Longitudinal Course of Posttraumatic Stress Disorder and Posttraumatic Stress Disorder Symptoms in a Community Sample of Adolescents and Young Adults
Abstract
OBJECTIVE: Few studies have focused on the natural course of posttraumatic stress disorder (PTSD) and its determinants in samples of the general population. The authors examined determinants of remission and chronicity of PTSD and associations with other disorders in a prospective community sample. METHOD: The data were drawn from a prospective, longitudinal epidemiological study of adolescents and young adults (age 14–24 years) in Munich, Germany (N=2,548). The course of PTSD from baseline to follow-up 34–50 months later was studied in 125 respondents with DSM-IV PTSD or subthreshold PTSD at baseline. RESULTS: Although 52% of the PTSD cases remitted during the follow-up period, 48% showed no significant remission of PTSD symptoms. Respondents with a chronic course were more likely to experience new traumatic event(s) during follow-up (odds ratio=5.21, 95% confidence interval [CI]=1.95–13.92), to have higher rates of avoidant symptoms at baseline (odds ratio=10.16, 95% CI=1.73–59.51), and to report more help seeking (odds ratio=5.50, 95% CI=1.04–29.05), compared to respondents with remission. Rates of incident somatoform disorder (odds ratio=4.24, 95% CI=1.60–11.19) and other anxiety disorders (odds ratio=4.07, 95% CI=1.15–14.37) were also significantly associated with a chronic course. CONCLUSIONS: PTSD is often a persistent and chronic disorder. Specific symptom clusters—especially avoidant symptoms—might be associated with the course of PTSD. In addition, the occurrence of new traumatic events differentiates PTSD cases with a chronic course from those with remission.
Posttraumatic stress disorder (PTSD) is a prevalent disorder for which overall community lifetime prevalence estimates range from a minimum of 1% in earlier DSM-III studies to a maximum of 12.3% in more recent surveys (1–8).
A few epidemiological studies, most of them retrospective, have focused on the natural course of PTSD and its determinants. Chronic DSM-III or DSM-III-R PTSD was frequently reported in rape victims, victims of torture and political violence, refugees, and combat veterans (9–11). Kilpatrick et al. (9) reported that 16.5% of women who had been raped continued to meet PTSD diagnostic criteria an average of 17 years afterward. Risk factors for lifetime chronic (duration at least 1 year) PTSD have been reported for a random sample of young adults in the Detroit metropolitan area by Breslau and Davis (10). Compared to young adults with nonchronic PTSD, those with chronic PTSD had a higher number of DSM-III-R PTSD symptoms and higher rates of interpersonal numbing and overreactivity to stimuli that symbolized the stressor, as well as higher rates of psychiatric comorbidity and other medical conditions. Davidson et al. (11) noted significant differences between chronic and acute DSM-III PTSD in a general population sample; chronic PTSD was associated with reduced social support, a greater frequency of social phobia, and greater avoidant symptoms.
Most of our knowledge of the course of PTSD and its determinants is based on prospective (12–15) or retrospective (16) cohort studies involving people who have experienced specific types of traumatic events (e.g., natural disasters). For example, a prospective study among Australian firefighters reported a 30% rate of PTSD identified by assessment with the General Health Questionnaire 29 months after a bush fire (14). Retrospective data from adult survivors of the Buffalo Creek flood showed that after 14 years, 28% of the survivors with PTSD still had not had remission (15). Results from the National Vietnam Veterans Readjustment Study showed that 15% of all male Vietnam veterans still had PTSD 19 years after combat exposure (16). Some studies found that specific symptom clusters and clinical features fluctuated over time and sometimes increased in intensity after several decades of decline (14). Furthermore, numerous pre-, peri-, and postexposure risk factors have been reported, suggesting a multifactorial model of longitudinal course with various pathways (14). For example, studies of acute stress reactions or acute stress disorder provided support for associations between the immediate response after a traumatic event (i.e., acute motor restlessness) and the longitudinal course of PTSD (17). Some studies suggested a significant role of cognitive processing style (18), coping behavior (13), and social support (19). However, generalizability of these findings is an unresolved issue.
Several epidemiological studies have shown that PTSD is strongly associated with comorbid disorders (1, 5, 20). Most of these findings are based on retrospective or cross-sectional data, and the causal explanations of psychiatric sequelae or temporal associations between PTSD and other disorders are unclear (21, 22). The few extant studies on the course of PTSD and psychiatric risk factors showed that other anxiety disorders and depressive symptoms after the onset of PTSD are related to a more chronic course (12, 23). However, no studies with an epidemiological and longitudinal approach have assessed a broader range of psychiatric risk factors after various types of traumatic events in the general population.
The high degree of comorbidity was also confirmed in a community sample of adolescents and young adults ages 14–24 years in the Early Developmental Stages of Psychopathology study (5). We previously reported that 1.3% of the baseline sample (0.4% of male respondents and 2.2% of female respondents) and approximately 8% of those who reported traumatic events fulfilled the DSM-IV criteria for PTSD. PTSD and traumatic events were strongly associated with other DSM-IV disorders that occurred as either a primary or secondary disorder before or after the onset of PTSD. We also previously reported the patterns of incidence of PTSD in this community sample (24).
In this article, we report results from the follow-up component of the Early Developmental Stages of Psychopathology study, which focused on the 42-month longitudinal course of PTSD and PTSD symptoms. We explored the following questions:
| 1. | How many persons with subthreshold PTSD or full PTSD at baseline had entire or partial remission of PTSD during the follow-up period? | ||||
| 2. | How do persons with a chronic course differ from persons who experience remission(s) during follow-up with respect to specific PTSD characteristics and risk factors? | ||||
| 3. | Is a chronic course of PTSD associated with the onset of other disorders? | ||||
Method
Sample and Overall Design
The data presented here were collected as part of the Early Developmental Stages of Psychopathology study (25, 26). The Early Developmental Stages of Psychopathology study was designed as a prospective-longitudinal survey to explore prevalence and incidence, familial and other risk factors, and comorbidity and course of mental disorders in a population sample of adolescents and young adults randomly and proportionally drawn from regional registries to represent the distribution of persons age 14–24 years in the area. After complete description of the study to the subjects, written informed consent was obtained.
The study was divided into three waves. The first wave was conducted in 1995 (baseline) and included the representative sample of persons age 14–24 years (N=3,021). The second wave was conducted in 1996–1997 (time 1) and included only respondents who were age 14–17 years at baseline (N=1,228). The third wave was conducted in 1998–1999 (time 2) and again included all respondents who were age 14–24 years at baseline (N=2,548). Detailed information on the sampling procedure has been reported elsewhere (25). Briefly, at baseline, a total of 3,021 interviews were completed (response rate=71%). The first follow-up (time 1), among the respondents who were age 14–17 years at baseline, was conducted an average of 19.7 months (range=15–25.6) after the baseline interviews (response rate=88%). The second follow-up (time 2), which was intended to include all baseline participants, was conducted in 1998–1999, an average of 42 months (range=34–50) after the baseline interviews (response rate=84%). The findings reported here are based on baseline and second follow-up data (N=2,548). For the younger cohort (respondents age 14–17 years at baseline), information from the first follow-up (i.e., on new traumatic events) was added.
The sociodemographic characteristics of the baseline and entire follow-up (baseline to time 2) sample have been published (5, 26). Briefly, at baseline, most of the respondents were attending school (89%) and living with their parents (97.8%). About 10% were in job training. The majority was classified as belonging to the middle class (61.4%). Noteworthy changes in sociodemographic characteristics from baseline to the second follow-up were found for school status (42% were attending school at follow-up) and employment status (24% were in a job training program and 12% were employed at follow-up).
Diagnostic Assessment
Diagnostic assessments at the baseline and the two follow-up investigations were based on the computer-assisted personal version of the Munich-Composite International Diagnostic Interview (27), which allows for the assessment of symptoms, syndromes, and diagnoses of 48 mental disorders according to the DSM-IV criteria and for collection of data on onset, duration, severity, and psychosocial impairment. Diagnostic findings were obtained by using the Munich-Composite International Diagnostic Interview/DSM-IV algorithms. At baseline, the lifetime version of the Munich-Composite International Diagnostic Interview was used. At each follow-up, the interval version was applied. In all assessments, the Munich-Composite International Diagnostic Interview was supplemented by a separate respondents’ booklet that included several scales and questionnaires for assessing psychological constructs relevant to the study (26). For the purpose of this examination, we additionally used a self-competence scale (28). Test-retest reliability and validity of the full Munich-Composite International Diagnostic Interview, along with descriptions of the Munich-Composite International Diagnostic Interview format and coding conventions, have been reported in detail elsewhere (29, 30). The test-retest reliability of the diagnostic modules of the Munich-Composite International Diagnostic Interview was fair to good, with kappa values ranging from 0.64 (Yule’s Y=0.80) to 0.78 (Yule’s Y=0.82). In tests of validity, a good concordance between clinicians’ diagnoses and interview DSM-IV diagnoses was found for all disorders (kappa=0.50–0.96) except psychotic disorders (kappa=0.21).
Posttraumatic stress disorder (and other mental disorders) was defined according to the DSM-IV criteria by using the Munich-Composite International Diagnostic Interview diagnostic algorithm (27). Details of PTSD diagnosis have been presented previously (5). Briefly, a screening question, a written list of 10 groups of potentially traumatic events, and an open-ended question about any other traumatic events (to avoid the necessity of speaking about embarrassing and stigmatizing traumas) were presented, followed by questions about the presence of the DSM-IV A2 criterion (intense fear, helplessness, or horror) during each reported event and questions that probed for the most severe (i.e., most distressing to the individual) event, as well as linkages between events. If the respondent indicated several qualifying events (fulfilling the DSM-IV A1 and A2 criteria) that did not cluster, only the criteria for the most distressing event were assessed by asking which of the events had been the most upsetting at the time it occurred. For this report, the 10 specific event types plus the open category were grouped into a category with two exclusive groups: assaultive events (horrific experience during war, imprisonment, being taken hostage or kidnapped, physical attacks, sexual abuse, and rape) and nonassaultive events (serious accidents, experience of natural catastrophes, sudden death or threat of death of associates, and witnessing traumatic events that happened to others). Similar categories have been used in other studies (31). One-week test-retest reliability of the Munich-Composite International Diagnostic Interview PTSD section was acceptable (kappa=0.79), as was the validity (kappa=0.85) assessed by using the diagnostic concordance between the Munich-Composite International Diagnostic Interview diagnosis and the clinical diagnosis (29, 30).
For this report, we specified two additional categories: “subthreshold PTSD” and “PTSD symptoms.” The category of subthreshold PTSD refers to persons who fulfilled the A, B (traumatic event, fear, and persistent reexperiences), and E criteria (duration) for DSM-IV PTSD but did not completely fulfill the C (avoidance or numbing of general responsiveness) and/or D criteria (increased arousal), although they reported at least one symptom of each of the C and D criteria categories with a duration of more than 1 month. The DSM-IV criterion of impairment was not required (although it was met by some respondents with subthreshold PTSD). Similar subthreshold diagnoses of PTSD have been discussed in the literature (32). The category of “PTSD symptoms” at follow-up refers to persons who fulfilled the A and the B criteria of DSM-IV PTSD but did not meet the criteria for full or subthreshold PTSD. The course specifiers of a chronic course or remission refer to the time between the baseline and second follow-up interviews and describe transitions from subthreshold PTSD to full DSM-IV PTSD, unchanged status between baseline and second follow-up, or transitions to remission (not fulfilling the criteria for the categories defined earlier). Partial remission with PTSD symptoms was included in the category of chronic course. Only persons who failed to meet the criteria for DSM-IV PTSD or our operational criteria for subthreshold PTSD or PTSD symptoms (as described earlier) were considered to have remission for the purpose of this investigation.
Statistical Analysis
Data were weighted to consider different sampling probabilities as well as systematic nonresponse at baseline. The Stata software package (33) was used to calculate proportions and standard errors as well as robust confidence intervals (CIs) for weighted data. Multiple logistic regression analyses with odds ratios were used to describe significant differences between the respondents with remission and those with a chronic course. Logistic regression analyses with adjustment for age and gender were used to calculate odds ratios for incident disorders (i.e., first onset) in the two course specifier groups; the total follow-up sample (without respondents with PTSD) was used as the reference group. Persons with a preexisting case (at baseline) of any of the disorders considered in the analysis of incident disorders were excluded from each of these regression analyses because they were not at risk for the incidence of that disorder. In addition, to avoid confounding findings with new traumatic events, we conducted all logistic regression analyses using data from a sample that excluded persons who experienced new traumatic events between baseline and follow-up. We did not find selective attrition from baseline to follow-up relevant to our categories of DSM-IV PTSD and subthreshold PTSD.
Results
Diagnostic and Symptom Status From Baseline to the Second Follow-Up
As Table 1 shows, at baseline 5.7% (N=125) of the respondents age 14–24 years fulfilled the criteria for either subthreshold PTSD (4.4%) or full DSM-IV PTSD (1.3%). The proportion of female respondents was significantly higher among respondents with full PTSD (83.9%) (odds ratio=5.22, 95% CI=1.61–16.80).
A total of 56.7% of respondents with subthreshold PTSD at baseline and 42.9% of those with full PTSD at baseline reported not meeting the criteria for PTSD symptoms at either the first or the second follow-up assessment, for an overall remission rate of 52% (N=65). The probability of having full DSM-IV PTSD at the second follow-up was highest among respondents with baseline full PTSD (25.6%); only 4.2% of those with subthreshold PTSD at baseline progressed to full PTSD. The remaining 48% of those with full or subthreshold PTSD at baseline reported experiencing full or subthreshold PTSD or PTSD symptoms during the follow-up periods and were classified as having a chronic course (N=60). There were no significant differences in the distribution of respondents with subthreshold PTSD and with full PTSD in the two course specifier groups (difference between remission and a chronic course among respondents with subthreshold PTSD: odds ratio=0.57, 95% CI=0.21–1.59; difference between remission and a chronic course among respondents with full PTSD: odds ratio=1.74, 95% CI=0.62–4.84). However, 44.5% of those with subthreshold PTSD and 22.6% of those with full PTSD experienced new traumatic events during the follow-up period (odds ratio=2.57, 95% CI=1.64–4.02; odds ratio=0.89, 95% CI=0.36–2.22, respectively).
Differences Between Complete Remission and a Chronic Course
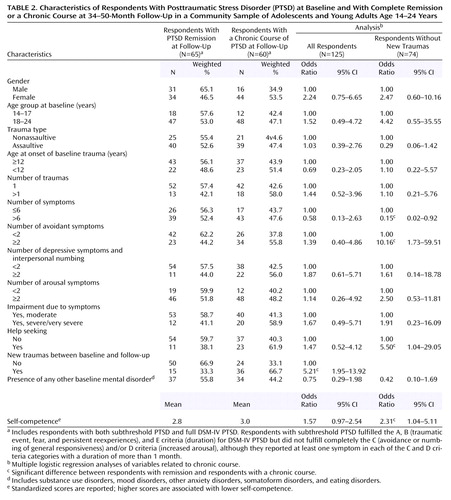
Table 2 shows differences in certain baseline PTSD characteristics and additional factors between respondents with full remission and those with a chronic course. Overall, respondents with a chronic course had higher rates of most of the PTSD characteristics and other risk factors that were assessed, except for assaultive trauma types, number of symptoms, and presence of other baseline mental disorders.
To identify core variables associated with chronicity, we performed multiple logistic regression analyses with all significant variables from Table 2. The experience of new traumatic events between baseline and follow-up was the most robust and significant difference between the two course specifier groups (odds ratio=5.21, 95% CI=1.95–13.92). To avoid confounding between the other predictors and new traumatic events, we also performed the multiple logistic regression analyses using data from the subsample of respondents who had not experienced new traumatic events. Significant differences between the two course specifier groups were found for avoidant symptoms (odds ratio=10.16, 95% CI=1.73–59.51), help seeking (odds ratio=5.50, 95% CI=1.04–29.05), and self-competence (odds ratio=2.31, 95% CI=1.04–29.05). The number of symptoms, however, was negatively associated with chronicity (odds ratio=0.15, 95% CI=0.02–0.92).
Incident Disorders During Follow-Up
Table 3 shows associations between the two course specifiers and other incident mental disorders with onset during the follow-up period among persons who had never before fulfilled the criteria for these disorders. We did not directly compare differences between the two groups, but we compared rates of onset of new disorders in the two groups with the rates of incident disorders during follow-up in the total sample of respondents with no PTSD and no history of the specific disorder at baseline. In addition, to avoid confounding of new traumatic events and the onset of other disorders, we conducted the analysis with data from a subset of persons who had not experienced new traumatic events.
Both course specifier groups experienced other incident disorders during the follow-up period, but the overall rate was not significantly different in the category “any disorder” from the rate of follow-up disorders in the reference group. However, although we found no significant odds ratios for specific incident disorders among respondents with remission of PTSD at follow-up, a chronic PTSD course was significantly associated with higher rates of incident somatoform disorders (odds ratio=4.24, 95% CI=1.60–11.19) and incident other anxiety disorders (odds ratio=4.07, 95% CI=1.15–14.37) during the follow-up period. Table 3 also shows that new traumatic events were specifically associated with incident mood disorders among those with a chronic course (odds ratio=2.46, 95% CI=1.12–5.41).
Discussion
The key findings of the study are as follows: More than one-half of the sample with full DSM-IV PTSD at baseline remained symptomatic for more than 3 years, and more than one-half fulfilled the criteria for subthreshold PTSD or DSM-IV PTSD at 34–50-month follow-up. Nearly one-half of those with subthreshold PTSD at baseline remained symptomatic or fulfilled the criteria for subthreshold PTSD or DSM-IV PTSD at follow-up. These estimates are close to those from other epidemiological studies in older populations (1, 14).
Compared to our previous findings and findings from other studies, the predictors of course partly seemed to differ from the predictors of traumatic events and predictors of the onset of PTSD. For example, an early onset and number of traumas were not significantly associated with the course of PTSD in this sample. However, the experience of new traumas during the follow-up interval distinguished a chronic course from a more favorable course with remission. Furthermore, a higher number of avoidant symptoms (from cluster C) at baseline predicted a chronic course. Higher self-competence, which may indicate a greater ability to cope with the effects of recurrent or new traumatic events, was associated with a lower risk of chronicity. It remains to be shown whether these results are stable during a longer course of illness or whether they reflect fluctuating symptoms (14). It is further noteworthy that we found no significant differences for other baseline disorders between respondents with remission and those with a chronic course. This finding might be related to the high rate of comorbidity of other disorders at baseline in both groups (more than 50%).
However, a chronic course of PTSD seems to be significantly associated with incident disorders during follow-up. A higher risk of somatoform disorders or syndromes in persons with PTSD has often been described (34) and was associated with a chronic course in our study. The lack of association between mood disorders and chronicity was somewhat surprising and may be an artifact of the low number of cases of depression in this young adult sample. The role of depression in relation to traumatic events and PTSD has been discussed in the literature, and further empirical evidence in larger samples is required, especially with regard to the course of PTSD (22). Although previous research found associations between substance use disorders and PTSD (5), we could not show that incident substance use disorders were significantly related to course during this relatively brief follow-up period.
Some limitations of the study should be addressed. The findings were restricted to a small number of respondents with full syndromal cases of DSM-IV PTSD at baseline and follow-up. But, as we have noted previously, in this representative community sample of adolescents and young adults, the prevalence of full-blown DSM-IV PTSD is lower than in other epidemiological studies (5). It is also possible that our findings from this relatively young, urban German community sample, which consisted of well-educated persons from an area with a relatively high economic status, may not generalize to other populations. Our definition of remission refers to the lack of PTSD criterion B (reexperiencing) and E (duration), but it is possible that some persons might have residual symptoms confined to avoidance and/or hyperarousal. Although one might question whether lack of criterion B and E symptoms constitutes remission, we felt that continuing to refer to these persons as having PTSD-related symptoms was less than parsimonious, because such symptoms might be attributable to other DSM disorders. Finally, our findings on course may not generalize to the course after exposure to specific types of traumatic events that were rare or did not occur at all in the present sample (such as natural catastrophes or terrorist attacks).
In conclusion, the results of this longitudinal study confirm in a prospective cohort that PTSD is often a persistent and chronic disorder. In adolescents and young adults, exposure to new traumatic events and seeking help for PTSD symptoms (which may be either an indicator of severity or of coping ability) are associated with poorer outcomes. Avoidant symptoms in particular seem to predict a chronic course. Efforts to prevent persons from being exposed to new traumatic events during the course of PTSD could lessen the chronicity of this disorder. Prevention may be achieved through the implementation of therapies that include techniques for teaching individuals how to seek safe living environments and nonabusive social and romantic relationships (35). The role of other comorbid disorders (e.g., anxiety and somatoform disorders) in influencing the course of PTSD and the possibility that concurrent treatment of these symptom domains might reduce chronicity require further investigation.
 |
 |
 |
Received April 23, 2003; revision received June 23, 2004; accepted Aug. 18, 2004. From the Department of Clinical Psychology and Epidemiology, Max Planck Institute of Psychiatry; the Department of Clinical Psychology and Psychotherapy, University of Technology, Dresden, Germany; and the Department of Psychiatry, University of California San Diego, La Jolla, Calif. Address correspondence and reprint requests to Dr. Perkonigg, Clinical Psychology and Epidemiology Department, Max Planck Institute of Psychiatry, Kraepelinstr. 2–10, D-80804 Munich, Germany; [email protected] (e-mail). This work is part of the Early Developmental Stages of Psychopathology (EDSP) study and is funded by the German Ministry of Research and Technology (project nos. 01 EB 9405/6, 01 EB 9901/6, 01 EB 140, and 01 EB 0440). Principal investigators are Hans-Ulrich Wittchen, Ph.D., and Roselind Lieb, Ph.D. Current or former staff members of the EDSP group are Kirsten von Sydow, Ph.D., Gabriele Lachner, Dr.rer.biol.hum., Axel Perkonigg, Ph.D., Peter Schuster, Ph.D., Franz Gander, Ph.D., Michael Höfler, Dipl.-Stat., Holger Sonntag, Dipl.-Psych., and Petra Zimmermann, Dr.rer.nat., as well as Esther Beloch, Mag. Phil., Martina Fuetsch, Ph.D., Elzbieta Garczynski, Dipl.-Psych., Alexandra Holly, Dipl.-Psych., Barbara Isensee, Dr. rer.nat., Marianne Mastaler, Ph.D., Chris Nelson, Ph.D., Hildegard Pfister, Dipl.-Inf., Victoria Reed, Ph.D., Andrea Schreier, Dipl.-Psych., Dilek Türk, Dipl.-Psych., Antonia Vossen, Dipl.-Psych., and Ursula Wunderlich, Ph.D. Scientific advisors are Jules Angst, M.D. (Zurich), Jürgen Margraf, Dr.rer.nat. (Basel), Günther Esser, Ph.D. (Potsdam), Kathleen Merikangas, Ph.D. (NIMH, Bethesda, Md.), Jim van Os, M.D., Ph.D. (Maastricht), and Ron Kessler, Ph.D. (Harvard University, Boston).
1. Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB: Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 1995; 52:1048–1060Crossref, Medline, Google Scholar
2. Helzer JE, Robins LN, McEvoy L: Posttraumatic stress disorder in the general population. N Engl J Med 1987; 317:1630–1634Crossref, Medline, Google Scholar
3. Shore JH, Vollmer WM, Tatum EJ: Community patterns of posttraumatic stress disorder. J Nerv Ment Dis 1989; 177:681–685Crossref, Medline, Google Scholar
4. Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, Best CL: Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. J Consult Clin Psychol 1993; 61:984–991Crossref, Medline, Google Scholar
5. Perkonigg A, Kessler RC, Storz S, Wittchen H-U: Traumatic events and posttraumatic stress disorder in the community: prevalence, risk factors and comorbidity. Acta Psychiatr Scand 2000; 101:46–59Crossref, Medline, Google Scholar
6. Breslau N, Davis GC, Andreski P, Peterson E: Traumatic events and posttraumatic stress disorder in an urban population of young adults. Arch Gen Psychiatry 1991; 48:216–222Crossref, Medline, Google Scholar
7. Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P: Trauma and posttraumatic stress disorder in the community. Arch Gen Psychiatry 1998; 55:626–632Crossref, Medline, Google Scholar
8. Cuffe SP, Addy CL, Garrison CZ, Waller JL, Jackson KL, McKeown RE, Chilappagari S: Prevalence of PTSD in a community sample of older adolescents. J Am Acad Child Adolesc Psychiatry 1998; 37:147–154Crossref, Medline, Google Scholar
9. Kilpatrick DG, Saunders BE, Veronen LJ, Best CL, Von JM: Criminal victimization: lifetime prevalence, reporting to police, and psychological impact. Crime Delinq 1987; 33:479–489Crossref, Google Scholar
10. Breslau N, Davis GC: Posttraumatic stress disorder in an urban population of young adults: risk factors for chronicity. Am J Psychiatry 1992; 149:671–675Link, Google Scholar
11. Davidson JRT, Hughes D, Blazer DG, George LK: Post-traumatic stress disorder in the community: an epidemiological study. Psychol Med 1991; 21:731–721Google Scholar
12. Goenjian AK, Steinberg AM, Najarian LM, Fairbanks LA, Tashjian M, Pynoos RS: Prospective study of posttraumatic stress, anxiety, and depressive reactions after earthquake and political violence. Am J Psychiatry 2000; 157:911–916Link, Google Scholar
13. Asarnow J, Glynn S, Pynoos RS, Nahum J, Guthrie D, Cantwell DP, Franklin B: When the earth stops shaking: earthquake sequelae among children diagnosed for pre-earthquake psychopathology. J Am Acad Child Adolesc Psychiatry 1999; 38:1016–1023Crossref, Medline, Google Scholar
14. McFarlane AC: Posttraumatic stress disorder: a model of the longitudinal course and the role of risk factors. J Clin Psychiatry 2000; 61(suppl 5):15–20Google Scholar
15. Green BL, Lindy JD, Grace MC, Glesser GC, Leonard AC, Korol M, Winget C: Buffalo Creek survivors in the second decade: stability of stress symptoms. Am J Orthopsychiatry 1990; 60:43–54Crossref, Medline, Google Scholar
16. Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, Weiss DS: Trauma and the Vietnam War Generation: Report of Findings From the National Vietnam Veterans Readjustment Study. New York, Brunner/Mazel, 1990Google Scholar
17. Harvey AG, Bryant RA: Two-year prospective evaluation of the relationship between acute stress disorder and posttraumatic stress disorder following mild traumatic brain injury. Am J Psychiatry 2000; 157:626–628Link, Google Scholar
18. Mayou RA, Ehlers A, Bryant B: Posttraumatic stress disorder after motor vehicle accidents: 3-year follow-up of a prospective longitudinal study. Behav Res Ther 2002; 30:665–675Crossref, Google Scholar
19. Widows MR, Jacobson PB, Fields KK: Relation of psychological vulnerability factors to posttraumatic stress disorder symptomatology in bone marrow transplant recipients. Psychosom Med 2000; 62:873–882Crossref, Medline, Google Scholar
20. Maercker A, Schützwohl M: Long-term effects of political imprisonment: a group comparison study. Soc Psychiatry Psychiatr Epidemiol 1997; 32:434–442Google Scholar
21. Breslau N, Davis GC, Peterson EL, Schultz L: Psychiatric sequelae of posttraumatic stress disorder in women. Arch Gen Psychiatry 1997; 54:81–87Crossref, Medline, Google Scholar
22. Breslau N, Davis GC, Peterson EL, Schultz LR: A second look at comorbidity in victims of trauma: the posttraumatic stress disorder-major depression connection. Biol Psychiatry 2000; 48:902–909Crossref, Medline, Google Scholar
23. Bolton D, O’Ryan D, Udwin O, Boyle S, Yule W: The long-term psychological effects of a disaster experienced in adolescence, II: general psychopathology. J Child Psychol Psychiatry 2000; 4:513–523Crossref, Google Scholar
24. Stein MB, Hoefler M, Perkonigg A, Lieb R, Pfister H, Maercker A, Wittchen H-U: Patterns of incidence and psychiatric risk factors for traumatic events. Int J Methods Psychiatr Res 2002; 11:143–153Crossref, Medline, Google Scholar
25. Wittchen H-U, Perkonigg A, Lachner G, Nelson CB: The Early Developmental Stages of Psychopathology study (EDSP): objectives and design. Eur Addict Res 1998; 4:18–27Crossref, Medline, Google Scholar
26. Lieb R, Isensee B, von Sydow K, Wittchen H-U: The Early Development Stages of Psychopathology study (EDSP): a methodological update. Eur Addict Res 2000; 6:170–182Crossref, Medline, Google Scholar
27. Wittchen H-U, Pfister H (eds): DIA-X-Interviews: Manual für Screening-Verfahren und Interview; Interviewheft Längsschnittuntersuchung (DIA-X-Lifetime); Ergänzungsheft (DIA-X lifetime); Interviewheft Querschnittuntersuchung (DIA-X 12 Monate); Ergänzungsheft (DIA-X 12 Monate); PC-Programm zur Durchführung des Interviews (Längs- und Querschnittuntersuchung); Auswertungsprogramm. Frankfurt, Germany, Swets & Zeitlinger; 1997Google Scholar
28. Lachner G, Wittchen H-U: Skala zum Vergleich von Kompetenzen. Munich, Max-Planck-Institut, Eigendruck, 1995Google Scholar
29. Reed V, Gander F, Pfister H, Steiger A, Sonntag H, Trenkwalder C, Hundt W, Wittchen HU: To what degree does the Composite International Diagnostic Interview (CIDI) correctly identify DSM-IV disorders? testing validity issues in a clinical sample. Int J Methods Psychiatr Res 1998; 7:142–155Crossref, Google Scholar
30. Wittchen H-U, Lachner G, Wunderlich U, Pfister H: Test-retest reliability of the computerized DSM-IV version of the Munich-Composite International Diagnostic Interview (M-CIDI). Soc Psychiatry Psychiatr Epidemiol 1998; 33:568–578Crossref, Medline, Google Scholar
31. Breslau N, Chilcoat HD, Kessler RC, Davis GC: Previous exposure to trauma and PTSD effects of subsequent trauma: results from the Detroit Area Survey of Trauma. Am J Psychiatry 1999; 156:902–907Link, Google Scholar
32. Marshall RD, Olfson M, Hellman F, Blanco C, Guardino M, Struening EL: Comorbidity, impairment, and suicidality in subthreshold PTSD. Am J Psychiatry 2001; 158:1467–1473Link, Google Scholar
33. Stata Reference Manual: Release 6.0. College Station, Tex, Stata Corp, 1999Google Scholar
34. Andreski P, Chilcoat H, Breslau N: Post-traumatic stress disorder and somatization symptoms: a prospective study. Psychiatry Res 1998; 79:131–138Crossref, Medline, Google Scholar
35. Kubany S, Hill EE, Owens JA, Ianne-Spencer C, McCaig MA, Tremayne KJ, Williams PL: Cognitive trauma therapy for battered women with PTSD (CTT-BW). J Consult Clin Psychol 2004; 72:3–18Crossref, Medline, Google Scholar



