Age-Dependent Decline of Symptoms of Attention Deficit Hyperactivity Disorder: Impact of Remission Definition and Symptom Type
Abstract
OBJECTIVE: Symptom decline in attention deficit hyperactivity disorder (ADHD) was examined with different definitions of remission.METHOD: Symptoms in 128 boys were measured five times over 4 years. The prevalences of syndromatic (less than full syndrome), symptomatic (less than subthreshold diagnosis), and functional (full recovery) remission were estimated as a function of age with multivariate logistic regression.RESULTS: Age was significantly associated with decline in total ADHD symptoms and symptoms of hyperactivity, impulsivity, and inattention. Symptoms of inattention remitted for fewer subjects than did symptoms of hyperactivity or impulsivity. The proportion of subjects experiencing remission varied considerably with the definition used (highest for syndromatic remission, lowest for functional remission).CONCLUSIONS: These results indicate that differences in reported remission rates reflect the definition used rather than the disorder’s course. They provide systematic support for the clinical observation that hyperactivity and impulsivity symptoms tend to decline at a higher rate than inattention symptoms.
Although follow-up studies have consistently documented the persistence of attention deficit hyperactivity disorder (ADHD) into adolescence and adulthood, the level of persistence has been inconsistent across studies (1–3). One possible explanation for these discrepant results is the use of different definitions of remission across studies. As recently proposed by Keck et al. (4), the distinction between different types of remission may clarify components of complex recovery processes. Syndromatic remission refers to the loss of full diagnostic status, symptomatic remission refers to the loss of partial diagnostic status, and functional remission refers to the loss of partial diagnostic status plus functional recovery (full recovery). The purpose of this report was to use our longitudinal sample of carefully diagnosed ADHD children to examine these three different patterns of remission with regard to ADHD symptoms.
Method
The original sample consisted of 140 ADHD and 120 normal comparison Caucasian boys ascertained from psychiatric and nonpsychiatric settings who were assessed at baseline and at 1- and 4-year follow-ups (5). Psychiatric assessments were made with the Schedule for Affective Disorders and Schizophrenia for School-Age Children—Epidemiologic Version (6) and were based on independent interviews with the mothers and direct interviews of the subjects, except for children younger than 12 years, whose diagnoses were based on maternal report only. Only the ADHD subjects who returned for the 4-year follow-up are included in this analysis (N=128). As we have reported elsewhere (5), there were no significant differences between the subjects successfully followed up and those lost to follow up on measures of ADHD severity, psychiatric comorbidity, psychosocial functioning, or cognitive functioning. For each ADHD subject, we had observations of symptoms at five time points: 1) symptoms that had occurred at the disorder’s onset, as reported retrospectively during the baseline assessment; 2) symptoms that were currently active at baseline; 3) symptoms that were currently active at the year 1 follow-up assessment; 4) symptoms that were active at the beginning of the 2-year interval covered by the 4-year follow-up, according to subject recall; and 5) symptoms that were active in the most recent month at the final follow-up assessment.
The 14 DSM-III-R symptoms of ADHD were grouped into clusters by type: inattentive (six symptoms), hyperactive (four symptoms), and impulsive (four symptoms). The number of symptoms in each cluster was determined for each subject. On the basis of the classification of Keck et al. (4), we defined “syndromatic remission” as failing to meet the full diagnostic criteria for ADHD (i.e., having fewer than eight of the 14 possible symptoms, or 57%). “Symptomatic remission” required that the subject have fewer than the number of symptoms required for a subthreshold diagnosis (i.e., fewer than five symptoms, or 36% of symptoms) regardless of impairment, while “functional remission” required that the subject have fewer than 36% of the symptoms of ADHD and no impairment (score on the Global Assessment of Functioning Scale higher than 60). The same categories were created for each of the ADHD symptom clusters.
Symptom decline was modeled as a function of age at each assessment. Because the repeated measurements of our 128 ADHD subjects were not independent from each other, model-based tests of statistical significance would be incorrect. To account for this bias we adjusted our analyses by using generalized estimating equations to produce robust statistical tests in each of the logistic regression models. All statistical tests were two-tailed at the 0.05 level of statistical significance.
Results
The prevalences of each type of remission for all ADHD symptoms and for each symptom cluster were modeled as a function of the following age categories: <6 years, 6–8 years, 9–11 years, 12–14 years, 15–17 years, and 18–20 years (Figure 1). Although age was significantly associated with all forms of remission for ADHD and the three symptom clusters (Wald χ2>5.1 in all cases, df=1, p<0.02 in all cases), the prevalence of remission varied considerably. For example, in the oldest age group (18–20 years) the prevalence of syndromatic ADHD remission was greater than 60%, while the rate of functional ADHD remission was only 10%. The prevalence of remission of inattentiveness was lower than the rate of remission of either hyperactivity or impulsivity. This was most apparent for the syndromatic and symptomatic definitions of remission and less so for the functional definition of remission (Figure 1).
Discussion
Our results show that patterns of remission of ADHD are highly sensitive to the definition of remission and suggest that the differences in remission reported in the literature (1–3, 7, 8) reflect the variable definitions of remission used rather than the natural history of the disorder. While our rate of syndromatic remission (60%) is in full agreement with the rate of syndromatic remission (65%–70%) estimated by Hill and Schoener (8), our results also indicate that a majority of subjects continue to struggle with a substantial number of ADHD symptoms and high levels of dysfunction despite a sizable rate of syndromatic remission by the age of 20.
Although the definition of remission affected the rate of symptom decline for the ADHD core symptom types, inattention was more persistent than hyperactivity or impulsivity within each definition of remission. These results provide systematic support for the long-held clinical observation that symptoms of hyperactivity and impulsivity tend to decline at a higher rate and at an earlier age that those of inattention.
The findings reported here should be viewed against methodological limitations. Because we studied clinically referred, Caucasian boys, our results may not generalize to ADHD in the community, to girls with ADHD, or to children with ADHD in other racial or ethnic groups. We also did not stratify our data by social class and, therefore, did not account for this potentially important predictor of outcome. Despite these considerations, our results stress the critical importance of different definitions of remission in assessing the longitudinal course of children and adolescents with ADHD. These results also show that symptom clusters, as represented by the DSM-IV ADHD subtypes, should be considered separately.
Received Feb. 8, 1999; revisions received June 30 and Oct. 13, 1999; accepted Oct. 28, 1999. From the Pediatric Psychopharmacology Unit, Psychiatry Service, Massachusetts General Hospital; the Massachusetts Mental Health Center, Commonwealth Research Center, Harvard Institute of Psychiatric Epidemiology and Genetics, Boston; and the Department of Psychiatry, Harvard Medical School, Boston. No reprints are available. Address correspondence to Dr. Biederman, Pediatric Psychopharmacology Unit, Massachusetts General Hospital, ACC 725, 15 Parkman St., Boston, MA 02114; [email protected] (e-mail). Supported by NIMH grant MH-41314.
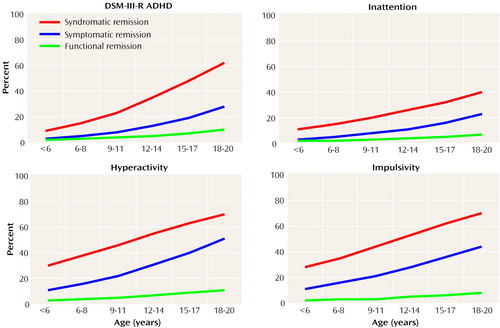
Figure 1. Age-Specific Prevalence of Remission From ADHD Among 128 Boys, According to Definition of Remission and Symptom Typea
aSyndromatic remission: failing to meet the full diagnostic criteria for ADHD (ie., having fewer than eight of 14 possible symptoms). Symptomatic remission: having fewer than the number of symptoms required for a subthreshold diagnosis (i.e., fewer than five symptoms). Functional remission: having fewer than five ADHD symptoms and no impairment (score on the Global Assessment of Functioning Scale higher than 60).
1. Barkley RA, Fischer M, Edelbrock CS, Smallish L: The adolescent outcome of hyperactive children diagnosed by research criteria, I: an 8-year prospective follow-up study. J Am Acad Child Adolesc Psychiatry 1990; 29:546–557Crossref, Medline, Google Scholar
2. Weiss G, Hechtman L, Milroy T, Perlman T: Psychiatric status of hyperactives as adults: a controlled prospective 15-year follow-up of 63 hyperactive children. J Am Acad Child Psychiatry 1985; 24:211–220Crossref, Medline, Google Scholar
3. Mannuzza S, Klein RG, Bessler A, Malloy P, LaPadula M: Adult outcome of hyperactive boys: educational achievement, occupational rank and psychiatric status. Arch Gen Psychiatry 1993; 50:565–576Crossref, Medline, Google Scholar
4. Keck PE Jr, McElroy SL, Strakowski SM, West SA, Sax KW, Hawkins JM, Bourne ML, Haggard P:12-month outcome of patients with bipolar disorder following hospitalization for a manic or mixed episode. Am J Psychiatry 1998; 155:646–652Google Scholar
5. Biederman J, Faraone S, Milberger S, Guite J, Mick E, Chen L, Mennin D, Marrs A, Ouellette C, Moore P, Spencer T, Norman D, Wilens T, Kraus I, Perrin J: A prospective four-year follow-up study of attention deficit hyperactivity and related disorders. Arch Gen Psychiatry 1996; 53:437–446Crossref, Medline, Google Scholar
6. Schedule for Affective Disorder and Schizophrenia for School-Age Children—Epidemiologic Version. Ft Lauderdale, Fla, Nova Southeastern University, Center for Psychological Studies, 1994Google Scholar
7. Mannuzza S, Klein RG, Bessler A, Malloy P, LaPadula M: Adult psychiatric status of hyperactive boys grown up. Am J Psychiatry 1998; 155:493–498Link, Google Scholar
8. Hill JC, Schoener EP: Age-dependent decline of attention deficit hyperactivity disorder. Am J Psychiatry 1996; 153:1143–1146Google Scholar



