Increased Positive Versus Negative Affective Perception and Memory in Healthy Volunteers Following Selective Serotonin and Norepinephrine Reuptake Inhibition
Abstract
OBJECTIVE: Antidepressants that inhibit the reuptake of serotonin (SSRIs) or norepinephrine (SNRIs) are effective in the treatment of disorders such as depression and anxiety. Cognitive psychological theories emphasize the importance of correcting negative biases of information processing in the nonpharmacological treatment of these disorders, but it is not known whether antidepressant drugs can directly modulate the neural processing of affective information. The present study therefore assessed the actions of repeated antidepressant administration on perception and memory for positive and negative emotional information in healthy volunteers. METHOD: Forty-two male and female volunteers were randomly assigned to 7 days of double-blind intervention with the SSRI citalopram (20 mg/day), the SNRI reboxetine (8 mg/day), or placebo. On the final day, facial expression recognition, emotion-potentiated startle response, and memory for affect-laden words were assessed. Questionnaires monitoring mood, hostility, and anxiety were given before and after treatment. RESULTS: In the facial expression recognition task, citalopram and reboxetine reduced the identification of the negative facial expressions of anger and fear. Citalopram also abolished the increased startle response found in the context of negative affective images. Both antidepressants increased the relative recall of positive (versus negative) emotional material. These changes in emotional processing occurred in the absence of significant differences in ratings of mood and anxiety. However, reboxetine decreased subjective ratings of hostility and elevated energy. CONCLUSIONS: Short-term administration of two different antidepressant types had similar effects on emotion-related tasks in healthy volunteers, reducing the processing of negative relative to positive emotional material. Such effects of antidepressants may ameliorate the negative biases in information processing that characterize mood and anxiety disorders. They also suggest a mechanism of action potentially compatible with cognitive theories of anxiety and depression.
Antidepressants that potentiate serotonin (5-HT) or norepinephrine neurotransmission are effective in the treatment of major depression and anxiety (1, 2). While the pharmacological and cellular actions of antidepressants are well characterized, there is little understanding of how such effects act to improve the symptoms of low mood, anxiety, and social dysfunction that define the disorders they treat. In fact, there is a growing tendency to emphasize secondary cellular effects outside the domain of the classical monoamine transmitters in trying to understand antidepressant drug action. By contrast, there has been much less attention to the actions of antidepressant drugs at a systems level, specifically on the emotion-related functions of neural systems believed to play a role in anxiety and depression.
Psychological approaches to depression have emphasized the role of negative biases in information processing in the maintenance of this disorder (3). Mood-congruent biases in the recall of emotionally valenced information in incidental memory tasks (4) and in the monitoring and classification of emotional information (5, 6) have been reported to occur in depression. In a previous study, depressed patients were also more likely to classify ambiguous facial expressions as negative, and this tendency predicted subsequent relapse (7). Similarly, anxiety has been associated with both preattentive and conscious biases toward threatening stimuli (8, 9). The translation of these negative biases of perception, attention, and memory into conscious thoughts, memories, and actions is believed to play a key role in maintaining symptoms of these disorders. Such negative cognitions are an important target for treatment in cognitive behavior therapy for depression and anxiety (10).
Antidepressant drug treatment or recovery from depression appears to reduce the excessive processing of negative emotional material (7, 9, 11). However, it is unclear whether this represents a direct action of the treatment or an indirect, and nonspecific, consequence of symptom improvement. Investigating antidepressant drug effects on key psychological processes in healthy volunteers allows us to elucidate the direct actions of antidepressants unconfounded by symptom remission or significant mood improvement. The current investigation therefore compared the effects of 7 days administration of the selective serotonin reuptake inhibitor (SSRI) citalopram, the selective norepinephrine reuptake inhibitor (SNRI) reboxetine, or placebo on the processing of emotional material in healthy volunteers. A battery of tasks was given to assess different aspects of cognitive function relevant to both depression and anxiety: these included emotional categorization, emotional memory, facial expression perception, and emotion-potentiated startle response. It was predicted that both antidepressants would lead to a similar enhancement of positive versus negative processing in tasks measuring categorization, memory, and interpretation of emotional or social information. However, given the wider usage of SSRIs in anxiety disorders (1), citalopram was predicted to have greater impact on reactivity to threat-relevant stimuli, especially in the emotion-potentiated startle task, which is based on a well-validated animal model of anxiety (12). Specific hypotheses relating to each task are detailed in the Method section.
Method
Volunteers and Design
Forty-two volunteers (21 men and 21 women) provided written informed consent to the study, which was approved by the local ethics committee. From assessment with the Structured Clinical Interview for DSM-IV, the subjects were determined to be free of either current or past axis I disorder (including anxiety disorders, depression, eating disorders, psychosis, and substance abuse). They had no current physical illness and had been free of medication for at least 3 months. The premenstrual week was avoided for the study period in female volunteers.
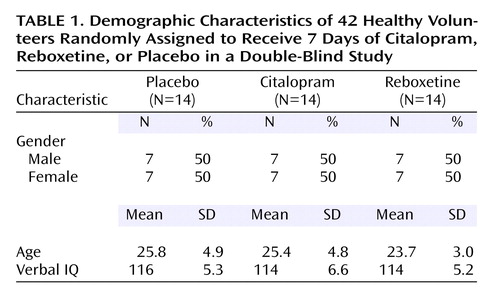
Subjects were randomly allocated to double-blind intervention with one of the three following oral treatments for a period of 7 days: placebo, citalopram (20 mg/day), or reboxetine (4 mg b.i.d.). Medication was given in identical capsules twice daily to maintain blinding. The three groups were matched in terms of gender, verbal IQ (assessed with the National Adult Reading Test), and age (Table 1).
Subjective state was recorded every day throughout treatment using the Befindlichkeits scale of mood and energy to provide a sensitive measure of day-by-day variation in mood (13). The following questionnaires were given before and on the seventh day of intervention: State-Trait Anxiety Inventory (14), Buss-Durkee Hostility Inventory (15), Beck Depression Inventory (16), Positive and Negative Affect Schedule (17), and Social Adaptation Self-Evaluation Scale (18).
Administration of a battery of tests commenced at 12:00 noon on the seventh day of intervention.
Facial Expression Recognition
Stimuli
The facial expression recognition task featured six basic emotions (happiness, surprise, sadness, fear, anger, and disgust) taken from the Pictures of Affect Series (19), which had been morphed between each prototype and neutral (20). Briefly, this procedure involved taking a variable percentage of the shape and texture differences between the two standard images 0% (neutral) and 100% (full emotion) in 10% steps. Four examples of each emotion at each intensity were given (total of 10 individuals). Each face was also given in a neutral expression, giving a total of 250 stimuli presentations.
Procedure
The facial stimuli were presented on a computer screen (random order) for 500 msec and replaced by a blank screen. Volunteers made their responses by pressing a labeled key on the keyboard. Each participant was asked to respond as quickly and as accurately as possible.
Accuracy (number correct out of 40), reaction time for correct choices, and misclassifications (number of responses to each facial expression category classified as each of the other facial expression categories) were recorded in this task. Negative biases in the interpretation of social signals, such as facial expressions, have been reported to occur in depression and are thought to be important in relapse and maintenance of this disorder (7). We have suggested that antidepressants directly modulate the neural processing of this kind of social/emotional information as part of their therapeutic action. Therefore, in this task it was hypothesized that antidepressant administration would decrease the perception of negative facial expressions (particularly disgust, anger, and fear) while increasing the perception of the positive facial expressions of happiness in healthy volunteers.
Emotional Categorization Task
Sixty personality characteristics selected to be extremely disagreeable (e.g., domineering, untidy, hostile) or agreeable (cheerful, honest, optimistic) (taken from Anderson [21]) were presented on the computer screen for 500 msec. These words were matched in terms of word length and ratings of frequency and meaningfulness. Volunteers were asked to categorize these personality traits as likable or dislikable as quickly and as accurately as possible. Specifically, they were asked to imagine whether they would be pleased or upset if they overheard someone else referring to them as possessing this characteristic, so that the judgment was in part self-referring. Classifications and reaction times for correct identifications were computed for this task. In line with the suggestion that antidepressants may work by decreasing negative biases in depression, it was predicted that both antidepressants would decrease the reaction time to identify positive compared with negative characteristics in this task.
Emotional Memory
Immediately after completion of the emotional categorization task, volunteers were asked to recall as many of the personality traits as possible. This task therefore allowed the assessment of incidental memory for positive and negative characteristics. It was hypothesized that both antidepressants would increase the relative recall of the positive relative to the negative stimuli.
Emotion-Potentiated Startle Response
Stimuli
Picture stimuli from the International Affective Picture System (22) were used, which were designed to elicit positive, negative, or neutral emotions (stimuli set taken from Larson et al. [23]). These stimuli had been rated and selected such that the negative and positive pictures were similar in terms of arousal but opposite in valence, whereas the neutral pictures were low on arousal and average on valence. Stimuli were presented for 13 seconds (intertrial interval: mean=13 seconds, range=11–15) on a 43-cm computer screen approximately 1 m away from the volunteer. Pictures were presented in three blocks each containing seven pictures of each category in a fixed random order with the constraint that no two of the same type (neutral, positive, or negative) were presented successively.
Procedure and recording
The eye-blink component of the startle response was recorded from the orbicularis oculi using electromyography (EMG startle response system, San Diego Instruments, Inc., San Diego). Acoustic probes were 50-msec, 95-dB bursts of white noise with a nearly instantaneous rise time and were delivered binaurally through headphones (generated through the noise generator and amplifier component of the EMG startle response system, San Diego Instruments). Probes were delivered at 1.5, 4.5, or 7.5 seconds following picture onset. Within each block of 21 pictures, probes were delivered during five of each trial type (neutral, positive, or negative). To limit expectation of the noise, two trials per valence did not contain any startle probes, and three probes per block were given within the intertrial interval. To habituate volunteers to the startle probes and to orient them to the procedure, volunteers viewed an introductory set of nine neutral pictures and received nine startle probes (two of these within the intertrial interval).
EMG signals were filtered (low cutoff: 0.5 Hz; high cutoff: 100 Hz) and rectified. Eye-blink reflex magnitudes in μV were calculated by subtracting the amount of integrated EMG at reflex onset from the peak amplitude maximum amount of integrated EMG between 20 and 120 msec following probe onset. Trials with no perceptible eye-blink reflex were assigned a magnitude of zero and included in the analysis. Eye-blink reflexes with excessive noise during a 20-msec, prestartle baseline period were excluded. Of the 42 volunteers, nine volunteers were not included in the analysis because of equipment failure (N=2), electrode interference (N=3), or because they displayed fewer than 25% satisfactory blink responses in the paradigm (N=4). This task provides a measure of the relative acoustic startle response during unpleasant, pleasant, and neutral pictorial stimuli presentation. Therefore, eye-blink reflex magnitudes were z-transformed within subjects to allow comparison between these different conditions and minimize intersubject variability that was often due to small differences in electrode placement or impedance.
The enhanced acoustic startle response observed during a state of fear in rodents is used to assess anxiolytic properties of pharmacological treatments (24). Given the therapeutic effects of citalopram in anxiety disorders as well as depression it was predicted that this SSRI would specifically reduce the priming effects of the negative pictures on acoustic startle in this task (i.e., the heightened startle found to the white noise when volunteers are viewing the unpleasant relative to neutral pictures). There is little published on the effects of SNRIs in such paradigms.
Statistics
Data were analyzed by using between-group one-way (emotional memory, subjective state) or split-plot two-way (facial expression recognition, emotion-potentiated startle response, reaction time) analyses of variance (ANOVAs). For the two-way ANOVAs, group (citalopram, reboxetine, or placebo) was the between-subject factor, and emotion or stage was the within-subject factor. Significant interactions were followed up by using two-way ANOVAs with each antidepressant relative to placebo and completed using simple main effect analyses.
Results
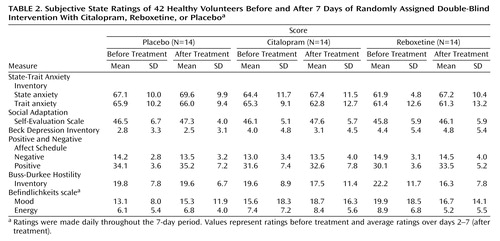
Subjective Mood, Anxiety, and Hostility
Neither citalopram nor reboxetine significantly affected ratings of positive or negative affect on the Positive and Negative Affect Schedule, depression on the Beck Depression Inventory, trait and state anxiety, or self-evaluation of social adaptation (p>0.50 for all comparisons) (Table 2). However, antidepressant administration tended to affect hostility ratings on the Buss-Durkee inventory (one way analysis of variance F=3.0, df=2, 39, p=0.06). Significant group-by-time interactions relative to placebo were seen for reboxetine (F=4.9, df=1, 26, p=0.04) but not citalopram (F=1.3, df=1, 26, p=0.30). Reboxetine also decreased scores on the Befindlichkeits scale relative to the other two groups (group-by-time interaction: F=4.5, df=2, 39, p=0.02), apparently the result of endorsing fewer descriptions of low energy (group-by-time: F=3.4, df=2, 39, p=0.04) rather than of low mood (group-by-time: F=1.9, df=2, 39, p=0.20).
Facial Expression Recognition
Accuracy
Performance in the facial expression recognition task was significantly affected by intervention group (overall group-by-facial expression interaction: F=1.9, df=6, 234, p=0.03) (Figure 1). The two-way analyses of variance comparing each antidepressant to the placebo group revealed a significant group-by-emotion interaction for both citalopram (F=3.0, df=6, 156, p=0.008) and reboxetine (F=2.5, df=6, 156, p=0.03). In particular, both antidepressants decreased the recognition of fearful (citalopram: t=2.8, df=26, p=0.008; reboxetine: t=3.5, df=26, p=0.002) and angry (citalopram: t=2.0, df=26, p=0.055; reboxetine: t=2.1, df=26, p=0.04) facial expressions relative to placebo. Citalopram additionally decreased the facial expression recognition of disgust (t=3.5, df=26, p=0.002) and surprise (t=3.0, df=26, p=0.006). None of the other comparisons attained statistical significance for either citalopram or reboxetine (all comparisons p>0.20).
When disgust or anger were misclassified, they tended to be mistaken for each other, but this tendency was not exaggerated in those receiving citalopram or reboxetine. The mean percentages of responses to disgusted facial expressions labeled as anger were 12% (SD=3%), 10% (SD=2%), and 10% (SD=3%) following citalopram, reboxetine, and placebo, respectively (F=0.3, df=2, 39, p=0.80). The respective mean percentages of responses to angry facial expressions labeled as disgust were 7% (SD=2%), 4% (SD=1%), and 7% (SD=2%) (F=1.3, df=2, 39, p=0.30). However, misclassifications of fear as surprise were more common in groups receiving citalopram (mean=17%, SD=3%) or reboxetine (mean=17%, SD=2%) than placebo (mean=8%, SD=1%) (citalopram versus placebo: t=2.7, df=26, p=0.01; reboxetine versus placebo: t=3.3, df=26, p=0.003). The volunteers who received citalopram were also more likely than the placebo group to misclassify all three of these negative emotions as happy, suggesting a positive bias in facial expression recognition: the mean values of the citalopram, reboxetine, and placebo groups were 8% (SD=2%), 2% (SD=1%), and 3% (SD=1%) for disgust (t=2.2, df=26, p=0.03); 5% (SD=1%), 3% (SD=1%), and 2% (SD=1%) for fear (t=2.0, df=26, p=0.06); and 3% (SD=1%), 1% (SD=1%), and 1% (SD=1%) for anger (t=2.0, df=26, p=0.06).
Reaction time
There were no differences between the three groups in terms of speed of correct responses (group-by-emotion: F=0.9, df=6, 234, p=0.40; main effect of group: F=1.1, df=2, 39, p=0.40), which suggests the absence of sedation in the antidepressant groups.
Emotional Categorization
The difference in reaction time to classify positive and negative personality characteristics was significantly affected by group (F=3.2, df=2, 39, p=0.05) (Figure 2). In particular, reboxetine-treated volunteers were relatively quicker to classify positive versus negative personality characteristics compared with the placebo-treated volunteers (t=3.1, df=26, p=0.005). A similar, but nonsignificant, tendency was seen in volunteers receiving citalopram compared with those receiving placebo (t=1.5, df=26, p=0.10).
Emotional Memory
The total number of words recalled did not differ significantly between the three groups (F=0.2, df=2, 39, p=0.90). However, the percentage of these words that were positive was higher in both the antidepressant groups relative to placebo (one-way ANOVA F=3.5, df=2, 39, p=0.04) (Figure 2).
Emotion-Potentiated Startle Response
Both the reboxetine and placebo group showed potentiation of eye blink with the negatively valenced pictures (main effect of stimulus type: F=3.7, df=2, 20, p=0.04; F=5.7, df=2, 18, p=0.01, respectively). By contrast, this potentiation of the startle response by negative pictures was abolished in the volunteers receiving citalopram (interaction between emotional stimulus and group: F=2.7, df=4, 60, p=0.04) (Figure 3). This is unlikely to be the consequence of reduced blinking or reactivity per se, since untransformed eye blinks during the neutral stimuli were similar across the three groups (F=1.7, df=2, 30, p>0.20).
Discussion
Overall, these results show that antidepressants modulate the perception and memory for negative versus positive emotional material in healthy volunteers with no current or previous history of mood or anxiety disorder. In particular, the two different types of antidepressant increased the relative processing of positive to negative affective information in a manner directly opposite to the negative biases previously described in depression (10). Both reboxetine and citalopram increased memory for positively valenced emotional material and decreased the perception of fear and anger from facial expression cues. Citalopram additionally decreased emotion-potentiated startle response and produced a wider profile of action in the facial expression recognition task compared with reboxetine. Such effects may be important in the therapeutic actions of antidepressant drugs in anxiety as well as depression.
Modulation of the Processing of Positive Material Following Antidepressant Administration
Cognitive studies suggest that depressed patients show increased attention and memory to stimuli when they are unpleasant or aversive in valence (e.g., references 3–7). These biases are believed to play a key role in maintaining the symptoms of anhedonia, low mood, guilt, and decreased self-esteem that are defining features of depression. Our tasks of self-referent classification and memory for positive and negative personality characteristics were also designed to draw upon these cognitive functions. Both citalopram and reboxetine facilitated incidental memory for positive self-referent social information compared with the placebo group, and reboxetine also significantly increased the speed of classification for positive characteristics. These changes in categorization and memory for positive social information, independent of changes in subjective mood, suggest that antidepressants can directly modulate the neural processing of emotional material. If such changes occur following antidepressant drug treatment in depressed patients, they may help remediate negative biases in attention and memory to social stimuli and provide an important therapeutic mechanism in the response to these agents. However, these changes in emotional processing occurred following just 7 days of antidepressant administration in the current study—earlier than the full therapeutic effects actually occur (1). It is therefore possible that changes in psychological function precede (and ultimately contribute to) the development of improved mood over time as the patient learns to evaluate and respond to “new” social input and memories. Indeed, we have recently found that a single dose of reboxetine (4 mg) is sufficient to facilitate positive emotional classification and memory in healthy volunteers (25). Future studies are required to evaluate whether these effects on emotional processing accrue over longer-term (e.g., 6 weeks) administration of antidepressants.
Although acute administration of both reboxetine and citalopram in previous studies were observed to increase the recognition of happy facial expressions (25, 26), there was only a tendency for a similar facilitation here following 7 days administration. However, the misclassification of ambiguous (difficult to classify) expressions suggested a significant bias toward positive facial expressions in the subjects receiving the antidepressants. Volunteers receiving citalopram were more likely to mislabel negative facial expressions as happy, and both groups tended to mistake fear for the more positive emotion of surprise. Therefore, it is possible that specific increases in the perception of happiness, which were previously reported to occur with single doses of antidepressants, become more generalized with longer-term administration of these drugs.
Fear Processing and the Actions of SSRIs
In addition to the effects on affective processing relevant to mood-congruent biases in depression, we predicted that the SSRI citalopram would reduce responses to threat-relevant stimuli in line with therapeutic indications in anxiety. Findings from two different paradigms used here, facial expression recognition and emotion-potentiated startle response, confirmed this prediction. Volunteers receiving citalopram for 7 days showed reduced startle responses to threatening pictures in the emotion-potentiated startle task and decreased interpretation of threatening facial expressions of anger, disgust, and fear. These findings are of interest given the anxiolytic actions of SSRIs in a range of anxiety disorders, including generalized anxiety, social phobia, panic, and obsessive-compulsive disorder (1). We suggest that this human equivalent of the rodent fear potentiated startle paradigm is a sensitive measure of anxiolytic action.
The effects of citalopram on the processing of fear are consistent with a role for the amygdala in SSRI action. The amygdala plays a primary role in the enhanced startle response during fear, largely characterized in animal models (12) but supported by studies of patients with amygdala damage (27). The processing of fear cues from facial expressions has also been associated with the amygdala by functional neuroimaging (28) and neuropsychological case studies (29). A role for the amygdala in the actions of SSRIs is also supported by the results of a recent fMRI study in depressed patients that showed hyperarousal of the amygdala in response to nonconscious presentation of fearful facial expressions (11). Following treatment with SSRIs, this response was normalized, suggesting that antidepressant treatment may have acted to constrain amygdala overactivity (11). However, this study did not use a placebo control, so symptom remission or repeated testing could also explain the finding. The current results support the more interesting hypothesis that SSRIs directly modulate amygdala-dependent processing, normalizing excessive activation in depression and anxiety (reviewed by Whalen et al. [30] and Drevets [31]), and reducing reactivity to negatively valenced emotional stimuli in humans.
In contrast with the present findings with repeated dosing, we have previously found that acute administration of the SSRI citalopram increased the recognition of fearful facial expressions of emotion (26). This increased fear perception is in line with the clinical observation that SSRIs often increase anxiety before therapeutic effects are seen (1) and preclinical studies identifying acute anxiogenic actions of SSRI administration given systemically or directly into the amygdala (32). This effect does not appear to be the result of a paradoxical acute decrease in serotonin function due to 5-HT1A autoreceptor activation (33), since acute serotonin depletion was found to produce the opposite pattern in the facial expression recognition task, leading to a decrease in fear perception in healthy female volunteers (34). At present, the mechanism underlying this reversal of action from acute to subchronic administration of SSRIs is unknown but is clearly of critical importance to our understanding of any delay in antidepressant efficacy. The models of fear processing used here may therefore be useful in future studies exploring this elusive mechanism in humans.
Does Citalopram Have a Broader Spectrum of Action on Fear-Related Processing Than Reboxetine?
Like the SSRI, the selective noradrenergic antidepressant reboxetine decreased the recognition of fearful and angry facial expressions. However, it did not affect emotion-potentiated startle response and produced more specific impairments in the facial expression recognition task. It is of interest that reboxetine affected the perception of fearful facial expressions but not the emotional modulation of response to acoustic startle, although these have been postulated to be dependent on similar neurobiological substrates such as the amygdala. Differential sensitivity levels of these two tasks to small changes in amygdala function may explain this apparent effect. Alternatively, the difference may lie in the type of fear processing/labeling measured by the two tasks. In particular, while the facial expression recognition task requires the interpretation and categorization of emotional stimuli, the emotion-potentiated startle response relies on the priming effects of emotional stimuli on an eye-blink reflex. This difference may be relevant to dissociations of cognitive function reported in patients with depression relative to anxiety. For example, while depression has been suggested to reflect increased elaborative or interpretative processing of threatening stimuli, anxiety has been additionally associated with nonconscious bias (6). It is therefore tempting to speculate that while the facial expression recognition task measures the interpretation of threat (potentially relevant to both depression and anxiety), the emotional modulation of startle reflexes may be more dependent on nonconscious reactivity to these stimuli (more relevant to anxiety). In this case, the dissociation between citalopram (affecting both emotion-potentiated startle response and fear recognition) and reboxetine (affecting only fear recognition) would be consistent with their differential therapeutic indications in anxiety disorders. Further studies using functional neuroimaging are currently in progress to assess more directly the neural basis of these differences.
Subjective State
The current changes in processing and memory for emotional material following antidepressant administration occurred in the absence of significant subjective changes in positive and negative mood, anxiety, and well being. The tasks could therefore be studied in the absence of the changes that confound clinical observation and appear to be more sensitive than subjective mood to modulation of neural systems involved in emotion. However, there were measurable changes in subjective experience. Volunteers receiving reboxetine rated themselves as less hostile relative to placebo-treated volunteers, although the similar but smaller reduction following citalopram was nonsignificant. Knutson et al. (35) also reported a reduction in assaultiveness on the Buss-Durkee inventory following intervention with the SSRI paroxetine. These results therefore confirm that antidepressants may reduce hostility measures in healthy volunteers and extend this action to a noradrenergic antidepressant. Reboxetine also improved self-rated energy on the Befindlichkeits scale, with volunteers tending to endorse more positive descriptions of their current state of energy or motivation, such as being refreshed rather than exhausted or alert rather than listless. None of these changes correlated with measures of emotional processing, but they may also contribute, of course, to antidepressant action.
Implications for Antidepressant Drug Action in Depression and Anxiety
Negative biases in information processing in depression and anxiety are the explicit target for psychological treatments such as cognitive behavior therapy (3). The actions of antidepressant treatment are not usually explored in a psychological framework, and reductions of biases toward threat or aversive information following treatment with antidepressants are often attributed to mood improvement. However, the current results show that antidepressants change emotional processing and memory even in the absence of a measurable change in subjective mood. In particular, both reboxetine and citalopram increased positive emotional processing, which may be expected to help redress negative processing of social and emotional information in depression. As such, the tasks described here may be useful human experimental models that could be used alongside animal models, such as fear-potentiated startle response, to enhance our understanding of how antidepressant and anxiolytic drugs are working.
Conclusions
Results from the current study suggest that two different antidepressants, putatively acting via different neurochemical mechanisms, both reduce the processing of negative emotional material and increase memory for positively valenced items in healthy nondepressed volunteers. Such actions of antidepressants may act to reverse the pervasive negative biases in memory and information processing that are apparent during periods of clinical anxiety and depression. Such a mechanism could be the necessary and sufficient action required for treatment effect. Further studies will be needed in patient groups to explore how changes in emotional processing through pharmacological treatment relate to alterations in subjective experience and clinical state. In addition, the use of brain imaging will allow in vivo assessment of the role of the amygdala in the effects of antidepressant drugs on emotional processing. Finally, but most importantly, we have a new message for patients who may be asked to accept long-term treatment with antidepressant medicines: these agents influence human psychology in an understandable way, and one that plausibly complements the mechanism of action of psychological treatments.
 |
 |
Received April 28, 2003; revision received Oct. 8, 2003; accepted Oct. 31, 2003. From the University Department of Psychiatry, Warneford Hospital. Address reprint requests to Dr. Harmer, University Department of Psychiatry, Warneford Hospital, Oxford, OX3 7JX, United Kingdom.
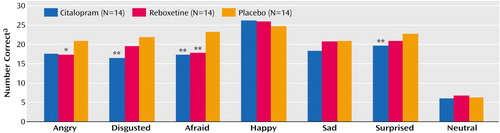
Figure 1. Facial Expression Recognition Performance of 42 Healthy Volunteers After 1 Week of Randomly Assigned Double-Blind Intervention With Citalopram, Reboxetine, or Placebo
aOut of 40 for each emotion, 10 for neutral. Asterisks depict significance level of difference from placebo.
*p<0.05. **p<0.01.
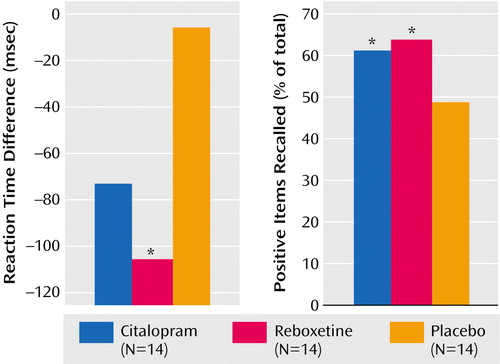
Figure 2. Reaction Time for Classifying Positive Versus Negative Personality Characteristics and Recall of Positive Personality Characteristics as a Percent of Total Correct Words Recalled in 42 Healthy Volunteers After 1 Week of Randomly Assigned Double-Blind Intervention With Citalopram, Reboxetine, or Placeboa
aAsterisks depict significance level of difference from placebo.
*p<0.05.
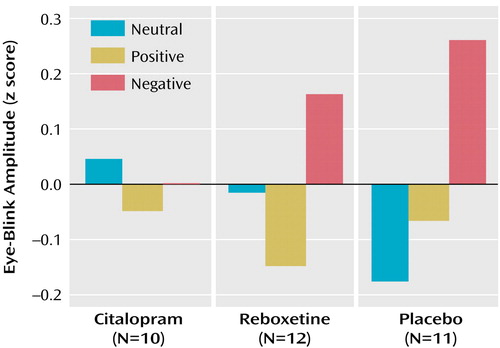
Figure 3. Emotion-Potentiated Eye-Blink Startle Response in 33 Healthy Volunteers After 1 Week of Randomly Assigned Double-Blind Intervention With Citalopram, Reboxetine, or Placeboa
aValues represent mean eye blinks (z transformed) during presentation of positive, negative, and neutral pictures. There was a significant interaction between group and stimulus type (F=2.7, df=3, 60, p=0.04).
1. Kent JM, Coplan JD, Gorman JM: Clinical utility of the selective serotonin reuptake inhibitors in the spectrum of anxiety. Biol Psychiatry 1998; 44:812–824Crossref, Medline, Google Scholar
2. Nutt DJ: The neuropharmacology of serotonin and noradrenaline in depression. Int Clin Psychopharmacol 2002; 17(suppl 1):S1-S12Google Scholar
3. Beck AT, Rush AJ, Shaw BF, Emery G: Cognitive Therapy of Depression. New York, Guilford, 1979Google Scholar
4. Bradley BP, Mogg K, Williams R: Implicit and explicit memory for emotion-congruent information in clinical depression and anxiety. Behav Res Ther 1995; 33:755–770Crossref, Medline, Google Scholar
5. Murphy FC, Sahakian BJ, Rubinsztein JS, Michael A, Rogers RD, Robbins TW, Paykel ES: Emotional bias and inhibitory control processes in mania and depression. Psychol Med 1999; 29:1307–1321Crossref, Medline, Google Scholar
6. Bradley BP, Mogg K, Lee SC: Attentional biases for negative information in induced and naturally occurring dysphoria. Behav Res Ther 1997; 35:911–927Crossref, Medline, Google Scholar
7. Bouhuys AL, Geerts E, Gordijn MC: Depressed patients’ perceptions of facial emotions in depressed and remitted states are associated with relapse: a longitudinal study. J Nerv Ment Dis 1999; 187:595–602Crossref, Medline, Google Scholar
8. Mogg K, Bradley BP: Selective orienting of attention to masked threat faces in social anxiety. Behav Res Ther 2002; 40:1403–1414Crossref, Medline, Google Scholar
9. Mogg K, Bradley BP, Millar N, White J: A follow-up study of cognitive bias in generalized anxiety disorder. Behav Res Ther 1995; 33:927–935Crossref, Medline, Google Scholar
10. Salkovskis PM (ed): Frontiers of Cognitive Therapy: The State of the Art and Beyond. New York, Guilford, 1997Google Scholar
11. Sheline YI, Barch DM, Donnelly JM, Ollinger JM, Snyder AZ, Mintun MA: Increased amygdala response to masked emotional faces in depressed subjects resolves with antidepressant treatment: an fMRI study. Biol Psychiatry 2001; 50:651–658Crossref, Medline, Google Scholar
12. Lang PJ, Davis M, Ohman A: Fear and anxiety: animal models and human cognitive psychophysiology. J Affect Disord 2000; 61:137–159Crossref, Medline, Google Scholar
13. von Zerssen D, Strian F, Schwarz D: Evaluation of depressive states, especially in longitudinal studies, in Psychological Measurements in Psychopharmacology. Edited by Pichot P. Basel, Switzerland, Karger, 1974, 189–202Google Scholar
14. Spielberger CD, Gorsuch RL, Lushene RD: STAI Manual. Palo Alto, Calif, Consulting Psychologists Press, 1970Google Scholar
15. Buss AH, Durkee A: An inventory for assessing different kinds of hostility. J Consult Psychol 1957; 21:343–349Crossref, Medline, Google Scholar
16. Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J: An inventory for measuring depression. Arch Gen Psychiatry 1961; 4:561–571Crossref, Medline, Google Scholar
17. Watson D, Clark LA, Tellegen A: Development and validation of brief measures of positive and negative affect: the Positive and Negative Affect Schedule scales. J Pers Soc Psychol 1988; 54:1063–1070Crossref, Medline, Google Scholar
18. Bosc M, Dubini A, Polin V: Development and validation of a social functioning scale, the Social Adaptation Self-Evaluation Scale. Eur Neuropsychopharmacol 1997; 7(suppl 1):S57-S70Google Scholar
19. Ekman P, Friesen WV: Pictures of Facial Affect. Palo Alto, Calif, Consulting Psychologists Press, 1976Google Scholar
20. Young AW, Rowland D, Calder AJ, Etcoff NL, Seth A, Perrett DI: Facial expression megamix: tests of dimensional and category accounts of emotion recognition. Cognition 1997; 63:271–313Crossref, Medline, Google Scholar
21. Anderson NH: Likableness ratings of 555 personality trait words. J Pers Soc Psychol 1968; 9:272–279Crossref, Medline, Google Scholar
22. Lang PJ, Bradley MM, Cuthbert BN: International Affective Picture System (IAPS): Technical Manual and Affective Ratings. Gainesville, University of Florida, Center for Research in Psychophysiology, 1998Google Scholar
23. Larson CL, Ruffalo D, Nietert JY, Davidson RJ: Temporal stability of the emotion-modulated startle response. Psychophysiology 2000; 37:92–101Crossref, Medline, Google Scholar
24. Davis M: The role of the amygdala in fear-potentiated startle: implications for animal models of anxiety. Trends Pharmacol Sci 1992; 13:35–41Crossref, Medline, Google Scholar
25. Harmer CJ, Hill SA, Taylor MJ, Cowen PJ, Goodwin GM: Toward a neuropsychological theory of antidepressant drug action: increase in positive emotional bias after potentiation of norepinephrine activity. Am J Psychiatry 2003; 160:990–992Link, Google Scholar
26. Harmer CJ, Bhagwagar Z, Perrett DI, Vollm BA, Cowen PJ, Goodwin GM: Acute SSRI administration affects the processing of social cues in healthy volunteers. Neuropsychopharmacology 2003; 28:148–152Crossref, Medline, Google Scholar
27. Funayama ES, Grillon C, Davis M, Phelps EA: A double dissociation in the affective modulation of startle in humans: effects of unilateral temporal lobectomy. J Cogn Neurosci 2001; 13:721–729Crossref, Medline, Google Scholar
28. Morris JS, Frith CD, Perrett DI, Rowland D, Young AW, Calder AJ, Dolan RJ: A differential neural response in the human amygdala to fearful and happy facial expressions. Nature 1996; 383:812–815Crossref, Medline, Google Scholar
29. Adolphs R, Tranel D, Damasio H, Damasio A: Impaired recognition of emotion in facial expressions following bilateral damage to the human amygdala. Nature 1994; 372:669–672Crossref, Medline, Google Scholar
30. Whalen PJ, Shin LM, Somerville LH, McLean AA, Kim H: Functional neuroimaging studies of the amygdala in depression. Semin Clin Neuropsychiatry 2002; 7:234–242Crossref, Medline, Google Scholar
31. Drevets WC: Functional anatomical abnormalities in limbic and prefrontal cortical structures in major depression. Prog Brain Res 2000; 126:413–431Crossref, Medline, Google Scholar
32. Burghardt NS, Sullivan GM, LeDoux JE: Fear increases with acute and decreases with chronic systemic citalopram treatment in rats. Abstracts of the Society for Neuroscience 2002, program number 85.17Google Scholar
33. Hjorth S, Auerbach SB: 5-HT1A autoreceptors and the mode of action of selective serotonin reuptake inhibitors (SSRI). Behav Brain Res 1996; 73:281–283Crossref, Medline, Google Scholar
34. Harmer CJ, Rogers RD, Tunbridge E, Cowen PJ, Goodwin GM: Tryptophan depletion decreases fear recognition in healthy females. Psychopharmacology (Berl) 2003; 167:411–417Crossref, Medline, Google Scholar
35. Knutson B, Wolkowitz OM, Cole SW, Chan T, Moore EA, Johnson RC, Terpstra J, Turner RA, Reus VI: Selective alteration of personality and social behavior by serotonergic intervention. Am J Psychiatry 1998; 155:373–379Link, Google Scholar



