Two-Year Prospective Evaluation of the Relationship Between Acute Stress Disorder and Posttraumatic Stress Disorder Following Mild Traumatic Brain Injury
Abstract
OBJECTIVE: To assess the ability of acute stress disorder to predict posttraumatic stress disorder (PTSD), the relationship between acute stress disorder and PTSD over the 2 years following mild traumatic brain injury was determined. METHOD: Survivors of motor vehicle accidents who sustained mild traumatic brain injuries were assessed for acute stress disorder within 1 month of the trauma (N=79) and for PTSD at 6 months (N=63) and 2 years (N=50) posttrauma. RESULTS: Acute stress disorder was diagnosed in 14% of the patients. Among the patients who participated in all three assessments, 80% of the subjects who met the criteria for acute stress disorder were diagnosed with PTSD at 2 years. Of the total initial group, 73% of those diagnosed with acute stress disorder had PTSD at 2 years. CONCLUSIONS: This study provides further support for the utility of the acute stress disorder diagnosis as a predictor of PTSD but indicates that the predictive power of the diagnostic criteria can be increased by placing greater emphasis on reexperiencing, avoidance, and arousal symptoms.
It is widely accepted that an individual who sustains a mild traumatic brain injury can also suffer acute stress disorder and posttraumatic stress disorder (PTSD) (1–3). The proposal that the absence of recall for the traumatic event precludes the development of PTSD (4) has been called into question by evidence relating to the implicit encoding of traumatic memories (5), the reconstruction of memories on the basis of a secondary source (6), and the intact islands of memory of the trauma during the period of posttraumatic amnesia (7).
Acute stress disorder was introduced in DSM-IV to describe acute reactions that predict PTSD (8). One standard by which any new diagnosis is measured is its long-term stability across longitudinal studies (9). Previous reports indicate that 13% of the people who sustain mild traumatic brain injuries suffer acute stress disorder (3) and that the majority of these individuals (82%) are diagnosed with PTSD at 6 months posttrauma (10). This research provides initial evidence for the proposal that acute stress disorder is a precursor of PTSD. Longer-term prospective study is required to validate the predictive ability of the acute stress disorder diagnosis. Accordingly, we determined the relationship between the acute stress disorder diagnosis and PTSD status 2 years posttrauma.
METHOD
The study group was selected from adult victims of motor vehicle accidents who were consecutively admitted to a major trauma hospital. A total of 79 patients were assessed within 1 month of the trauma, and 63 were reassessed at 6 months posttrauma. The participation of 50 individuals at the 2-year follow-up represents a retention rate of 63% of the initial study group and 79% of the group assessed at 6 months. The groups assessed at 1 and 6 months are described in full elsewhere (10). At the 2-year assessment, two patients refused to participate and 11 had changed residences. The final study group included 31 men and 19 women, who ranged in age from 17 to 58 years (mean=27.00, SD=10.62). The subjects were assessed an average of 721.68 (SD=49.41) days posttrauma, and the mean injury severity score was 10.08 (SD=6.38) (10, 11), indicating moderately severe injuries. Of the 50 subjects, 22 had been drivers in their accidents, 10 had been passengers, 12 had been motorbike riders, five had been pedestrians, and one had been a cyclist. Those who participated in the 2-year posttrauma assessment did not differ from nonparticipants in terms of age, diagnosis, length of hospital stay, injury severity score, or interval between trauma and assessment for acute stress disorder. At the 2-year follow-up, three patients (6%) had received anxiolytic medication, and three (6%) had received cognitive behavior therapy; 14 (28%) had settled compensation claims, and 19 (38%) still had compensation claims pending.
All three assessments were carried out by clinical psychologists with more than 5 years of experience in assessing traumatized individuals (including A.G.H.). After complete description of the study to the subjects, written informed consent was obtained. The diagnosis of acute stress disorder was made by using the Acute Stress Disorder Interview (12). Dissociative amnesia was excluded as a possible symptom of acute stress disorder because of the overlap between dissociative and organic amnesia following mild traumatic brain injury. The 6-month and 2-year assessments involved the administration of the PTSD module from the Composite International Diagnostic Interview (13). In addition, the patients were asked whether they had received psychological treatment and the status of any legal proceedings arising from the motor vehicle accident.
The full criteria for acute stress disorder were met by 14% (N=11) of the initial study group. PTSD was diagnosed in 24% (N=15) at 6 months posttrauma and in 22% (N=11) at 2 years posttrauma. Chi-square analyses indicated that the patients with PTSD were not more likely to report pending compensation than those without PTSD (χ2=1.57, N=50, df=1, with Yates’s correction, n.s.) (14).
Of the 11 subjects with acute stress disorder, 10 completed all three assessments; 80% (N=8) met the criteria for PTSD at the 2-year follow-up, and 20% (N=2) did not. Of the 40 who were not diagnosed with acute stress disorder and completed the three assessments, 8% (N=3) met the criteria for PTSD and 93% (N=37) did not. To provide the most conservative estimate, we also considered diagnostic status at 2 years posttrauma as a function of the initial study group; by this calculation, 73% of the patients with a diagnosis of acute stress disorder (eight of 11) met the criteria for PTSD at the 2-year follow-up.
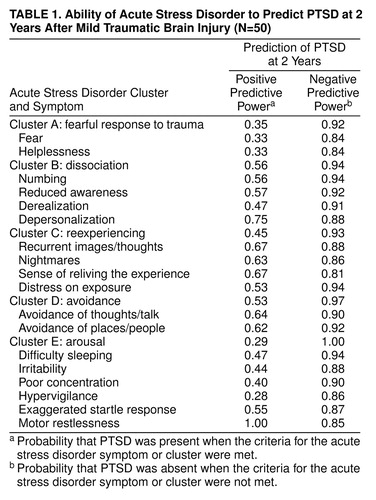
Table 1 presents the positive and negative predictive power of each acute stress disorder symptom and each symptom cluster on the basis of diagnostic status at 2 years posttrauma. Whereas all of the symptoms of acute stress disorder had reasonably strong negative predictive power, the symptoms with the strongest positive predictive power were numbing, reduced awareness, depersonalization, recurrent images/thoughts, nightmares, a sense of reliving the traumatic experience, avoidance, and motor restlessness.
Table 1 also presents the positive and negative predictive power for each acute stress disorder diagnostic cluster. All clusters had strong negative predictive power; positive predictive power varied. When the threshold for the dissociative cluster was set at two (rather than three) symptoms, the positive predictive power increased to 0.82, but the negative predictive power decreased to 0.77. When two symptoms were required for each of the reexperiencing and avoidance clusters, there was an increase in positive predictive power (0.73 and 0.92, respectively), and the negative predictive power stayed constant (0.92 and 0.97, respectively). When three arousal symptoms were required, the positive predictive power improved to 0.56 and the negative predictive power decreased marginally to 0.94.
DISCUSSION
At 2 years posttrauma, 22% of the participants met the full criteria for PTSD. This rate is consistent with previously reported incidence rates of PTSD following motor vehicle accidents (15). The finding that 80% of the patients who satisfied the criteria for acute stress disorder had PTSD at 2 years posttrauma adds support to the utility of the acute stress disorder diagnosis as a predictor of chronic PTSD. It needs to be recognized that this figure may not take into account the individuals who did not participate in the follow-up assessments. The current findings also indicate that the predictive power of the acute stress disorder criteria may be enhanced by placing greater emphasis on acute reexperiencing, avoidance, and arousal symptoms. This suggestion is consistent with findings in prospective studies of study groups without traumatic brain injury that indicate that many trauma survivors who do not display acute dissociative symptoms subsequently develop PTSD (16).
The strong predictive power of numbing and depersonalization supports the notion that dissociative mechanisms may prevent the processing and integration of trauma-related information and thereby contribute to ongoing PTSD (17). The role of acute motor restlessness in predicting subsequent PTSD accords with evidence that persistent PTSD may be mediated by heightened arousal in the acute posttrauma phase (18, 19).
When the patients who had received therapy were excluded, the findings were nearly identical to those from the initial analyses. Although comparable proportions of PTSD and non-PTSD patients reported ongoing litigation, we recognize that compensation issues may influence the reporting of PTSD symptoms. Also, these results may not be generalized to other trauma populations. Moreover, future research needs to determine the relationship between acute stress disorder and development of other psychiatric disorders in the acute posttrauma phase. In summary, although the current findings point to the utility of the acute stress disorder criteria, there appears to be a need for refinement of these criteria to enhance predictive power.
Received Dec. 14, 1998; revision received July 9, 1999; accepted Oct. 1, 1999. From the School of Psychology, University of New South Wales, Sydney, Australia. Address reprint requests to Dr. Harvey, Department of Experimental Psychology, University of Oxford, South Parks Rd., Oxford OX1 3UD, U.K.; [email protected] (e-mail). Supported by the National Health and Medical Research Council.
 |
1. Ohry A, Rattok J, Solomon Z: Post-traumatic stress disorder in brain injury patients. Brain Inj 1996; 10:687–695Crossref, Medline, Google Scholar
2. Rattok J, Ross B: Post traumatic stress disorder in the traumatically head injured (abstract). J Clin Exp Neuropsychol 1993; 6:243Google Scholar
3. Harvey AG, Bryant RA: Acute stress disorder after mild traumatic brain injury. J Nerv Ment Dis 1998; 186:333–337Crossref, Medline, Google Scholar
4. Sbordone RJ, Liter JC: Mild traumatic brain injury does not produce post-traumatic stress disorder. Brain Inj 1995; 9:405–412Crossref, Medline, Google Scholar
5. Brewin CR, Dalgleish T, Joseph S: A dual representation theory of posttraumatic stress disorder. Psychol Rev 1996; 103:670–686Crossref, Medline, Google Scholar
6. Bryant RA: Posttraumatic stress disorder, flashbacks, and pseudomemories in closed head injury. J Trauma Stress 1996; 9:621–629Crossref, Medline, Google Scholar
7. Hyman IE Jr, Loftus EF: Errors in autobiographical memory. Clin Psychol Rev 1998; 18:933–947Crossref, Medline, Google Scholar
8. Bryant RA, Harvey AG: Acute stress disorder: a critical review of diagnostic issues. Clin Psychol Rev 1997; 17:757–773Crossref, Medline, Google Scholar
9. Robins E, Guze SB: Establishment of diagnostic validity in psychiatric illness: its application to schizophrenia. Am J Psychiatry 1970; 126:983–987Link, Google Scholar
10. Bryant RA, Harvey AG: Relationship between acute stress disorder and posttraumatic stress disorder following mild traumatic brain injury. Am J Psychiatry 1998; 155:625–629Link, Google Scholar
11. Association for the Advancement of Automotive Medicine: The Abbreviated Injury Scale. Des Plaines, Ill, AAAM, 1990Google Scholar
12. Bryant RA, Harvey AG, Dang ST, Sackville T: Assessing acute stress disorder: psychometric properties of a structured clinical interview. Psychol Assess 1998; 10:215–220Crossref, Google Scholar
13. Peters L, Andrews G, Cottler LB, Chatterji S, Janca A, Smeets R: The Composite International Diagnostic Interview posttraumatic stress disorder module: preliminary data. Int J Methods Psychiatry Res 1996; 6:167–174Crossref, Google Scholar
14. Fleiss JL: Statistical Methods for Rates and Proportions, 2nd ed. New York, John Wiley & Sons, 1981Google Scholar
15. Blanchard EB, Hickling EJ, Taylor AE, Loos WR, Forneris CA, Jaccard J: Who develops PTSD from motor vehicle accidents? Behav Res Ther 1996; 34:1–10Google Scholar
16. Harvey AG, Bryant RA: The relationship between acute stress disorder and posttraumatic stress disorder: a prospective evaluation of motor vehicle accident survivors. J Consult Clin Psychol 1998; 66:507–512Crossref, Medline, Google Scholar
17. Foa EB, Hearst-Ikeda D: Emotional dissociation in response to trauma: an information-processing approach, in Handbook of Dissociation: Theoretical and Clinical Perspectives. Edited by Michelson LK, Ray WJ. New York, Plenum, 1996, pp 207–222Google Scholar
18. Shalev AY, Sahar T, Freedman S, Peri T, Glick N, Brandes D, Orr SP, Pitman RK: A prospective study of heart rate response following trauma and the subsequent development of posttraumatic stress disorder. Arch Gen Psychiatry 1998; 55:553–559Crossref, Medline, Google Scholar
19. Bryant RA, Harvey AG, Guthrie R, Moulds M: A prospective study of psychophysiological arousal, acute stress disorder, and posttraumatic stress disorder. J Abnorm Psychol (in press)Google Scholar



