin Room); Duke University Medical Center (Dan Blazer, Marvin Swartz); Harvard Medical School (Richard Frank, Ronald Kessler); Johns Hopkins University (James Anthony, William Eaton, Philip Leaf); the Max Planck Institute of Psychiatry Clinical Institute (Hans-Ulrich Wittchen); the Medical College of Virginia (Kenneth Kendler); the University of Miami (R. Jay Turner); the University of Michigan (Lloyd Johnston, Roderick Little); New York University (Patrick Shrout); the State University of New York, Stony Brook (Evelyn Bromet); and Washington University School of Medicine (Linda Cottler, Andrew Heath). A complete list of all National Comorbidity Survey publications, along with abstracts, study documentation, interview schedules, and the raw National Comorbidity Survey public use data files, can be obtained directly from the National Comorbidity Survey World Wide Web home page (http://www.hcp.med.harvard.edu/ncs).
Received July 23, 1997; revisions received Feb. 6 and May 11, 1998; accepted June 15, 1998. From the Department of Health Care Policy, Harvard Medical School; the Department of Sociology, Temple University, Philadelphia; the Departments of Internal Medicine and Health Services Management and Policy, University of Michigan, Ann Arbor; the Department of Mental Hygiene, Johns Hopkins University, Baltimore; and the Department of Psychiatry, University of California, Los Angeles. Address reprint requests to Dr. Kessler, Department of Health Care Policy, Harvard Medical School, 180 Longwood Ave., Boston, MA 02115. The authors thank Mark Olfson for helpful comments.
 |
 |
 |
1. Report to the President From the President"s Commission on Mental Health, vol I: Number 040-000-00390-8. Washington, DC, US Government Printing Office, 1978, p 1Google Scholar
2. Regier DA, Narrow WE, Rae DS, Manderscheid RW, Locke BZ, Goodwin FK: The de facto US mental and addictive disorders service system: Epidemiologic Catchment Area prospective 1-year prevalence rates of disorders and services. Arch Gen Psychiatry 1993; 50:85–94Crossref, Medline, Google Scholar
3. Narrow WE, Regier DA, Rae DS, Manderscheid RW, Locke BZ: Use of services by persons with mental and addictive disorders: findings from the National Institute of Mental Health Epidemiologic Catchment Area Program. Arch Gen Psychiatry 1993; 50:95–107Crossref, Medline, Google Scholar
4. Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen H-U, Kendler KS: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry 1994; 51:8–19Crossref, Medline, Google Scholar
5. Ware JE Jr, Manning WG Jr, Duan N, Wells KB, Newhouse JP: Health status and the use of outpatient mental health service. Am Psychologist 1984; 39:1090–1100Crossref, Medline, Google Scholar
6. Kessler RC, Little RJA, Groves RM: Advances in strategies for minimizing and adjusting for survey nonresponse. Epidemiol Rev 1995; 17:192–204Crossref, Medline, Google Scholar
7. World Health Organization: Composite International Diagnostic Interview (CIDI), version 1.0. Geneva, WHO, 1990Google Scholar
8. Wittchen H-U: Reliability and validity studies of the WHO-Composite International Diagnostic Interview (CIDI): a critical review. J Psychiatr Res 1994; 28:57–84Crossref, Medline, Google Scholar
9. Blazer DG, Kessler RC, McGonagle KA, Swartz MS: The prevalence and distribution of major depression in a national community sample: the National Comorbidity Survey. Am J Psychiatry 1994; 151:979–986Link, Google Scholar
10. Kessler RC, Crum RM, Warner LA, Nelson CB, Schulenberg J, Anthony JC: The lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Arch Gen Psychiatry 1997; 54:313–321Crossref, Medline, Google Scholar
11. Warner LA, Kessler RC, Hughes M, Anthony JC, Nelson CB: Prevalence and correlates of drug use and dependence in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry 1995; 52:219–229Crossref, Medline, Google Scholar
12. Wittchen H-U, Kessler RC, Zhao S, Abelson J: Reliability and clinical validity of UM-CIDI DSM-III-R generalized anxiety disorder. J Psychiatr Res 1995; 29:95–110Crossref, Medline, Google Scholar
13. Wittchen H-U, Zhao S, Abelson JM, Abelson JL, Kessler RC: Reliability and procedural validity of UM-CIDI DSM-III-R phobic disorders. Psychol Med 1996; 26:1169–1177Crossref, Medline, Google Scholar
14. Kessler RC, Rubinow DR, Holmes C, Abelson JM, Zhao S: The epidemiology of DSM-III-R bipolar I disorder in a general population survey. Psychol Med 1997; 27:1079–1089Crossref, Medline, Google Scholar
15. Kendler KS, Gallagher TJ, Abelson JM, Kessler RC: Lifetime prevalence, demographic risk factors, and diagnostic validity of nonaffective psychosis as assessed in a US community sample. Arch Gen Psychiatry 1996; 53:1022–1031Crossref, Medline, Google Scholar
16. Kish L, Frankel MR: Inference from complex samples. J Royal Statistical Society 1974; 36:1–37Google Scholar
17. SAS Introductory Guide, release 6.03. Cary, NC, SAS Institute, 1988Google Scholar
18. Kessler RC, Frank RG, Edlund M, Katz SJ, Lin E, Leaf P: Differences in the use of psychiatric outpatient services between the United States and Ontario. N Engl J Med 1997; 8:551–557Crossref, Google Scholar
19. Bridges KW, Goldberg DP: Somatic presentation of DSM III psychiatric disorders in primary care. J Psychosom Res 1985; 29:563–569Crossref, Medline, Google Scholar
20. Kirmayer LJ, Robbins JM: Patients who somatize in primary care: a longitudinal study of cognitive and social characteristics. Psychol Med 1996; 26:937–951Crossref, Medline, Google Scholar
21. Mechanic D: Treating mental illness: generalist versus specialist. Health Aff (Millwood) 1990; 9:61–75Crossref, Medline, Google Scholar
22. Jencks SF: Recognition of mental distress and diagnosis of mental disorder in primary care. JAMA 1985; 253:1903–1907Crossref, Medline, Google Scholar
23. Olfson M, Pincus HA: Measuring outpatient mental health care in the United States. Health Aff (Millwood) 1994; 13:172–180Crossref, Medline, Google Scholar
24. Zinman S: Self-help: the wave of the future. Hosp Community Psychiatry 1986; 37:213Abstract, Google Scholar
25. Madara EJ: A comprehensive system approach to promoting mutual aid self-help groups: the New Jersey Self-Help Clearinghouse model. J Voluntary Action and Res 1986; 15:57–63Google Scholar
26. Powell TJ: Self-Help Organizations and Professional Practice. Silver Spring, Md, National Association of Social Workers, 1987Google Scholar
27. Wollert RW, Knight B, Levy LH: Make today count: a collaborative model for professionals and self-help groups. Prof Psychol 1980; 11:130–138Google Scholar
28. Kessler RC, Mickelson KD, Zhao S: Patterns and correlates of self-help group membership in the United States. Social Policy 1997; 27:27–46Google Scholar
29. Regier DA, Kaelber CT, Rae DS, Farmer ME, Kn�uper B, Kessler RC, Norquist GS: Limitations of diagnostic criteria and assessment instruments for mental disorders: implications for research and policy. Arch Gen Psychiatry 1998; 55:109–115Crossref, Medline, Google Scholar
30. Spitzer RL: Diagnosis and need for treatment are not the same. Arch Gen Psychiatry 1998; 55:120Crossref, Medline, Google Scholar
31. Kessler RC: Some considerations in making resource allocation decisions for the treatment of psychiatric disorders, in Unmet Need in Mental Health Service Delivery. Edited by Andrews G. Cambridge, England, Cambridge University Press (in press)Google Scholar
32. Olfson M, Pincus HA: Outpatient mental health care in nonhospital settings: distribution of patients across provider groups. Am J Psychiatry 1996; 153:1353–1356Link, Google Scholar
33. Knesper DJ, Pagnucco DJ, Wheeler RC: Similarities and differences across mental health services providers and practice settings in the United States. Am Psychol 1985; 40:1352–1369Crossref, Medline, Google Scholar
34. Dew MA, Dunn LO, Bromet EJ, Schulberg HC: Factors affecting help-seeking during depression in a community sample. J Affect Disord 1988; 14:223–234Crossref, Medline, Google Scholar
35. Wells KB, Burnam MA, Camp P: Severity of depression in prepaid and fee-for-service general medical and mental health specialty practices. Med Care 1995; 33:350–364Crossref, Medline, Google Scholar
36. Riessman F, Carroll D (eds): Redefining Self-Help: Policy and Practice. San Francisco, Jossey-Bass, 1995Google Scholar



