The Relationship Between Cocaine Craving, Psychosocial Treatment, and Subsequent Cocaine Use
Abstract
OBJECTIVE: Regular measurement of craving during treatment for cocaine dependence can monitor patients’ clinical status and potentially assess their risk for drug use in the near future. Effective treatment can reduce the correlation between craving and subsequent drug use by helping patients abstain despite high craving. This study examined the relationship between cocaine craving, psychosocial treatment, and cocaine use in the ensuing week. METHOD: In the National Institute on Drug Abuse Collaborative Cocaine Treatment Study, which compared four psychosocial treatments for cocaine dependence, a three-item craving questionnaire was administered weekly to 449 patients to see whether it predicted cocaine use in the ensuing week. Cocaine use was assessed with self-reports and urine screening. RESULTS: With control for the previous week’s cocaine use, a higher composite score on the craving questionnaire was associated with greater likelihood of cocaine use in the subsequent week; each 1-point increase on the composite score of the craving questionnaire increased the likelihood of cocaine use in the ensuing week by 10%. However, among patients who received individual plus group drug counseling, the treatment condition with the best overall cocaine use outcome, increased craving scores were not associated with greater likelihood of cocaine use in the subsequent week. CONCLUSIONS: A three-item cocaine craving questionnaire predicted the relative likelihood of cocaine use during the subsequent week. Moreover, the relationship between craving and subsequent cocaine use varied by treatment condition, suggesting that the most effective treatment in the study might have weakened the link between craving and subsequent use.
Regular measurement of craving during substance abuse treatment can be helpful in monitoring patients’ clinical status and potentially assessing their risk for drug use in the near future. Measures of craving have been shown to predict future use of a variety of substances, including nicotine (1), methamphetamine (2), alcohol (3), and cocaine (4). Moreover, reduction in craving has been posited to be a mechanism of action of certain substance dependence treatments (5, 6) and has itself been used as a measure of treatment outcome (7).
A key goal of substance abuse treatment is to help patients abstain from drug use, even in the face of powerful urges, i.e., to resist craving (8). Thus, effective treatment might reduce the correlation between craving and subsequent drug use by helping patients abstain despite high levels of craving. We are aware of no studies, however, that have examined the possible interaction between craving and treatment to predict subsequent substance use.
The current study was carried out in the context of the National Institute on Drug Abuse Collaborative Cocaine Treatment Study (9, 10), a multicenter collaborative study designed to compare four psychosocial treatments for cocaine-dependent outpatients. The purpose of the current study was twofold. First, we used a slightly shortened version of a craving scale that we previously studied (the Cocaine Craving Scale) (11, 12) to assess its ability to predict a patient’s level of risk for cocaine use in the ensuing week. Second, we examined the relationship between craving levels and subsequent cocaine use in different treatment conditions. Our research questions were as follows:
Question 1: Does the score on the Cocaine Craving Scale in a given week predict the relative risk for cocaine use in the subsequent week?
Question 2: Does the relationship between craving in a given week and cocaine use in the subsequent week vary according to the type of treatment a patient receives?
Method
Patients
Patients were recruited for an outpatient treatment study of cocaine dependence from multiple sources at five sites (Brookside Hospital, Nashua, N.H., N=124; Massachusetts General Hospital, Boston, N=72; McLean Hospital, Belmont, Mass., N=48; the University of Pennsylvania, Philadelphia, N=120; and Western Psychiatric Institute and Clinic, Pittsburgh, N=123). Patients were eligible for the study if they had a principal diagnosis of cocaine dependence, according to DSM-IV criteria, were ages 18–60, and had used cocaine in the previous 30 days. Patients were excluded if they planned or required ongoing psychopharmacologic or psychotherapeutic treatment, presented an imminent homicide or suicide risk, were mandated to treatment, or had been hospitalized for cocaine dependence for more than 10 days in the past month. After complete description of the study to subjects, written informed consent was obtained.
Data for the National Institute on Drug Abuse Collaborative Cocaine Treatment Study were collected for 487 patients; they were primarily white (57.9%), male (76.8%), unmarried (69.6%), and employed (60.3%). Their mean age was 33.9 years (SD=6.3), and the patients had completed a mean of 13.0 years (SD=2.0) of education. The patients had used cocaine regularly for a mean of 6.9 years (SD=4.8); 79.0% had used cocaine primarily by smoking, 18.9% had primarily used the drug intranasally, and 2.1% had used the drug by injection. Patients had used cocaine a mean of 10.4 days (SD=7.8) in the month before study entry; they had spent a mean of $143 (SD=218) on cocaine during the past week. Their mean drug composite score on the Addiction Severity Index (13) was 0.24 (SD=0.06), and their mean alcohol composite score on the Addiction Severity Index was 0.22, both indicating a moderate level of severity, comparable to other groups of cocaine-dependent patients (14). One-third also met DSM-IV criteria for alcohol dependence and 4.5% for cannabis dependence. Most patients (56.8%) had received prior treatment for substance use disorder. In general, the group had low levels of psychiatric severity: their mean psychiatric composite score on the Addiction Severity Index was 0.19 (SD=0.19), similar to that reported in other outpatient cocaine treatment research studies (15). As noted previously, patients requiring psychotropic medication were excluded from the National Institute on Drug Abuse Collaborative Cocaine Treatment Study. There were no baseline differences in sociodemographic characteristics or on drug composite scores on the Addiction Severity Index among the four treatment groups. For more information on the subjects, see Crits-Christoph et al. (10).
Comparison of the subset of 449 patients in this study with the remaining 38 patients in the National Institute on Drug Abuse Collaborative Cocaine Treatment Study data set who did not have craving data (i.e., they completed fewer than two Cocaine Craving Scale questionnaires) revealed no significant differences between the groups on most of the foregoing descriptive variables. The excluded subjects were younger (mean=31.3 years, SD=5.6, versus mean=34.1 years, SD=6.3) (t=–2.62, df=485, p<0.01) and were more likely to be diagnosed with alcohol dependence (50.0% versus 31.8%) (χ2=5.20, df=1, p<0.03) when compared to the patients reported here.
Treatments
After screening and a brief stabilization period, the subjects received 24 weeks of active treatment. The treatments, all of which were manualized, were 1) individual drug counseling (16), based on the 12-step philosophy of treatment. Individual drug counseling emphasized the disease model of addiction, advocated healthy behavioral and lifestyle changes, and strongly encouraged self-help group therapy attendance; 2) supportive-expressive psychodynamic therapy (17), an individual therapy that focused on the importance of core interpersonal and intrapsychic themes in the genesis and maintenance of cocaine use; 3) cognitive therapy (18), an individual therapy that emphasized the importance of maladaptive beliefs and cognitions in addiction; and 4) group drug counseling (19), which educated patients about addiction recovery and strongly encouraged 12-step group participation.
Patients were randomly assigned to 1) individual drug counseling plus group drug counseling, 2) supportive-expressive psychodynamic therapy plus group drug counseling, 3) cognitive therapy plus group drug counseling, or 4) group drug counseling alone. Individual treatment occurred twice a week for the first 12 weeks and weekly during weeks 13 through 24. Group drug counseling sessions were held weekly for 24 weeks, with new patients entering and old patients completing treatment on an ongoing basis. Patients were referred for further treatment after study completion as clinically indicated. All treatment sessions were audiotaped, and sessions were independently reviewed for treatment adherence and fidelity. Study procedures and treatments are described in greater detail in Crits-Christoph et al. (9). Individual drug counselors had more experience treating substance-dependent patients than did supportive-expressive or cognitive therapists. All treatments were delivered as intended, and the treatments could readily be discriminated from each other (10). Results from the study revealed that patients who received individual drug counseling plus group drug counseling had cocaine use outcomes that were significantly better than those in the other treatment conditions, as shown by the greatest degree of improvement on the drug use composite score of the Addiction Severity Index (13), the fewest days of cocaine use, and the greatest number of abstinent months (10). There were no treatment-by-site interactions (10).
Measures
Cocaine Craving Scale
Craving for cocaine was assessed each week with the three-item Cocaine Craving Scale (11, 12). We previously reported a high degree of internal consistency for a slightly longer, five-item version of the Cocaine Craving Scale: Cronbach’s alphas ranged from 0.85 to 0.90 during the first 3 days of enrollment in the pilot phase of the National Institute on Drug Abuse Collaborative Cocaine Treatment Study (12). The three questions on the Cocaine Craving Scale were the following:
1. Please rate how strong your desire was to use cocaine during the last 24 hours.
2. Please imagine yourself in the environment in which you previously used drugs and/or alcohol. If you were in this environment today, what is the likelihood that you would use cocaine?
3. Please rate how strong your urges are for cocaine when something in the environment reminds you of it.
Response options ranged from 0 for “no desire/likelihood of use” to 9 for “strong desire/likelihood of use.” The composite score was a sum of these three items, ranging from 0 to 27. The previous five-item questionnaire was reduced to three items in the main trial of the National Institute on Drug Abuse Collaborative Cocaine Treatment Study to test the most parsimonious scale that could be administered regularly in a typical clinical setting with minimal patient and clinician burden. The two items eliminated were those that correlated most highly (0.78–0.91) with the remaining items and that added no predictive validity to the questionnaire. The omitted items were the following:
1. Please rate how strong your desire for cocaine is right now.
2. Please rate how often you had the urge to use cocaine during the past 24 hours.
In the current study, the Cocaine Craving Scale was administered just before a patient’s first treatment session each week; a treatment session could be held on any day of the week. If the patient missed a treatment session, the Cocaine Craving Scale was administered when the patient came in the next day for a urine screen.
Cronbach’s alpha was computed for the three-item Cocaine Craving Scale during the patients’ first month of treatment by using a mean of the scores reported for that month. Since the alpha was high (0.78), subsequent data are reported on the basis of the composite craving score rather than for each item.
Cocaine Use
To evaluate the ability of the Cocaine Craving Scale to predict cocaine use during the subsequent week, cocaine use was assessed as either present or absent each week. This was determined from information gathered from the Quantitative Cocaine Inventory (20), which was administered weekly, and an observed urine toxicology screen, also collected weekly. If either assessment indicated cocaine use during the previous week, the patient was coded as having used cocaine during that week. Assessments are described in greater detail in Crits-Christoph et al. (9). This dichotomous measure of cocaine use was also used as an independent variable in the lagged data analyses.
Data Analysis
Longitudinal analyses of the relationship between craving during a particular week and cocaine use in the following week required two consecutive weeks of craving and cocaine use data. Generalized estimating equations methods were used to account for the correlation of repeated measures for each patient over time and was implemented by using SAS version 6.12 (SAS Institute, Cary, N.C.). Linear and quadratic trends were compared to analyses of composite scores on the Cocaine Craving Scale, with linear models presented since they were more predictive. Patients with incomplete data were included in the analyses, after assessment of the data to determine whether this was appropriate, i.e., whether missing data were informative or not. Addressing the problem of missing data by excluding patients with incomplete data or imputing data was ruled out as potentially producing biased results. The pattern-mixture method described by Hedeker and Gibbons (21) was applied to the longitudinal analyses of the Cocaine Craving Scale score, treatment type, and cocaine use, indicating that missing data patterns did not alter the results; therefore, missing data were not informative, and inferences from the generalized estimating equations model are valid. Since recent cocaine use can cause high levels of craving (22) and predicts a greater likelihood of subsequent use (23), we controlled for cocaine use in the previous week. To address the second research question, regarding whether craving interacts with type of treatment to predict cocaine use, treatment condition was added as a covariate.
Results
Question 1: Does the Score on the Cocaine Craving Scale in a Given Week Predict the Relative Risk for Cocaine Use in the Subsequent Week?
We found that craving, as measured by the score on the composite Cocaine Craving Scale, was a statistically significant predictor of cocaine use in the following week (odds ratio=1.1, z=7.05, p<0.001). The odds ratio for the composite score was based on a 27-point scale, so that an odds ratio of 1.1 corresponded to a 10% greater likelihood of use in the subsequent week for every 3-point difference in the composite score, with higher scores indicating greater risk.
Question 2: Does the Relationship Between Craving in a Given Week and Cocaine Use in the Subsequent Week Vary According to the Type of Treatment a Patient Receives?
Treatment condition was added to the previous statistical model predicting cocaine use as a function of craving and cocaine use in the preceding week. While the composite score on the Cocaine Craving Scale remained a statistically significant predictor of cocaine use in the ensuing week (χ2=54.95, df=1, p<0.0001), treatment condition was also a statistically significant predictor of cocaine use (χ2=54.27, df=3, p<0.002). Furthermore, the interaction of treatment and composite score on the Cocaine Craving Scale on cocaine use was significant (χ2=8.80, df=3, p<0.04). Pairwise comparisons indicated that individual drug counseling plus group drug counseling was significantly different from both cognitive therapy plus group drug counseling and group drug counseling alone (p<0.01) and marginally different from supportive-expressive therapy plus group drug counseling (p<0.08). Individual drug counseling plus group drug counseling compared to the three other treatments combined was quite significant (p<0.005). All remaining pairwise and group comparisons were not significant (p>0.23), although group drug counseling alone versus all other treatments was marginally significant (p<0.09). Least square means of cocaine use were calculated, with adjustment for cocaine use in the preceding week, the composite score on the Cocaine Craving Scale in the preceding week, and the interaction between the score on the Cocaine Craving Scale and treatment condition. The results, presented in Figure 1, show a significant interaction of treatment condition and the relationship between craving in a given week and cocaine use in the subsequent week.
We found that a higher composite score on the Cocaine Craving Scale was associated with a greater likelihood of cocaine use in the subsequent week, with one exception. That is, the relationship between craving and cocaine use in the subsequent week among patients in the individual drug counseling plus group drug counseling treatment condition appeared to be relatively flat, showing that cocaine use by patients in the individual drug counseling plus group drug counseling group, who had, on average, the least cocaine use in the study (10), did not vary by the severity of their craving for cocaine. To portray this interaction visually, a three-level ordinal variable was created for the composite score on the Cocaine Craving Scale: mild (score=1–5), moderate (score=6–11), and severe (score=12–27), with a well-balanced design of 37%, 30%, and 33%, respectively, for the craving composite scores in each category (Figure 1).
Discussion
In this study of 449 cocaine-dependent patients who received psychosocial treatment in the National Institute on Drug Abuse Collaborative Cocaine Treatment Study, a brief three-item questionnaire on different aspects of cocaine craving predicted the relative likelihood of cocaine use during the subsequent week. Of interest, the relationship between craving and subsequent cocaine use varied by treatment condition, suggesting that the combination of individual drug counseling plus group drug counseling, the most effective treatment in the study (10), might have weakened the link between cocaine craving and subsequent use.
The concept of craving is controversial (24), as is its measurement. Numerous instruments have been developed to assess craving (25–28), reflecting different conceptualizations of the phenomenon. Although the Cocaine Craving Scale assessed different aspects of craving, this instrument, like any questionnaire, is a purely subjective measure of craving; the same phenomenon that may feel like a strong craving to one individual may be experienced as a weak craving by someone else. Some craving researchers have emphasized the balance between urges and urge resistance in determining use or abstinence (3, 28, 29); this approach implies that a high level of desire for a drug can be mitigated or counterbalanced by other factors (e.g., the desire to abstain), which can reduce the likelihood of use. Abrams (30) has also suggested that craving can interact with phenomena such as self-efficacy to predict subsequent drug use.
The ability of a type of treatment to weaken the link between craving and drug use has potentially interesting implications in understanding the mechanism of action of effective therapies for substance use disorders. While patients receiving the combination of individual drug counseling plus group drug counseling had significantly better cocaine use outcomes than did patients receiving other forms of treatment in the National Institute on Drug Abuse Collaborative Cocaine Treatment Study, it is unclear exactly which components of individual drug counseling plus group drug counseling were particularly useful. The findings from this study suggest that one helpful aspect of this treatment was its ability to help patients cope effectively with craving. Because individual drug counseling was more behaviorally prescriptive than the other study treatments, the counselor delivering the individual drug counseling component of individual plus group drug counseling would be most likely to firmly advise a patient to avoid former drug-using environments (under the rubric of “avoid risky people, places, and things”), particularly when the patient felt at risk to use cocaine. Thus, while individual drug counseling did not focus primarily on craving, its straightforward behavioral emphasis on the importance of abstinence may have helped patients cope with the strong desire to use cocaine.
Previous clinical research has primarily focused either on the predictive validity of craving or on its reduction by a particular treatment modality. Craving reduction has, in fact, been a target outcome in the development and testing of certain medications (5, 31). The current study shows the potential promise of another avenue of craving research, specifically, the examination of altering the strength of the link between craving and drug use. One could, for example, posit that certain types of treatments could reduce craving, while other treatments could help patients cope more effectively with craving, either by increasing impulse control, by enhancing motivation for abstinence, or by helping patients develop coping skills. It is possible that a combination of treatments, e.g., pharmacotherapy and psychotherapy, could target both complementary goals, although current pharmacotherapies to reduce craving in cocaine-dependent patients have not been shown to be reliably effective (32).
Of course, other factors might also attenuate the link between craving and use, such as length of time (11) or the attachment of positive or negative contingencies to abstinence or drug use, respectively. It is possible that high levels of craving during a weekend may be more likely to lead to drug use than similar craving levels during the week, since drug availability may be greater during the weekend. Moreover, some patients may use drugs in the absence of urges, as part of a long-standing habitual automatic behavior pattern (33). In such cases, it could be posited that while the urge to use is low, the resistance to use is even lower, thus resulting in drug use.
The present study is limited by the fact that the study patients were sufficiently motivated to enter a demanding and time-intensive treatment research program. Less motivated patients might have had less response to any treatment intervention in the face of strong urges. It would also have been interesting to see the relationship between craving and subsequent cocaine use in a group of patients receiving no treatment, since a no-treatment control group was not included in the National Institute on Drug Abuse Collaborative Cocaine Treatment Study. Moreover, it is possible that the 38 patients who did not complete Cocaine Craving Scale forms, who were generally younger and more likely to be alcohol dependent, may have been less responsive to treatment than the 449 patients included in the study group. The inclusion of primarily white male patients exclusively from the Northeast and the exclusion of patients involved in other psychotherapeutic or psychopharmacologic treatment could have reduced the generalizability of the results. Our findings suggest, however, that future research with other populations could productively examine factors that affect the relationship between craving and drug use.
Acknowledgments
The National Institute on Drug Abuse Collaborative Cocaine Treatment Study is a cooperative agreement funded by the National Institute on Drug Abuse involving four clinical sites, a coordinating center, and the National Institute on Drug Abuse staff. The coordinating center at the University of Pennsylvania includes Paul Crits-Christoph, Ph.D. (principal investigator), Lynne Siqueland, Ph.D. (project coordinator), Karla Moras, Ph.D. (assessment unit director), Jesse Chittams, M.A., and Bob Gallop, Ph.D. (directors of data management/analysis), and Larry Muenz, Ph.D. (statistician). The collaborating scientists at the Treatment Research Branch, Division of Clinical and Research Services, include Jack Blaine, M.D., and Lisa Simon Onken, Ph.D. The four participating clinical sites are the University of Pennsylvania: Lester Luborsky, Ph.D. (principal investigator), Jacques P. Barber, Ph.D. (co-principal investigator), and Delinda Mercer, Ph.D. (project director); Brookside Hospital/Harvard Medical School: Arlene Frank, Ph.D. (principal investigator), Stephen F. Butler, Ph.D. (co-principal investigator/Innovative Training Systems), and Sarah Bishop, M.A. (project director); McLean/Massachusetts General Hospital/Harvard University Medical School: Roger D. Weiss, M.D. (principal investigator), David R. Gastfriend, M.D. (co-principal investigator), Lisa M. Najavits, Ph.D., and Margaret L. Griffin, Ph.D. (project directors); University of Pittsburgh/Western Psychiatric Institute and Clinic: Michael E. Thase, M.D. (principal investigator), Dennis Daley, Ph.D. (co-principal investigator), Ishan M. Salloum, M.D. (co-principal investigator), and Judy Lis, M.S.N. (project director).
The training unit includes heads of the Cognitive Therapy Training Unit: Aaron T. Beck, M.D. (University of Pennsylvania) and Bruce Liese, Ph.D. (University of Kansas Medical Center); heads of the Supportive-Expressive Therapy Training Unit: Lester Luborsky, Ph.D., and David Mark, Ph.D. (University of Pennsylvania); heads of the Individual Drug Counseling Unit: George Woody, M.D. (Veterans Administration/University of Pennsylvania Medical School) and the Group Drug Counseling Unit: Delinda Mercer (head), Dennis Daley (assistant head, University of Pittsburgh/Western Psychiatric Institute and Clinic) and Gloria Carpenter, M.Ed. (assistant head, Treatment Research Unit, University of Pennsylvania). The monitoring board includes Larry Beutler, Ph.D., Jim Klett, Ph.D., Bruce Rounsaville, M.D., and Tracie Shea, Ph.D.
Presented in part at the 62nd Annual Scientific Meeting of the College on Problems of Drug Dependence, San Juan, Puerto Rico, June 17–22, 2000. Received Sept. 25, 2001; revision received Sept. 13, 2002; accepted Dec. 10, 2002. From the Department of Psychiatry, Harvard Medical School, Boston; McLean Hospital; the Center for Psychotherapy Research, Department of Psychiatry, the University of Pennsylvania, Philadelphia; Massachusetts General Hospital, Boston; the National Institute on Drug Abuse, Bethesda, Md.; the Department of Psychiatry, University of Pittsburgh; and Western Psychiatric Institute and Clinic, Pittsburgh. Address reprint requests to Dr. Weiss, McLean Hospital, 115 Mill St., Belmont, MA 02478; [email protected] (e-mail). Funded by grants DA-07090, DA-00326, DA-07663, DA-07673, DA-07693, DA-07085 from the National Institute on Drug Abuse and MH-45178 from NIMH and a grant from the Dr. Ralph and Marian C. Falk Medical Research Trust. The authors thank John Boren, Ph.D., and Deborah Grossman, M.A., from the National Institute on Drug Abuse, the project officers for this cooperative agreement.
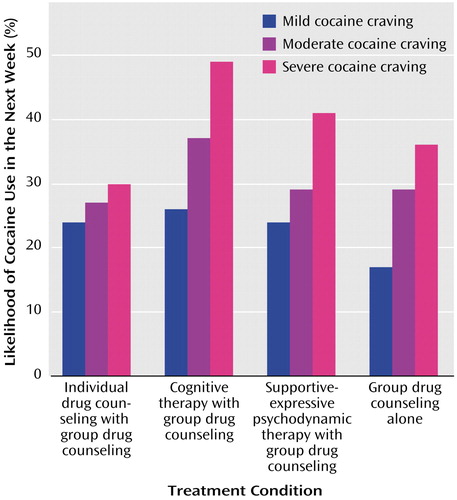
Figure 1. Relationship Between Treatment Condition, Cocaine Craving, and Likelihood of Cocaine Use in the Next Week Among 449 Patients in the National Institute on Drug Abuse Collaborative Cocaine Treatment Studya
aCocaine craving was assessed weekly with a three-item version of the Cocaine Craving Scale (11, 12), on which a composite score of 1–5 indicated mild craving; 6–11, moderate craving; and 12–27, severe craving. Cocaine use was assessed weekly with self-reports and urine screening.
1. Killen JD, Fortmann SP, Newman B, Varady A: Prospective study of factors influencing the development of craving associated with smoking cessation. Psychopharmacology (Berl) 1991; 105:191-196Crossref, Medline, Google Scholar
2. Hartz DT, Frederick-Osborn SL, Galloway GP: Craving predicts use during treatment for methamphetamine dependence: a prospective, repeated-measures, within-subject analysis. Drug Alcohol Depend 2001; 63:269-276Crossref, Medline, Google Scholar
3. Roberts JS, Anton RF, Latham PK, Moak DH: Factor structure and predictive validity of the Obsessive Compulsive Drinking Scale. Alcohol Clin Exp Res 1999; 23:1484-1491Crossref, Medline, Google Scholar
4. Rohsenow DJ, Martin R, Monti PM: Predicting cocaine use outcomes from craving in simulated high risk situations: preliminary results, in Problems of Drug Dependence 1998: Proceedings of the 60th Annual Scientific Meeting of the National Institute on Drug Abuse: NIDA Research Monograph 179. Edited by Harris LS. Bethesda, Md, NIDA, 1998, p 165Google Scholar
5. Kosten TR: Can cocaine craving be a medication development outcome? drug craving and relapse in opioid and cocaine dependence. Am J Addict 1992; 1:230-239Google Scholar
6. Swift RM: Drug therapy for alcohol dependence. N Engl J Med 1999; 340:1482-1490Crossref, Medline, Google Scholar
7. Gawin FH, Morgan CR, Osten TK: Double-blind evaluation of the effect of acute amantadine on cocaine craving. Psychopharmacology (Berl) 1989; 97:402-403Crossref, Medline, Google Scholar
8. Marlatt GA: Cognitive factors in the relapse process, in Relapse Prevention: Maintenance Strategies in the Treatment of Addictive Behaviors. Edited by Marlatt GA, Gordon JR. New York, Guilford Press, 1985, pp 128-200Google Scholar
9. Crits-Christoph P, Siqueland L, Blaine J, Frank A, Luborsky L, Onken LS, Muenz L, Thase ME, Weiss RD, Gastfriend DR, Woody G, Barber JP, Butler SF, Daley D, Bishop S, Najavits LM, Lis J, Mercer D, Griffin ML, Moras K, Beck AT: The National Institute on Drug Abuse Collaborative Cocaine Treatment Study: rationale and methods. Arch Gen Psychiatry 1997; 54:721-726Crossref, Medline, Google Scholar
10. Crits-Christoph P, Siqueland L, Blaine J, Frank A, Luborsky L, Onken LS, Muenz L, Thase ME, Weiss RD, Gastfriend DR, Woody G, Barber JP, Butler SF, Daley D, Salloum I, Bishop S, Najavits LM, Lis J, Mercer D, Griffin ML, Moras K, Beck AT: Psychosocial treatments for cocaine dependence: National Institute on Drug Abuse Collaborative Cocaine Treatment Study. Arch Gen Psychiatry 1999; 56:493-502Crossref, Medline, Google Scholar
11. Weiss RD, Griffin ML, Hufford C: Craving in hospitalized cocaine abusers as a predictor of outcome. Am J Drug Alcohol Abuse 1995; 21:289-301Crossref, Medline, Google Scholar
12. Weiss RD, Griffin ML, Hufford C, Muenz LR, Najavits LM, Jansson SB, Kogan J, Thompson HJ: Early prediction of initiation of abstinence from cocaine: use of a craving questionnaire. Am J Addict 1997; 6:224-231Medline, Google Scholar
13. McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, Pettinati H, Argeriou M: The Fifth Edition of the Addiction Severity Index. J Subst Abuse Treat 1992; 9:199-213Crossref, Medline, Google Scholar
14. McKay JR, Alterman AI, McLellan AT, Snider EC: Treatment goals, continuity of care, and outcome in a day hospital substance abuse rehabilitation program. Am J Psychiatry 1994; 151:254-259Link, Google Scholar
15. Carroll KM, Rounsaville BJ, Gordon LT, Nich C, Jatlow P, Bisighini RM, Gawin FH: Psychotherapy and pharmacotherapy for ambulatory cocaine abusers. Arch Gen Psychiatry 1994; 51:177-187Crossref, Medline, Google Scholar
16. Mercer D, Woody G: Addiction Counseling. Philadelphia, University of Pennsylvania/Philadelphia Veterans Affairs Medical Center, Center for Studies of Addiction, 1992Google Scholar
17. Mark D, Luborsky L: A Manual for the Use of Supportive-Expressive Psychotherapy in the Treatment of Cocaine Abuse. Philadelphia, University of Pennsylvania, Department of Psychiatry, 1992Google Scholar
18. Beck AT, Wright FD, Newman CF, Liese BS: Cognitive Therapy of Substance Abuse. New York, Guilford, 1993Google Scholar
19. Mercer D, Carpenter G, Daley D, Patterson C, Volpicelli J: Addiction Recovery Manual, vol 2. Philadelphia, University of Pennsylvania, Treatment Research Unit, 1994Google Scholar
20. Gawin FH, Kleber HD, Byck R, Rounsaville BJ, Kosten TR, Jatlow PI, Morgan C: Desipramine facilitation of initial cocaine abstinence. Arch Gen Psychiatry 1989; 46:117-121Crossref, Medline, Google Scholar
21. Hedeker D, Gibbons RD: Application of random-effects pattern-mixture models for missing data in longitudinal studies. Psychol Methods 1997; 2:64-78Crossref, Google Scholar
22. Jaffe JH, Cascella NG, Kumor KM, Sherer MA: Cocaine-induced cocaine craving. Psychopharmacology (Berl) 1989; 97:59-64Crossref, Medline, Google Scholar
23. Alterman AI, Kampman K, Boardman CR, Cacciola JS, Rutherford MJ, McKay JR, Maany I: A cocaine-positive baseline urine predicts outpatient treatment attrition and failure to attain initial abstinence. Drug Alcohol Depend 1997; 46:79-85Crossref, Medline, Google Scholar
24. Kozlowski LT, Wilkinson D: Use and misuse of the concept of craving by alcohol, tobacco, and drug researchers. Br J Addict 1987; 82:31-36Crossref, Medline, Google Scholar
25. Tiffany ST: A cognitive model of drug urges and drug use behavior: role of autonomic and non-autonomic processes. Psychol Rev 1990; 97:147-168Crossref, Medline, Google Scholar
26. Halikas JA, Kuhn KL, Crosby R, Carlson G, Crea F: The measurement of craving in cocaine patients using the Minnesota Cocaine Craving Scale. Compr Psychiatry 1991; 32:22-27Crossref, Medline, Google Scholar
27. Anton RF, Moak DH, Latham PK: The Obsessive Compulsive Drinking Scale: a new method of assessing outcome in alcoholism treatment studies. Arch Gen Psychiatry 1996; 53:225-231Crossref, Medline, Google Scholar
28. Flannery BA, Volpicelli JR, Pettinati HM: Psychometric properties of the Penn Alcohol Craving Scale. Alcohol Clin Exp Res 1999; 12:1289-1295Crossref, Google Scholar
29. Anton RF: Alcohol craving—a renaissance (editorial). Alcohol Clin Exp Res 1999; 12:1287-1288Crossref, Google Scholar
30. Abrams DB: Transdisciplinary concepts and measures of craving: commentary and future directions. Addiction 2000; 95(suppl 2):S237-S246Google Scholar
31. Renshaw P, Daniels S, Lundahl L, Rogers V, Lukas S: Short-term treatment with citicoline (CDP-choline) attenuates some measures of craving in cocaine-dependent subjects: a preliminary report. Psychopharmacology (Berl) 1999; 142:132-138Crossref, Medline, Google Scholar
32. O’Leary G, Weiss RD: Pharmacotherapies for cocaine dependence. Curr Psychiatry Rep 2000; 2:508-513Crossref, Medline, Google Scholar
33. Tiffany ST, Barter BL: Is craving the source of compulsive drug use? J Psychopharmacol 1998; 12:23-30Crossref, Medline, Google Scholar



