The Mood Spectrum in Unipolar and Bipolar Disorder: Arguments for a Unitary Approach
Abstract
OBJECTIVE: This study examined the extent to which individuals with a lifetime diagnosis of recurrent unipolar disorder endorse experiencing manic/hypomanic symptoms over their lifetimes and compared their reports with those of patients with bipolar I disorder. METHOD: The study group included 117 patients with remitted recurrent unipolar depression and 106 with bipolar I. Subjects had their clinical diagnosis confirmed by the Mini International Neuropsychiatric Interview and were administered the Structured Clinical Interview for the Mood Spectrum, which assesses lifetime symptoms, traits, and lifestyles that characterize threshold and subthreshold mood episodes as well as “temperamental” features related to mood dysregulation. RESULTS: The patients with recurrent unipolar depression endorsed experiencing a substantial number of manic/hypomanic symptoms over their lifetimes. In both patients with recurrent unipolar depression and patients with bipolar I disorder, the number of manic/hypomanic items endorsed was related to the number of depressive items endorsed. In the group with recurrent unipolar depression, the number of manic/hypomanic items was related to an increased likelihood of endorsing paranoid and delusional thoughts and suicidal ideation. In the bipolar I group, the number of lifetime manic/hypomanic items was related to suicidal ideation and just one indicator of psychosis. CONCLUSIONS: The presence of a significant number of manic/hypomanic items in patients with recurrent unipolar depression seems to challenge the traditional unipolar-bipolar dichotomy and bridge the gap between these two categories of mood disorders. The authors argue that their mood spectrum approach is useful in making a more accurate diagnostic evaluation in patients with mood disorders.
For most of the 20th century, depressed patients were dichotomized by using the categories “single episode” versus “recurrent” and “unipolar” versus “bipolar.” There is now ample evidence that almost all depressions are recurrent to a greater or lesser degree (1–5). Now the question arises whether almost all recurrent depressions are bipolar to a greater or lesser degree.
The distinction between bipolar and unipolar disorder served our field well in the early days of psychopharmacology. However, this distinction has been challenged in the last decades by the following:
| 1. | Clinical studies (6, 7) showing that bipolar disorder is frequently misdiagnosed as unipolar major depressive disorder and consequently mistreated | ||||
| 2. | Theoretical studies (8, 9) warning about limitations of the categorical diagnoses of bipolar disorder and unipolar depression | ||||
| 3. | Epidemiological studies (10) supporting a widening of the boundaries of the bipolar spectrum to include hypomania, cyclothymia, and bipolar disorder not otherwise specified | ||||
| 4. | Familial and genetic studies (11, 12) indicating that the familial aggregation of bipolar disorder and severe unipolar depression is at least partly due to genetic factors | ||||
Despite converging evidence on its clinical validity, what has been termed “bipolar II disorder,” with its requirement of discrete episodes of hypomania, has proven to be a diagnosis on which it is difficult to achieve good agreement between clinicians (13), mainly because hypomanic symptoms frequently fail to cluster in the way presumed by the diagnostic criteria that are drawn from our concept of manic episodes. Akiskal and Pinto (14) have claimed that there is a substantial proportion of unipolar patients whose mood disorder shows bipolar affinity and that such patients occupy a large terrain between the extremes of classic unipolarity and bipolarity. To address this diagnostic conundrum, he and his colleagues have proposed a number of discrete syndromes characterized by decreasing severity of mania/hypomania under a rubric of “bipolar spectrum.” We agree with Akiskal and Pinto that there are large numbers of so-called unipolar patients who exhibit mild hypomanic symptoms; however, we argue that the field would benefit from a unitary and continuous approach to the assessment of both manic/hypomanic and depressive symptoms. On the basis of this unitary conceptualization of mood disorders, we hypothesized that patients with recurrent major depression without discrete lifetime hypomanic episodes would nonetheless report lifetime hypomanic/manic symptoms and that the number of lifetime hypomanic/manic symptoms would be related to the number of lifetime depressive symptoms. Finally, we hypothesized that manic/hypomanic symptoms would be associated with indicators of greater severity of depression.
We tested these hypotheses in 223 patients with mood disorders who were administered a structured clinical interview for the spectrum of mood disorders (15). This instrument focuses on lifetime manic and depressive symptoms, traits, and lifestyles that characterize threshold and subthreshold mood episodes and “temperamental” features related to affective dysregulation.
Method
Study Group
The study group was drawn from a larger cross-sectional study, described in detail by Fagiolini et al. (15) and conducted at nine Italian academic departments (Pisa, Messina, Milan, Modena, Naples, Parma, Rome, Sassari, and Turin). In the full study, four groups of subjects were recruited: inpatients and outpatients with recurrent unipolar depression, inpatients and outpatients with bipolar I disorder (all of whom were currently in treatment in one of the nine departments), gastrointestinal outpatients at these same sites, and university students. Exclusion criteria were age <18 years, substance abuse, and current depressive or manic episodes. Eligible subjects of both genders were assessed initially through a clinical interview, and the resulting diagnoses were subsequently required to be confirmed by the Mini International Neuropsychiatric Interview (16). All subjects were Caucasian and Italian speaking. The patient groups included 117 subjects with recurrent unipolar depression who had recently achieved a partial or complete remission of an index episode of major depression and had no history of hypomanic episodes and 106 subjects with bipolar I disorder who had recently achieved a partial or complete remission of an index episode of major depression or mania. The comparison groups consisted of 139 university students and 114 patients being treated for gastrointestinal problems. To be included in the study, the subjects in the two comparison groups had to be without any current psychiatric diagnosis but could have a lifetime mood disorder. Eight students and nine patients with gastrointestinal problems had experienced a major depressive, manic, or hypomanic episode in the past.
The group size was determined to test, by using analysis of variance (ANOVA) and post hoc pairwise comparisons between groups, the primary study hypotheses (15) that 1) bipolar patients would endorse more manic/hypomanic spectrum items than depressed patients and comparison subjects and 2) unipolar and bipolar patients would endorse more depressive spectrum items than each of the comparison groups at alpha=0.016 and a power of 80%.
The present article reports secondary analyses conducted on the two patient groups. A total of 51% of the bipolar I disorder and 73% of the recurrent unipolar depression groups were women. Mean age in the two groups was, respectively, 43.7 years (SD=12.4) and 48.7 years (SD=13.9).
The ethical committee of the University of Pisa approved the study procedures. All subjects entering the protocol provided written informed consent after receiving a complete description of the study and having the opportunity to ask questions.
Instruments
Structured Clinical Interview for the Spectrum of Mood Disorders
The Structured Clinical Interview for the Spectrum of Mood Disorders was developed simultaneously in English and Italian by capitalizing on the long-standing clinical experience of Italian and American psychiatrists and psychologists, including several of the authors. It consists of 140 items coded as present or absent for one or more periods of at least 3–5 days throughout the subject’s lifetime. For some questions, such as exploring temperamental features or the occurrence of specific events (for instance, suicide attempts), the duration is not specified because it would not be applicable.
Items are organized into manic/hypomanic and depressive components as well as a section that assesses disturbances in rhythmicity and vegetative functions, yielding a total of seven domains. The rhythmicity and vegetative functions domain consists of 23 items, the energy-depressed functions consist of nine items, the energy-manic functions of 12 items, the mood-depressed functions of 22 items, the mood-manic functions of 28 items, the cognition-depressed functions of 26 items, and the cognition-manic functions of 20 items. Symptoms are assessed by groups of statements arranged by increasing severity. For instance, suicidality is explored by questions asking whether the subject has ever experienced periods of 3–5 days or more when he or she 1) felt like life was not worth living, 2) hoped to die, 3) wanted to die, and 4) made suicide plans and two questions asking (5) whether he or she actually made a suicide attempt and (6) whether medical attention was required after the attempt. At the end of each domain, one question probes whether the symptoms explored caused significant impairment. The number of energy-, mood-, and cognition-depressed items endorsed by subjects makes up the “depressive component” (57 items), and the mood-, energy-, and cognition-manic items form the “manic component” (60 items). The structure of the instrument, defined a priori by the investigators on the basis of face validity, was examined by using confirmatory factor analysis, which confirmed the expected structure (P. Rucci, personal communication). The reliability of the interview proved to be excellent (15): the interrater reliability of domains ranged between 0.93 and 0.94, and the internal consistency of domains ranged between 0.79 and 0.92. In terms of discriminant validity, the mood patients had significantly higher total and domain scores than the comparison subjects, and the bipolar patients had significantly higher scores on the manic component than the patients with recurrent depression.
The Mini International Neuropsychiatric Interview
The Mini International Neuropsychiatric Interview is a brief structured interview designed conjointly by American and European psychiatrists to diagnose axis I disorders as well as antisocial personality disorder according to DSM-IV and ICD-10 criteria. For the purposes of this study, we used the three sections of the instrument exploring current or past episodes of major depression, suicidal ideation, and current or past mania or hypomania episodes. The Mini International Neuropsychiatric Interview has been shown to be reliable in multicenter clinical trials and in epidemiological and clinical studies and is administered in a median of 15 minutes (16).
Statistics
The Kolmogorov-Smirnov statistic was used to test the normality of the frequency distributions of the mood scores. Pearson product-moment correlation coefficients were used to analyze the association among continuous variables. Logistic regression models were fit to analyze the relationships between the number of manic/hypomanic symptoms and some indicators of the severity of depression in the recurrent unipolar depression patients and the bipolar I disorder patients. Bonferroni correction to the alpha level (0.05/2=0.025) was performed to adjust for multiple testing in the logistic regression. All statistical analyses were performed with SPSS, version 10.0 (SPSS, Inc., Chicago, 2000).
Results
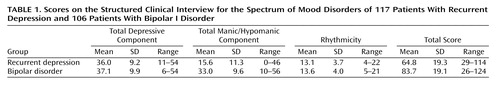
The mean number of mood spectrum items endorsed by the patients with recurrent unipolar depression and the patients with bipolar I disorder was 64.8 and 83.7, respectively (maximum=140) (Table 1). The frequency distribution of the depressive component was essentially overlapping and normal in the recurrent unipolar depression patients and the bipolar I disorder patients, while the frequency distribution of the manic/hypomanic component was normal among the bipolar patients and significantly skewed to the right among the patients with recurrent unipolar depression (Kolmogorov-Smirnov test=1.4, p=0.03).
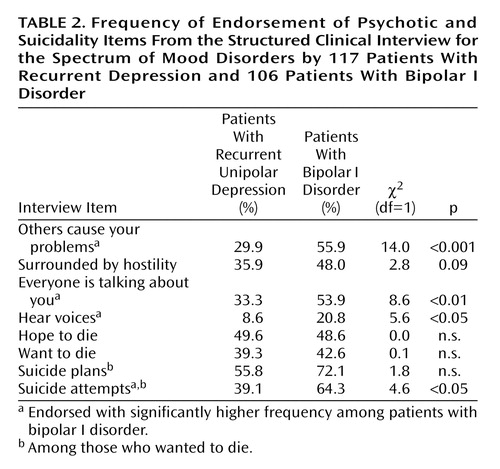
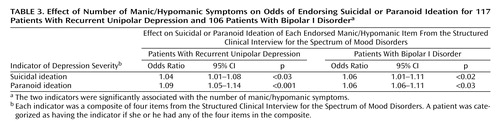
The correlation between lifetime depressive and manic component scores was similar in the bipolar I disorder (r=0.45, p<0.001) and recurrent unipolar depression (r=0.40, p<0.001) patients. An alternative way to show this relationship is to plot the mean depressive and manic component scores versus the depressive-plus-manic score. As the latter increases, the two components increase almost linearly, both in patients with bipolar I disorder and in patients with recurrent unipolar depression (Figure 1). Thus, the number of depressive items endorsed, measured on a continuum, is related to the number of manic/hypomanic items endorsed. To further explore this issue, we selected psychotic and suicidality items as indicators of the severity of depression in the Structured Clinical Interview for the Spectrum of Mood Disorders. Four of these indicators, including paranoid ideation, auditory hallucinations, and suicide attempts, were significantly more common in the lifetime experience of patients with bipolar I disorder than in the patients with recurrent unipolar depression (Table 2). We investigated the relationship between the number of manic/hypomanic items and these indicators of the severity of depression separately in the groups with recurrent unipolar depression and bipolar I disorder by using logistic regression models. To this purpose, we combined the four indicators of suicidality and the four indicators of paranoid ideation into two composite indicators and then dichotomized these indicators as no/any symptom of suicidal ideation and no/any symptom of paranoid ideation.
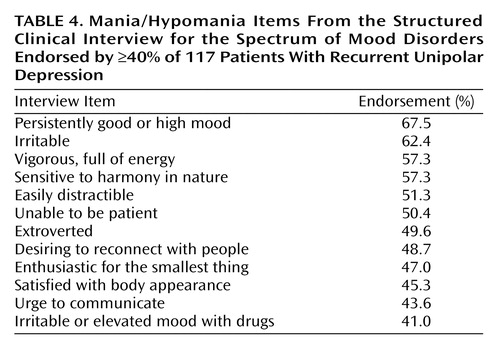
In the group with recurrent unipolar depression, the number of manic/hypomanic items was related to an increased likelihood of paranoid and suicidal ideation (Table 3). For example, we found that for each manic/hypomanic item endorsed, the likelihood of suicidal ideation was increased by 4.2% (odds ratio=1.042, 95% confidence interval 1.006–1.079, p<0.03). This odds ratio corresponds to a 42% increase in risk of suicidal ideation for a 10-item difference in the number of manic/hypomanic symptoms endorsed. Consistent with this result, we found that even the current level of suicidal risk (coded as none, low, moderate, or high in the Mini International Neuropsychiatric Interview) increased significantly with the number of lifetime mania/hypomania items endorsed (ANOVA: F=3.8, df=2, 114, p<0.03). Moreover, an earlier onset of the first depressive episode was significantly correlated with a higher number of manic/hypomanic items (r=–0.32, p<0.01). Neither gender nor the number of depressive episodes was related to the number of manic/hypomanic items endorsed, the number of depressive items endorsed, or the total score on the Structured Clinical Interview for the Spectrum of Mood Disorders. To characterize the profile of manic/hypomanic features endorsed by the patients with recurrent unipolar depression, we summarized the 12 items endorsed with a frequency equal to or higher than 40% by the patients with recurrent unipolar depression (Table 4).
In bipolar I disorder patients, the number of lifetime manic/hypomanic items endorsed was related to the endorsement of lifetime experiences of paranoid ideation and suicidal ideation (Table 3). The number of lifetime depressive episodes was not associated with the number of manic/hypomanic items endorsed, the number of depressive items endorsed, or the total score on the Structured Clinical Interview for the Spectrum of Mood Disorders. Women endorsed more depressive spectrum items than men (mean=39.1, SD=9.9, versus mean=34.9, SD=9.6) (t=2.2, df=100, p<0.05).
Discussion
We investigated the lifetime mood spectrum characteristics of a large group of patients with recurrent unipolar depression or bipolar I disorder by using the Structured Clinical Interview for the Spectrum of Mood Disorders. Symptoms such as paranoid ideation, auditory hallucinations, and suicide attempts were significantly more frequent in bipolar patients than in unipolar patients, which is in line with findings from the literature (17).
Of note, there was a linear relationship between the number of lifetime manic/hypomanic items and the number of depressive items endorsed by both the patients with bipolar I disorder and those with recurrent unipolar depression. In addition, in the patients with recurrent unipolar depression, the more manic/hypomanic items endorsed, the greater the likelihood of reporting suicidal ideation and delusions. This latter result corroborates the observation that the presence of even mild manic symptoms may change a depressive presentation into a mixed presentation and increase the likelihood of psychotic symptoms (18). Our results, indicating that the number and severity of depressive features experienced by any given mood disorder patient are related to the extent of the manic/hypomanic symptom that he or she has experienced in his or her lifetime, are in line with those of Goldberg et al. (19). They also reported that by the 15-year follow-up, 27% of the patients hospitalized for unipolar major depression eventually developed one or more distinct episodes of hypomania, and 19% had at least one episode of mania. They also showed that patients with psychotic depression are more likely than nonpsychotic patients to develop subsequent mania or hypomania at follow-up.
Although psychotic symptoms were more common in the patients with bipolar I disorder, the endorsement of symptoms such as “feeling as if others were causing all of your problems,” “feeling surrounded by hostility,” and auditory hallucinations were related to increasing levels of mania/hypomania both in recurrent unipolar depression patients and in bipolar I disorder patients. In recurrent unipolar depression patients, an earlier onset of illness was associated with a higher frequency of endorsement of manic/hypomanic symptoms, which confirms our expectations based on the present literature (20). Although this latter result seems to foreshadow that among patients with recurrent unipolar depression, an increasing number of manic/hypomanic symptoms correlates with a higher risk of recurrences, we did not find such an association. One explanation for this seemingly paradoxical finding is the range restriction in the number of depressive episodes (median=3) in the study group, resulting from the conservative inclusion criteria we adopted. Indeed, we selected patients with two or more depressive episodes and no hypomanic episodes, therefore excluding patients with single episodes and bipolar II patients. Still, evidence from a study contrasting a large group of patients with pure unipolar depression, hyperthymic unipolar depression, bipolar I disorder, and bipolar II disorder (21) indicates that the number of depressive episodes is not significantly increased in patients with hyperthymic unipolar depression (mean=4.1) versus pure unipolar depression (mean=3.7).
Cumulatively, our empirical findings support a continuous view of the mood spectrum as a unitary phenomenon that is best understood from a longitudinal perspective. Our data suggest that unipolar disorder and bipolar disorder are not two discrete and dichotomous phenomena but that mood fluctuations—up and down—are common to both conditions, as emphasized by Koukopoulos et al. (22). Indeed Swann (23), espousing the parsimonious Kraepelinian view, conceptualized recurrent affective disorders as one illness in which the apparently different bipolar and unipolar course may be determined by increased sensitization after the occurrence of a manic episode. Using a different term, Ghaemi et al. (7) proposed a view of the “affective spectrum” that spans the single depressive episode and bipolar I disorder to accommodate nonclassical parts of the bipolar spectrum, such as type II, not otherwise specified, and cyclothymia.
The implications of a unitary approach to mood disorders are not only nosographic. We believe that clinical attention should be paid to sporadic manic/hypomanic manifestations in treatment planning and the prognosis of recurrent unipolar depression. Our data suggest that manic/hypomanic features, as Judd and Akiskal (24) have argued, are not “benign” because they are associated with increased lifetime and current suicidality. Our findings are in line with the results of their recent reanalysis of Epidemiologic Catchment Area data that also emphasize how even subsyndromal manic symptoms are associated with increased service use for mental health problems and the need for welfare and disability benefits. However, it must be acknowledged that only a long-term prospective follow-up study of patients assessed with the Structured Clinical Interview for the Spectrum of Mood Disorders early in their course of illness could confirm the utility of this kind of evaluation.
The present study has a number of limitations. First, the Structured Clinical Interview for the Spectrum of Mood Disorders does not provide information on the frequency of occurrence of individual symptoms but only inquires whether symptoms did or did not occur for a period of at least 3–5 days in the subject’s lifetime. Thus, the relationship we found between the number of manic/hypomanic and depressive items does not imply anything about the co-occurrence or sequence of these experiences. Also, given that the instrument assesses symptoms and behaviors retrospectively, there might be a recall bias. In this article, we assumed that the bias does not differentially affect the recall of manic/hypomanic and depressive spectrum features. Finally, caution should be used in interpreting the results because of their preliminary nature. Further analyses conducted on separate samples since the submission of this article confirmed all of the findings we report here.
Conclusions
We agree with Akiskal and Pinto (14) that a true understanding of the continuum between unipolarity and bipolarity should be grounded on clinical observation. On the other hand, we argue that clinical observation should be structured into an instrument with sound psychometric properties, allowing for comparison between individuals and across groups. The Structured Clinical Interview for the Spectrum of Mood Disorders seems to be promising for such purposes because it provides clinicians with a conceptual frame of reference and operational criteria for diagnosing mood spectrum psychopathology and for testing research hypotheses in the context of an instrument with good psychometric properties. With this spectrum assessment, we showed that the presence of a significant number of manic/hypomanic items in patients with recurrent unipolar depression seems to challenge the traditional dichotomy of unipolar-bipolar disorder and bridges the gap between these two categories of mood disorders. Long-term prospective follow-up studies of patients assessed with the Structured Clinical Interview for the Spectrum of Mood Disorders early in their course of illness are warranted to confirm the utility of this kind of evaluation.
 |
 |
 |
 |
Received April 3, 2002; revision received Feb. 4, 2003; accepted Nov. 7, 2003. From the Department of Psychiatry, Neurobiology, Pharmacology, and Biotechnology, University of Pisa; and the Department of Psychiatry, Western Psychiatric Institute and Clinic, University of Pittsburgh, Pittsburgh. Address reprint requests to Dr. Cassano, Department of Psychiatry, Neurobiology, Pharmacology, and Biotechnology, University of Pisa, Via Roma n.67, 56100, Pisa, Italy; [email protected] (e-mail).
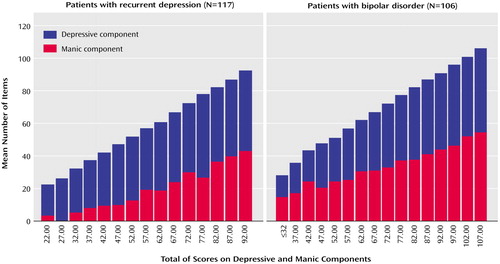
Figure 1. Relation of Scores on the Depressive and Manic Components of the Structured Clinical Interview for the Spectrum of Mood Disorders to the Combined Depressive-Plus-Manic Score for 117 Patients With Recurrent Unipolar Depression and 106 Patients With Bipolar I Disorder
1. Keller MB, Lavori PW, Rice J, Coryell W, Hirschfeld RMA: The persistent risk of chronicity in recurrent episodes of nonbipolar major depressive disorder: a prospective follow-up. Am J Psychiatry 1986; 143:24–48Link, Google Scholar
2. Judd LL: Major depressive disorder: longitudinal symptomatic structure, relapse and recovery. Acta Psychiatr Scand 2001; 104:81–83Crossref, Medline, Google Scholar
3. Judd LL, Akiskal HS, Schettler PJ, Coryell W, Endicott J, Maser JD, Solomon DA, Leon AC, Keller MB: A prospective investigation of the natural history of the long-term weekly symptomatic status of bipolar II disorder. Arch Gen Psychiatry 2003; 60:261–269Crossref, Medline, Google Scholar
4. Judd LL, Akiskal HS, Schettler PJ, Endicott J, Maser JD, Solomon DA, Leon AC, Rice JA, Keller MB: The long-term natural history of the weekly symptomatic status of bipolar I disorder. Arch Gen Psychiatry 2002; 59:530–537Crossref, Medline, Google Scholar
5. Solomon DA, Keller MB, Leon AC, Mueller TI, Lavori PW, Shea MT, Coryell W, Warshaw M, Turvey C, Maser JD, Endicott J: Multiple recurrences of major depressive disorder. Am J Psychiatry 2000; 157:229–233Link, Google Scholar
6. Ghaemi SN, Sachs GS, Chiou AM, Pandurangi AK, Goodwin FK: Is bipolar disorder still underdiagnosed? are antidepressants overutilized? J Affect Disord 1999; 52:135–144Crossref, Medline, Google Scholar
7. Ghaemi SN, Ko JY, Goodwin FK: The bipolar spectrum and the antidepressant view of the world. J Psychiatr Practice 2001; 7:287–297Crossref, Medline, Google Scholar
8. Blacker D, Tsuang MT: Contested boundaries of bipolar disorder and the limits of categorical diagnosis in psychiatry. Am J Psychiatry 1992; 149:1473–1483Link, Google Scholar
9. Kendler KS, Gardner CO Jr: Boundaries of major depression: an evaluation of DSM-IV criteria. Am J Psychiatry 1998; 155:172–177Abstract, Google Scholar
10. Angst J: The emerging epidemiology of hypomania and bipolar II disorder. J Affect Disord 1998; 50:143–151Crossref, Medline, Google Scholar
11. Duffy A, Grof P, Robertson C, Alda M: The implications of genetic studies of major mood disorders in clinical practice. J Clin Psychiatry 2000; 61:630–637Crossref, Medline, Google Scholar
12. McGuffin P, Katz R: The genetics of depression and manic-depressive disorder. Br J Psychiatry 1989; 155:294–304Crossref, Medline, Google Scholar
13. Widiger TA, Frances AJ, Pincus HA (eds): DSM-IV Sourcebook. Washington, DC, American Psychiatric Association, 1995Google Scholar
14. Akiskal HS, Pinto O: The soft bipolar spectrum: footnotes to Kraepelin on the interface of hypomania, temperament and depression, in Bipolar Disorders. Edited by Marneros A, Angst J. Dordrecht, the Netherlands, Kluwer Academic, 2000, pp 37–62Google Scholar
15. Fagiolini A, Dell’Osso L, Pini S, Armani A, Bouanani S, Rucci P, Cassano GB, Endicott J, Maser JD, Shear MK, Grochocinski VJ, Frank E: Validity and reliability of a new instrument for assessing mood symptomatology: the Structured Clinical Interview for Mood Spectrum (SCI-MOODS). Int J Methods Psychiatr Res 1999; 8:71–82Crossref, Google Scholar
16. Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC: The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998; 59(suppl 20):22–33Google Scholar
17. Mitchell PB, Wilhelm K, Parker G, Austin MP, Rutgers P, Malhi GS: The clinical features of bipolar depression: a comparison with matched major depressive disorder patients. J Clin Psychiatry 2001; 62:212–216Crossref, Medline, Google Scholar
18. Dell’Osso L, Placidi GF, Nassi R, Freer P, Cassano GB, Akiskal HS: The manic-depressive mixed state: familial, temperamental and psychopathologic characteristics in 108 female inpatients. Eur Arch Psychiatry Clin Neurosci 1991; 240:234–239Crossref, Medline, Google Scholar
19. Goldberg JF, Harrow M, Whiteside JE: Risk for bipolar illness in patients initially hospitalized for unipolar depression. Am J Psychiatry 2001; 158:1265–1270Link, Google Scholar
20. Akiskal HS, Maser JD, Zeller PJ, Endicott J, Coryell W, Keller M, Warshaw M, Clayton P, Goodwin FK: Switching from “unipolar” to bipolar II: an 11-year prospective study of clinical and temperamental predictors in 559 patients. Arch Gen Psychiatry 1995; 52:114–123Crossref, Medline, Google Scholar
21. Cassano GB, Akiskal HS, Savino M, Musetti L, Perugi G: Proposed subtypes of bipolar II and related disorders: with hypomanic episodes (or cyclothymia) and with hyperthymic temperament. J Affect Disord 1992; 26:127–140Crossref, Medline, Google Scholar
22. Koukopoulos A, Sani G, Koukopoulos AE, Girardi P: Cyclicity and manic depressive illness, in Bipolar Disorders. Edited by Marneros A, Angst J. Dordrecht, the Netherlands, Kluwer Academic, 2000, pp 315–334Google Scholar
23. Swann AC: “A two-illness model of bipolar disorder”—RT Joffe, LT Joung, and GM McQueen: a commentary. Bipolar Disord 1999; 1:38–41Crossref, Medline, Google Scholar
24. Judd LL, Akiskal HS: The prevalence and disability of bipolar spectrum disorders in the US population: reanalysis of the ECA database taking into account subthreshold cases. J Affect Disord 2003; 73:123–131Crossref, Medline, Google Scholar



