Previous Exposure to Trauma and PTSD Effects of Subsequent Trauma: Results From the Detroit Area Survey of Trauma
Abstract
OBJECTIVE: With the exception of a few reports of higher rates of childhood trauma in Vietnam veterans with posttraumatic stress disorder (PTSD), little is known about the influence of previous exposure to trauma on the PTSD effects of subsequent trauma. The authors examine interrelated questions about the effects of previous exposure to trauma. METHOD: A representative sample of 2,181 individuals in southeast Michigan were interviewed by telephone to record lifetime history of traumatic events specified in DSM-IV as potentially leading to PTSD. PTSD was assessed with respect to a randomly selected index trauma from the list of events reported by each respondent. RESULTS: History of any previous exposure to traumatic events was associated with a greater risk of PTSD from the index trauma. Multiple previous events had a stronger effect than a single previous event. The effect of previous assaultive violence persisted over time with little change. When they examined several features of the previous exposure to trauma, the authors found that subjects who experienced multiple events involving assaultive violence in childhood were more likely to experience PTSD from trauma in adulthood. Furthermore, previous events involving assaultive violence—single or multiple, in childhood or later on—were associated with a higher risk of PTSD in adulthood. CONCLUSIONS: Previous exposure to trauma signals a greater risk of PTSD from subsequent trauma. Although these results are consistent with a sensitization hypothesis, like the results from previous research on PTSD, they do not address the mechanism of increased responsivity to trauma. Long-term observational studies can further elucidate these observations.
An association between previous exposure to traumatic experiences and posttraumatic stress disorder (PTSD) resulting from subsequent trauma has been reported (1–6). High rates of childhood trauma have been reported in Vietnam combat veterans with PTSD (1–4). Previous victimization in women who have been raped and previous combat stress in men fighting a subsequent war have been reported to have adverse effects on the likelihood and course of the psychological sequelae of the later trauma (5, 6). Apart from the few reports on the effects of specific types of traumatic events (chiefly childhood trauma) on PTSD resulting from subsequent trauma in special populations, little is known about the influence of previous exposure to trauma on the PTSD effects of subsequent trauma.
In this study, we examine the influence of previous exposure to trauma on the risk of PTSD from a subsequent trauma in a large representative sample of the general population. We elicited a complete history of traumatic events, as specified in DSM-IV, and, in respondents who reported any exposure to trauma, we assessed PTSD symptoms that followed a randomly selected event from the list of events reported by each respondent. This strategy allowed us to focus on PTSD resulting from a representative sample of traumatic events experienced in the community and avoid the bias of studies focusing on events designated by the respondents as the worst they had ever experienced (7–9). The availability of a complete list of events for each respondent and information on the age at which events occurred allowed us to locate the randomly selected event within the respondent’s life history of events. We used this information to estimate the risk of PTSD from the randomly selected events in subjects with varying histories of previous exposure to trauma.
In a previous report from this study (7), we documented that the risk of PTSD resulting from the randomly selected traumatic events varied by type of event and was greatest for events subsumed under the type of assaultive violence. We also reported a higher risk of PTSD in women than men after controlling for type of event, a finding also reported in other studies (8–11). In this report, controlling for sex and type of events, we examine five questions regarding the effects of previous exposure to trauma: 1) Does previous exposure to trauma increase the risk of PTSD from the index trauma? 2) Does the number of previous events influence that risk? 3) Does previous exposure to trauma involving assaultive violence influence that risk? 4) Does the influence of previous exposure to trauma fade over time? 5) Does childhood exposure to trauma increase the risk of PTSD resulting from trauma in adulthood?
METHOD
Sample
The 1996 Detroit Area Survey of Trauma is a representative sample of 2,181 individuals 18–45 years of age in the Detroit primary metropolitan statistical area. The cutoff age of 45 years was selected on the basis of evidence that the onset of PTSD occurs primarily in early adulthood (10, 11). The Detroit primary metropolitan statistical area is a six-county area that contained 4,266,654 residents at the time of the 1990 census; 1,922,173 of these residents were in the 18–45 age range, of whom 442,100 (23%) resided in the city of Detroit (12). A random-digit dialing method was used to select the sample, and a computer-assisted telephone interview was used to obtain the data (13, 14). Detailed information on the sampling is given elsewhere (7). Screening for eligibility was completed in 2,513 (76.2%) of the 3,297 randomly selected households, and the cooperation rate in eligible households was 2,181 (86.8%). One respondent per household was interviewed. Weights were used to adjust for differences in the number of age-eligible persons in the household, for oversampling men (in anticipation of lower cooperation among men than women [15]),and for differences in the probability of completing the interview (16). Finally, to approximate the sample distribution to the population, poststratification weights were applied on the basis of the joint distribution of age, sex, race, income, and education in the 1990 U.S. census for the area (12). (Detailed information on the weighting is available from N.B. on request.) A comparison of the sample with the Detroit primary metropolitan statistical area census data suggests that we succeeded in getting a representative sample with respect to key characteristics (7). The study was approved by the Institutional Review Board of the Henry Ford Health System, and oral informed consent was elicited and recorded at the start of the interview.
Assessment of Exposure to Traumatic Events and PTSD
A computer-assisted telephone interview averaging 30 minutes in duration was used to collect the data. The interview began with a complete enumeration of the 19 lifetime traumatic events, which operationalize the DSM-IV definition and the accompanying text. The 19 specific events are grouped into four categories: 1) assaultive violence (combat, rape, held captive/tortured/kidnapped, shot or stabbed, sexual assault, mugged/held-up/threatened with a weapon, and badly beaten-up), 2) other injury or shocking experience (serious motor accident, other serious accident, disaster, life-threatening illness, child diagnosed with life-threatening illness, witnessing violence, discovering a dead body), 3) learning about trauma experienced by a loved one (rape, sexual assault, physical attack, serious accident), and 4) learning about the sudden unexpected death of a loved one. An endorsement of an event was followed by questions on the number of times an event of that type had occurred and the respondent’s age at each time.
Using a slightly modified version of the PTSD section of the National Institute of Mental Health Diagnostic Interview Schedule for DSM-IV (DIS) (17) and the World Health Organization Composite International Diagnostic Interview, version 2.1 (18), which is modeled after the DIS, we evaluated the PTSD effects of a computer-selected random event out of the complete list of events reported by each respondent. The DIS/Composite International Diagnostic Interview is a fully structured diagnostic interview designed to be administered by experienced interviewers without clinical training.A validation study conducted on a subset of the sample (N=53) found high concordance of the structured interview with independent clinical reinterviews conducted on the telephone (sensitivity=95.6%, specificity=71%, and kappa=0.63) (19).
Although information on the subjective response to the traumatic event—whether it involved intense fear, helplessness, or horror—was elicited, the analysis was conducted on all those who reported exposure to any one in our list of traumatic events that potentially lead to PTSD. Of all those who were exposed, nearly 80% reported that their response to the randomly selected event involved intense fear, helplessness, or horror. Repeating the statistical models in the subset with this subjective response did not alter the results.
Data Analysis
The analysis was conducted on 1,922 respondents whose randomly selected traumatic event, the index trauma, occurred after they were 5 years old. Assaultive violence was the index trauma in 336 (17.5%) of these respondents, other injury or shock in 655 (34.1%), learning about trauma to a loved one in 547 (28.4%), and sudden unexpected death of a loved one in 384 (20.0%). The risk of PTSD associated with previous exposure to trauma, or with number or type of previous traumatic events, was estimated by the adjusted odds ratio and 95% confidence intervals (CIs) calculated in multiple logistic models (20), which included sex and type of index trauma as covariates to adjust for their effects. Age at index trauma was found to be unrelated to PTSD and was not included in these models, except for the first model to illustrate the finding.
RESULTS
Effects of Any Previous Exposure to Trauma
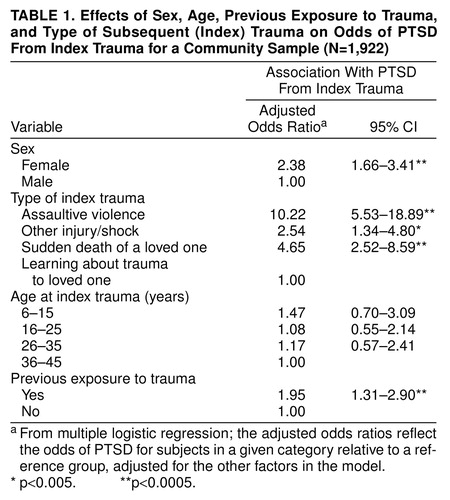
The risk of PTSD from the index trauma in respondents with previous exposure to trauma and in those who had no previous exposure was estimated in a model that included respondents’ sex, type of index trauma, and age at index trauma (Table 1). Subjects who reported any previous trauma were significantly more likely to experience PTSD from the index trauma than were subjects who had no previous exposure to trauma (Wald χ2=10.96, df=1, p=0.0009) (Table 1). We also found that the risk of PTSD was more than twice as high in women than men after controlling for type of index trauma and previous exposure to trauma. The risk of PTSD varied by type of index trauma: assaultive violence conferred the highest risk, more than 10 times the risk conferred by learning about a trauma to a loved one, the reference type with the lowest risk of PTSD. Age at the index trauma was not related to the risk of PTSD.
Applying the same analytic model, we also tested whether PTSD was associated with a greater risk of exposure to trauma after the index trauma. This analysis revealed no significant association between PTSD from the index trauma and subsequent exposure to trauma. The adjusted odds ratio for exposure to trauma occurring after the index trauma in subjects with PTSD compared with those without PTSD was 0.99 (95% CI=0.69–1.42). This analysis addressed alternative methodological and substantive explanations of the observed association between previous exposure to trauma and PTSD from the index trauma.
A potential methodological explanation involves the possibility of a reporting bias, that is, that subjects who report PTSD symptoms might overreport traumatic events. Because a bias of this sort would predict an association with subsequent exposure to trauma as well, its plausibility is dampened by our findings. A substantive alternative explanation is that common risk factors for both PTSD and exposure to trauma, such as preexisting psychiatric disorders (9, 10), might account for the observed association between PTSD and previous exposure to traumatic events. With respect to this explanation, too, a greater risk of both previous and subsequent traumatic events would be expected, but this was not supported by our data.
Number of Previous Events
The effect of number of previous events was tested in a model that distinguished among one, two, and three or more previous events, with no previous exposure to trauma as a reference. Of the 1,922 respondents with an index trauma that occurred after they were 5 years old, 742 (38.6%) had no previous exposure, 427 (22.2%) had exposure to one, 255 (13.3%) had exposure to two, and 498 (25.9%) had exposure to three or more. Compared with no previous exposure to trauma, the risk associated with a single previous event was not higher (odds ratio=1.03, 95% CI=0.61–1.76), but the risks associated with two previous events (odds ratio=2.12, 95% CI=1.26–3.58, Wald χ2=7.99, df=1, p=0.004) and with three or more previous events (odds ratio=2.41, 95% CI=1.57–3.69, Wald χ2=16.25, df=1, p=0.0001) were higher and similar in size.
Type of Previous Trauma: Assaultive Violence Versus Other Types
We tested whether previous assaultive violence had a stronger association with PTSD from the index trauma than previous exposure to trauma that did not involve assaultive violence. Controlling for sex and type of index trauma, we found that the odds ratio associated with previous assaultive violence was 2.63 (95% CI=1.71–4.05) and the odds ratio associated with previous exposure to trauma that did not involve assaultive violence was 1.36 (95% CI=0.89–2.10). The difference between the two odds ratios was significant (Wald χ2=9.57, df=1, p=0.002). We found no interaction between previous assaultive violence and either type of index trauma or sex, indicating that previous assaultive violence is associated with a greater risk of PTSD across all types of index trauma and in both sexes.
We also estimated the effects of multiple versus single previous exposure to trauma by type (Table 2). Previous exposure to both single and multiple traumatic events involving assaultive violence signaled a greater risk of PTSD from the index trauma. In contrast, only previous exposure to multiple traumatic events not involving assaultive violence signaled a greater risk.
Recency of Exposure to Trauma
We tested whether the effect of previous exposure to trauma on the risk of PTSD from a new traumatic event changes over time. Logistic regression was used with previous assaultive violence, other types of trauma, and number of years from previous exposure to the index trauma for each of the two types of trauma. We found that the risk of PTSD from the index trauma associated with previous assaultive violence persisted over time with no change (odds ratio=1.00; 95% CI=0.96–1.04, Wald χ2=0.001, df=1, p=0.97). In contrast, we found a negative time trend for other types of trauma (odds ratio=0.92; 95% CI=0.85–1.00, Wald χ2=4.53, df=1, p=0.03), indicating that the effect of trauma that did not involve assaultive violence attenuated by 8% each year, on the average (95% CI=0.2%–15.4%). According to the results of this analysis, approximately 5 years after the previous exposure to trauma, the risk of PTSD from a new trauma is predicted to be two times higher for subjects whose previous exposure to trauma involved assaultive violence than for subjects whose previous exposure to trauma did not involve assault.
Childhood Exposure to Trauma and PTSD From Trauma in Adulthood
Using respondents’ retrospective accounts of their age at each traumatic event, we examined the effect of childhood (15 years of age or younger) exposure to trauma in subjects whose index trauma occurred when they were 18 years of age or older (N=1,290). Controlling for sex and type of index trauma, we found that the odds ratio of PTSD from trauma in adulthood associated with childhood exposure to trauma was 2.06 (95% CI=1.18–3.60, Wald χ2=6.44, df=1, p=0.01), compared with 1.77 (95% CI=0.99–3.16, Wald χ2=3.75, df=1, p=0.05) for previous exposure to trauma after age 15.
Within the constraints of our sample size, we explored an expanded model with all three characteristics of previous exposure to trauma: whether it involved assaultive violence, occurred in childhood, and occurred at least twice. Table 3 presents the rates of PTSD from the index trauma in adulthood associated with previous exposure to trauma; it also presents the adjusted odds ratios from multiple regression controlling for sex and type of index trauma. A history of two or more traumatic events involving assaultive violence in childhood was associated with a high risk of PTSD from trauma in adulthood. However, compared with no previous exposure to trauma, even a single previous exposure to assaultive violence, whether in childhood or later on, was associated with a higher risk of PTSD from trauma in adulthood. The results on the effects of traumatic events that did not involve assaultive violence did not follow a clear pattern, although they suggest that multiple and less distant previous events (after age 15) were associated with a significantly higher risk of PTSD in adulthood than no previous exposure to trauma.
DISCUSSION
Key findings of this study are 1) compared with previous exposure to trauma that did not involve assaultive violence, previous exposure to trauma involving assaultive violence was associated with a higher risk of PTSD from subsequent trauma, 2) the effect of previous assaultive violence on the risk of PTSD from subsequent trauma persisted over time with little change, 3) compared with no history of previous exposure to trauma, a history of two or more traumatic events involving assaultive violence in childhood was associated with a nearly fivefold greater risk that a traumatic event in adulthood would lead to PTSD, and 4) even a single previous event involving assaultive violence, either in childhood or later on, was associated with a higher risk of PTSD from trauma in adulthood.
These results support the hypothesis that previous exposure to traumatic events is associated with greater vulnerability to the PTSD effects of a subsequent trauma. To our knowledge, the evidence of vulnerability to PTSD in adulthood in subjects who experienced childhood trauma is the first replication in a general population sample of previous findings based primarily on samples of Vietnam veterans (1–4). Effects of childhood adversity and trauma have been reported in relation to a variety of psychiatric disorders (21). Brown et al. (22, 23) reported such effects in relation to depression and anxiety disorders in adulthood. They proposed that the enduring vulnerability to anxiety disorders that originates in childhood experiences may involve cognitive predispositions, such as helplessness, and that “experiences in childhood m(22, p. 63).
The data in this study are retrospective, based on respondents’ accounts of their lifetime experiences. Therefore, a general caveat on the accuracy of the lifetime data, including the dating of events in childhood, is in order. Clearly, prospective data gathered in longitudinal studies would be less likely to be subject to recall errors. However, because an important aspect of this analysis concerns events in childhood, short of long-term longitudinal studies from childhood to adulthood, retrospective lifetime data are essential. It should be noted that there is no evidence in these data that a trauma in childhood is associated with a higher risk of PTSD than is a trauma that occurred later in life; age at exposure to trauma was not found to be related to the risk of PTSD. We found, instead, that childhood trauma increased the risk that a new trauma experienced in adulthood would lead to PTSD. The plausibility that this specific finding regarding the consequences of childhood trauma is likely to reflect a retrospective reporting bias is weaker than if we had found a generalized effect of childhood trauma on PTSD.
The results of this analysis, taken together with our previous findings (7), constitute strong evidence of the unique status of assaultive violence in terms of the high risk of PTSD it confers, the chronicity of PTSD symptoms resulting from it, and its persistent effect on an individual’s future response to trauma. In our earlier study (7), we showed that the period of high risk of exposure to assaultive violence is in late adolescence and early adulthood and that the risk declines precipitously after age 25. The current analysis indicates that the effect of previous exposure to trauma on the PTSD outcomes of any subsequent trauma represents a long-lasting vulnerability factor.
This analysis provides further evidence about the sex difference in the risk of PTSD. As we and others have reported, females are more likely to develop PTSD from exposure to trauma, even when the type of traumatic event is controlled (7–11, 24). The results presented here indicate that women’s higher risk of PTSD is not attributable to sex differences in history of previous exposure to trauma.
We found no evidence that the subject’s age at the index trauma influenced the risk of PTSD. Despite the intuitive importance of age at exposure to trauma as a risk factor for PTSD, previous reports have provided little information on the topic. General population surveys have reported on the prevalence of PTSD by age at interview, not age at exposure to trauma (9, 25). Green et al. (26) reported that younger age at time of military service in Vietnam was a significant predictor of combat-related PTSD more than 10 years after the war. The relationship between age at time of service and lifetime combat-related PTSD was not reported, leaving open the possibility that age at exposure to trauma might be associated with the chronicity of PTSD rather than with the risk of PTSD. Analysis of data from the National Comorbidity Survey (27), in which age at time of exposure to trauma was used, found no age effects on the risk of PTSD.
The observed risk of PTSD from the index trauma associated with previous exposure to trauma is unlikely to be a methodological artifact due to a reporting bias. A reporting bias, if present, would have predicted an association between PTSD and total number of traumatic events in lifetime, both before and after the index trauma, and we found no evidence of an association with subsequent exposure to trauma.
Substantive alternative explanations for the association between PTSD and previous exposure to trauma are suggested by evidence from previous research that there are common risk factors for both exposure to trauma and PTSD. Preexisting major depression was found to predispose to traumatic events and increase the vulnerability to the PTSD-inducing effects of traumatic events (9, 10, 28, 29). Similarly, neuroticism was found to be a risk factor for both exposure to traumatic events and their PTSD effects (24, 28, 29). These common risk factors would predict that individuals with PTSD report more traumatic events overall, both before and after the index trauma. Neuroticism is a personality trait with strong continuity over time, and there is little reason to expect that its effect on exposure to trauma would wane following the onset of PTSD. Functional impairment in emotional, motivational, and interpersonal capacities associated with major depression persist beyond the duration of illness episodes and would have increased the likelihood of traumatic events during the life spans of our respondents (30–33). The finding that PTSD from the index trauma was not associated with a higher risk of subsequent traumatic events addresses these potential explanations.
The possibility that early traumatic events might have led to the onset of psychiatric disorders, which in turn increased the vulnerability to PTSD from subsequent events, does not threaten the validity of our findings. In this chain of events, the onset of psychiatric disorders is a mediator (a mechanism) that links previous exposure to trauma with the PTSD response to subsequent events, not a confounder.
An alternative explanation that cannot be addressed in these data is the possibility that early social environments that are associated with a high risk of traumatic events in childhood are associated with a diminished competence for dealing with traumatic events in adulthood. Because it predicts an association between PTSD and early exposure to trauma specifically, this potential explanation remains intact.
The results of this study are consistent with a sensitization hypothesis, proposed to account for the association of childhood trauma and PTSD in Vietnam veterans (34–36). Specifically, our results show that respondents who experienced previous trauma are more vulnerable to the PTSD effects of subsequent trauma than those with no previous trauma. The results of this study also support the notions that repeated exposure to trauma has worse consequences than a single exposure and that the effects of previous assaultive violence are worse than the effects of previous trauma of lesser magnitude. Nonetheless, like earlier reports on previous trauma and PTSD (34–36), this study falls short of providing the necessary evidential support for sensitization because it has nothing to say about the process of increased responsivity to repeated exposure to trauma. It might be tempting to infer such a mechanism from the differences in the risk of PTSD between those who experienced previous trauma and those who did not. How else might these differences be understood? However, the lack of within-subjects comparisons leaves open the possibility of other mechanisms. Definitive evidence for ruling out noncausal explanations of the association between previous trauma and greater susceptibility to PTSD and for establishing that the mechanism at work is greater responsivity to repeated exposure to trauma must come from experimental research, probably an unfeasible design in human research. Other study designs with considerable value involve long-term observations of subjects known to have suffered distinct traumatic events, largely by chance, and of comparable subjects who escaped exposure to these events.
Received March 13, 1998; revisions received July 9, Oct. 16, and Dec. 15, 1998; accepted Jan. 20, 1999. From the Department of Psychiatry, Henry Ford Health System; and the Department of Health Care Policy, Harvard Medical School, Boston. Address reprint requests to Dr. Breslau, Department of Psychiatry, Henry Ford Health Sciences Center, One Ford Place 3A, Detroit, MI 48202-3450; [email protected] (e-mail). Supported in part by NIMH grant MH-48802.
 |
 |
 |
1. Davidson JRT, Hughes D, Blazer DG: Post-traumatic stress disorder in the community: an epidemiological study. Psychol Med 1991; 21:713–721Crossref, Medline, Google Scholar
2. Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, Weiss DS: Trauma and the Vietnam War Generation: Report of Findings From the National Vietnam Veterans Readjustment Study. New York, Brunner/Mazel, 1990Google Scholar
3. Zaidi LY, Foy DW: Childhood abuse experiences and combat-related PTSD. J Trauma Stress 1994; 7:33–42Crossref, Medline, Google Scholar
4. Bremner JD, Southwick SM, Johnson DR, Yehuda R, Charney DS: Childhood physical abuse and combat-related posttraumatic stress disorder in Vietnam veterans. Am J Psychiatry 1993; 150:235–239Link, Google Scholar
5. Foa EB, Riggs DS: Posttraumatic stress disorder and rape, in American Psychiatric Press Review of Psychiatry, vol 12. Edited by Oldham JM, Riba MB, Tasman A. Washington, DC, American Psychiatric Press, 1993, pp 273–303 Google Scholar
6. Solomon Z, Mikulincer M, Jakob BR: Exposure to recurrent combat stress: combat stress reactions among Israeli soldiers in the Lebanon war. Psychol Med 1987; 17:433–440Crossref, Medline, Google Scholar
7. Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P: Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry 1998; 55:626–632Crossref, Medline, Google Scholar
8. Kessler RC, Sonnega A, Bromet E, Nelson CB: Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 1995; 52:1048–1060Google Scholar
9. Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB, Breslau N: Epidemiologic risk factors for trauma and PTSD, in Risk Factors for Posttraumatic Stress Disorder. Edited by Yehuda R. Washington, DC, American Psychiatric Press (in press)Google Scholar
10. Breslau N, Davis GC, Peterson E, Schultz L: Psychiatric sequelae of posttraumatic stress disorder in women. Arch Gen Psychiatry 1997; 54:81–87Crossref, Medline, Google Scholar
11. Breslau N, Davis GC, Andreski P, Peterson EL, Schultz LR: Sex differences in posttraumatic stress disorder. Arch Gen Psychiatry 1997; 54:1044–1048Google Scholar
12. Census of Population and Housing, 1990: Public Use Microdata Sample:1-Percent Sample. Washington, DC, US Department of Commerce, Bureau of the Census, 1990Google Scholar
13. Survey Sampling, Inc, Random Digit Telephone Sampling Methodology. Fairfield, Conn, Survey Sampling, 1996Google Scholar
14. Potthoff RF: Telephone sampling in epidemiologic research: to reap the benefits, avoid the pitfalls. Am J Epidemiol 1994; 10:967–978Google Scholar
15. Groves RM: Survey Errors and Survey Costs. New York, John Wiley & Sons, 1989Google Scholar
16. Kessler RC, Little RJA, Groves RM: Advances in strategies for minimizing and adjusting for survey nonresponse. Epidemiol Rev 1995; 17:192–204Crossref, Medline, Google Scholar
17. Robins LN, Cottler L, Bucholz K, Compton W: Diagnostic Interview Schedule for DSM-IV. St Louis, Washington University, 1995Google Scholar
18. World Health Organization: Composite International Diagnostic Interview (CIDI), version 2.1. Geneva, Switzerland, World Health Organization, 1997Google Scholar
19. Breslau N, Kessler RC, Peterson EL: PTSD assessment with a structured interview: reliability and concordance with a standardized clinical interview. Int J Methods Psychiatr Res 1998; 7:121–127Crossref, Google Scholar
20. Hosmer DW, Lemeshow S: Applied Logistic Regression. New York, John Wiley & Sons, 1989, pp 25–36Google Scholar
21. Kessler RC, Davis CG, Kendler KS: Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychol Med 1997; 27:1101–1119Google Scholar
22. Brown GW, Harris TO, Eales MJ: Aetiology of anxiety and depressive disorders in an inner-city population, 1: early adversity. Psychol Med 1993; 23:143–154Crossref, Medline, Google Scholar
23. Brown GW, Harris TO, Eales MJ: Aetiology of anxiety and depressive disorders in an inner-city population, 2: comorbidity and adversity. Psychol Med 1993; 23:155–165Crossref, Medline, Google Scholar
24. Breslau N: Epidemiology of trauma and posttraumatic stress disorder, in Psychological Trauma. Edited by Yehuda R (American Psychiatric Press Review of Psychiatry, vol 17; Oldham JM, Riba MB, series editors). Washington, DC, American Psychiatric Press, 1998, pp 1–29Google Scholar
25. Norris FH: Epidemiology of trauma: frequency and impact of different potentially traumatic events on different demographic groups. J Consult Clin Psychol 1992; 60:409–418Crossref, Medline, Google Scholar
26. Green BL, Grace MC, Lindy JD, Gleser GC, Leonard A: Risk factors for PTSD and other diagnoses in a general sample of Vietnam veterans. Am J Psychiatry 1990; 147:729–733Link, Google Scholar
27. Bromet E, Sonnega A, Kessler RC: Risk factors for DSM-III-R posttraumatic stress disorder: findings from the National Comorbidity Survey. Am J Epidemiol 1998; 147:352–361Crossref, Google Scholar
28. Breslau N, Davis GC, Andreski P, Peterson E: Traumatic events and posttraumatic stress disorder in an urban population of young adults. Arch Gen Psychiatry 1991; 48:216–222Crossref, Medline, Google Scholar
29. Breslau N, Davis GC, Andreski P, Federman B, Anthony JC: Epidemiologic findings on PTSD and comorbid disorders, in Adversity, Stress, and Psychopathology. Edited by Dohrenwend BP. New York, Oxford University Press, 1998, pp 319–330Google Scholar
30. Broadhead WE, Blazer DG, George LK, Tse CK: Depression, disability days, and days lost from work in a prospective epidemiologic survey. JAMA 1990; 264:2524–2528Google Scholar
31. Hays RD, Wells KB, Sherbourne CD, Rogers W, Spritzer K: Functioning and well-being outcomes of patients with depression compared with chronic general medical illnesses. Arch Gen Psychiatry 1995; 52:11–19Crossref, Medline, Google Scholar
32. Ormel J, Von Korff M, Ustun B, Pini S, Korten A, Oldehinkel T: Common mental disorders and disability across cultures. JAMA 1994; 272:1741–1748Google Scholar
33. Von Korff M, Ormel J, Katon W, Lin EHB: Disability and depression among high utilizers of health care. Arch Gen Psychiatry 1995; 52:11–19Crossref, Medline, Google Scholar
34. Post RM, Weiss SRB, Smith MA: Sensitization and kindling: implications for the evolving neural substrates of post-traumatic stress disorder, in Neurobiological and Clinical Consequences of Stress: From Normal Adaptation to Post-Traumatic Stress Disorder. Edited by Friedman MJ, Charney DS, Deutch AY. Philadelphia, Lippincott-Raven, 1995, pp 203–224Google Scholar
35. Southwick SM, Yehuda R, Morgan CA III: Clinical studies of neurotransmitter alterations in post-traumatic stress disorder. Ibid, pp 335–349Google Scholar
36. Yehuda R, McFarlane AC: Conflict between current knowledge about posttraumatic stress disorder and its original conceptual basis. Am J Psychiatry 1995; 152:1705–1713Google Scholar



