Anticholinergic Medication Burden–Associated Cognitive Impairment in Schizophrenia
Abstract
Objective:
Many psychotropic medications used to treat schizophrenia have significant anticholinergic properties, which are linked to cognitive impairment and dementia risk in healthy subjects. Clarifying the impact of cognitive impairment attributable to anticholinergic medication burden may help optimize cognitive outcomes in schizophrenia. The aim of this study was to comprehensively characterize how this burden affects functioning across multiple cognitive domains in schizophrenia outpatients.
Methods:
Cross-sectional data were analyzed using inferential statistics and exploratory structural equation modeling to determine the relationship between anticholinergic medication burden and cognition. Patients with a diagnosis of schizophrenia or schizoaffective disorder (N=1,120) were recruited from the community at five U.S. universities as part of the Consortium on the Genetics of Schizophrenia−2. For each participant, prescribed medications were rated and summed according to a modified Anticholinergic Cognitive Burden (ACB) scale. Cognitive functioning was assessed by performance on domains of the Penn Computerized Neurocognitive Battery (PCNB).
Results:
ACB score was significantly associated with cognitive performance, with higher ACB groups scoring worse than lower ACB groups on all domains tested on the PCNB. Similar effects were seen on other cognitive tests. Effects remained significant after controlling for demographic characteristics and potential proxies of illness severity, including clinical symptoms and chlorpromazine-equivalent antipsychotic dosage.
Conclusions:
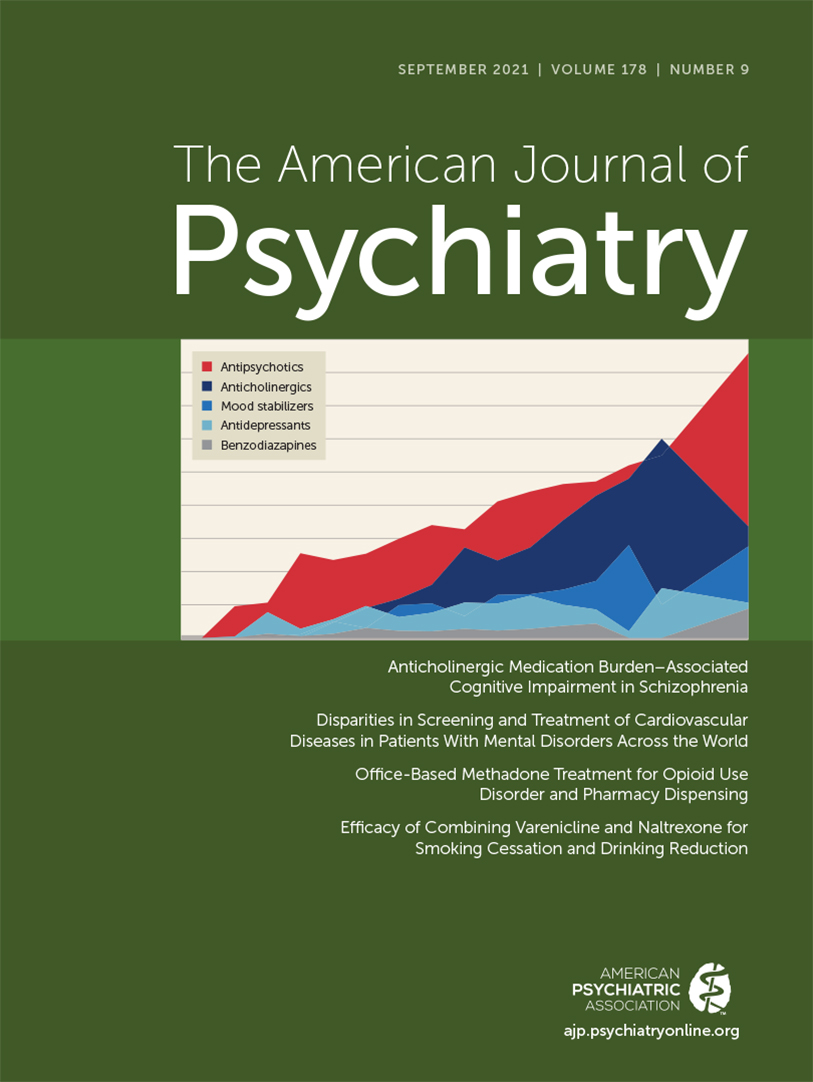
Anticholinergic medication burden in schizophrenia is substantial, common, conferred by multiple medication classes, and associated with cognitive impairments across all cognitive domains. Anticholinergic medication burden from all medication classes–including psychotropics used in usual care–should be considered in treatment decisions and accounted for in studies of cognitive functioning in schizophrenia.