Mental Disorders and Mental Health Treatment Among U.S. Department of Veterans Affairs Outpatients: The Veterans Health Study
Abstract
OBJECTIVE: The authors examined the self-reported presence and treatment of current depressive disorder, posttraumatic stress disorder (PTSD), and alcohol-related disorder in a group of outpatient veterans. METHOD: Data were obtained from the Veterans Health Study, a longitudinal investigation of male veterans’ health. A representative sample of 2,160 outpatients (mean age=62 years) was drawn from Boston-area U.S. Department of Veterans Affairs (VA) outpatient facilities. The participants completed screening measures for depression, PTSD, and alcohol-related disorder. Mental health treatment was assessed by interviews. RESULTS: The screening criteria for at least one current mental disorder were satisfied by 40% (N=856) of the patients. Screening rates were 31% (N=676) for depression, 20% (N=426) for PTSD, and 12% (N=264) for alcohol-related disorder. Patients who screened positively for current mental disorders were younger, less likely to be married or employed, and more likely to report traumatic exposure than were those without mental disorders. Of those who met the screening criteria for any of the targeted mental disorders, 68% (N=579) reported receiving mental health treatment. Younger, Caucasian men and those who reported more traumatic exposure were more likely to report receiving mental health treatment than were others who screened positively for mental disorders. CONCLUSIONS: Screening rates of depression and PTSD and rates of mental health treatment were considerably higher among these VA outpatients than among similar patients in primary care in the private sector. Although the VA is currently meeting the mental health care needs of its patients, future fiscal constraints could affect most adversely the treatment of non-Caucasian and older patients and those with a history of traumatic exposure.
Among patients in primary care, mental disorders often are inadequately recognized and inappropriately treated (1–4). The resultant burden, in terms of greater patient suffering (5–7), increased use of medical services (8, 9), and higher costs (9, 10), is borne by both patients and health care institutions. To reduce the institutional burden, managed care organizations often restrict the number of mental health care visits or their reimbursement. Critics warn, however, that such strategies are shortsighted and will ultimately intensify the burden (11).
The U.S. Department of Veterans Affairs (VA) health care system—the largest integrated U.S. health care system—shares the concern of efficiency with the private sector. The VA differs substantially from the private sector, however, in that it imposes few restrictions on mental health care access. This distinctive characteristic presents a unique opportunity to examine the prevalence, treatment, and outcomes of mental disorders.
We sought to characterize the screening rates of three mental disorders—depression, posttraumatic stress disorder (PTSD), and alcohol-related disorder—and their treatment among VA outpatients. These disorders were selected because they are debilitating conditions and are prevalent among VA patients (12–15). Specific study aims were to 1) determine the screening rates of these disorders, 2) identify characteristics that distinguished patients who did and did not satisfy the screening criteria for these disorders, 3) investigate the rates of mental health treatment among patients who satisfied the screening criteria for these disorders, and 4) identify characteristics among patients who screened positively for mental disorders that distinguished those who reported receiving mental health treatment from those who did not.
METHOD
Sample and Procedures
The Veterans Health Study is a prospective, longitudinal study of the health of male VA outpatients (16, 17). We identified and contacted 5,297 VA outpatients from among all male patients visiting Boston-area VA outpatient clinics during specified periods between June 1993 and May 1995. Of these, 1,061 were ineligible (100 had died, 377 were too ill, 108 were in residential care or were institutionalized, 84 had cognitive impairment, 188 had been relocated, 63 had no telephone, 44 were participating in another study, 5 had language problems, and 92 were ineligible for other reasons). Thus, 4,236 patients (80%) were eligible for participation.
Of those eligible, 2,425 (57.2%) agreed to participate. Details concerning study design and recruitment are presented elsewhere (16, 17). After a complete description of the study to the subjects, written informed consent was obtained. Complete data were available for 2,160 participants.
To address sample representativeness, we made two comparisons. First, to evaluate the potential bias from nonparticipants, we compared the 2,425 patients who agreed to participate with the 1,811 patients who refused. Groups were similar for sociodemographic variables, medical conditions, perceived global health status, and health care utilization, although those who agreed to participate were slightly more educated (average education, participants=12.6 years, nonparticipants=11.9 years) and more had visited a doctor in the past 3 months (participants=80.2%, nonparticipants=74.8%).
Second, we assessed regional and national representativeness. Two random samples of male patients who used VA services during the study enrollment period were identified from computerized medical records. The first sample consisted of 9,787 outpatients who had visited Boston-area VA clinics; the second was a national sample of 12,415 VA outpatients. The Veterans Health Study was found to be broadly representative of VA patients nationwide. It represents particularly well patients who regularly use VA outpatient services.
Measures
Self-report screening measures of depression, PTSD, and alcohol-related disorder were administered; information on demographics, trauma exposure, military history, and combat exposure was obtained by questionnaire. Mental health care utilization was obtained by trained research staff by using an interview based on the Medical Outcomes Study (18).
Depression. Patients who scored 16 or higher on the Center for Epidemiologic Studies Depression Scale (CES-D Scale) (19) received a screening diagnosis of depression.
PTSD. We assessed traumatic exposure by using several measures. A modified self-report version of the Traumatic Stress Schedule (20) assessed exposure to robbery, physical or sexual assault, serious motor vehicle accident, violent death of a loved one, and injury or property damage from fire or disaster. The Combat Scale (21) measured exposure to combat. Also included were single items evaluating exposure to combat or other traumatic events.
We assessed reexperiencing, avoidance and numbing, and arousal symptoms with the PTSD Checklist for Civilians (22), a 17-item, self-report measure based on DSM-IV. Per DSM-IV, patients received a PTSD screening diagnosis if they endorsed traumatic exposure and reported being at least “moderately bothered” by one or more reexperiencing symptoms, three or more numbing and avoidance symptoms, and two or more hyperarousal symptoms.
Alcohol-related disorder. Patients who reported two or more positive responses on the CAGE questionnaire (23) and past year alcohol consumption (24) received a screening diagnosis of alcohol-related disorder.
Mental health care utilization. During a medical history interview, participants were asked whether they currently, or had ever, received treatment for any of seven conditions (depression, PTSD, alcohol abuse, schizophrenia, bipolar disorder, anxiety or panic disorder, or drug abuse) or any other psychiatric condition. Treatment was nonspecific.
In a separate analysis, we compared administrative data on mental health visits during the previous 7 years. We found good overall agreement; of those who reported ever having received mental health treatment, 72% received treatment in a VA mental health clinic (kappa=0.57; 95% confidence interval [CI]=0.54–0.61).
Analytic Plan
To identify variables associated with a screening diagnosis, we first compared measures between patients who did and did not meet the screening criteria for a targeted mental disorder by using t tests for continuous variables and chi-square tests for categorical variables. For categorical variables with more than two levels, we also examined the cell contribution to the total chi-square in order to better indicate the levels contributing most to departures from independence. We then used logistic regression analysis to identify patient characteristics that were associated with the presence of each mental disorder, while controlling for sociodemographics. Analyses were conducted by using backward elimination and omitting characteristics that were not significant at the 0.05 level.
Among patients who satisfied the study criteria for any targeted mental disorder, we compared the patient characteristics of those who reported receiving mental health treatment and those who reported never receiving treatment. We used t tests for continuous variables and chi-square tests of independence (and cell contribution to overall chi-square) for categorical variables.
We then used logistic regression with backward elimination to identify patient characteristics associated with receiving mental health treatment. We also included continuous scores on screening measures of depression and PTSD and endorsement of the number of items on the CAGE questionnaire to assess the contribution of the severity of the disorders to receiving treatment.
In the logistic regression analyses, we estimated the effect on the odds ratio of having a score of one standard deviation above the mean for combat exposure—or, in the case of age, of being a decade older—by exponentiating the odds ratio to the standard deviation. Thus, a man who scored one standard deviation above the mean on the Combat Scale (SD=3.85) would have an odds ratio of 1.103.85, or 1.44—i.e., he would have a 44% greater odds of screening positively for depression.
RESULTS
Of the 2,160 study participants, the mean age was 61.6 years (SD=12.6); the mean years of education were 12.6 (SD=2.5). The majority (92%) were Caucasian. Over half (58%) were married. Thirty-six percent were employed, 44% were retired, 4% were unemployed, and 16% were disabled. The majority (51%) reported an annual income of less than $20,000. Eighty-five percent (N=1,836) reported exposure to any traumatic event (i.e., combat, robbery, physical or sexual assault, life-threatening illness or injury, serious motor vehicle accident, violent death of a loved one, or injury or property damage from fire or disaster). The mean Combat Scale score was 2.5 (SD=3.9).
Rates and Comorbidities of Screening Diagnoses
Over one-third (N=856, 40%) of the sample met the study criteria for at least one targeted mental disorder. Thirty-one percent (N=676; 95% CI=29%–33%) satisfied the screening criteria for depression, 20% (N=426; 95% CI=18%–22%) for PTSD, and 12% (N=264; 95% CI=10%–14%) for current alcohol-related disorder. By using sensitivity and specificity from comparable samples, we estimated the true prevalence (25) of depression (26) and alcohol-related disorder (27) among VA outpatients. We were unable to estimate the true prevalence of PTSD because the sensitivity and specificity of the PTSD Checklist for Civilians per DSM-IV scoring criteria were unavailable. After we adjusted for sensitivity and specificity, the population prevalence of depression was estimated at 29% and for alcohol-related disorder, 11%.
Among the 676 patients who screened positively for depression, 51% (N=348) also met the screening criteria for PTSD, and 21% (N=145) for alcohol-related disorder. Among the 426 patients who met the study criteria for PTSD, 82% (N=348) met the screening criteria for depression, and 24% (N=104) for alcohol-related disorder. Of the 264 patients who satisfied the screening criteria for alcohol-related disorder, 55% (N=145) met the screening criteria for depression, and 39% (N=104) for PTSD.
Patient Characteristics Associated With Mental Disorders
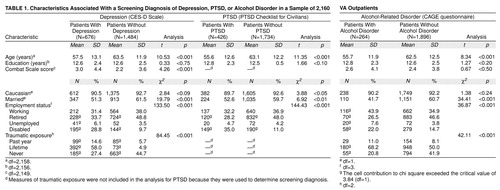
For each mental disorder, we compared the characteristics of patients who did and did not meet the screening criteria (table 1). Patients who satisfied the screening criteria for any targeted disorder were younger, less likely to be married or retired, and more likely to be disabled and to have reported exposure to a traumatic event. (We excluded traumatic exposure from the analysis for PTSD because it was used to determine the screening diagnosis.)
We examined the multivariate relationship between patient characteristics and the screening diagnosis of each mental disorder. For each disorder, older men were at a lower risk of meeting the screening criteria, as were men who were married or working (goodness-of-fit chi-square: depression, χ2=238.43, df=8, p<0.001; PTSD, χ2=174.70, df=2, p<0.001; alcohol-related disorder, χ2=103.46, df=5, p<0.001). Race and education were considered but did not meet the criterion for retention.
After we controlled for age and marital and employment status, men who reported experiencing a traumatic event in the past year were three times more likely to meet the screening criteria for depression than were men who did not report experiencing recent trauma (odds ratio=3.12, 95% CI=2.15–4.51); those who reported lifetime traumatic exposure were 46% more likely to meet the criteria for depression than were those who did not report experiencing lifetime trauma (95% CI=1.17–1.84). A man with a combat exposure score one standard deviation (SD=3.85) higher than the mean had a 24% greater odds of screening positively for depression (95% CI=1.12–1.36).
Because PTSD was defined in part on the basis of experiencing a traumatic event, we did not include measures of this characteristic in the model.
When we controlled for age and marital and employment status, men who reported experiencing a traumatic event during their lifetime (odds ratio=2.17, 95% CI=1.53–3.08) or during the past year (odds ratio=2.08, 95% CI=1.22–3.53) were twice as likely to meet the criteria for alcohol-related disorder than were men who did not report experiencing trauma.
Treatment of Mental Disorders
We examined self-reported mental health treatment history among the 856 participants who satisfied the study criteria for any targeted mental disorder. Of these, 68% (N=579) reported receiving mental health treatment. Among the 32% (N=277) who reported never receiving any mental health treatment, the majority (76%, N=211) met the screening criteria for one targeted disorder, 18% (N=51) met the criteria for two disorders, and 5% (N=15) met the criteria for three disorders.
Characteristics of Patients Receiving Mental Health Care
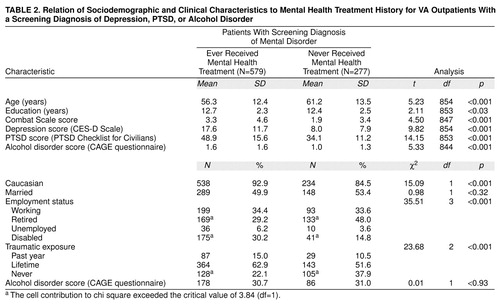
Among the participants who met the study criteria for any targeted mental disorder, we compared those who reported receiving mental health treatment and those who reported receiving no treatment. As shown in table 2, the patients who reported receiving mental health treatment were younger, more educated, more likely to be Caucasian, more likely to be disabled, and less likely to be retired. Treated men also reported more combat exposure, were more likely to have experienced a traumatic event during their lifetimes, and had more severe symptoms of depression, PTSD, and alcohol-related disorder.
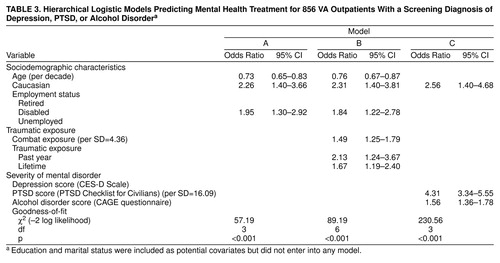
Among patients with any mental disorder, we used logistic regression analysis to examine the association with sociodemographic variables (table 3, model A). In successive models, we added measures of traumatic exposure (model B) and severity of mental disorders (model C). The addition of the traumatic exposure measures resulted in a significant improvement of the model (Δχ2=32.00, Δdf=3, p<0.001). The addition of severity of mental disorders, as assessed by continuous scores on the CES-D Scale, the PTSD Checklist for Civilians, and the CAGE questionnaire, eliminated the previously significant effects of age, employment status, and traumatic exposure. On the basis of model C, men who were Caucasian and had more severe PTSD symptoms and more severe alcohol-related symptoms were more likely to report receiving mental health treatment. A veteran with a score on the PTSD Checklist for Civilians one standard deviation higher than the mean had four times greater odds of receiving mental health treatment. For each additional CAGE questionnaire item endorsed, a veteran was 56% more likely to report receiving mental health treatment.
DISCUSSION
The screening criteria for at least one targeted mental disorder were met by 40% (N=856) of the patients. Screening rates for depression and PTSD among our sample (mean age=62 years) were higher than those among comparably aged patients in primary care in the private sector and similar to those of younger Vietnam veterans (13, 28–30). Because older adults tend to underreport psychological distress (31), we were surprised to find that they had such elevated rates of depression and PTSD.
Traumatic exposure was strongly associated with a higher risk for the targeted mental disorders. This finding is confirmed by other studies that document high rates of mental disorders among those with traumatic exposure (12–15). Recent research links traumatic exposure with poorer health outcomes and increased health care utilization (32). In concert with this research, our findings suggest that routine screening for traumatic exposure could yield important information regarding mental and physical health status. Such routine screening, combined with appropriate referrals for mental health treatment, may attenuate the impact of traumatic exposure.
Over two-thirds of the Veterans Health Study participants who satisfied the screening criteria for any targeted mental disorder reported receiving mental health treatment; rates were twice those of primary care patients in the private sector (33). There are several possible interpretations for this finding. First, more patients with mental disorders may come to the VA than to facilities in the private sector. This interpretation is supported by findings that VA patients have poorer mental health status than primary care patients in the private sector (17). Second, veterans who do not use VA health care exclusively may be more inclined to seek mental health treatment from the VA. This interpretation is consistent with research that suggests that veterans with mental disorders such as PTSD prefer to receive mental health treatment from the VA (34). Third, because of broad access to mental health services, VA providers may face fewer barriers in referring patients for mental health treatment.
Non-Caucasian patients were less likely to report receiving mental health treatment. This is consistent with research documenting lower rates of mental health treatment among ethnic and racial minorities (35). However, Rosenheck and Fontana (36) found that minority status only affects non-VA mental health care use. Perhaps minorities seek VA mental health care because they believe they can obtain fairer treatment from an institution operated by the federal government (36). Additionally, the integration of mental and medical services offered by the VA may reduce the stigma perceived by some minorities regarding mental health treatment (36). In light of this, our findings suggest that future limitations in access to VA mental health care could most adversely affect veterans from racial and ethnic minorities.
Older patients were less likely to report receiving mental health treatment. Although this age effect disappeared when the severity of the mental disorder was included in our model, it suggests that VA health care providers, like those in the private sector (37), may be less likely to refer older patients for mental health treatment. Conversely, older patients, like their counterparts in the private sector (38), may be less inclined to seek mental health treatment.
Our study has several limitations. First, we used screening measures rather than clinical interviews to identify mental disorders, and some patients may have been misclassified. Second, we used only one screening measure to assess each targeted disorder; although we would have preferred to use multiple measures, we were limited by previously established procedures of the Veterans Health Study. Third, because different time periods were associated with each screening measure (1 week for depression, 1 month for PTSD, and 1 year for alcohol-related disorder), the timing for “current” comorbidities was not the same. Fourth, the symptoms of mental disorders and treatment were determined by self-report; only patients willing to disclose such information were identified. Finally, we obtained retrospective accounts of treatment; therefore, relationships between disorders and mental health treatments are postdictive (39).
Notwithstanding these limitations, the present study is the first, to our knowledge, to examine the rates of mental disorders and treatment among a large sample of VA outpatients. Findings indicate that 1) screening rates of depression and PTSD are higher than rates found among comparably aged patients in primary care in the private section; 2) traumatic exposure is associated with a higher risk for the three targeted disorders; 3) the majority of patients who met the screening criteria for any of the targeted mental disorders reported receiving mental health treatment; and 4) non-Caucasian and older patients who screened positively for these targeted mental disorders were less likely to report receiving mental health treatment.
In the face of federal budget constraints, the VA is reorganizing health services delivery (40). Because of ensuing staff reductions, inadvertent capitation of mental health services may result, whereby fewer providers will be available, and patients may wait longer to receive nonemergency treatments such as mental health care. Our findings suggest that the resultant burden created by restricted access to VA mental health care may most adversely affect non-Caucasian patients, those who are older, and those who have a history of traumatic exposure. Thus, as the VA increasingly emulates the private sector, both patient and institutional burden may intensify.
Presented in part at the 14th annual meeting of the Association for Health Services Research, Chicago, June 15–17, 1997. Received Jan. 12, 1998; revisions received Sept. 30, 1998, and March 9, 1999; accepted April 13, 1999. From the Center for Health Quality, Outcomes, and Economic Research, Health Services Research and Development Center of Excellence, VA Medical Center, Bedford, Mass.; Center for Health Care Evaluation, Health Services Research and Development Center of Excellence, Palo Alto. Address reprint requests to Dr. Hankin, HSR&D, VA Medical Center (152), 3801 Miranda Ave., Palo Alto, CA 94304-1207; [email protected] (e-mail). Supported by grants SDR 91-006.S and IIR 96-30.1 from the Health Services Research and Development Service, Veterans Health Administration, U.S. Department of Veterans Affairs. The authors thank the veterans and staff who participated in this study and Dorcas Mansell, Walter Penk, William Rogers, Paula Schnurr, and Alfredo Selim, who commented on earlier drafts of this article.
 |
 |
 |
1. Fauman MA: Psychiatric components of medical and surgical practice, II: referral and treatment of psychiatric disorders. Am J Psychiatry 1983; 140:760–763Link, Google Scholar
2. Katon W, von Korff M, Lin E, Bush T, Ormel J: Adequacy and duration of antidepressant treatment in primary care. Med Care 1992; 30:67–76Crossref, Medline, Google Scholar
3. Perez-Stable EJ, Miranda J, Munoz RF, Ying YW: Depression in medical outpatients: underrecognition and misdiagnosis. Arch Intern Med 1990; 150:1083–1088Google Scholar
4. Wells KB, Katon W, Rogers B, Camp P: Use of minor tranquilizers and antidepressant medications by depressed outpatients: results from the Medical Outcomes Study. Am J Psychiatry 1994; 151:694–700Link, Google Scholar
5. Bruce ML, Leaf PJ, Rozal GP, Florio L, Hoff RA: Psychiatric status and 9-year mortality data in the New Haven Epidemiologic Catchment Area study. Am J Psychiatry 1994; 151:716–721Link, Google Scholar
6. Hays RD, Wells KB, Sherbourne CD, Rogers W, Spritzer K: Functioning and well-being outcomes of patients with depression compared with chronic general medical illnesses. Arch Gen Psychiatry 1995; 52:11–19Crossref, Medline, Google Scholar
7. Wells KB, Stewart A, Hays RD, Burnam MA, Rogers W, Daniels M, Berry S, Greenfield S, Ware J: The functioning and well-being of depressed patients: results from the Medical Outcomes Study. JAMA 1989; 262:914–919Crossref, Medline, Google Scholar
8. Barsky AJ, Wyshak G, Klerman GL: Medical and psychiatric determinants of outpatient medical utilization. Med Care 1986; 24:548–560Crossref, Medline, Google Scholar
9. Levenson JL, Hamer RM, Rossiter LF: Relation of psychopathology in general medical inpatients to use and cost of services. Am J Psychiatry 1990; 147:1498–1503Google Scholar
10. Pallak MS, Cummings NA, Dorken H, Henke CJ: Effect of mental health treatment on medical costs. Mind/Body Medicine 1994; 1:7–12Google Scholar
11. Barsky AJ, Borus MF: Somatization and medicalization in the era of managed care. JAMA 1995; 274:1931–1934Google Scholar
12. Helzer JE, Robins LN, Davis DH: Depressive disorders in Vietnam returnees. J Nerv Ment Dis 1976; 163:177–185Crossref, Medline, Google Scholar
13. Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, Weiss DS: Trauma and the Vietnam War Generation: Report of Findings From the National Vietnam Veterans Readjustment Study. New York, Brunner/Mazel, 1990Google Scholar
14. Molgaard CA, Poikolainen K, Elder JP, Nissinen A, Pekkanen J, Golbeck AL, de Moor C, Lahtela K, Puska P: Depression late after combat: a follow-up of Finnish World War Two veterans from the Seven Countries East-West Cohort. Mil Med 1991; 156:219–221Crossref, Medline, Google Scholar
15. Walker RD, Howard MO, Lambert MD, Suchinsky R: Psychiatric and medical comorbidities of veterans with substance use disorders. Hosp Community Psychiatry 1994; 45:232–237Abstract, Google Scholar
16. Kazis LE, Miller DR, Clark JA, Skinner K, Lee A, Rogers W: Health-Related Quality of Life in Veterans: The Veterans Health Study. Washington, DC, Department of Veterans Affairs, Health Services Research and Development Service, July 1995Google Scholar
17. Kazis LE, Miller DR, Clark J, Skinner K, Lee A, Rogers W, Spiro A III, Payne S, Fincke G, Selim A, Linzer M: Health-related quality of life in patients served by the Department of Veterans Affairs: results from the Veterans Health Study. Arch Intern Med 1998; 158:626–632Crossref, Medline, Google Scholar
18. Kravitz RL, Greenfield S, Rogers W, Manning WG Jr, Zubkoff M, Nelson EC, Tarlov AR, Ware JE Jr: Differences in the mix of patients among medical specialties and systems of care: the Medical Outcomes Study. JAMA 1992; 267:1617–1623Google Scholar
19. Radloff LS: The CES-D Scale: a self-report depression scale for research in the general population. J Applied Psychol Measurement 1977; 1:385–401Crossref, Google Scholar
20. Norris FH: Screening for traumatic stress: a scale for use in the general population. J Appl Soc Psychol 1990; 20:1704–1718Google Scholar
21. Laufer RS, Gallops MS, Frey-Wouters E: War stress and trauma: the Vietnam veteran experience. J Health Soc Behav 1984; 25:65–85Crossref, Medline, Google Scholar
22. Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM: The PTSD Checklist (PCL): reliability, validity, and diagnostic utility, in Proceedings of the 9th Annual Meeting of the International Society for Traumatic Stress Studies. Chicago, ISTSS, 1993, p 38Google Scholar
23. Ewing JA: Detecting alcoholism: the CAGE questionnaire. JAMA 1984; 252:1905–1907Google Scholar
24. Callahan CM, Tierney WM: Health services use and mortality among older primary care patients with alcoholism. J Am Geriatr Soc 1995; 43:1378–1383Google Scholar
25. Rogan WJ, Gladen B: Estimating prevalence from the results of a screening test. Am J Epidemiol 1978; 107:71–76Crossref, Medline, Google Scholar
26. Zimmerman M, Coryell W: Screening for major depressive disorder in the community: a comparison of measures. Psychol Assessment 1994; 6:71–74Crossref, Google Scholar
27. Liskow B, Campbell J, Nickel EJ, Powell BJ: Validity of the CAGE questionnaire in screening for alcohol dependence in a walk-in (triage) clinic. J Stud Alcohol 1995; 56:277–281Crossref, Medline, Google Scholar
28. Callahan CM, Hui SL, Nienaber NA, Musick BS, Tierney WM: Longitudinal study of depression and health services use among elderly primary care patients. J Am Geriatr Soc 1994; 42:833–838Crossref, Medline, Google Scholar
29. Coulehan JL, Schulberg HC, Block MR, Janosky JE, Arena BC: Medical comorbidity of major depressive disorder in primary medical practice. Arch Intern Med 1990; 150:2363–2367Google Scholar
30. Card J: Lives After Vietnam: The Personal Impact of Military Service. Lexington, Mass, DC Heath, 1983Google Scholar
31. Blazer DG: Is depression more frequent in late life? an honest look at the evidence. Am J Geriatr Psychiatry 1994; 2:193–199Crossref, Medline, Google Scholar
32. Friedman MJ, Schnurr PP: The relationship between trauma, post-traumatic stress disorder, and physical health, in Neurobiological and Clinical Consequences of Stress: From Normal Adaptation to PTSD. Edited by Friedman MJ, Charney DS, Deutch AY. Philadelphia, Lippincott-Raven, 1995, pp 507–524Google Scholar
33. Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen H-U, Kendler KS: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry 1994; 51:8–19Crossref, Medline, Google Scholar
34. Rosenheck R, Fontana A: Do Vietnam-era veterans who suffer from posttraumatic stress disorder avoid VA mental health services? Mil Med 1995; 160:136–142Google Scholar
35. Padgett DK, Patrick C, Burns BJ, Schlesinger HJ: Ethnicity and the use of outpatient mental health services in a national insured population. Am J Public Health 1994; 84:222–226Crossref, Medline, Google Scholar
36. Rosenheck R, Fontana A: Utilization of mental health services by minority veterans of the Vietnam era. J Nerv Ment Dis 1994; 182:685–691Crossref, Medline, Google Scholar
37. German PS, Shapiro S, Skinner EA: Mental health of the elderly: use of health and mental health services. J Am Geriatr Soc 1985; 33:246–252Crossref, Medline, Google Scholar
38. Goldstrom IG, Burns BJ, Kessler LG, Feuerberb MA, Larson DB, Miller NE, Cromer WJ: Mental health services use by elderly adults in a primary care setting. J Gerontol 1987; 42:147–153Crossref, Medline, Google Scholar
39. Manning WG, Newhouse JP, Ware JE Jr: The status of health in demand estimation; or beyond excellent, good, fair, and poor, in Economic Aspects of Health. Edited by Fuchs VR. Chicago, University of Chicago Press, 1982, pp 143–184Google Scholar
40. Igelhart JK: Reform of the Veterans Affairs health care system. N Engl J Med 1996; 335:1407–1411Google Scholar



