Impairment in Pure and Comorbid Generalized Anxiety Disorder and Major Depression at 12 Months in Two National Surveys
Abstract
OBJECTIVE: Generalized anxiety disorder might be better conceptualized as a prodrome, residual, or severity marker of major depression or other comorbid disorders than as an independent diagnosis. The authors questioned whether generalized anxiety disorder itself is associated with role impairment or whether the impairment of patients with generalized anxiety disorder is due to depression or other comorbid disorders. METHOD: The authors assessed data from the National Comorbidity Survey and the Midlife Development in the United States Survey for generalized anxiety disorder and major depression at 12 months by using the DSM-III-R criteria with modified versions of the Composite International Diagnostic Interview. RESULTS: The prevalences of generalized anxiety disorder at 12 months were 3.1% and 3.3%, respectively, in the National Comorbidity Survey and the Midlife Development in the United States Survey; the prevalences of major depression at 12 months were 10.3% and 14.1%. The majority of respondents with generalized anxiety disorder at 12 months in the National Comorbidity Survey (58.1%) and the Midlife Development in the United States Survey (69.7%) also met the criteria for major depression at 12 months. Comparisons of respondents with one versus neither disorder showed that both disorders had statistically significant independent associations with impairment that were roughly equal in magnitude. These associations could not be explained by the other comorbid DSM-III-R disorders or by sociodemographic variables. CONCLUSIONS: These results show that a substantial amount of generalized anxiety disorder occurs independently of major depression and that the role impairment of generalized anxiety disorder is comparable to that of major depression.
Interest in comorbidity between generalized anxiety disorder and major depression has grown dramatically over the past decade on the basis of evidence that this type of comorbidity is very common (1), that it is associated with more impairment than either pure generalized anxiety disorder (2) or pure major depression (3), and that it predicts poor outcomes both among patients in treatment for generalized anxiety disorder (4) and among patients in treatment for major depression (5). There is also considerable interest in the relative impairment of pure generalized anxiety disorder and pure major depression. This interest can be traced to the controversy that has surrounded generalized anxiety disorder since its introduction in DSM-III in relation to the fact that the vast majority of patients with generalized anxiety disorder also carry one or more other psychiatric diagnoses (6). This high comorbidity has led to the suggestion that generalized anxiety disorder might be better conceptualized as a prodrome, residual, or severity marker of major depression or other comorbid disorders than as an independent diagnosis (7, 8). An issue central to this nosological debate is whether generalized anxiety disorder itself is associated with role impairment or whether the impairment of patients with generalized anxiety disorder is due to depression or other comorbid disorders (9).
Some information about the relative impairment of generalized anxiety disorder and major depression can be gleaned from three studies of untreated mental disorders among primary care patients (10–12). All three of these studies found that both “pure” major depression and “pure” generalized anxiety disorder, defined as current episodes of these disorders in the absence of any of the other mood, anxiety, or substance use disorders assessed in the surveys, were associated with meaningful levels of impairment in a number of life domains. For example, Ormel et al. (10) found that mean numbers of disability days in the past month were much higher among primary care patients with pure generalized anxiety disorder (4.4 days) and pure major depression (6.3 days) than among patients with none of the psychiatric disorders assessed in their survey (1.7 days), whereas Schonfeld et al. (12) found that mean age-sex adjusted scores on the 36-item Medical Outcomes Study Short-Form General Health Survey (13) scale of social functioning (possible score of 0–100) were much lower (a high score is indicative of good functioning) among primary care patients with pure generalized anxiety disorder (71.0) and pure major depression (60.3) than among those with none of the psychiatric disorders assessed in their survey (83.6).
The impairment associated with pure major depression is greater and more varied than that associated with pure generalized anxiety disorder in two of these studies (11, 12). However, the reliability of these findings can be questioned based on the fact that the numbers of patients with pure disorders in these studies were quite small: only four cases in one study (11) and 14 in the other (12) with pure generalized anxiety disorder and only 25 in the one study (11) and 54 in the other (12) with pure depression. Differences in the magnitude of impairment associated with pure generalized anxiety disorder and pure major depression were much smaller in the study by Ormel et al. (10), which included considerably larger numbers of respondents with pure generalized anxiety disorder (N=272) and pure major depression (N=438). Aggregate impairment of generalized anxiety disorder and major depression was also quite similar in a large primary care study carried out by Spitzer et al. (14) that did not distinguish between pure and comorbid patient cases.
It is important to note that the evaluations of comorbidity in all of these studies included other psychiatric disorders in addition to generalized anxiety disorder and major depression. Given the much higher prevalence of comorbidity between generalized anxiety disorder and major depression than with other types of anxiety-mood comorbidity (15), it is desirable to obtain more focused general population data to evaluate the separate and joint effects of these two disorders as well as to evaluate the effects of broader comorbidities in the general population. The current report presents data of this sort on work and social role impairment and perceived mental health status from two large nationally representative general population surveys, the National Comorbidity Survey (16) and the Midlife Development in the United States Survey (17).
METHOD
Samples
The National Comorbidity Survey is a nationally representative household survey of 8,098 persons age 15 to 54 years in the noninstitutionalized civilian population of the 48 coterminous United States, along with a representative supplemental sample of students living in campus group housing. The National Comorbidity Survey was administered to 8,098 respondents between September 1990 and February 1992 in face-to-face, in-home interviews. The response rate was 82.4%. A part two subsample of 5,877 respondents, consisting of all those with any Composite International Diagnostic Interview diagnosis and a random subsample of others, was administered a series of questions about the risk factors and consequences of psychiatric disorders. The data on impairment reported here are from the part two subsample. These data have been weighted to adjust for differential probabilities of selection and nonresponse. More details on the National Comorbidity Survey design, field procedures, and sample weights were reported elsewhere (16, 18).
The Midlife Development in the United States Survey is a nationally representative survey of 3,032 persons age 25–74 years in the noninstitutionalized civilian population of the 48 coterminous United States. The Midlife Development in the United States Survey was carried out by the John D. and Catherine T. MacArthur Foundation Network on Successful Midlife Development between January 1995 and January 1996. All respondents completed a 30-minute telephone interview (70.0% response rate) and filled out two mailed questionnaires estimated to take a total of about 90 minutes to complete (86.8% conditional response rate in the subsample of telephone respondents). The overall response rate (0.700×0.868) was 60.8%. The data reported here were weighted to adjust for differential probabilities of selection and nonresponse. More details on the Midlife Development in the United States Survey design, field procedures, and sampling weights are available elsewhere (17).
Diagnostic Assessment
National Comorbidity Survey diagnoses are based on a modified version of the Composite International Diagnostic Interview (19), a fully structured interview designed to be administered by interviewers who are not clinicians and to generate diagnoses according to the definitions and criteria of both DSM-III-R and ICD-10. The current report uses DSM-III-R criteria. Although the focus is on the prevalences of generalized anxiety disorder and major depression within the year prior to the interview (prevalences at 12 months), we also controlled for prevalences of the other disorders assessed in the National Comorbidity Survey at 12 months. These included other anxiety disorders (panic disorder, simple phobia, social phobia, agoraphobia, and posttraumatic stress disorder), mania, substance use disorders (alcohol and drug abuse and dependence), and nonaffective psychosis. Diagnoses were made without hierarchy rules. A National Comorbidity Survey clinical reappraisal study found good test-retest reliability and procedural validity of all of the diagnoses compared to clinical reassessments (20), with the exceptions of mania and nonaffective psychosis. On the basis of the finding that the Composite International Diagnostic Interview validly assesses only manic patients with a euphoric-grandiose symptom profile (21), our control for mania was limited to this subtype of manic patients. On the basis of the finding that the Composite International Diagnostic Interview substantially overdiagnoses nonaffective psychosis (22), our control for nonaffective psychosis was based on clinical reinterviews with all National Comorbidity Survey respondents who screened positive for nonaffective psychosis in the Composite International Diagnostic Interview.
The DSM diagnostic hierarchy rule for generalized anxiety disorder and major depression stipulates that an episode of generalized anxiety that occurs exclusively within a major depressive episode is not classified as generalized anxiety disorder. This rule was put into use in the National Comorbidity Survey in a series of three questions asked of all respondents who met the criteria for generalized anxiety disorder without hierarchy and major depression. The first asked whether the generalized anxiety disorder never, sometimes, or always occurred during times when the respondent was depressed. If it occurred sometimes or always, the second question asked which syndrome started first during these episodes of overlapping symptoms—the depression, the anxiety, both at the same time, or it varied. The third question was similar to the second except that it asked which symptoms ended first when and if either of them ever resolved. Only 4.6% of the National Comorbidity Survey respondents with comorbid generalized anxiety disorder at 12 months (without hierarchy) and major depression reported that their episodes of generalized anxiety disorder occurred exclusively within their episodes of major depression.
The Midlife Development in the United States Survey diagnoses were based on the Composite International Diagnostic Interview Short Form scales (23), a series of diagnosis-specific scales that were developed from item-level analyses of the Composite International Diagnostic Interview questions in the National Comorbidity Survey. The Composite International Diagnostic Interview Short Form scales were designed to reproduce the full Composite International Diagnostic Interview diagnoses as exactly as possible with only a small subset of the original questions. Comparison of the Composite International Diagnostic Interview Short Form classifications of generalized anxiety disorder with the full Composite International Diagnostic Interview classifications in the National Comorbidity Survey yielded a sensitivity of 96.6%, a specificity of 99.8%, and 99.6% overall agreement. A comparison of the Composite International Diagnostic Interview Short Form classifications of major depression with the full Composite International Diagnostic Interview classifications in the National Comorbidity Survey yielded a sensitivity of 89.6%, a specificity of 93.9%, and an overall agreement of 93.2%. Additional Composite International Diagnostic Interview Short Form diagnoses at 12 months included in the Midlife Development in the United States Survey are panic disorder (with or without agoraphobia), alcohol abuse and dependence, and drug abuse and dependence.
Measures of Impairment
Three measures of impairment were considered in this study. The first dealt with perceived mental health on the basis of parallel questions in both surveys that asked respondents to rate their mental health as excellent, very good, good, fair, or poor. A separate dichotomous version of this scale was created as an outcome for logistic regression analysis by assigning respondents who reported either fair or poor mental health a code of one and all others a code of zero.
The next measure dealt with work role impairment on the basis of two parallel questions in which respondents were asked about work loss and work cutback in the past month. Work loss was assessed by asking respondents how many days in the past month they were totally unable to work or carry out their normal daily activities because of problems with their emotions, nerves, or mental health. Work cutback was assessed by asking respondents how many days in the past month, exclusive of work loss days, they had to cut back on the amount of work they got done or did not get as much done as usual because of problems with their emotions, nerves, or mental health. Responses to the two questions were summed and collapsed into the categories 0, 1 to 2, 3 to 5, and 6 or more work impairment days. A separate dichotomous variable was created as an outcome for logistic regression analysis by assigning respondents with six or more combined work loss and work cutback days a code of one and all others a code of zero.
The last measure dealt with social role impairment on the basis of previously developed six-item scales of social support and negative social interaction (24). These scales were used to assess impairment in relationships with friends and relatives. The social support scale asked respondents to rate the following items with response categories of a lot, some, a little, and not at all: “How much friends and relatives…1) really care about you, 2) understand the way you feel about things, and 3) appreciate you. 4) How much can you rely on them for help if you have a serious problem? 5) How much can you open up to them if you need to talk about your worries? and 6) How much can you relax and be yourself around them?” The negative social interaction scale asked respondents to rate the following items with response categories of often, sometimes, rarely, and never: “How often do your friends and relatives 1) make too many demands on you, 2) make you feel tense, 3) argue with you, 4) criticize you, 5) let you down when you are counting on them, and 6) get on your nerves?”
Scores on the social support scale were reversed, so that low support had the highest score, and scores were summed with the negative interaction scale. The total score was then divided into four discrete categories on the basis of total sample percentiles of 0%–50% (lowest social role impairment), 51%–80%, 81%–90%, and 91% or higher (highest role impairment). A separate dichotomous measure of extreme social role impairment was also created as an outcome variable for logistic regression analysis by assigning respondents with answers in the 90%-or-higher range a code of one and all others a code of zero.
Analysis
Simple cross-tabulations were used to estimate the overlap between generalized anxiety disorder and major depression at 12 months. Conditional logistic regression analysis was then used to estimate the associations of generalized anxiety disorder and major depression at 12 months with measures of impairment in subsamples that differed in the presence or absence of the other disorder. All equations controlled for the other DSM-III-R disorders assessed in the surveys as well as for sociodemographic variables (age, gender, education, race/ethnicity, employment status, marital status, and urbanicity). Finally, a series of equations was estimated in the subsample of National Comorbidity Survey respondents with comorbid generalized anxiety disorder and major depression at 12 months to investigate whether temporal priority of one disorder over the other in age at first onset or timing of onset or offset within episodes significantly predicted the impairment.
Significance tests for individual coefficients were computed by using jackknife repeated replications (25) to estimate standard errors that adjusted for design effects introduced by the clustering (only in the National Comorbidity Survey as there was no geographic clustering in the Midlife Development in the United States Survey because it used a telephone sampling frame rather than a multistage area frame) and weighting of observations. Jackknife repeated replication is one of several methods that uses simulations of coefficient distributions in subsamples to generate empirical estimates of standard errors and significance tests. These estimates were used to compute 95% confidence intervals for unstandardized linear regression coefficients as well as for odds ratios obtained by exponentiating logistic regression coefficients. Tests for the significance of sets of predictors taken together were computed by using Wald chi-square tests. Design effects were introduced into these calculations by basing the Wald tests on coefficient variance-covariance matrices obtained from jackknife repeated replication simulations. All evaluations of statistical significance were made at the 0.05 level by using z tests, two-tailed.
RESULTS
The majority of respondents with generalized anxiety disorder at 12 months in both the National Comorbidity Survey (58.1%) and the Midlife Development in the United States Survey (69.7%) also had major depression at 12 months, whereas 17.5% of the respondents with major depression also had generalized anxiety disorder in the National Comorbidity Survey and 16.3% in the Midlife Development in the United States Survey (Figure 1).
Scores on the measures of impairment are presented in table 1. There is good consistency in results across the two surveys. In comparison with respondents in all three categories of disorder, the impairment of respondents with neither disorder is substantially lower than that of respondents with one or both disorders. Furthermore, the impairment of respondents with only one of the two disorders is consistently lower than that of respondents with both disorders, although this pattern is weak for social role impairment in the National Comorbidity Survey.
Data on the associations between pure generalized anxiety disorder and pure major depression and impairment, adjusted for other comorbid disorders and for sociodemographic variables, are presented in table 2. The first four columns report associations involving pure generalized anxiety disorder. Five of these six coefficients show that generalized anxiety disorder is associated with higher impairment than that found among respondents who do not have generalized anxiety disorder. Three of these five coefficients are statistically significant at the 0.05 level. The exception is social role impairment in the Midlife Development in the United States Survey, where there is no meaningful elevation among respondents with generalized anxiety disorder. The next four columns report associations involving pure major depression. All of these coefficients show that major depression is associated with significantly higher impairment than that found among respondents who do not have major depression. Comparison of the impairment associated with pure generalized anxiety disorder and pure major depression is reported in the last four columns of the table. None of these differences is statistically significant.
Data on the incremental effects of generalized anxiety disorder or major depression in the subsample of respondents with the other disorder are presented in table 3. The first four columns report associations involving the incremental effects of generalized anxiety disorder over and above those of major depression. Five of the six coefficients show that generalized anxiety disorder and major depression are associated with higher impairment than that found among depressed respondents who do not have generalized anxiety disorder. Three of these five are significant at the 0.05 level. The exception is social role impairment in the National Comorbidity Survey, in which the odds ratio is not meaningfully different from 1.0. The next four columns report associations involving the incremental effects of major depression over and above those of generalized anxiety disorder. Five of the six coefficients show that generalized anxiety disorder and major depression are associated with higher impairment than that found among respondents with pure generalized anxiety disorder. Two of these coefficients are significant at the 0.05 level. The exception is social role impairment in the National Comorbidity Survey, in which the odds ratio is 1.0.
Finally, we carried out more detailed analyses of the National Comorbidity Survey data to consider the possibility that the impairment associated with comorbid generalized anxiety disorder and major depression differs depending on which of the two disorders is primary and which is secondary. Similar analyses could not be carried out in the Midlife Development in the United States Survey because data on the primary-secondary distinction were not collected in that survey. Because this distinction is defined in several different ways (26), the analyses were carried out by estimating a series of three different models to predict impairment in the subsample of respondents who had both generalized anxiety disorder and major depression at 12 months and controlling for other DSM-III-R disorders at 12 months and sociodemographic variables.
The first of these models introduced information about whether age at onset of generalized anxiety disorder was before, after, or at the same age at onset as major depression. This information is not significantly related to any of the impairment measures. The second model added information about whether the symptoms of generalized anxiety disorder usually begin first, the symptoms of major depression usually begin first, both syndromes usually begin at about the same time, or it varies at the onset of episodes of comorbid generalized anxiety disorder and major depression. This information is not significantly related to any of the impairment measures. Finally, the third model added information about the typical order in which symptoms remit during episodes of comorbid generalized anxiety disorder and major depression. This information is not significantly related to any of the impairment measures.
DISCUSSION
A number of limitations need to be noted. First, the Composite International Diagnostic Interview is a lay-administered diagnostic interview that only imperfectly captures the diagnostic distinctions made by experienced clinicians. This is of special concern in an analysis of the comorbidity of generalized anxiety disorder and major depression because the core symptoms of generalized anxiety disorder and major depression overlap. The evidence of good concordance between the Composite International Diagnostic Interview and independent clinical diagnoses argues against a pervasive bias (20), but it remains possible that imprecision in the Composite International Diagnostic Interview in distinguishing cases of generalized anxiety disorder and major depression plays a part in the results reported here. Second, the impairment measures are based on self-reports. Because mood disturbances can lead to distorted perceptions of role functioning (27), it is conceivable that the results reflect the influences of comorbidity on perceptions of impairment rather than on actual impairment. This is especially problematic for the measures of work impairment because respondents had to report not only days of work loss and work cutback, but they also had to make attributions as to whether these work impairments were due to problems with their emotions, nerves, or mental health.
Within the context of these limitations, our results are similar to those in previous studies in the general population (1, 28, 29), in primary care samples (11, 30), and in mental health specialty samples (31, 32) in showing that major depression is a good deal more common than generalized anxiety disorder, that there is a strong comorbidity between generalized anxiety disorder and major depression, that major depression occurs in the majority of people with generalized anxiety disorder, and that generalized anxiety disorder occurs in a substantial minority of people with major depression. This is not to say that generalized anxiety disorder and major depression are so strongly related that they cannot be distinguished—they can. For example, Brown et al. (33) tested several models of structural relationships between symptoms of anxiety and depression and found separate latent factors of positive affectivity, negative affectivity, and autonomic suppression (related to generalized anxiety disorder). This finding strongly argues that generalized anxiety disorder and major depression can be distinguished despite the overlap in many of their core symptoms. Consistent with this finding, analyses of twin data by using an additive behavior genetic model concluded that the environmental determinants of generalized anxiety disorder and major depression are distinct (34). In turn, this result is consistent with the finding in epidemiologic research that generalized anxiety disorder and major depression have significantly different sociodemographic predictors (35).
It is noteworthy that twin studies also suggest that the genes for generalized anxiety disorder and major depression are the same (34), raising the possibility that the two syndromes are different manifestations of the same underlying disorder. However, the model on which this conclusion is based assumes that the joint effects of genes and environment are additive—that is, the impact of environmental determinants is not influenced by the presence or absence of the genes. This is implausible. A more realistic interactive specification, which cannot be identified with conventional twin data, might well show a differentiation of genetic effects. Consistent with this possibility, family studies show a differential aggregation of mental disorders in the families of patients with generalized anxiety disorder and major depression (36) and raise the possibility that comorbid generalized anxiety disorder and major depression might be a distinct disorder from pure generalized anxiety disorder or pure major depression (37).
We were able to go beyond simple bivariate analysis at 12 months with the National Comorbidity Survey data, but not with the Midlife Development in the United States Survey data (because of the absence of data on lifetime disorders and age at onset) to shed some light on two broader patterns of comorbidity. First, additional National Comorbidity Survey analysis not reported in this article shows that the absence of major depression at 12 months is uncommon among respondents with generalized anxiety disorder at 12 months and a lifetime history of major depression (8.3%). This result indirectly implies that generalized anxiety disorder and major depression covary over time within persons who have a history of both disorders. This is an implication that is consistent with previously reported direct evidence of a significant association between the persistence of generalized anxiety disorder and the persistence of major depression in the National Comorbidity Survey (15) and indirectly consistent with the suggestion that comorbid generalized anxiety disorder and major depression might be a distinct disorder. Second, further National Comorbidity Survey analysis, again not reported in this article, found that the majority (66.6%) of respondents with comorbid generalized anxiety disorder and major depression at 12 months also reported at least one other DSM-III-R anxiety disorder with an earlier age at onset than that of both generalized anxiety disorder and major depression. This means that the comorbidity of generalized anxiety disorder and major depression is often part of a larger anxiety-depression syndrome in which other anxiety disorders are temporally primary. This larger syndrome, which was not examined in the present report, warrants detailed examination in future research.
As noted in the introduction, some commentators have argued that comorbidity among patients with generalized anxiety disorder is so high that generalized anxiety disorder might more accurately be conceptualized as a prodrome, residual, or severity marker than as an independent disorder (6, 8). In evaluating this suggestion, it is important to appreciate that major depression is much more prevalent than generalized anxiety disorder (16). This means that the strong comorbidity between the two disorders translates into only a minority of people with major depression having comorbid generalized anxiety disorder but a majority of those with generalized anxiety disorder having comorbid major depression (15). The suggestion that generalized anxiety disorder is not an independent disorder fails to take a statistical artifact into consideration: less prevalent disorders, all else equal, have higher rates of comorbidity than more common disorders even when the strength of associations (odds ratios) of the two disorders with other disorders are identical. It is noteworthy in this regard that the comparative odds ratios of generalized anxiety disorder and major depression with other disorders in the National Comorbidity Survey are not consistently larger for generalized anxiety disorder (15). Furthermore, when we look at overall lifetime comorbidities of generalized anxiety disorder and major depression with any of the DSM-III-R disorders assessed in the National Comorbidity Survey, the rates are not dramatically different: 91% lifetime comorbidity for generalized anxiety disorder and 83% for major depression. Rates of episode comorbidity, which have been the focus of recent studies in primary care samples, are also not dramatically different for the two disorders. For example, Ormel et al. (10) found 61% episode comorbidity for generalized anxiety disorder and 63% for major depression, whereas Olfson et al. (11) found 88% episode comorbidity for generalized anxiety disorder and 66% for major depression. These rates are not so different as to argue that major depression is a true independent disorder whereas generalized anxiety disorder is not.
The issue of primary importance in this report regards the comparative impairment of generalized anxiety disorder and major depression. We found, consistent with previous research, that comorbid generalized anxiety disorder and major depression are associated with more impairment than are pure generalized anxiety disorder or pure major depression. We also found that respondents with only one of these disorders have more impairment than do respondents who have neither disorder, after adjusting for additional diagnoses and sociodemographic differences. However, more important from a nosological perspective, we also found that the impairment of pure generalized anxiety disorder is equivalent in magnitude to the impairment of pure major depression. This is true even when we control for the co-occurrence of all the other DSM-III-R disorders assessed in the two surveys. The finding of equivalent effects suggests that generalized anxiety disorder is consequential in and of itself and that its impairment is not due to other disorders. It is also important to note, although the results are not reported here, that these conclusions are insensitive to variation in the specifications of functional form. Specifically, whereas we presented results for dichotomous versions of the impairment measures, similar results were found in linear regression analyses by using continuous versions of these measures and separating submeasures such as work loss versus work cutback and the quality of relationships with friends versus relatives (results available on request from Dr. Kessler).
A question can be raised regarding the inconsistency of our findings with the conclusions of Olfson et al. (11) and Schonfeld et al. (12) in primary care samples that pure generalized anxiety disorder is not associated with significant impairment. However, it must be remembered that Olfson et al. and Schonfeld et al. studied very small numbers of respondents with pure generalized anxiety disorder, which introduced instability into their findings. The fact that significant independent effects of generalized anxiety disorder were found in the much larger and nationally representative National Comorbidity Survey and Midlife Development in the United States Survey calls the findings of Olfson et al. and Schonfeld et al. into question. The inconsistency of the results certainly suggests that this issue should be reexamined in other available data sets. However, the weight of the evidence at the moment, on the basis of the results reported here, is clear that—contrary to the suggestion that generalized anxiety disorder is better conceptualized as a prodrome, residual, or severity marker of depression rather than as an independent disorder in its own right—a substantial proportion of the cases of generalized anxiety disorder in the general population occur independently of major depression. The role impairment due to generalized anxiety disorder is comparable to that due to major depression, even after adjusting for a wide range of other comorbid disorders.
Received Nov. 9, 1998; revision received April 6, 1999; accepted May 17, 1999. From the Department of Health Care Policy, Harvard Medical School; DuPont Associates, Rockville, Md.; the Institute for Social Research, University of Michigan, Ann Arbor; and the Max Planck Institute of Psychiatry, Munich. Address reprint requests to Dr. Kessler, Department of Health Care Policy, Harvard Medical School, 180 Longwood Ave., Boston, MA 02115; [email protected] (e-mail). Supported by NIMH grants MH-46376, MH-49098, and MH-52861; National Institute on Drug Abuse grant DA-11121; W.T. Grant Foundation grant 90135190 to Dr. Kessler (National Comorbidity Survey); the John D. and Catherine T. MacArthur Foundation Network in Successful Midlife Development (Midlife Development in the United States Survey); NIMH Research Scientist Award (MH-00507) to Dr. Kessler; and an unrestricted educational grant from Wyeth-Ayerst Laboratories. The authors thank Philip Leaf and Paul Stang for their help on an earlier version of the article.
 |
 |
 |
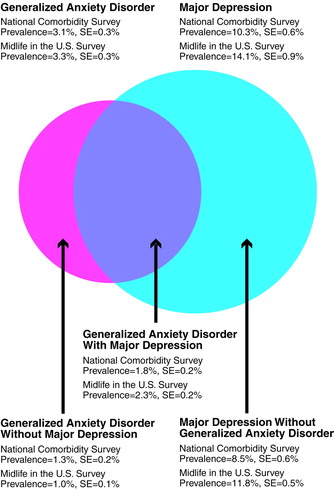
FIGURE 1. Prevalence and Comorbidity of Generalized Anxiety Disorder and Major Depression at 12 Months in Two National General Population Surveys
1. Kessler RC: The epidemiology of psychiatric comorbidity, in Textbook of Psychiatric Epidemiology. Edited by Tsuang M, Tohen M, Zahner G. New York, John Wiley & Sons, 1995, pp 179–197Google Scholar
2. Wittchen H-U, Zhao S, Kessler RC, Eaton WW: DSM-III-R generalized anxiety disorder in the National Comorbidity Survey. Arch Gen Psychiatry 1994; 51:355–364Crossref, Medline, Google Scholar
3. Kessler RC, Nelson CB, McGonagle KA, Liu J, Swartz MS, Blazer DG: Comorbidity of DSM-III-R major depressive disorder in the general population: results from the US National Comorbidity Survey. Br J Psychiatry 1996; 168:17–30Google Scholar
4. Durham RC, Allan T, Hackett CA: On predicting improvement and relapse in generalized anxiety disorder following psychotherapy. Br J Clin Psychol 1997; 36:101–119Crossref, Medline, Google Scholar
5. Brown C, Schulberg HC, Madonia MJ, Shear MK, Houck PR: Treatment outcomes for primary care patients with major depression and lifetime anxiety disorders. Am J Psychiatry 1996; 153:1293–1300Google Scholar
6. Breslau N, Davis GC: Further evidence on the doubtful validity of generalized anxiety disorder. Psychiatry Res 1985; 16:177–179Crossref, Medline, Google Scholar
7. Gorman JM: Comorbid depression and anxiety spectrum disorders. Depress Anxiety 1996–1997; 4:160–168Google Scholar
8. Nisita C, Petracca A, Akiskal HS, Galli L, Gepponi I, Cassano GB: Delimitation of generalized anxiety disorder: clinical comparisons with panic and major depressive disorders. Compr Psychiatry 1990; 31:409–415Crossref, Medline, Google Scholar
9. Roy-Byrne PP: Generalized anxiety and mixed anxiety-depression: association with disability and health care utilization. J Clin Psychiatry 1996; 57:86–91Medline, Google Scholar
10. Ormel J, Von Korff M, Ustun B, Pini S, Korten A, Oldehinkel T: Common mental disorders and disability across cultures: results from the WHO Collaborative Study on Psychological Problems in General Health Care. JAMA 1994; 272:1741–1748Google Scholar
11. Olfson M, Fireman B, Weissman MM, Leon AC, Sheehan DV, Kathol RG, Hoven C, Farber L: Mental disorders and disability among patients in a primary care group practice. Am J Psychiatry 1997; 154:1734–1740Google Scholar
12. Schonfeld WH, Verboncoeur CJ, Fifer SK, Lipschutz RC, Lubeck DP, Buesching DP: The functioning and well-being of patients with unrecognized anxiety disorders and major depressive disorder. J Affect Disord 1997; 43:105–119Crossref, Medline, Google Scholar
13. Stewart AL, Hays RD, Ware JE Jr: The MOS Short-Form General Health Survey: reliability and validity in a patient population. Med Care 1988; 26:724–735Crossref, Medline, Google Scholar
14. Spitzer RL, Kroenke K, Linzer M, Hahn SR, Williams JB, deGruy FV III, Brody D, Davies M: Health-related quality of life in primary care patients with mental disorders. JAMA 1995; 274:1511–1517Google Scholar
15. Kessler RC: The prevalence of psychiatric comorbidity, in Treatment Strategies for Patients With Psychiatric Comorbidity. Edited by Wetzler S, Sanderson WC. New York, John Wiley & Sons, 1997, pp 23–48Google Scholar
16. Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen H-U, Kendler KS: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry 1994; 51:8–19Crossref, Medline, Google Scholar
17. Kessler RC, Mickelson KD, Zhao S: Patterns and correlates of self-help group membership in the United States. Soc Policy 1997; 27:27–46Google Scholar
18. Kessler RC, Little RJA, Groves RM: Advances in strategies for minimizing and adjusting for survey nonresponse. Epidemiol Rev 1995; 17:192–204Crossref, Medline, Google Scholar
19. World Health Organization: Composite International Diagnostic Interview (CIDI), version 1.0. Geneva, WHO, 1990Google Scholar
20. Kessler RC, Wittchen H-U, Abelson JM, McGonagle KA, Schwarz N, Kendler KS, Knäuper B, Zhao S: Methodological studies of the Composite International Diagnostic Interview (CIDI) in the US National Comorbidity Survey. Int J Methods in Psychiatr Res 1998; 7:33–55Crossref, Google Scholar
21. Kessler RC, Rubinow DR, Holmes C, Abelson JM, Zhao S: The epidemiology of DSM-III-R bipolar I disorder in a general population survey. Psychol Med 1997; 27:1079–1089Google Scholar
22. Kendler KS, Gallagher TJ, Abelson JM, Kessler RC: Lifetime prevalence, demographic risk factors, and diagnostic validity of nonaffective psychosis as assessed in a US community sample: the National Comorbidity Survey. Arch Gen Psychiatry 1996; 53:1022–1031Google Scholar
23. Kessler RC, Andrews G, Mroczek D, Ustun B, Wittchen H-U: The World Health Organization Composite International Diagnostic Interview Short Form (CIDI-SF). Int J Methods in Psychiatr Res 1998; 7:171–185Crossref, Google Scholar
24. Schuster TL, Kessler RC, Aseltine RH Jr: Supportive interactions, negative interactions, and depressed mood. Am J Community Psychol 1990; 18:423–438Crossref, Medline, Google Scholar
25. Kish L, Frankel MR: Inferences from complex samples. J Royal Statistical Society 1974; 36:1–37Google Scholar
26. Schuckit MA: Genetic and clinical implications of alcoholism and affective disorder. Am J Psychiatry 1986; 143:140–147Link, Google Scholar
27. Morgado A, Smith M, Lecrubier Y, Widlocher D: Depressed subjects unwittingly over-report poor social adjustment which they reappraise when recovered. J Nerv Ment Dis 1991; 179:614–619Crossref, Medline, Google Scholar
28. Robins LN, Locke BZ, Regier DA: An overview of psychiatric disorders in America, in Psychiatric Disorders in America: The Epidemiologic Catchment Area Study. Edited by Robins LN, Regier DA. New York, Free Press, 1991, pp 328–366Google Scholar
29. Kendler KS, Walters EE, Neale MC, Kessler RC, Heath AC, Eaves LJ: The structure of the genetic and environmental risk factors for six major psychiatric disorders in women: phobia, generalized anxiety disorder, panic disorder, bulimia, major depression, and alcoholism. Arch Gen Psychiatry 1995; 52:374–383Crossref, Medline, Google Scholar
30. Sherbourne CD, Jackson CA, Meredith LS, Camp P, Wells KB: Prevalence of comorbid anxiety disorders in primary care outpatients. Arch Fam Med 1996; 5:27–34Crossref, Medline, Google Scholar
31. Shores MM, Glubin T, Cowley DS, Dager SR, Roy-Byrne PP, Dunner DL: The relationship between anxiety and depression: a clinical comparison of generalized anxiety disorder, dysthymic disorder, panic disorder, and major depressive disorder. Compr Psychiatry 1992; 33:237–244Crossref, Medline, Google Scholar
32. Pini S, Cassano GB, Simonini E, Savino M, Russo A, Montgomery SA: Prevalence of anxiety disorders comorbidity in bipolar depression, unipolar depression and dysthymia. J Affect Disord 1997; 42:145–153Crossref, Medline, Google Scholar
33. Brown TA, Chorpita BF, Barlow DH: Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. J Abnorm Psychol 1998; 107:179–192Crossref, Medline, Google Scholar
34. Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ: Major depression and generalized anxiety disorder: same genes, (partly) different environments? Arch Gen Psychiatry 1992; 49:716–722Google Scholar
35. Skodal AE, Schwartz S, Dohrenwend BP, Levav I, Shrout PE: Minor depression in a cohort of young adults in Israel. Arch Gen Psychiatry 1994; 51:542–551Crossref, Medline, Google Scholar
36. Reich J: Distinguishing mixed anxiety/depression from anxiety and depressive groups using the family history method. Compr Psychiatry 1993; 34:285–290Crossref, Medline, Google Scholar
37. Reich J: Family psychiatric histories in male patients with generalized anxiety disorder and major depressive disorder. Ann Clin Psychiatry 1995; 7:71–78Crossref, Medline, Google Scholar



