Suicide and Serious Suicide Attempts in Youth: A Multiple-Group Comparison Study
Abstract
OBJECTIVE: This study compared risk factors for suicide and medically serious nonfatal suicide attempts among youth under 25 years of age. METHOD: Three groups were examined: individuals who committed suicide (N=60), individuals who made serious suicide attempts (N=125), and nonsuicidal community comparison subjects (N=151). Suicidal and nonsuicidal subjects were compared in terms of sociodemographic, childhood, family, psychosocial, and psychiatric factors. RESULTS: Suicides were characterized by male gender, lack of educational qualifications, mood disorder, history of mental health care, and stressful life events. Except for gender, similar risk factors were associated with serious suicide attempts. Suicides and serious suicide attempts were discriminated by gender and mood disorder. Gender differences between suicides and nonfatal suicide attempts were explained by gender differences in methods. CONCLUSIONS: The same risk factors (mood disorder, history of psychiatric care, educational disadvantage, stressful circumstances) play a similar role in suicide and serious suicide attempts. Suicide and suicide attempts are discriminated by mood disorder and gender differences in methods.
In the last decade, there has been growing concern about youth suicide (1, 2). These concerns arose from evidence of increasing rates of youth suicide in many societies during the 1980s and 1990s. In New Zealand, which has one of the highest youth suicide rates among developed countries, rates of suicide among youths 15–24 years of age more than doubled during the period from 1985 to 1995 (3).
This increase in suicide rate has led to growing research into the prevalence, correlates, and etiology of suicidal behaviors in young people. However, the low prevalence of completed suicide has led to a focus on suicidal ideation and suicide attempts in young people (for reviews, see references 4–7) or to studies of completed suicide that have extended the upper age limit to 30 or 35 years (8–10). Studies that have analyzed completed suicides among youth under 25 years of age have been based on relatively small numbers of cases. In all, there have been only 13 psychological autopsy studies of suicide in the last 20 years that have focused on youth 15–24 years of age. These studies have included, in total, less than 700 subjects, the majority of whom were teenagers, and most studies were conducted in the United States (11–26).
The net result of these trends is that much of what is known about youth suicide, and most policy in this area, has been based on findings for suicidal ideation and suicide attempts supplemented by a small number of studies of completed suicide based on relatively small samples.
This conclusion raises some important issues. One issue concerns the extent to which the risk factors for attempted and completed suicide are the same. Establishing this is important to the extent that findings from studies of suicide attempts are often used as a proxy for completed suicide. However, it is clear that suicide attempts and suicide differ in some important ways. For example, while completed suicide is more common among men, the majority of suicide attempts are made by women (27). Thus, studies of suicide attempts may emphasize factors associated with female suicidal behavior at the expense of factors associated with male suicidal behavior.
This article reports on risk factors associated with serious suicide attempts and suicide among young people under 25 years of age. This study had three aims. First, risk factors for suicide were examined by comparing 60 young people who committed suicide with a series of 151 randomly selected nonsuicidal comparison subjects on a series of measures, including sociodemographic, childhood, family, psychiatric, and psychosocial factors. Second, risk factors for medically serious suicide attempts were examined by comparing a consecutive series of 125 young people who made serious suicide attempts with the 151 nonsuicidal comparison subjects. Third, risk factors for suicide and serious suicide attempts were compared by contrasting the 60 subjects who committed suicide with the 125 subjects who made serious suicide attempts. This analysis will make it possible to identify factors that discriminate young people who commit suicide from those who make serious suicide attempts.
Method
Overview
The Canterbury Suicide Project is a comparison study of subjects of all ages who committed suicide (N=202) or made a medically serious suicide attempt (N=302) and 1,028 randomly selected nonsuicidal subjects. Data for the whole case series have been analyzed previously (28). This report compares characteristics and risk factors of suicide and serious suicide attempts for subjects from this study under 25 years of age for whom data were available from interviews with “significant others” (individuals who knew the subjects well). Significant others were used as the source of information in order to provide a similar basis for comparison for all three subject groups. It is noted that analyses of the under-25 subjects have been presented previously for those who made a serious suicide attempt and the comparison subjects (see, for example, reference 29), but this is the first analysis that includes the subjects under 25 years of age who committed suicide.
Subjects
The suicide group was a consecutive series of 60 subjects under 25 years of age from the Christchurch city and Canterbury region in New Zealand who, according to coroners’ verdicts, committed suicide during the period from 1991 to 1995. Christchurch city has a population of 315,000, and the Canterbury region has a population (including Christchurch city) of approximately 430,000. During the study period, 64 individuals under 25 committed suicide; the families of 60 agreed to participate in the study, a response rate of 93.8%. Of these 60 individuals, 49 (81.7%) were male, and 11 (18.3%) were female. Their mean age was 19.98 years (SD=2.53, range=14–24). Methods of suicide included hanging (41.7%, N=25), vehicle exhaust gas (31.7%, N=19), self-poisoning (15.0%, N=9), and firearms (8.3%, N=5).
The medically serious suicide attempt group was a consecutive series of 125 individuals under 25 years of age from the Christchurch city and Canterbury region who made medically serious suicide attempts during the period from 1991 to 1994. A medically serious suicide attempt was defined as one that required hospital admission, via the sole regional Emergency Department, for >24 hours and met one of the following treatment criteria: 1) treatment in specialized units; 2) surgery under general anesthesia (superficial cuts that did not require surgical repair were excluded); or 3) extensive medical treatment, including antidotes for drug overdoses, telemetry, or repeated tests or investigations. In addition, individuals who attempted suicide by methods with a high risk of fatality, specifically, hanging or gunshot, who were hospitalized for >24 hours but did not meet the preceding treatment criteria, were also included in the group of persons with serious suicide attempts.
In total, 132 individuals made serious suicide attempts during the study period. Of these, 129 agreed to participate in the study, with 125 (96.9%) agreeing to interview information being obtained from a significant other. Of these 125 individuals, 57 (45.6%) were male, and 68 (54.4%) were female. Their mean age was 19.31 years (SD=3.1, range=13–24). Methods of serious suicide attempt included self-poisoning (77.6%, N=97), vehicle exhaust gas (11.2%, N=14), hanging (2.4%, N=3), and firearms (2.4%, N=3).
The comparison subjects for this analysis were a stratum of the comparison series from the larger study of suicidal behavior, which had been selected from regional electoral rolls. An age- and gender-stratified sample was obtained for six age strata (18–24, 25–29, 30–39, 40–49, 50–59, ≥60), with the number of subjects in each age-and-gender stratum proportional to the known age-by-gender distribution of the population 18 years of age and older. A total of 153 subjects 18–24 years of age were selected as part of the stratified sample. Of these, 151 agreed to information being obtained from a significant other, a response rate of 98.7% for significant other informants. Of these, 51.7% (N=78) were male, and 48.3% (N=73) were female. Their mean age was 21.43 years (SD=1.52, range=18–24).
Subjects selected from electoral rolls were mailed a letter of introduction explaining the study. The study interviewer then called at subjects’ homes, discussed the study, and arranged to return to conduct an interview. Each subject nominated a significant other who knew him or her well. This individual was then contacted and interviewed in person.
The study was approved by ethics committees of the Canterbury Area Health Board and the Southern Regional Health Authority. Written informed consent was obtained from all study participants after the aims and procedures of the study had been fully explained.
Risk Factors
Trained, experienced interviewers personally conducted a semistructured interview with each subject’s significant other to retrospectively construct a life history and to obtain information about risk factors for suicidal behavior.
Lethality of method
Method of suicide or suicide attempt was classified into two groups: highly lethal (hanging, vehicle exhaust gas, firearms, jumping) and less lethal (self-poisoning, cutting, and all other methods).
Sociodemographic characteristics
Two areas were assessed: socioeconomic status and educational level. Socioeconomic status was measured with the scale for socioeconomic status in New Zealand (30), which ranks the population into six groups on the basis of occupation. For the purposes of this analysis, socioeconomic status was dichotomized to give a measure of “low socioeconomic status,” defined as membership in socioeconomic status classes 5 and 6. Educational level was also dichotomized to give a measure of “no formal educational qualification,” defined as no secondary school or tertiary or trade qualification.
Family environment
The presence or absence of three items was determined: 1) parental separation or divorce; 2) poor parental relationship (i.e., parents were viewed as having gotten along “not very well” or “poorly”); and 3) childhood sexual abuse. This last item was measured by asking each significant other if, to their knowledge, the subject had been “physically or psychologically forced by anyone to engage in any unwanted sexual activity, such as unwanted sexual touching of his/her body or sexual intercourse,” a definition previously used by Murphy (1985 news release from St. Cloud State University). Those who responded positively to this question were then asked further questions relating to this issue. Subjects were classified as having a history of childhood sexual abuse if there was a positive response to the initial question and subsequent questioning established a history of childhood sexual abuse.
Stressful life events
The short list of Threatening Life Experiences (31) was used as a basis to evaluate life events that had occurred during the previous year. For the purposes of the present analysis, measures of life events were classified into a series of categories of related events: serious interpersonal difficulties, serious financial problems, serious problems with the law or police, and serious work-related problems. Subjects were classified as having a recent stressful life event if they had experienced at least one event in any of these four categories.
Psychiatric morbidity
The interviews with significant others regarding each subject included a modified version of the Structured Clinical Interview for DSM-III-R—Patient Version (32) to generate DSM-III-R diagnoses of selected mental disorders. The information was integrated in a diagnostic conference to produce, for each subject, best-estimate diagnoses of mental disorders (according to DSM-III-R criteria). In the present analysis, four diagnostic groupings were used for disorders in the month preceding the suicide event (or interview): 1) mood disorders (major depression, bipolar I disorder, bipolar II disorder); 2) substance use disorders (alcohol, cannabis, or other psychoactive substance abuse or dependence); 3) anxiety disorders (panic disorder, agoraphobia, obsessive-compulsive disorder, simple phobia, social phobia); and 4) antisocial disorder (conduct disorder or antisocial personality disorder). For antisocial disorder, a lifetime history was obtained. Multiple axis I diagnoses were permitted.
The reliability of the best-estimate diagnostic procedure was ascertained by reevaluation of a random sample of 20% of the entire group. The test-retest agreement was high, with kappa coefficients (33) for the principal diagnostic categories (mood disorders, substance use disorders, anxiety disorders, antisocial disorders) ranging from 0.95 to 0.99.
Mental health history
Two areas were assessed. The first was previous suicide attempts, or whether the subject had a history of at least one previous suicide attempt during his or her lifetime. The second was a history of contact or care for mental health problems, or whether the subject had at least one admission to a psychiatric hospital or substance abuse clinic during the previous year or a lifetime history of outpatient psychiatric treatment.
Social interaction
The Interview Schedule for Social Interaction (34) was used as a basis to evaluate the extent of current social interaction. For the purposes of this analysis the measure was dichotomized to give measures of high and low social interaction.
Statistical Analysis
Data were analyzed as three between-group comparisons. The first analysis compared the suicide group with the nonsuicidal comparison subjects; the second compared the serious suicide attempt group and the nonsuicidal comparison subjects; the third compared the suicide and serious suicide attempt groups. For each analysis, estimates of unadjusted and adjusted odds ratios and 95% confidence intervals (CIs) are reported. Estimates of the adjusted odds ratios were obtained by fitting logistic regression models in which all variables shown in the analysis were included in the model. Final models were produced by using a combination of forward and backward elimination methods to produce a stable model. The parameters and standard errors of the logistic regression model were transformed (by exponentiation) to produce corresponding estimates of the adjusted odds ratios and CIs. All cases in which tests of significance are reported are based upon the chi-square test of independence or the log likelihood chi-square. All analyses were conducted by using the SAS program LOGIST (35).
Results
Table 1 compares the 60 suicide victims and the 151 nonsuicidal comparison subjects on a series of risk factors spanning sociodemographic and psychosocial background and mental health history. The association between suicide status and each risk factor is described by the odds ratio and 95% CI. The table also reports adjusted odds ratios.
Risk of suicide was significantly associated with male gender and exposure to recent stressful life events. Other factors (lack of formal educational qualification, mood disorder in the preceding month, and history of care for mental health problems) made smaller contributions to suicide risk.
A parallel analysis compared the 125 individuals who made a serious suicide attempt with the 151 nonsuicidal comparison subjects (Table 2). With one exception (male gender), the set of risk factors associated with completed suicide was similarly predictive of serious suicide attempt. Those making serious suicide attempts were characterized by mood disorder, lack of formal educational qualifications, history of psychiatric care, and exposure to recent stressful life events.
The results in Table 1 and Table 2 suggested that, with the exception of male gender (associated with suicide but not with serious suicide attempt), a similar array of risk factors (mood disorder, psychiatric care, educational disadvantage, and stressful life events) predicted both suicide and serious suicide attempts. However, the relative weightings of these factors tended to vary with outcome, with mood disorder having a higher odds ratio for serious suicide attempt than for suicide and stressful life events having a higher odds ratio for suicide than for serious suicide attempt. These differences suggest that while the same set of etiological risk factors predicted both suicide and serious suicide attempts, the relative weightings of these factors depended on outcome (suicide/serious suicide attempt).
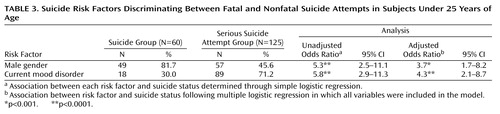
This issue is explored in Table 3, which examines the factors that discriminated between suicide and serious suicide attempt. Suicide and serious suicide attempt were discriminated by two factors: gender and mood disorder. Suicide victims were more often male, whereas serious suicide attempters tended to have higher rates of mood disorder.
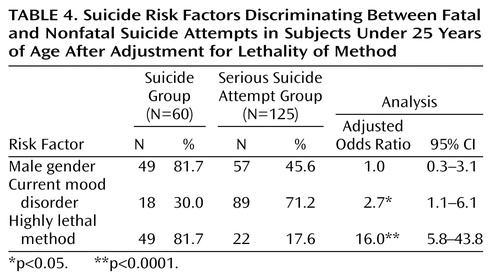
To explore reasons for the gender difference in suicidal outcome (i.e., suicide versus serious suicide attempt) reported in Table 3, a supplementary logistic regression analysis was conducted. This regression included mood disorder, gender, and method of suicide/suicide attempt. Method of suicide/suicide attempt was a dichotomous variable that classified methods into two groups: highly lethal and less lethal. The results of this analysis are summarized in Table 4. While mood disorder and method were predictors of the difference between suicide and serious suicide attempt, gender was not a predictor (p>0.50). The implication of this finding is that the gender-related differences in suicide and serious suicide attempt (Table 3) were largely explained by gender-related differences in method choice. In particular, 61.3% of all male fatal and nonfatal suicide attempts involved highly lethal methods (hanging, vehicle exhaust gas, firearms, jumping). In contrast, 92.4% of all female fatal and nonfatal serious suicide attempts involved less lethal methods, particularly self-poisoning. Table 4 shows that the predominance of more lethal methods used by the male subjects explains their higher rate of suicide.
Discussion
This study used multiple between-group comparisons to analyze a series of 60 suicide victims, 125 serious suicide attempters, and 151 nonsuicidal comparison subjects under 25 years of age. Information for all three subject groups was provided by reports from significant others to provide a common basis for comparison.
The present study confirms previous research that has linked suicide and suicide attempts to a series of factors, including gender, economic and educational disadvantage, childhood and family adversity, mental health problems (particularly mood disorder), and exposure to stressful circumstances (11–25, 36). In the present study, rates of suicide were elevated among men, those with mood disorders, those with a history of psychiatric care, those who lacked formal educational qualifications, and those with exposure to stressful life events. With the exception of male gender, which was associated with suicide but not with serious suicide attempts, a similar set of risk factors was associated with risk of medically serious suicide attempt. Those making a serious suicide attempt had higher rates of mood disorder, psychiatric care, educational disadvantage, and exposure to stressful life events. Clearly, youth suicides and medically serious suicide attempts are two overlapping populations that had many risk factors in common. However, there were some differences between the two populations. Those who committed suicide were much more likely to be male than were those who made suicide attempts, and serious suicide attempters were more likely than those who committed suicide to have a mood disorder at the time of their attempt.
The fact that male subjects were more likely than female subjects to commit suicide was completely explained by the male subjects’ use of more immediately lethal methods. While the majority of male subjects who committed suicide used hanging, vehicle exhaust gas, firearms, and jumping, the majority of serious suicide attempts by female subjects were by self-poisoning, a method which, while it may have high toxicity, tends to have low lethality and a relatively slow rate of action. While previous research has suggested that the choice by men of more immediately lethal methods may contribute to their higher suicide rates (15, 20, 37), the results of this study suggest that, at least among those young people who make serious suicide attempts, gender differences in outcome are completely explained by method choice. The important implication of this finding is that if women were to adopt more lethal methods, then the female suicide rate may approach or even exceed the male suicide rate (owing to the larger number of suicide attempts made by women). There is some evidence of the effect of shifts in method choice on female suicide rates from New Zealand. In particular, rates of female youth suicide in New Zealand more than doubled from 1977 to 1996, with this increase accounted for, almost entirely, by the growing use of hanging and vehicle exhaust gas by women (38).
Further evidence on the role of gender-related method choice in suicide may be found in suicide data from China, which show a higher rate of suicide in young women than in young men, contrary to the male excess in suicides seen in Western societies. The higher female rate in China is most likely explained by the ready access that Chinese women have to agricultural pesticides, which are used in self-poisoning attempts and have high lethality (39).
The male gender dominance in completed suicide has often been portrayed as reflecting a greater male vulnerability to suicide (40, 41). However, the present analysis suggests that this male vulnerability is not fundamental to the development of suicidal behaviors. Rather, the higher rate of suicide among men in Western societies arises from culturally determined gender preferences in method choices. Notwithstanding this, the possibility remains that other gender-specific factors, such as aggressivity and substance use, may in some contexts contribute to higher male suicide rates.
The suicide and serious suicide attempt populations were also discriminated by mood disorder, with those dying by suicide having a significantly lower rate of mood disorder (30%) than those making serious suicide attempts (71.2%). There are two possible explanations for this association. First, it may be that while the development of mental disorders (particularly mood disorders) encourages young people to make suicide attempts, these disorders may impair the effectiveness of the attempt, leading to a situation in which mood disorder is more common among those making serious (but nonfatal) suicide attempts. Alternatively, this result may reflect errors of measurement in the assessment of psychopathology. It will be recalled that in order to compare suicide victims, suicide attempters, and nonsuicidal comparison subjects on the same basis, data from significant others were used to form psychiatric diagnoses. It could be suggested that this might have resulted in the prevalence of mood disorders among those committing suicide being underestimated relative to the prevalence of those making serious suicide attempts. Significant others would have been able to confirm the presence of mood disorder among those making a serious suicide attempt. This would not be possible in the case of those who committed suicide. In this respect, it should be noted that the rate of mood disorder found among the suicide series was relatively low (30%) but was within the range reported in previous psychological autopsy studies (16%–76%) (42, 43). At this stage it is not possible to ascertain which of these explanations is the more likely. Nonetheless, this result raises the distinct possibility that mood disorder may play a lesser etiological role in completed suicides than in serious suicide attempts.
The strengths of this study include the multiple-group comparisons and the relatively large group sizes. The limitations include the focus on medically serious suicide attempts and, as discussed above, possible biases and errors arising from the use of significant other data used to describe psychopathology in young people.
 |
 |
 |
 |
Received May 9, 2002; revision received Dec. 13, 2002; accepted Jan. 2, 2003. From the Canterbury Suicide Project. Address reprint requests to Dr. Beautrais, Canterbury Suicide Project, Christchurch School of Medicine, P.O. Box 4345, Christchurch, New Zealand; [email protected] (e-mail). Funded by a grant from the Health Research Council of New Zealand and supported by Healthlink South and the Canterbury Area Health Board.
1. National Strategy for Suicide Prevention: Goals and Objectives for Action. Rockville, Md, US Department of Health and Human Services, 2001Google Scholar
2. Figures and Facts About Suicide. Geneva, World Health Organization, Department of Mental Health, 1999Google Scholar
3. New Zealand Ministry of Health: Suicide Trends in New Zealand 1978-1998. Wellington, New Zealand, New Zealand Health Information Service, 2001Google Scholar
4. Beautrais AL: Risk Factors for Suicide and Attempted Suicide Amongst Young People. Canberra, Australia, National Health and Medical Research Council, 2000Google Scholar
5. de Wilde EJ: Adolescent suicidal behaviour: a general population perspective, in The International Handbook of Suicide and Attempted Suicide. Edited by Hawton K, van Heeringen K. New York, John Wiley & Sons, 2000, pp 249-259Google Scholar
6. Gould MS, Kramer RA: Youth suicide prevention. Suicide Life Threat Behav 2001; 31:6-31Crossref, Medline, Google Scholar
7. Spirito A, Brown L, Overholser J, Fritz G: Attempted suicide in adolescence: a review and critique of the literature. Clin Psychol Rev 1989; 9:335-363Crossref, Google Scholar
8. Appleby L, Cooper J, Amos T, Faragher B: Psychological autopsy study of suicides by people aged under 35. Br J Psychiatry 1999; 175:168-174Crossref, Medline, Google Scholar
9. Lesage AD, Boyer R, Grunberg F, Vanier C, Morissette R, Menard-Buteau C, Loyer M: Suicide and mental disorders: a case-control study of young men. Am J Psychiatry 1994; 151:1063-1068Link, Google Scholar
10. Runeson B: Mental disorder in youth suicide: DSM-III-R axes I and II. Acta Psychiatr Scand 1989; 79:490-497Crossref, Medline, Google Scholar
11. Apter A, Bleich A, King RA, Kron S, Fluch A, Kotler M, Cohen DJ: Death without warning? a clinical postmortem study of suicide in 43 Israeli adolescent males. Arch Gen Psychiatry 1993; 50:138-142Crossref, Medline, Google Scholar
12. Brent DA, Perper JA, Goldstein CE, Kolko DJ, Allan MJ, Allman CJ, Zelenak JP: Risk factors for adolescent suicide: a comparison of adolescent suicide victims with suicidal inpatients. Arch Gen Psychiatry 1988; 45:581-588Crossref, Medline, Google Scholar
13. Brent DA, Perper JA, Moritz G, Allman C, Friend A, Roth C, Schweers J, Balach L, Baugher M: Psychiatric risk factors for adolescent suicide: a case-control study. J Am Acad Child Adolesc Psychiatry 1993; 32:521-529Crossref, Medline, Google Scholar
14. Brent DA, Bridge J, Johnson BA, Connolly J: Suicidal behavior runs in families: a controlled family study of adolescent suicide victims. Arch Gen Psychiatry 1996; 53:1145-1152Crossref, Medline, Google Scholar
15. Brent DA, Baugher M, Bridge J, Chen T, Chiappetta L: Age- and sex-related risk factors for adolescent suicide. J Am Acad Child Adolesc Psychiatry 1999; 38:1497-1505Crossref, Medline, Google Scholar
16. Eisele JW, Frisino J, Haglund W, Reay DT: Teenage suicide in King County, Washington, II: comparison with adult suicide. Am J Forensic Med Pathol 1987; 8:210-216Crossref, Medline, Google Scholar
17. Gould MS, Fisher P, Shaffer D, Parides M, Flory M: Psychosocial risk factors of child and adolescent completed suicide. Arch Gen Psychiatry 1996; 53:1155-1162Crossref, Medline, Google Scholar
18. Houston K, Hawton K, Shepperd R: Suicide in young people aged 15-24: a psychological autopsy study. J Affect Disord 2001; 63:159-170Crossref, Medline, Google Scholar
19. Leblhuber F, Schony W, Fischer F, Sommereder M, Kienbacher G: Study on suicides committed by adolescents in upper Austria covering a period of three years, in Depression and Suicide. Edited by Soubrier JP, Vedrienne J. Paris, Pergamon Press, 1983, pp 652-655Google Scholar
20. Marttunen MJ, Aro HM, Henriksson MM, Lonnqvist JK: Mental disorders in adolescent suicide: DSM-III-R axes I and II diagnoses in suicides among 13- to 19-year-olds in Finland. Arch Gen Psychiatry 1991; 48:834-839Crossref, Medline, Google Scholar
21. Marttunen MJ, Aro HM, Lonnqvist JK: Adolescent suicide: endpoint of long-term difficulties. J Am Acad Child Adolesc Psychiatry 1992; 31:649-654Crossref, Medline, Google Scholar
22. Rich CL, Sherman M, Flowler RC: San Diego Suicide Study: the adolescents. Adolescence 1990; 25:855-865Medline, Google Scholar
23. Shaffer D, Gould MS, Fisher P, Trautman P, Moreau D, Kleinman M, Flory M: Psychiatric diagnosis in child and adolescent suicide. Arch Gen Psychiatry 1996; 53:339-348Crossref, Medline, Google Scholar
24. Shafii M, Carrigan S, Whittinghill JR, Derrick A: Psychological autopsy of completed suicide in children and adolescents. Am J Psychiatry 1985; 142:1061-1064Link, Google Scholar
25. Shafii M, Steltz-Lenarsky J, Derrick AM, Beckner C, Whittinghill JR: Comorbidity of mental disorders in the post-mortem diagnosis of completed suicide in children and adolescents. J Affect Disord 1988; 15:227-233Crossref, Medline, Google Scholar
26. Groholt B, Ekeberg O, Wichstrom L, Haldorsen T: Suicide among children and younger and older adolescents in Norway: a comparative study. J Am Acad Child Adolesc Psychiatry 1998; 37:473-481Crossref, Medline, Google Scholar
27. Suicide among children, adolescents, and young adults—United States, 1980-1992. MMWR Morb Mortal Wkly Rep 1995; 44:289-291Medline, Google Scholar
28. Beautrais AL: Suicides and serious suicide attempts: two populations or one? Psychol Med 2001; 31:837-845Crossref, Medline, Google Scholar
29. Beautrais AL, Joyce PR, Mulder RT: Psychiatric contacts among youths aged 13 through 24 years who made serious suicide attempts. J Am Acad Child Adolesc Psychiatry 1998; 37:504-511Crossref, Medline, Google Scholar
30. Elley WB, Irving JC: Revised socio-economic index for New Zealand. New Zealand J Educational Studies 1976; 11:25-36Google Scholar
31. Brugha T, Bebbington P, Tennant C, Hurry J: The list of threatening experiences: a subset of 12 life event categories with considerable long-term contextual threat. Psychol Med 1985; 15:189-194Crossref, Medline, Google Scholar
32. Spitzer RL, Williams JBW, Gibbon M, First MB: Structured Clinical Interview for DSM-III-R—Patient Version (SCID-P). New York, New York State Psychiatric Institute, Biometrics Research, 1988Google Scholar
33. Fleiss JL: Statistical Methods for Rates and Proportions, 2nd ed. New York, John Wiley & Sons, 1981Google Scholar
34. Henderson S, Duncan-Jones P, Bryne DG, Scott R: Measuring social relationships: the Interview Schedule for Social Interaction. Psychol Med 1980; 10:723-734Crossref, Medline, Google Scholar
35. SAS/STAT Software: Changes and Enhancements Through Release 6.12, Cary, NC, SAS Institute, 1997Google Scholar
36. Hawton K, Fagg J: Suicide, and other causes of death, following attempted suicide. Br J Psychiatry 1988; 152:359-366Crossref, Medline, Google Scholar
37. Rich CL, Ricketts JE, Fowler RC, Young D: Some differences between men and women who commit suicide. Am J Psychiatry 1988; 145:718-722Link, Google Scholar
38. Beautrais AL: Methods of youth suicide in New Zealand: trends and implications for prevention. Aust NZ Psychiatry 2000; 34:413-419Crossref, Medline, Google Scholar
39. Phillips MR, Li X, Zhang Y: Suicide rates in China, 1995-1999. Lancet 2002; 359:835-840Crossref, Medline, Google Scholar
40. Arora RC, Meltzer HY: Serotonergic measures in the brains of suicide victims: 5-HT2 binding sites in the frontal cortex of suicide victims and control subjects. Am J Psychiatry 1989; 146:730-736Link, Google Scholar
41. Moscicki EK: Gender differences in completed and attempted suicides. Ann Epidemiol 1994; 4:152-158Crossref, Medline, Google Scholar
42. Marttunen MJ, Aro HM, Lonnqvist JK: Adolescence and suicide: a review of psychological autopsy studies. Eur Child Adolesc Psychiatry 1993; 2:10-18Crossref, Medline, Google Scholar
43. Flisher AJ: Annotation: mood disorder in suicidal children and adolescents: recent developments. J Child Psychol Psychiatry 1999; 40:315-324Crossref, Medline, Google Scholar



