Psychiatric Aspects of Impulsivity
Abstract
OBJECTIVE: The authors discuss the relationship of impulsivity to psychiatric disorders and present selected hypotheses regarding the reasons for these relationships. METHOD: Previous research has shown significantly higher levels of impulsivity among patients with conduct disorder, personality disorders, substance use disorders, and bipolar disorder, compared to other psychiatric patients or healthy comparison subjects. A literature review of the theoretical bases of the relationship between these disorders and impulsivity is presented. Measurements of impulsivity and treatment options are discussed in relation to the physiology of impulsivity and the disorders in which it is a prominent feature. RESULTS: Impulsivity, as defined on the basis of a biopsychosocial approach, is a key feature of several psychiatric disorders. Behavioral and pharmacological interventions that are effective for treating impulsivity should be incorporated into treatment plans for these disorders. CONCLUSIONS: The high comorbidity of impulsivity and selected psychiatric disorders, including personality disorders, substance use disorders, and bipolar disorder, is in a large part related to the association between impulsivity and the biological substrates of these disorders. Before treatment studies on impulsivity can move forward, measures of impulsivity that capture the core aspects of this behavior need to be refined and tested on the basis of an ideologically neutral model of impulsivity.
Although impulsivity is directly mentioned in the DSM-IV diagnostic criteria for several disorders and is implied in the criteria for others, until recently little work has been done to clarify the role of impulsivity in psychiatric illness. Likewise, although some examples of impulsive behavior are given in DSM-IV, impulsivity is not explicitly defined. This lack of specificity regarding the role of impulsivity in psychiatric illness results in part from disagreements in the literature about how to define and measure impulsivity. Impulsivity has been variously defined as swift action without forethought or conscious judgment (1), behavior without adequate thought (2), and the tendency to act with less forethought than do most individuals of equal ability and knowledge (3). Some definitions of impulsivity include a number of subtraits. Eysenck and Eysenck (4) related impulsivity to risk taking, lack of planning, and making up one’s mind quickly. Patton et al. (5) separated impulsivity into three components: 1) acting on the spur of the moment (motor activation), 2) not focusing on the task at hand (attention), and 3) not planning and thinking carefully (lack of planning). Some authors argue that impulsivity and compulsivity are opposite ends of a spectrum (6, 7). Others contend that event-related cortical potentials can be used to measure impulsivity (8), and still others that impulsivity can be measured with laboratory behavioral tasks (9, 10).
The overall goal of this article is to provide a definition of impulsivity that can be used to bridge the gap between clinical work and research and to discuss the relationship between impulsivity and several psychiatric disorders. Our hypotheses are that 1) impulsivity is an important aspect of several psychiatric disorders, 2) basic biological and behavioral research is hindered by rigid adherence to current nosological schemes, and 3) biological and psychological treatments for psychiatric disorders should incorporate methods aimed at the reduction of impulsivity.
A Biopsychosocial Definition of Impulsivity
Biological studies examining impulsive aggression (11, 12) have found that individuals who planned aggressive acts have larger evoked potential amplitudes and higher CSF serotonin metabolite levels than those who did not plan similar aggressive acts. Likewise, individuals with impulsive aggression responded differently to treatment with anticonvulsants than did individuals with planned aggressive acts (13). Thus, a definition of impulsivity that takes into account research on biologically distinct groups needs to incorporate rapidity of response and lack of planning.
Within the psychological literature, several behavioral models of impulsivity have been developed on the basis of findings from laboratory tasks used to measure impulsivity. These tasks fall into three broad categories: 1) punished and/or extinction paradigms, in which impulsivity is defined as the perseverance of a response that is punished or unrewarded (14); 2) reward-choice paradigms, in which impulsivity is defined as preference for a small immediate reward over a larger delayed reward (15); and 3) response disinhibition/attentional paradigms, in which impulsivity is defined either as making responses that are premature or as the inability to withhold a response (16, 17).
To incorporate these models into a definition of impulsivity, the definition should include the following elements: 1) decreased sensitivity to negative consequences of behavior; 2) rapid, unplanned reactions to stimuli before complete processing of information; and 3) lack of regard for long-term consequences.
Socially, impulsivity has been thought of as a learned behavior, coming from a family environment in which the child learns to “react immediately to obtain what is desired for gratification” (18). In this conceptual framework, impulsive individuals do not have the capacity to weigh the consequences of actions, either for themselves or for others. Thus, a definition that includes the social aspects of impulsivity needs to incorporate the fact that impulsivity often has an impact, not only on the impulsive individual, but also on others.
Impulsivity is defined here as a predisposition toward rapid, unplanned reactions to internal or external stimuli without regard to the negative consequences of these reactions to the impulsive individual or to others.
Several key features of this definition should be highlighted. First, impulsivity is defined as a predisposition, part of a pattern of behavior rather than a single act. This distinction is important clinically because research on treatment of impulsive aggression, to be discussed later, shows that individuals with a pattern of impulsive aggression respond differently to medication than those with a pattern of primarily premeditated aggression (13). Second, it is noteworthy that impulsivity involves rapid unplanned action that occurs before the opportunity to consciously weigh the consequences of an act. This feature separates impulsivity from impaired judgment or compulsive behaviors, in which planning occurs before the behavior. Again, this distinction is important for research and treatment. Incarcerated individuals with premeditated aggression (arguably poor judgment) exhibited different patterns of brain activity than incarcerated individuals with impulsive aggression (11). Last, impulsivity implies action without regard to the consequences of these actions. Impulsivity often involves risks, but it is not the result of the types of risk often related to sensation seeking.
We believe these aspects of impulsivity are important because they can be related to the underlying biological substrates of impulsive behavior and hence to treatment for impulsivity.
Measurement of Impulsivity
Although a wide variety of measures are correlated with impulsivity and have been used as “measures” of impulsivity, there are primarily three main classes of instruments that appear to measure key aspects of impulsivity: self-report measures, behavioral laboratory measures, and event-related potentials.
Self-Report Measures
Self-report measures, such as the Barratt Impulsiveness Scale (5) and the Eysenck Impulsiveness Questionnaire (19), have the advantage of allowing the researcher to gather information on a variety of types of acts and on whether these acts constitute long-term patterns of behavior. Examples of items used in self-report measures include: “I act on impulse” and “I plan tasks carefully.” The drawbacks of self-report measures include the need to rely on the veracity of the individual completing the questionnaire. In addition, these measures are unsuitable for repeated use, thus limiting their usefulness in treatment studies.
Behavioral Laboratory Measures
Three broad categories of laboratory paradigms have been used to measure impulsivity: 1) punished and/or extinction paradigms (14), 2) reward-choice paradigms (15), and 3) response disinhibition/attentional paradigms (16, 17). The advantages of laboratory measures of impulsivity include their suitability for repeated use, with consequent suitability for treatment studies, and their potential for use in laboratory animals, thus allowing for comparative studies of the basic biochemistry of these behaviors. For example, animal studies using paradigms that are based on reward-choice models and response disinhibition/attentional models have found evidence for a negative correlation between impulsivity and serotonin function (20, 21). The primary disadvantages of these measures are that they do not incorporate the social aspects of impulsivity and do not measure long-term patterns of behavior.
Event-Related Potentials
Electrical brain activity recorded while persons perform various tasks have targeted specific waveforms as potential measures of biological predispositions to impulsiveness. A positive waveform (P300) recorded in response to target stimuli during the performance of a wide range of “oddball” tasks has been related to impulsivity and impulse control disorders (22, 23). The advantage of this type of measure is that it is directly related to brain function. One disadvantage is that, like behavioral laboratory measures, event-related potentials do not incorporate the social aspects of impulsivity. Another disadvantage is that event-related potentials have been reported to be related to a variety of neurologic and psychiatric conditions (24, 25) and thus are not a specific measure of impulsivity. Although event-related potentials are not unique markers, combined with other measures of impulsivity, they are valuable predictors.
The Role of Impulsivity in Psychiatric Disorders
Although impulsivity can be present in any individual with or without a DSM-IV axis I or II diagnosis, it is more likely to be present in individuals with certain psychiatric disorders, such as personality disorders, mania, and substance dependence. The association between these disorders and impulsivity is at least partly due to the manner in which these disorders have been conceptualized, with a lack of behavioral inhibition being an element of all of these disorders. Impulsivity may be related to an underlying mechanism of behavioral inhibition (26, 27). Results of a principal components analysis of the Barratt Impulsiveness Scale suggest a three-factor model of impulsivity that includes greater motor activation, less attention, and less planning (5). In this model, greater motor activation, less attention, or decreased planning are key factors of impulsivity.
Since these three variables have been implicated in impulse control disorders, it is possible that different psychiatric disorders are related to impulsivity through different patterns of these underlying mechanisms. As will be discussed in detail later, frontal lobe brain injury has been reported to lead to symptoms of personality disorders (28). Frontal lobe injury also affects attention and planning (29). Greater motor activation is found in mania (30), and impulsivity is a key aspect of mania (31). Although impulsivity is a key factor in a number of psychiatric disorders and is related to response to treatment, the current diagnostic criteria are problematic because they do not differentiate impulsive from nonimpulsive individuals within diagnostic groups.
Antisocial Personality Disorder
Antisocial personality disorder is probably the psychiatric diagnosis in which the distinction between impulsive and nonimpulsive behaviors is most obvious. Antisocial personality disorder is defined in DSM-IV as “a consistent pattern of disregard for and violation of the rights of others occurring since age 15” (p. 649). The role of impulsivity in antisocial personality disorder as defined by DSM-IV is problematic because “impulsivity or failure to plan ahead” is listed as one of the possible, but not necessary, criteria for the disorder.
Thus, it is likely that subpopulations of individuals with antisocial personality disorder, as categorized by DSM-IV, vary in impulsivity. Evidence for subtypes of antisocial personality disorder differentiated on the basis of impulsivity comes from Barratt et al. (11), who studied aggression among inmates who met DSM-IV criteria for antisocial personality disorder. Responses to a structured interview were used to classify inmates into two groups on the basis of whether they committed impulsive aggressive acts or premeditated aggressive acts. Of the 132 inmates who agreed to participate, 27 (20%) had committed primarily impulsive aggressive acts and 30 (23%) had committed primarily nonimpulsive aggressive acts. The remainder had a mixture of impulsive and premeditated aggressive acts. Three differences between the groups with primarily impulsive aggression versus premeditated aggression support a basic biological/behavioral distinction: 1) the impulsive aggressive inmates had poorer verbal skills, 2) peak P300 evoked-potential amplitudes were significantly lower for the impulsive aggressive inmates, and 3) impulsive aggressive inmates had a significant decrease in aggressive behavior in a double-blind, placebo-controlled trial of the anticonvulsant phenytoin (13).
Other studies of individuals with personality disorders support a biological basis for the dichotomy between impulsive aggressive and nonimpulsive aggressive behavior. In a study by Linnoila et al. (12) involving 36 violent individuals with personality disorders, subjects with impulsive violence had significantly lower levels of the serotonin metabolite 5-hydroxyindoleacetic acid in CSF than individuals who had premeditated violence. Similarly, Coccaro et al. (32) reported a significant correlation between the prolactin response to the serotonin-releasing agent fenfluramine and ratings of impulsive aggression in individuals with personality disorders.
Another possible explanation for the etiology of impulsivity in individuals with antisocial personality disorder is traumatic brain injury. Patients with acquired antisocial personality disorder after head trauma have been described (33). Damage to the frontal cortex is often cited as a source of impulsivity (34), and research has supported the idea that damage to the frontal cortex is a cause of at least some aspects of impulsivity. Bechara et al. (35) found that patients with prefrontal cortical injuries have deficits in distinguishing between choices with good or bad future outcomes and that these deficits are related to lack of a physiological response (skin conductance) before making bad choices.
In summary, a high level of impulsivity is frequently a component of antisocial personality disorder in general, but the degree of impulsivity can vary between individuals with this disorder. Individuals with antisocial personality disorder who have a pattern of impulsive acts, at least of impulsive aggressive acts, are biologically distinct from those without this pattern. In addition, as will be discussed in the later section on treatment, the two groups respond differently to pharmacologic intervention. These facts support the need to look beyond the current nosology in future research on and treatment of antisocial personality disorder.
Borderline Personality Disorder
Impulsivity is one of the DSM-IV diagnostic criteria for borderline personality disorder (p. 654), as are affective instability and identity disturbance. Links et al. (36) recently determined which aspect of borderline personality disorder appeared basic to the disorder. In a stepwise multiple regression, the “impulse action” subscale score from the Diagnostic Interview for Borderline Patients best predicted borderline psychopathology at follow-up. The authors concluded that “impulsivity is stable over time and highly predictive of borderline psychopathology over 7 years’ follow-up” (36).
Several studies have found a relationship between suicidality and impulsivity in patients with borderline personality disorder. In a recent study by Soloff et al. (37), patients with borderline personality disorder (some of whom also had major depression) were compared to patients with major depression alone on measures of depressed mood, hopelessness, impulsive aggression, and suicidal behavior. A higher level of impulsive aggression or hopelessness or a diagnosis of borderline personality disorder predicted a greater number of suicide attempts.
Similarly, in a previous study by Soloff and colleagues (38), borderline personality disorder patients with a history of suicide attempts had more impulsive actions, antisocial personality disorder comorbidity, and depression than those without a history of suicide attempts. To determine which factors are most important in predicting suicidality, Mann et al. (39) examined suicide attempts in patients with mood disorders, psychoses, and other diagnoses. The severity of observer-rated depression or psychosis did not distinguish the patients who had attempted suicide from those who had never attempted suicide. However, rates of lifetime aggression and impulsivity were greater in attempters. Thus, impulsivity appears to be an important factor in suicide attempts in patients with borderline personality disorder.
At least one study that used questionnaire and laboratory measures of impulsivity supported a higher level of impulsivity in patients with borderline personality disorder. Dougherty et al. (10) obtained measures of impulsive behavior for 14 hospitalized women with borderline personality disorder and 17 comparison subjects. The patients with borderline personality disorder responded in ways to avoid longer delays on the laboratory task and had higher Barratt Impulsiveness Scale total scores than the comparison subjects.
In summary, studies of patients with borderline personality disorder have found that impulsivity is a key factor in the diagnosis, linking borderline personality disorder to antisocial personality disorder and (as will be discussed later) to mania. Behavioral and pharmacologic treatment studies of borderline personality disorder that target impulsive behaviors are discussed in detail in the section on treatment approaches.
Substance Abuse/Dependence
Substance abuse is a complex behavior that is not inherently impulsive, according to our definition of impulsivity. However, in response to stress or environmental cues, an individual with substance abuse could use the substance in a rapid unplanned action without regard to the consequences. Once the substance has been used, craving and withdrawal may lead to continued use or dependence (34).
If impulsivity is related to substance use at least in some individuals, it would be expected that the incidence of substance use would be greater in individuals who exhibit other impulsive behaviors. This is in fact the case. In a review by Brady et al. (40) of prior studies of impulsively violent offenders, impulsive arsonists, and individuals with intermittent explosive disorder, higher rates of substance abuse or dependence were found in these groups than in the general population.
Studies measuring impulsivity in substance-dependent individuals have also supported a link between impulsivity and substance abuse. Most studies that use questionnaire measures of impulsivity find higher levels of impulsivity in substance-dependent individuals than in healthy comparison subjects (5, 41, 42), although one study did not find this relationship (43).
Similarly, among substance-dependent individuals, those who are dependent on multiple substances are more impulsive than those who are dependent on single substances (44, 45), and those with borderline personality disorder use more substances and are more impulsive than those who do not meet criteria for borderline personality disorder (46).
Human behavioral laboratory measures of impulsivity also differentiate substance abusers from healthy comparison subjects. Studies using reward-choice paradigms have found that individuals with a history of substance abuse are more likely to choose the more immediate reward even if it is smaller (47–50).
If impulsivity is a factor that leads to substance abuse, children who have difficulty with impulsivity should subsequently have problems with substance abuse. There is a clear association between conduct disorder and substance abuse (51, 52); however, the association between attention deficit hyperactivity disorder (ADHD) and substance abuse is less clear. Some studies have found a higher incidence of substance abuse in adolescents with ADHD (53), and other studies have found that ADHD alone does not increase the risk of substance abuse but that the presence of concomitant conduct disorder does increase the risk (51, 54). The heterogeneity of ADHD, like that of antisocial personality disorder, may be the source of the disagreement between different studies regarding its relationship to substance abuse.
In summary, studies that have used human laboratory and questionnaire measures of impulsivity suggest a high level of impulsivity in substance-dependent populations. The question of whether the higher level of impulsivity is a factor leading to or resulting from substance abuse has not been answered. Likewise, the effect of impulsivity on the treatment of substance abuse remains to be determined, as will be discussed in the section on treatment.
Bipolar Disorder
It is virtually impossible to meet DSM-IV criteria for a manic episode without impulsive behavior (23). Swann et al. (31) recently reported that impulsivity, as reflected in psychiatric rating scale scores, was ubiquitous in manic episodes, while other characteristics varied widely. Depressive episodes are also potentially associated with impulsivity, especially if suicidality is present (55).
Although it may be generally accepted that episodes of illness are associated with impulsivity in bipolar disorder, less is known about impulsivity outside of these episodes. Impulsivity could have any of several relationships to bipolar disorder, possibly depending on the way in which it was measured:
1. Related to susceptibility: adolescents at risk for mania were described in a semistructured evaluation as more “impulsive” than their peers (22).
2. Related to episodes of illness or to prodromes of episodes: increased impulsivity may accompany episodes or may appear earlier in the course of an episode than the diagnostic affective symptoms.
3. Related to risk of complications like suicide (55) or substance abuse (5).
4. Related to response to specific treatments or to treatment in general.
5. Related to pathophysiology of illness: impulsivity could result from some combination of increased norepinephrine (26, 56), decreased serotonin (12), or impaired prefrontal cortex function (34).
Few studies have directly measured impulsivity in bipolar disorder. Swann et al. (57) found a higher level of impulsivity, as measured by the Barratt Impulsiveness Scale, in patients with bipolar disorder than in comparison subjects, even when the patients were between episodes of mania or depression. In the same study, human laboratory measures of impulsivity correlated with severity of manic symptoms in mildly ill patients but did not differ significantly from measures of impulsivity in comparison subjects. There was no correlation with depressive symptoms. These data suggest that, in bipolar and related disorders, impulsivity has both state- and trait-dependent components.
The trait-dependent component, reflected in personality measures such as the Barratt Impulsiveness Scale, may be related to relatively stable biological measures of impulsivity such as level of serotonergic function (58). The state-dependent component, reflected by increased commission errors in a challenging version of the Continuous Performance Test (the IMT-DMT), appears to correlate with severity of manic but not of depressive symptoms (57). This aspect of impulsivity may therefore be related to noradrenergic function, which is increased in manic and mixed states of bipolar disorder and correlates with severity of mania but not of depression (59).
In summary, although few studies have directly measured impulsivity in bipolar disorder, there does appear to be an association between bipolar disorder and impulsivity that goes beyond individual episodes of mood-related illness. Whether interepisode impulsivity is a risk factor for the disorder or a consequence of multiple episodes remains unclear.
ADHD and Conduct Disorder
Along with inattention, hyperactivity and impulsivity are symptoms used to subcategorize children with ADHD in DSM-IV (pp. 83–84). In a study of ADHD subtypes, Willcutt et al. (60) found that the impulsive/hyperactive subtype, but not the inattentive subtype, was associated with a high rate of comorbid symptoms of oppositional defiant disorder and conduct disorder.
Likewise, in a study of adults who had behavior ratings as children, both hyperactive/impulsive symptoms and conduct disorder symptoms predicted adult criminal behavior, but inattention alone did not (61). In a recent study of risk for substance abuse in 626 pairs of adolescent twins (51), conduct disorder but not ADHD increased the risk of substance use and abuse regardless of gender.
Studies using behavioral laboratory measures have found increased impulsivity in children with ADHD. Several studies (62–65) have found that “impulsive” commission errors on the continuous performance test are made more frequently by children with ADHD than by normal comparison subjects.
Various theories have been proposed to explain the etiology of ADHD and conduct disorder. Probably the strongest evidence in humans supporting a role for dopamine has come from treatment studies in which psychostimulants are used to treat ADHD and conduct disorder. Psychostimulants are potent dopamine-releasing agents, although they also lead to increases in the levels of other neurotransmitters, including serotonin and norepinephrine (66). Other evidence supporting a role for dopamine in impulsivity includes findings in genetic studies of a relationship between dopamine transporter and D4 receptor alleles and ADHD (67, 68) and findings of increased activity of dopamine-synthesizing enzymes in brains of children with ADHD (69).
In summary, studies that have used human behavioral laboratory tasks to measure impulsivity have found high levels of impulsivity in ADHD and conduct disorder. Indirect evidence suggests that this increase in impulsivity may be related to dopamine function, which has an impact on treatment of these disorders.
Psychotherapeutic and Pharmacological Approaches to Treatment of Impulsivity
Insight-Oriented Psychotherapy
Fenichel described an “impulse neurosis” in which patients experienced intense ego-syntonic pathological impulses that were often irresistible (70). The source of these impulses was seen as a fusion of instinctual urges and defensive strivings. Patients with an impulse neurosis were further described as having a low frustration tolerance and difficulty postponing immediate reactions or actions. As can be seen from Fenichel’s description, the concept of impulse neurosis incorporates many aspects of what we now call impulsivity.
Examples of psychoanalytic therapies for impulsivity are found primarily in the clinical literature on treatment of borderline personality disorder. Writers of the 1940s–1960s emphasized a supportive, ego-building approach, rather than one that strives to resolve intrapsychic conflict by attacking or undermining defensive functioning (18, 71). This supportive approach stands in contrast to the writings of analytic authors of the 1970s who shifted the focus of therapy toward achieving more fundamental personality change in borderline personality disorder by using more intensive, expressive, and regressive techniques (e.g., reference 72). Modern psychoanalytic techniques have continued to move toward the expressive end of the supportive-expressive continuum (73). The literature on insight-oriented therapies is unfortunately limited by its reliance on uncontrolled reports on small patient samples.
Cognitive Behavior Psychotherapy
Cognitive behavior therapy uses behavior therapy techniques to achieve behavior change through the modification of cognitive processes that lead to problem behaviors (74). Given the research demonstrating deficits in problem-solving abilities in impulsive populations, including drug abusers (75, 76) and juvenile delinquents (77, 78), a strong argument has been made for using cognitive behavior therapy to directly train such individuals in these skills. Platt and colleagues (79) proposed a structured and manualized cognitive behavior therapy program, titled training in interpersonal problem solving. The literature on its effectiveness extends across populations, including chronic psychiatric patients (80), impulsive preschool children (81), and drug-dependent patients (82, 83).
Overall, the empirical evidence suggests that training in interpersonal problem solving improves problem-solving skills and, in some cases, more general outcomes, such as hospital recidivism, arrest rates, and general interpersonal adjustment. Direct assessment of changes in impulsive or aggressive behaviors per se has not been reported in treatment studies that have used training in interpersonal problem solving.
Another type of structured cognitive behavior therapy for the treatment of impulsivity associated with borderline personality disorder is called dialectical behavior therapy, developed by Linehan (84). The approach uses a specific skills training manual for teaching patients general problem-solving skills, emotional regulation strategies, interpersonal skills, and distress tolerance. The efficacy of dialectical behavior therapy has been demonstrated in a study of women with borderline personality disorder (85). Those receiving dialectical behavior therapy had fewer and less severe episodes of parasuicidal behavior and fewer days of hospitalization compared to those receiving treatment as usual in the community.
Cognitive and behavioral therapies have also been used to reduce impulsivity in children. In a meta-analytic review of 36 outcome studies of cognitive behavior treatment in children, Baer and Nietzel (86) reported that these interventions were associated with improvements in impulsivity of approximately one-third to three-quarters of a standard deviation relative to untreated or placebo-treated comparison subjects.
Contingency Management
Of the operant therapies used in treating individuals with impulsive-related disorders, contingency management procedures have received the most clinical and research attention. Contingency management involves the use of predetermined positive or negative consequences to reward or punish (and thus deter) the occurrence of a target behavior.
Thus, a contingency management procedure to decrease impulsivity might arrange consequences to provide an incentive for choosing the less immediate, more planned behavior over the immediate, impulsive action. The most popular application of this type of contingency management procedure is in treating substance use disorders where the target behavior is typically drug abstinence but has included treatment attendance, medication compliance, and other clinic behaviors. Higgins and colleagues (87, 88) have demonstrated in a series of studies that contingency management is superior to noncontingency management interventions in reducing drug use. Impulsivity was not assessed directly in these efficacy studies, making it difficult to draw conclusions about its direct relevance to this procedure.
Reinforcement and response cost contingencies have been used in reducing impulsive behaviors in children. In the classroom, token economy systems have proven to be an effective short-term method for reducing disruptive behavior and promoting on-task, academic behavior (89, 90). Outside the classroom, the efficacy of contingency management procedures has not been demonstrated, and such procedures are generally considered to be impractical in home settings (91). Furthermore, recent studies have shown that contingency management procedures produce smaller gains than stimulants like methylphenidate, and gains engendered by contingency management treatment do not persist once reinforcement is terminated (92). Thus, generalization and maintenance continue to be central problems in using these behavioral reinforcement systems.
Pharmacologic Treatment of Impulsivity
A large number of case reports and open-label trials report efficacy of a wide variety of classes of medication for impulsive behaviors (e.g., references 93, 94). Due to problems associated with open-label studies, this review will focus on placebo-controlled trials.
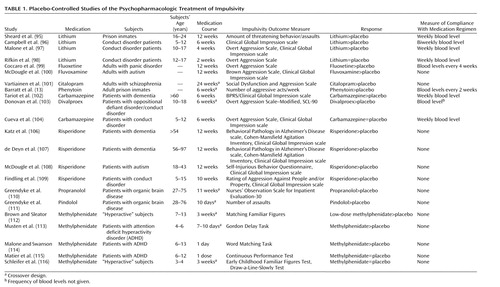
The results of placebo-controlled trials for impulsive behaviors are listed in Table 1. The majority of these studies have focused on the treatment of aggression as an impulse control disorder.
As Table 1 shows, most studies support the efficacy of lithium for impulsive aggression in children, adolescents, and young adults (95–97). One study did not find an improvement compared to placebo, but this study lasted only 2 weeks (98). Unfortunately, lithium has significant side effects that decrease its use (97).
Selective serotonin reuptake inhibitors (SSRIs) and anticonvulsants have also been used successfully to treat impulsive aggression in controlled clinical trials. In a 3-month controlled trial, Coccaro and Kavoussi (99) reported that fluoxetine significantly decreased impulsive aggressive behavior compared to placebo in personality disorder patients. A decrease in aggression was also reported for fluvoxamine, compared to placebo, in autistic adults (100) and for citalopram, compared with placebo, in patients with schizophrenia (101).
Research from other populations supports the efficacy of anticonvulsants for decreasing impulsive aggression. Phenytoin, carbamazepine, and divalproex have all been found to decrease impulsive aggression (13, 102, 103). However, another study (104) found that carbamazepine was not superior to placebo for aggressive behavior and was associated with frequent side effects.
Because of their lack of specificity for aggression, most antipsychotic medications are appropriate only for the treatment of acute aggressive behavior (105). However, there is emerging evidence for a more specific antiaggressive effect of atypical antipsychotic medications. Two placebo-controlled trials of risperidone in adults with dementia reported a significant decrease in aggression without significant sedation (106, 107). Similar results were reported in a placebo-controlled trial of risperidone in adults with autism (108) and in a small study in children with conduct disorder (109).
The β-adrenergic antagonists constitute another class of medications that have been used to treat impulsive aggression. A few small placebo-controlled trials have reported efficacy of propranolol and pindolol for impulsive aggression in populations with organic brain injury (110, 111).
Several controlled studies have found that psychostimulants, compared with placebo, improve attention and decrease impulsivity in patients with ADHD (112–114). Other studies have disagreed, finding that hyperactivity or attention is changed, but not impulsivity (115, 116). The discrepancies in findings regarding the efficacy of stimulants may have resulted from the use of different measures of impulsivity. Further research is needed on the specificity of treatment for impulsivity in ADHD.
Directions for Future Research
Impulsivity as a symptom cuts across a number of psychiatric disorders, and treatment of impulsivity is related to the social, biological, and psychological etiologies of impulsivity. With impulsivity a key factor in so many disorders and an important factor in treatment, it could be argued that biological and psychological research is limited by current diagnostic categories and that a dimensional approach may be more appropriate than the categorical approach used in psychiatric diagnosis and treatment. Before such a change could take place, further research on the measurement of impulsivity and its response to treatment will be needed. The majority of work that has been done in this area has focused on impulsive aggression. This focus is partly the result of the fact that aggressive acts are more easily measured than other aspects of impulsivity. Repeatable measures of impulsivity that capture the core aspects of this behavior are needed. Laboratory measures of impulsivity show promise in this regard, but more work needs to be done in humans to validate these measures in impulsive populations. As Barratt and his colleagues (117, 118) have proposed, the true relationship of impulsivity to behavioral disorders may be best predicted by an “impulsivity index” that combines measurements from behavioral, biological, social, and environmental areas.
Last, as reflected in this review, there is a large body of basic behavioral, personality, biological psychiatry, and neurology research on impulsivity. However, few studies have attempted to integrate these data. To take advantage of the work that has been done, future researchers will benefit from using an ideologically neutral model of impulsivity (118). It is hoped that the definition of impulsivity proposed here is a step in that direction. Development of a more complete understanding of the etiology and treatment of impulsivity will lead to improvements in the treatment of a variety of psychiatric disorders.
 |
Received Oct. 11, 2000; revision received March 19, 2001; accepted April 19, 2001. From the Department of Psychiatry and Behavioral Sciences, University of Texas Houston Health Science Center; and the Department of Psychiatry, University of Texas Medical Branch, Galveston. Address reprint requests to Dr. Moeller, Department of Psychiatry and Behavioral Sciences, University of Texas Houston Health Science Center, 1300 Moursund, Houston, TX 77030; [email protected] (e-mail).Supported in part by grants DA-08425 and DA-00403 from the National Institute on Drug Abuse and by the Department of Psychiatry and Behavioral Sciences, University of Texas Houston Health Science Center.
1. Hinslie L, Shatzky J: Psychiatric Dictionary. New York, Oxford University Press, 1940Google Scholar
2. Smith L: A Dictionary of Psychiatry for the Layman. London, Maxwell, 1952Google Scholar
3. Dickman SJ: Impulsivity and information processing, in The Impulsive Client: Theory, Research, and Treatment. Edited by McCown WG, Johnson JL, Shure MB. Washington, DC, American Psychological Association, 1993, pp 151-184Google Scholar
4. Eysenck SB, Eysenck HJ: The place of impulsiveness in a dimensional system of personality description. Br J Soc Clin Psychol 1977; 16:57-68Crossref, Medline, Google Scholar
5. Patton JH, Stanford MS, Barratt ES: Factor structure of the Barratt Impulsiveness Scale. J Clin Psychol 1995; 51:768-774Crossref, Medline, Google Scholar
6. Stein DJ, Hollander E, Simeon D, Cohen L: Impulsivity scores in patients with obsessive-compulsive disorder. J Nerv Ment Dis 1994; 182:240-241Crossref, Medline, Google Scholar
7. Stein DJ, Trestman RL, Mitropoulou V, Coccaro EF, Hollander E, Siever LJ: Impulsivity and serotonergic function in compulsive personality disorder. J Neuropsychiatry Clin Neurosci 1996; 8:393-398Crossref, Medline, Google Scholar
8. Marinkovic K, Halgren E, Klopp J, Maltzman I: Alcohol effects on movement-related potentials: a measure of impulsivity? J Stud Alcohol 2000; 61:24-31Crossref, Medline, Google Scholar
9. Cherek DR, Moeller FG, Dougherty DM, Rhoades H: Studies of violent and nonviolent male parolees, II: laboratory and psychometric measurements of impulsivity. Biol Psychiatry 1997; 41:523-529Crossref, Medline, Google Scholar
10. Dougherty DM, Bjork JM, Huckabee HC, Moeller FG, Swann AC: Laboratory measures of aggression and impulsivity in women with borderline personality disorder. Psychiatry Res 1999; 85:315-326Crossref, Medline, Google Scholar
11. Barratt ES, Stanford MS, Kent TA, Felthous A: Neuropsychological and cognitive psychophysiological substrates of impulsive aggression. Biol Psychiatry 1997; 41:1045-1061Crossref, Medline, Google Scholar
12. Linnoila M: Low cerebrospinal fluid 5-hydroxyindoleacetic acid concentration differentiates impulsive from nonimpulsive violent behavior. Life Sci 1983; 33:2609-2614Crossref, Medline, Google Scholar
13. Barratt ES, Stanford MS, Felthous AR, Kent TA: The effects of phenytoin on impulsive and premeditated aggression: a controlled study. J Clin Psychopharmacol 1997; 17:341-349Crossref, Medline, Google Scholar
14. Matthys W, van Goozen SH, de Vries H, Cohen-Kettenis PT, van Engeland H: The dominance of behavioural activation over behavioural inhibition in conduct disordered boys with or without attention deficit hyperactivity disorder. J Child Psychol Psychiatry 1998; 39:643-651Crossref, Medline, Google Scholar
15. Ainslie G: Specious reward: a behavioral theory of impulsiveness and impulse control. Psychol Bull 1975; 82:463-496Crossref, Medline, Google Scholar
16. Dougherty DM, Moeller FG, Steinberg JL, Marsh DM, Hines SE, Bjork JM: Alcohol increases commission error rates for a continuous performance test. Alcohol Clin Exp Res 1999; 23:1342-1351Crossref, Medline, Google Scholar
17. Halperin JM, Wolf L, Greenblatt ER, Young G: Subtype analysis of commission errors on the Continuous Performance Test. Dev Neuropsychol 1991; 7:207-217Crossref, Google Scholar
18. L’Abate L: A family theory of impulsivity, in The Impulsive Client. Edited by McCown WG, Johnson JL, Shure MB. Washington, DC, American Psychological Association, 1993, pp 93-117Google Scholar
19. Eysenck SB, Pearson PR, Easting G, Allsopp JF: Age norms for impulsiveness, venturesomeness and empathy in adults. Personality and Individual Differences 1985; 6:613-619Crossref, Google Scholar
20. Evenden JL: The pharmacology of impulsive behaviour in rats, VII: the effects of serotonergic agonists and antagonists on responding under a discrimination task using unreliable visual stimuli. Psychopharmacology (Berl) 1999; 146:422-431Crossref, Medline, Google Scholar
21. Puumala T, Sirvio J: Changes in activities of dopamine and serotonin systems in the frontal cortex underlie poor choice accuracy and impulsivity of rats in an attention task. Neuroscience 1998; 83:489-499Crossref, Medline, Google Scholar
22. Sunohara GA, Malone MA, Rovet J, Humphries T, Roberts W, Taylor MJ: Effect of methylphenidate on attention in children with attention deficit hyperactivity disorder (ADHD): ERP evidence. Neuropsychopharmacology 1999; 21:218-228Crossref, Medline, Google Scholar
23. Harmon-Jones E, Barratt ES, Wigg C: Impulsiveness, aggression, reading, and the P300 of the event-related potential. Personality and Individual Differences 1997; 22:439-445Crossref, Google Scholar
24. Korpelainen JT, Kauhanen ML, Tolonen U, Brusin E, Mononen H, Hiltunen P, Sotaniemi KA, Suominen K, Myllyla VV: Auditory P300 event related potential in minor ischemic stroke. Acta Neurol Scand 2000; 101:202-208Crossref, Medline, Google Scholar
25. Iwanami A, Okajima Y, Kuwakado D, Isono H, Kasai K, Hata A, Nakagome K, Fukuda M, Kamijima K: Event-related potentials and thought disorder in schizophrenia. Schizophr Res 2000; 42:187-191Crossref, Medline, Google Scholar
26. Gray JA: A model of the limbic system and basal ganglia: applications to anxiety and schizophrenia, in The Cognitive Neurosciences. Edited by Gazzaniga MS. Cambridge, Mass, MIT Press, 1995, pp 1165-1176Google Scholar
27. Rachlin H: The Science of Self Control. Cambridge, Mass, Harvard University Press, 2000Google Scholar
28. Damasio AR, Tranel D, Damasio H: Individuals with sociopathic behavior caused by frontal damage fail to respond autonomically to social stimuli. Behav Brain Res 1990; 41:81-94Crossref, Medline, Google Scholar
29. Spikman JM, Deelman BG, van Zomeren AH: Executive functioning, attention and frontal lesions in patients with chronic CHI. J Clin Exp Neuropsychol 2000; 22:325-338Crossref, Medline, Google Scholar
30. Cassidy F, Murry E, Forest K, Carroll BJ: Signs and symptoms of mania in pure and mixed episodes. J Affect Disord 1998; 50:187-201Crossref, Medline, Google Scholar
31. Swann AC, Janicak PL, Calabrese JR, Bowden CL, Dilsaver SC, Morris DD, Petty F, Davis LL: Structure of mania: subgroups with distinct clinical characteristics and course of illness in randomized clinical trial participants. J Affect Disord (in press)Google Scholar
32. Coccaro EF, Siever LJ, Klar HM, Maurer G, Cochrane K, Cooper TB, Mohs RC, Davis KL: Serotonergic studies in patients with affective and personality disorders: correlates with suicidal and impulsive aggressive behavior. Arch Gen Psychiatry 1989; 46:587-599Crossref, Medline, Google Scholar
33. Blair RJ, Cipolotti L: Impaired social response reversal: a case of “acquired sociopathy.” Brain 2000; 123:1122-1141Crossref, Medline, Google Scholar
34. Jentsch JD, Taylor JR: Impulsivity resulting from frontostriatal dysfunction in drug abuse: implications for the control of behavior by reward-related stimuli. Psychopharmacology (Berl) 1999; 146:373-390Crossref, Medline, Google Scholar
35. Bechara A, Damasio H, Tranel D, Damasio AR: Deciding advantageously before knowing the advantageous strategy. Science 1997; 275:1293-1295Crossref, Medline, Google Scholar
36. Links PS, Heslegrave R, van Reekum R: Impulsivity: core aspect of borderline personality disorder. J Personal Disord 1999; 13:1-9Crossref, Medline, Google Scholar
37. Soloff PH, Lynch KG, Kelly TM, Malone KM, Mann JJ: Characteristics of suicide attempts of patients with major depressive episode and borderline personality disorder: a comparative study. Am J Psychiatry 2000; 157:601-608Link, Google Scholar
38. Soloff PH, Lis JA, Kelly T, Cornelius J, Ulrich R: Risk factors for suicidal behavior in borderline personality disorder. Am J Psychiatry 1994; 151:1316-1323Link, Google Scholar
39. Mann JJ, Waternaux C, Haas GL, Malone KM: Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry 1999; 156:181-189Abstract, Google Scholar
40. Brady KT, Myrick H, McElroy S: The relationship between substance use disorders, impulse control disorders, and pathological aggression. Am J Addict 1998; 7:221-230Crossref, Medline, Google Scholar
41. Allen TJ, Moeller FG, Rhoades HM, Cherek DR: Impulsivity and history of drug dependence. Drug Alcohol Depend 1998; 50:137-145Crossref, Medline, Google Scholar
42. Moss HB, Yao JK, Panzak GL: Serotonergic responsivity and behavioral dimensions in antisocial personality disorder with substance abuse. Biol Psychiatry 1990; 28:325-338Crossref, Medline, Google Scholar
43. Lejoyeux M, Feuche N, Loi S, Solomon J, Ades J: Impulse-control disorders in alcoholics are related to sensation seeking and not to impulsivity. Psychiatry Res 1998; 81:149-155Crossref, Medline, Google Scholar
44. McCown WG: Multi-impulsive personality disorder and multiple substance abuse: evidence from members of self-help groups. Br J Addict 1988; 83:431-432Crossref, Medline, Google Scholar
45. O’Boyle M, Barratt ES: Impulsivity and DSM-III-R personality disorders. Personality and Individual Differences 1993; 14:609-611Crossref, Google Scholar
46. Kruedelbach N, McCormick RA, Schulz SC, Grueneich R: Impulsivity, coping styles, and triggers for craving in substance abusers with borderline personality disorder. J Personal Disord 1993; 7:214-222Crossref, Google Scholar
47. Kirby KN, Petry NM, Bickel WK: Heroin addicts have higher discount rates for delayed rewards than non-drug-using controls. J Exp Psychol Gen 1999; 128:78-87Crossref, Medline, Google Scholar
48. Mitchell SH: Measures of impulsivity in cigarette smokers and non-smokers. Psychopharmacology (Berl) 1999; 146:455-464Crossref, Medline, Google Scholar
49. Madden GJ, Petry NM, Badger GJ, Bickel WK: Impulsive and self-control choices in opioid-dependent patients and non-drug-using control patients: drug and monetary rewards. Exp Clin Psychopharmacol 1997; 5:256-262Crossref, Medline, Google Scholar
50. Vuchinich RE, Simpson CA: Hyperbolic temporal discounting in social drinkers and problem drinkers. Exp Clin Psychopharmacol 1998; 6:292-305Crossref, Medline, Google Scholar
51. Disney ER, Elkins IJ, McGue M, Iacono WG: Effects of ADHD, conduct disorder, and gender on substance use and abuse in adolescence. Am J Psychiatry 1999; 156:1515-1521Link, Google Scholar
52. Young SE, Mikulich SK, Goodwin MB, Hardy J, Martin CL, Zoccolillo MS, Crowley TJ: Treated delinquent boys’ substance use: onset, pattern, relationship to conduct and mood disorders. Drug Alcohol Depend 1995; 37:149-162Crossref, Medline, Google Scholar
53. Chilcoat HD, Breslau N: Pathways from ADHD to early drug use. J Am Acad Child Adolesc Psychiatry 1999; 38:1347-1354Crossref, Medline, Google Scholar
54. Molina BSG, Smith BH, Pelham WE: Interactive effects of attention deficit hyperactivity disorder and conduct disorder on early adolescent substance use. Psychol Addict Behav 1999; 13:348-358Crossref, Google Scholar
55. Corruble E, Damy C, Guelfi JD: Impulsivity: a relevant dimension in depression regarding suicide attempts? J Affect Disord 1999; 53:211-215Crossref, Medline, Google Scholar
56. Coccaro EF: Central serotonin and impulsive aggression. Br J Psychiatry Suppl 1989; 8:52-62Medline, Google Scholar
57. Swann AC, Anderson JC, Dougherty DM, Moeller FG: Measurement of inter-episode impulsivity in bipolar disorder. Psychiatry Res 2001; 101:195-197Crossref, Medline, Google Scholar
58. Manuck SB, Flory JD, McCaffery JM, Matthews KA, Mann JJ, Muldoon MF: Aggression, impulsivity, and central nervous system serotonergic responsivity in a nonpatient sample. Neuropsychopharmacology 1998; 19:287-299Crossref, Medline, Google Scholar
59. Swann AC, Koslow SH, Katz MM, Maas JW, Javaid J, Secunda SK, Robins E: Lithium carbonate treatment of mania: cerebrospinal fluid and urinary monoamine metabolites and treatment outcome. Arch Gen Psychiatry 1987; 44:345-354Crossref, Medline, Google Scholar
60. Willcutt EG, Pennington BF, Chhabildas NA, Friedman MC, Alexander J: Psychiatric comorbidity associated with DSM-IV ADHD in a nonreferred sample of twins. J Am Acad Child Adolesc Psychiatry 1999; 38:1355-1362Crossref, Medline, Google Scholar
61. Babinski LM, Hartsough CS, Lambert NM: Childhood conduct problems, hyperactivity-impulsivity, and inattention as predictors of adult criminal activity. J Child Psychol Psychiatry 1999; 40:347-355Crossref, Medline, Google Scholar
62. Sykes DH, Douglas VI, Morganstern G: Sustained attention in hyperactive children. J Child Psychol Psychiatry 1973; 14:213-220Crossref, Medline, Google Scholar
63. O’Toole K, Abramowitz A, Morris R, Dulcan MK: Effects of methylphenidate and nonverbal learning in children with attention-deficit hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 1997; 36:531-538Crossref, Medline, Google Scholar
64. Halperin JM, Wolf LE, Pascualvaca DM, Newcorn JH, Healey JM, O’Brien JD, Morganstein A, Young JG: Differential assessment of attention and impulsivity in children. J Am Acad Child Adolesc Psychiatry 1988; 27:326-329Crossref, Medline, Google Scholar
65. Dykman RA, Ackerman PT, Oglesby DM: Selective and sustained attention in hyperactive, learning-disabled and normal boys. J Nerv Ment Dis 1979; 167:288-297Crossref, Medline, Google Scholar
66. Cooper JR, Bloom FE, Roth RH: The Biochemical Basis of Neuropharmacology. New Haven, Conn, Yale University Press, 1996Google Scholar
67. Daly G, Hawi Z, Fitzgerald M, Gill M: Mapping susceptibility loci in attention deficit hyperactivity disorder: preferential transmission of parental alleles at DAT1, DBH and DRD5 to affected children. Mol Psychiatry 1999; 4:192-196Crossref, Medline, Google Scholar
68. Smalley SL, Bailey JN, Palmer CG, Cantwell DP, McGough JJ, Del’Homme MA, Asarnow JR, Woodward JA, Ramsey C, Nelson SF: Evidence that the dopamine D4 receptor is a susceptibility gene in attention deficit hyperactivity disorder. Mol Psychiatry 1998; 3:427-430Crossref, Medline, Google Scholar
69. Ernst M, Zametkin AJ, Matochik JA, Pascualvaca D, Jons PH, Cohen RM: High midbrain [18F]DOPA accumulation in children with attention deficit hyperactivity disorder. Am J Psychiatry 1999; 156:1209-1215Abstract, Google Scholar
70. Fenichel O: The Psychoanalytic Theory of Neurosis. New York, WW Norton, 1945Google Scholar
71. Frosch J: Technique in regard to some specific ego defects in the treatment of borderline patients. Psychiatr Q 1971; 45:216-220Crossref, Medline, Google Scholar
72. Kernberg OF: Borderline Conditions and Pathological Narcissism. New York, Jason Aronson, 1975Google Scholar
73. Aronson TA: A critical review of psychotherapeutic treatments of borderline personality. J Nerv Ment Dis 1989; 177:511-528Crossref, Medline, Google Scholar
74. Gray JA: A theory of anxiety: the role of the limbic system. Encephale 1983; 9:161B-166BMedline, Google Scholar
75. Appel PW, Kaestner E: Interpersonal and emotional problem-solving among narcotic drug abusers. J Consult Clin Psychol 1979; 47:1125-1127Crossref, Medline, Google Scholar
76. Platt JJ, Scura WC, Hannon JR: Problem-solving thinking of youthful incarcerated heroin addicts. J Community Psychol 1973; 1:278-291Crossref, Google Scholar
77. Platt JJ, Spivack G, Altman N, Altman D, Peizer SB: Adolescent problem-solving thinking. J Consult Clin Psychol 1974; 42:787-793Crossref, Medline, Google Scholar
78. Spivack G, Levine M: Self-Regulation in Acting-Out and Normal Adolescents: Report M-4531. Washington, DC, National Institutes of Health, 1963Google Scholar
79. Platt JJ, Taube DO, Metzger D, Duome MAJ: Training in interpersonal problem solving (TIPS). J Cognitive Psychotherapy 1988; 2:5-34Crossref, Google Scholar
80. Hansen DJ, St Lawrence JS, Christoff KA: Effects of interpersonal problem-solving training with chronic aftercare patients on problem-solving component skills and effectiveness of solutions. J Consult Clin Psychol 1985; 53:167-174Crossref, Medline, Google Scholar
81. Shure MB, Spivack G: Interpersonal problem solving in young children: a cognitive approach to prevention. Am J Community Psychol 1982; 10:341-356Crossref, Medline, Google Scholar
82. Intagliata J: Increasing the interpersonal problem-solving skills of an alcoholic population. J Consult Clin Psychol 1978; 46:489-498Crossref, Medline, Google Scholar
83. Platt JJ, McKim P, Husband SD: TIPS: Training in Interpersonal Problem Solving: Enhanced Health Promotion and AIDS Prevention Program: Trainer’s Manual. Camden, University of Medicine and Dentistry of New Jersey, 1990Google Scholar
84. Linehan MM: Dialectical behavioral therapy in groups: treating borderline personality disorders and suicidal behavior, in Women’s Therapy Groups: Paradigms of Feminist Treatment. Edited by Brody CM. New York, Springer, 1987, pp 145-162Google Scholar
85. Linehan MM, Armstrong HE, Suarez A, Allmon D, Heard HL: Cognitive-behavioral treatment of chronically parasuicidal borderline patients. Arch Gen Psychiatry 1991; 48:1060-1064Crossref, Medline, Google Scholar
86. Baer RA, Nietzel MT: Cognitive and behavioral treatment of impulsivity in children: a meta-analytic review of the outcome literature. J Clin Child Psychol 1991; 20:400-412Crossref, Google Scholar
87. Higgins ST, Stitzer ML, Bigelow GE, Liebson IA: Contingent methadone delivery: effects on illicit-opiate use. Drug Alcohol Depend 1986; 17:311-322Crossref, Medline, Google Scholar
88. Higgins ST, Wong CJ, Badger GJ, Ogden DE, Dantrona RL: Contingent reinforcement increases cocaine abstinence during outpatient treatment and 1 year of follow-up. J Consult Clin Psychol 2000; 68:64-72Crossref, Medline, Google Scholar
89. Ayllon T, Layman D, Kendel HJ: A behavioral-educational alternative to drug control of hyperactive children. J Appl Behav Anal 1975; 8:137-146Crossref, Medline, Google Scholar
90. Rosen LA, O’Leary KD, Jacob RG: Behavioral intervention with hyperactive children. Behavior Therapy 1975; 6:315-323Crossref, Google Scholar
91. Hinshaw SP, Erhardt D: Behavioral treatment, in Handbook of Behavior Therapy and Pharmacotherapy for Children: A Comparative Analysis. Edited by Van Hasselt VB, Hersen M. Boston, Allyn and Bacon, 1993, pp 233-250Google Scholar
92. Pelham WE, Carlson C, Sams SE, Vallano G, Dixon MJ, Hoza B: Separate and combined effects of methylphenidate and behavior modification on boys with attention deficit hyperactivity disorder in the classroom. J Consult Clin Psychol 1993; 61:506-515Crossref, Medline, Google Scholar
93. Jensen HV, Andersen J: An open, noncomparative study of amoxapine in borderline disorders. Acta Psychiatr Scand 1989; 79:89-93Crossref, Medline, Google Scholar
94. Kavoussi RJ, Coccaro EF: Divalproex sodium for impulsive aggressive behavior in patients with personality disorder. J Clin Psychiatry 1998; 59:676-680Crossref, Medline, Google Scholar
95. Sheard MH, Marini JL, Bridges CI, Wagner E: The effect of lithium on impulsive aggressive behavior in man. Am J Psychiatry 1976; 133:1409-1413Link, Google Scholar
96. Campbell M, Adams PB, Small AM, Kafantaris V, Silva RR, Shell J, Perry R, Overall JE: Lithium in hospitalized aggressive children with conduct disorder: a double-blind and placebo-controlled study. J Am Acad Child Adolesc Psychiatry 1995; 34:445-453Crossref, Medline, Google Scholar
97. Malone RP, Delaney MA, Luebbert JF, Cater J, Campbell M: A double-blind placebo-controlled study of lithium in hospitalized aggressive children and adolescents with conduct disorder. Arch Gen Psychiatry 2000; 57:649-654Crossref, Medline, Google Scholar
98. Rifkin A, Karajgi B, Dicker R, Perl E, Boppana V, Hasan N, Pollack S: Lithium treatment of conduct disorders in adolescents. Am J Psychiatry 1997; 154:554-555Link, Google Scholar
99. Coccaro EF, Kavoussi RJ: Fluoxetine and impulsive aggressive behavior in personality-disordered subjects. Arch Gen Psychiatry 1997; 54:1081-1088Crossref, Medline, Google Scholar
100. McDougle CJ, Naylor ST, Cohen DJ, Volkmar FR, Heninger GR, Price LH: A double-blind, placebo-controlled study of fluvoxamine in adults with autistic disorder. Arch Gen Psychiatry 1996; 53:1001-1008Crossref, Medline, Google Scholar
101. Vartiainen H, Tiihonen J, Putkonen A, Koponen H, Virkkunen M, Hakola P, Lehto H: Citalopram, a selective serotonin reuptake inhibitor, in the treatment of aggression in schizophrenia. Acta Psychiatr Scand 1995; 91:348-351Crossref, Medline, Google Scholar
102. Tariot PN, Erb R, Podgorski CA, Cox C, Patel S, Jakimovich L, Irvine C: Efficacy and tolerability of carbamazepine for agitation and aggression in dementia. Am J Psychiatry 1998; 155:54-61Link, Google Scholar
103. Donovan SJ, Stewart JW, Nunes EV, Quitkin FM, Parides M, Daniel W, Susser E, Klein DF: Divalproex treatment for youth with explosive temper and mood lability: a double-blind, placebo-controlled crossover design. Am J Psychiatry 2000; 157:818-820Link, Google Scholar
104. Cueva JE, Overall JE, Small AM, Armenteros JL, Perry R, Campbell M: Carbamazepine in aggressive children with conduct disorder: a double-blind and placebo-controlled study. J Am Acad Child Adolesc Psychiatry 1996; 35:480-490Crossref, Medline, Google Scholar
105. Fava M: Psychopharmacologic treatment of pathologic aggression. Psychiatr Clin North Am 1997; 20:427-451Crossref, Medline, Google Scholar
106. Katz IR, Jeste DV, Mintzer JE, Clyde C, Napolitano J, Brecher M: Comparison of risperidone and placebo for psychosis and behavioral disturbances associated with dementia: a randomized, double-blind trial: Risperidone Study Group. J Clin Psychiatry 1999; 60:107-115Crossref, Medline, Google Scholar
107. de Deyn PP, Rabheru K, Rasmussen A, Bocksberger JP, Dautzenberg PL, Eriksson S, Lawlor BA: A randomized trial of risperidone, placebo, and haloperidol for behavioral symptoms of dementia. Neurology 1999; 53:946-955Crossref, Medline, Google Scholar
108. McDougle CJ, Holmes JP, Carlson DC, Pelton GH, Cohen DJ, Price LH: A double-blind, placebo-controlled study of risperidone in adults with autistic disorder and other pervasive developmental disorders. Arch Gen Psychiatry 1998; 55:633-641Crossref, Medline, Google Scholar
109. Findling RL, McNamara NK, Branicky LA, Schluchter MD, Lemon E, Blumer JL: A double-blind pilot study of risperidone in the treatment of conduct disorder. J Am Acad Child Adolesc Psychiatry 2000; 39:509-516Crossref, Medline, Google Scholar
110. Greendyke RM, Kanter DR: Therapeutic effects of pindolol on behavioral disturbances associated with organic brain disease: a double-blind study. J Clin Psychiatry 1986; 47:423-426Medline, Google Scholar
111. Greendyke RM, Kanter DR, Schuster DB, Verstreate S, Wootton J: Propranolol treatment of assaultive patients with organic brain disease: a double-blind crossover, placebo-controlled study. J Nerv Ment Dis 1986; 174:290-294Crossref, Medline, Google Scholar
112. Brown RT, Sleator EK: Methylphenidate in hyperkinetic children: differences in dose effects on impulsive behavior. Pediatrics 1979; 64:408-411Medline, Google Scholar
113. Musten LM, Firestone P, Pisterman S, Bennett S, Mercer J: Effects of methylphenidate on preschool children with ADHD: cognitive and behavioral functions. J Am Acad Child Adolesc Psychiatry 1997; 36:1407-1415Crossref, Medline, Google Scholar
114. Malone MA, Swanson JM: Effects of methylphenidate on impulsive responding in children with attention-deficit hyperactivity disorder. J Child Neurol 1993; 8:157-163Crossref, Medline, Google Scholar
115. Matier K, Halperin JM, Sharma V, Newcorn JH, Sathaye N: Methylphenidate response in aggressive and nonaggressive ADHD children: distinctions on laboratory measures of symptoms. J Am Acad Child Adolesc Psychiatry 1992; 31:219-225Crossref, Medline, Google Scholar
116. Schleifer M, Weiss G, Cohen N, Elman M, Cvejic H, Kruger E: Hyperactivity in preschoolers and the effect of methylphenidate. Am J Orthopsychiatry 1975; 45:38-50Crossref, Medline, Google Scholar
117. Barratt ES: Impulsivity: integrating cognitive, behavioral, biological, and environmental data, in The Impulsive Client. Edited by McCown WG, Johnson JL, Shure MB. Washington, DC, American Psychological Association, 1993, pp 39-53Google Scholar
118. Barratt ES, Slaughter L: Defining, measuring, and predicting impulsive aggression: a heuristic model. Behav Sci Law 1998; 16:285-302Crossref, Medline, Google Scholar



