Untreated Initial Psychosis: Its Relation to Quality of Life and Symptom Remission in First-Episode Schizophrenia
Abstract
OBJECTIVE: Previous studies have suggested that there may be an association between longer duration of untreated psychosis and poor outcome in schizophrenia. These studies have been interpreted as providing evidence that untreated psychosis may constitute an “active morbid process” that is “toxic” to the brain. If untreated psychosis is neurotoxic, this would form a strong basis for early intervention in schizophrenia. METHOD: Seventy-four neuroleptic-naive patients with DSM-IV schizophrenia were evaluated 6 months after their first inpatient hospitalization. The authors examined the relationship between untreated initial psychosis duration (measured from onset of first symptom as well as from onset of full positive syndrome) and quality of life, symptom severity, and time to remission of positive symptoms. RESULTS: Earlier age at illness onset was associated with longer duration of untreated prodromal psychotic symptoms. There were no significant gender differences in duration of untreated initial psychosis, nor were there any significant associations between untreated initial psychosis duration and premorbid functioning. After controlling for the effects of age at onset, the duration of untreated initial psychosis did not significantly impair subsequent quality of life, symptom severity, or remission of positive symptoms. CONCLUSIONS: Duration of untreated initial psychosis was not prognostic of poor outcome early in the course of schizophrenia. Biological measures of neurotoxicity are needed to examine the “toxic psychosis” hypothesis more directly.
Predicting outcome for patients with first-episode schizophrenia is a crucial clinical issue. Both patients and families would like to know “what the future holds.” A large number of studies have examined the prognostic value of premorbid, sociodemographic, and psychopathological factors on outcome in schizophrenia (1–19). Male gender, poor premorbid functioning, early age at onset, insidious onset, absence of precipitating factors, and negative symptoms all portend poor outcome in patients with schizophrenia.
More recently, several groups of investigators have proposed that a long duration of untreated initial psychosis may also adversely affect long-term outcome in schizophrenia. Wyatt was among the first to suggest that psychosis may be “biologically toxic” and that long-term morbidity in some patients with schizophrenia may be prevented if patients are treated early with neuroleptics (20–24). Some investigators have found an association between longer duration of untreated initial psychosis and poor outcome in schizophrenia and have explained such an association with the “toxic psychosis” hypothesis (10, 25–29). These investigators have also used findings from other previously published studies as evidence in support of the notion that untreated psychosis may be injurious (24, 30–40).
The indirect evidence from these studies has also spurred debate among researchers and ethicists about research procedures that induce a psychotic state (e.g., challenge studies) (41–43). If untreated psychosis leads to poor long-term outcome and is therefore potentially injurious, it will lead to arguing not only for early intervention but also against inducing psychosis.
However, the majority of these studies have been retrospective. Retrospective studies and reviews (24–27, 34, 37, 38) that have suggested an association between longer duration of untreated initial psychosis and poor outcome in schizophrenia have had significant methodological limitations, including unevenly characterized samples and not accounting for the effects of factors known to be prognostic of schizophrenia (44). On the other hand, the number of prospective studies has been small. The outcome measures used in the prospective studies (10, 36, 39, 40) have been based on symptoms, i.e., time to remission, level of remission, and relapse. Since the predictor measure (duration of untreated initial psychosis) and outcome measures (time to remission, level of remission, and relapse) are both symptom related, the chances of finding an association will be expectedly high. While symptom remission and relapse rates are important measures of outcome in schizophrenia, to solely use these measures in studies investigating the effects of untreated initial psychosis duration confounds the results and limits outcome measurement to a single dimension of the illness.
Outcome in schizophrenia is a complex phenomenon (45). Over the years, investigators have become increasingly sophisticated in the assessment of outcome—from categorizing outcome into “improved” versus “not improved” or “good” versus “poor” to the use of multiple domains of outcome (such as rehospitalization rates, symptom relapse/remission, quality of life measures, and cognitive functioning). During the past 20 years, the concept of quality of life (including psychosocial functioning) has become an important outcome measure not only in clinical studies but also in patient care and health economic analyses (46–48). Although there is still no clear consensus about what constitutes quality of life or how to best measure it, investigators often use information from multiple sources (including the patient’s perceptions, reports from reliable informants, and the clinician’s own assessment) to gauge both the subjective and objective aspects of quality of life (49, 50).
The aim of this study was to investigate the effects of untreated initial psychosis on outcome in schizophrenia. The potential confounding effects from other known prognosticators of schizophrenia and their interactions with untreated initial psychosis duration are explored. This permits better estimation of the unique contribution of untreated initial psychosis duration to outcome in schizophrenia. The outcome measures in this study will include both symptom severity and symptom remission as well as quality of life, assessed by examining both subjective and objective indicators.
Method
Subjects
The subjects were drawn from the ongoing Iowa Prospective Longitudinal Study of Recent-Onset Psychoses (51). After complete description of the study to the subjects, written informed consent was obtained. The study design and method have been previously described. In brief, the study consists of subjects with schizophrenia or schizophrenia spectrum disorders who have had their first hospitalization during the previous 5 years. Approximately half of these are first-episode, neuroleptic-naive subjects. At the time of intake into the study, the subjects undergo an extensive evaluation, which includes phenomenological assessment (symptoms, family history, and obstetric complications), neurological examination, a neuropsychological battery, and a magnetic resonance imaging scan of the brain.
Two structured interview instruments, the Comprehensive Assessment of Symptoms and History (52) and the Psychiatric Status You Currently Have—Baseline Version (53), were used as part of the phenomenological assessment. The Scale for the Assessment of Negative Symptoms (SANS) (54) and the Scale for the Assessment of Positive Symptoms (SAPS) (55) form part of the two structured interview instruments. The Psychiatric Status You Currently Have interview has items that assess both subjective as well as objective measures of quality of life. Information from all available sources, including the subject, family members, and previous medical records, were incorporated to arrive at a consensus rating for each item in these structured instruments.
This report focuses on 74 first-episode, neuroleptic-naive subjects with DSM-IV schizophrenia (46 men and 28 women) who had been followed for at least 6 months. The mean age at intake into the study was 24.7 years (SD=5.8).
Ascertainment of Untreated Initial Psychosis Duration
Duration of untreated initial psychosis was defined in two ways: 1) the time period from the onset of the first symptom to the initiation of neuroleptic treatment and 2) the time period from the onset of a full positive syndrome to the initiation of neuroleptic treatment. The “first symptom” could include both positive symptoms (delusions, hallucinations, bizarre [disorganized] behaviors, formal thought disorder, and catatonic motor behavior) as well as prodromal symptoms that were mild variants of either positive or negative symptoms (e.g., social isolation, impairment in role functioning, peculiar behavior, impaired hygiene and grooming, blunted affect, digressive or vague speech, odd or magical thinking, and unusual perceptual experiences such as illusions). On the other hand, “full syndrome” refers to the presence of any one of the five positive symptoms at a severity level of moderate or worse.
Age at Onset and Premorbid Functioning
Ascertaining the age at onset in schizophrenia can be difficult, particularly for cases where onset is insidious or when the first indications of illness are nonspecific (e.g., drop in grades, loss of job). Therefore, in the Comprehensive Assessment of Symptoms and History, age at onset refers to the age at which the subject “first had problems.”
Premorbid functioning was assessed using the Modified Premorbid Adjustment Scale (56). This scale yields two measures of premorbid functioning according to age group: childhood (ages 6–12, score range=0–10) and adolescence and young adulthood (ages 13–21, score range=0–13). The total Premorbid Adjustment Scale score is obtained by summing up the two subscores. Higher scores indicate poorer premorbid functioning.
The measures of untreated initial psychosis duration, age at onset, and Premorbid Adjustment Scale subscores had interrater and test-retest reliabilities (intraclass r values) that exceeded 0.87 and 0.55, respectively (52, 56).
Assessment at 6-Month Follow-Up
As part of the longitudinal study, each subject was reevaluated 6 months later by the rater who had made the intake assessment. Follow-up versions of the Comprehensive Assessment of Symptoms and History and the Psychiatric Status You Currently Have were administered at follow-up to document the subjects’ quality of life and severity of symptoms during the previous 6 months.
Several quality of life domains, determined through both subjective and objective indicators, were assessed at the 6-month follow-up: degree of impairment in interpersonal relationships with family members, degree of impairment in interpersonal relationships with friends, degree of impairment in enjoyment of recreational activities, overall satisfaction, occupational functioning (percent of time during the preceding 6 months the individual was employed and degree of occupational impairment during the month preceding the follow-up evaluation), income source (percent of time during the preceding 6 months the subject was financially dependent on social service agencies), performance of household duties (percent of time during the preceding 6 months the subject was unable to perform household duties and the degree of impairment during the month preceding the follow-up evaluation), overall level of psychosocial adjustment, and the Global Assessment Scale (GAS) score (57). For items in which degree of impairment was assessed, ratings were made on a 5-point scale, with 5 representing the most impairment.
The severity of symptoms during the week before the 6-month follow-up evaluation were assessed by using the SANS and SAPS. Three dimensions were used to summarize symptom severity, based on previous factor analytic studies (58–61). The negative symptom dimension was defined as the sum of the global ratings of alogia, anhedonia, avolition, and affective flattening (range=0–20). The psychotic symptom dimension was defined as the sum of the global ratings of delusions and hallucinations (range=0–10). The disorganized symptom dimension was the sum of the global ratings of bizarre (disorganized) behavior, positive thought disorder, and inappropriate affect (range=0–15). Higher scores represent greater symptom severity.
Positive symptom remission was defined as a rating of 2 or lower (not worse than mild severity) on all global scores within the psychotic and disorganized symptom dimensions persisting for at least 8 consecutive weeks. Positive symptom remission was dated from the time remission criteria were first met.
Statistical Analyses
As the two measures of untreated initial psychosis duration were not normally distributed, nonparametric statistical tests were used. Spearman’s correlation analyses were used to examine the relationships between the measures of untreated initial psychosis duration and age at onset, premorbid functioning, quality of life, and symptom severity at 6 months after the first hospitalization. Because multiple comparisons were made on outcome measures at 6 months, a Bonferroni correction (critical p=0.004) was applied to reduce the risk of type I error in the correlational and the extreme groups analyses. The Cox proportional hazards model (log rank test) was used to examine the relationship between untreated initial psychosis duration and remission of positive symptoms. All tests of significance were two-tailed.
Results
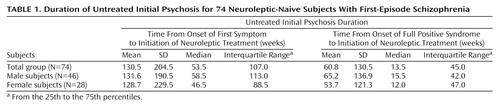
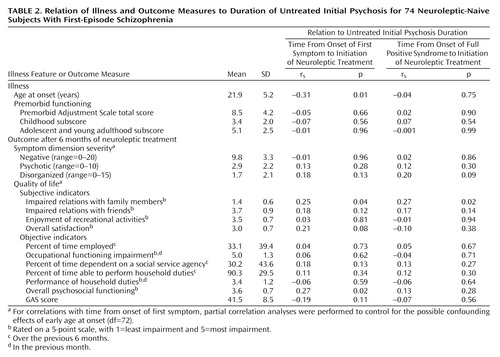
The duration of untreated initial psychosis for the 74 subjects, as well as a breakdown by gender, are summarized in Table 1. Although male subjects sought treatment later than female subjects, the gender differences in untreated initial psychosis duration were not statistically significant for the time period from onset of either the first symptom or the full psychotic syndrome to the initiation of neuroleptic treatment (Wilcoxon rank sum z=–0.36 and –0.54, respectively, p>0.59 for both). An earlier age at onset was moderately correlated with longer time since onset of first symptom (Table 2). Otherwise, no statistically significant associations were found between duration of untreated initial psychosis and age at onset or premorbid functioning.
All but one subject began neuroleptic treatment during the first psychiatric hospitalization. Since this is a naturalistic study, medication treatment was not controlled. The subjects received neuroleptics for the greater part of the 6 months after index assessment (mean duration of neuroleptic treatment=22.4 weeks, SD=6.6). At the 6-month follow-up, 15 subjects (20.3%) were not receiving neuroleptics, while 42 (56.8%) were taking typical neuroleptics (mean dose=502.5 mg/day of chlorpromazine equivalents, SD=476.8), and 17 (23.0%) were taking atypical neuroleptics (either risperidone [N=10; mean dose=4.8 mg/day, SD=2.0] or olanzapine [N=6; mean dose=8.8 mg/day, SD=3.8]; one patient was receiving clozapine, 300 mg/day). Multivariate correlation between duration of neuroleptic treatment and the 11 quality of life measures was examined after rank transformation of these variables. The overall R2 of 0.24 did not reach statistical significance (F=1.78, df=11, 62, p<0.08).
Quality of Life
In general, the quality of life was poor during the 6 months after discharge (Table 2). The quality of relationship with family members was between very good and good, but the quality of relationships with friends, level of involvement and enjoyment in recreational activities, and overall satisfaction in life were all between fair and poor. The subjects had severe impairment in occupational functioning and were employed for only about one-third of the 6-month period. While the mean ratings suggested mild to moderate impairment, the subjects were able to engage in performing household duties for most of the 6 months. By the 6-month follow-up evaluation, 56.7% (N=42) of the subjects were financially dependent on social service agencies and had been receiving payments from social service agencies for nearly one-third of the 6-month period. The subjects’ overall psychosocial functioning was moderately to markedly impaired. The mean GAS score approached a level signifying major impairment.
Since there was a significant inverse relationship between age at onset and time since onset of first symptom, the possible confounding effects from early age at onset were statistically controlled by using a partial correlation analysis. In general, the correlations between the two measures of untreated initial psychosis and quality of life 6 months after the first hospitalization were weak at best (Table 2). None of these outcome measures reached the critical p value of 0.004.
Symptom Severity and Remission of Positive Symptoms
At the 6-month follow-up evaluation, the disorganized and psychotic symptoms were of mild severity, and the negative symptoms were of moderate severity (Table 2). The correlations between duration of untreated initial psychosis and symptom severity were again weak.
The median time to remission of positive symptoms was 9 weeks after discharge from inpatient hospitalization. Only 58.1% (N=43) of the patients met criteria for positive symptom remission at 6 months (Figure 1). Neither measure of untreated initial psychosis duration approached significance based on the survival analysis (log rank test c2<0.07, df=1, p values >0.80), indicating no evidence for an effect of untreated initial psychosis duration on positive symptom remission.
We did an extreme groups analysis that compared subjects in the first quartile (median time from onset of full psychotic syndrome to treatment: 3 weeks) with those in the fourth quartile (median time from onset of full psychotic syndrome to treatment: 108 weeks) to further explore the effects of an extremely long duration of untreated initial psychosis. The pattern of results was similar to the correlation analyses. The quality of life and symptom severity of subjects whose durations of untreated initial psychosis were in the fourth quartile were not significantly worse than those of the first quartile (t values <2.5, df=36, p values >0.02). A stepwise discriminant analysis was also performed to find out which factors (quality of life and symptom severity measures at 6 months) best separated the groups with short and long durations of untreated initial psychosis. The only factor that discriminated the two groups was quality of family relationships (F=5.59, df=1, 35, p<0.02), which correctly identified 68.4% (N=13) of the subjects in the first quartile group and 63.2% (N=12) of the fourth quartile group.
Discussion
In this study of first-episode neuroleptic-naive subjects, we were interested in knowing what effects untreated initial psychosis has on outcome in schizophrenia. We first examined whether duration of untreated initial psychosis was related to known predictors of outcome (i.e., gender, age at onset of illness, and premorbid functioning) so as to better estimate the unique prognostic value of untreated initial psychosis. Only age at onset of illness was associated with untreated prodromal psychotic symptoms. There were no significant gender differences nor were there any significant associations between untreated initial psychosis duration and premorbid functioning. After partialing out the effects of age at onset, untreated initial psychosis duration did not significantly impair quality of life, symptom severity, or remission of positive symptoms 6 months after the first psychiatric hospitalization for treatment of schizophrenia.
While symptom severity and symptom remission are important measures of outcome, researchers have increasingly focused their attention on quality of life to arrive at a more comprehensive measure of outcome in schizophrenia. Assessing the quality of life allows one to understand the impact of schizophrenia on the patient’s general well-being, role functioning, and community integration. In our study, longer duration of untreated initial psychosis was not significantly associated with poorer quality of life. The median Spearman’s correlation coefficient between untreated initial psychosis duration and the different subjective and objective indicators of quality of life was only 0.115.
Unlike previous studies (10, 36), we did not find longer duration of untreated initial psychosis to predict poorer positive symptom remission. This may be related to the frequency of assessment. Although we used all available information to arrive at the best estimate of symptom severity for each week during the past 6 months, the accuracy of such an estimate is less than when subjects were reevaluated more frequently (fortnightly to monthly in the study by Loebel et al. [10]). Nevertheless, when symptom ratings for the previous week were obtained at the 6-month follow-up evaluation, there were still no significant correlations between positive symptoms and duration of untreated initial psychosis. Another possible reason for the lack of association between untreated initial psychosis duration and positive symptom remission may be related to the relatively short follow-up length. Hence, future studies will need to assess outcome after longer follow-up periods.
Duration of untreated initial psychosis is difficult to ascertain since the onset of psychosis is often subtle and insidious. Like previous studies (10, 36, 62), we have used similar dual definitions of untreated initial psychosis duration, i.e., dating from the onset of first nonspecific psychiatric symptoms as well as from the onset of more specific psychotic symptoms. Although such definitions allow for comparison across studies, the latter definition (time since onset of full psychotic syndrome) may be more relevant in studies examining the effects of untreated psychosis. Nevertheless, the lengthiness and wide variance for both measures of untreated initial psychosis duration in our study are comparable with those found in previous first-episode studies (10, 36, 62). Half of our patient group had experienced prodromal symptoms for greater than a year or had had severe psychotic symptoms for more than 3 months before they sought treatment. Many factors are likely to affect how soon after the onset of symptoms that patients with schizophrenia seek treatment. A wide array of sociocultural factors (such as educational level of patient and family members, socioeconomic status, availability and access to health care, beliefs and knowledge about mental illness, integrity of social support network) and psychopathological factors (e.g., insidious mode at onset, bizarre and disruptive behaviors, level of insight into illness and the need for treatment) may interact together to influence treatment-seeking behaviors (63–68). The net result of the interplay of these factors within the patient, and between the patient and his or her environment (family members and sometimes with the legal system as well), could either shorten or lengthen the duration of untreated initial psychosis.
Some investigators have proposed that there may be a threshold duration of untreated initial psychosis above which subsequent functioning may be impaired. However, such a relationship remains unclear, since these studies have significant methodological limitations. Browne and colleagues (28) reported on a cohort of 53 patients with schizophrenia or schizophreniform disorder for which the median duration of untreated initial psychosis was 6 months. However, 43.3% of the subjects had durations greater than 12 months, and when the investigators compared these patients with the rest of the cohort, they found that the former group had significantly poorer quality of life at the time of presentation for treatment. However, whether poor quality of life persists on subsequent follow-up remains to be seen. In another study, McGorry et al. (29) reported that patients with untreated initial psychosis durations greater than 28 days had poorer outcome at 12-month follow-up (i.e., slower remission of psychotic symptoms, greater symptom severity, and poorer quality of life) than those whose durations were less than 28 days. But only 40.5% of their patients met DSM-III-R criteria for schizophrenia or schizoaffective disorder, and 24% met criteria for schizophreniform disorder. A substantial proportion of the group (21.5%) consisted of patients with affective psychosis. More importantly, there were highly significant differences in untreated initial psychosis duration between diagnostic categories: the median duration of untreated psychosis in the schizophrenia-only group was 122.0 days, whereas the schizophreniform group and the remaining subjects had median durations of 10.5 and 14.0 days, respectively. McGorry et al.’s finding of poorer outcome among patients with longer durations of untreated initial psychosis may have been confounded by diagnosis. Patients with affective psychosis had shorter untreated initial psychosis durations, and, in general, they have better outcomes than do patients with schizophrenia.
In our extreme groups analysis, the minimum and median times from the onset of full psychotic syndrome to treatment for the group of patients in the fourth quartile were 50 weeks and more than 2 years, respectively. Yet, their quality of life, symptom severity, or rate of positive symptom remission were not significantly worse than those of patients in the first quartile (whose median and maximum times from onset of full psychotic syndrome to treatment were 3 weeks and 5 weeks, respectively). Thus, our data suggest that if there is a threshold duration of untreated initial psychosis above which subsequent outcome may be impaired, this threshold is greater than 50 weeks and may very likely be much longer than that.
Waddington et al. (25) and Scully et al. (26) have found longer duration of untreated initial psychosis to be associated with severe negative symptoms and cognitive dysfunction in a cohort of chronic schizophrenia patients with extremely long durations of untreated psychosis (means of 13.9 and 17.1 years). Because these patients became ill during the preneuroleptic era, psychosis had been left untreated for long periods of time—much longer than those of modern-day patients with schizophrenia. Under current psychiatric practice, such extremely long durations are seen only in a minority of patients and therefore may not be clinically relevant for the average patient with schizophrenia today.
Overall, the findings from this study bode well for patients. Despite the fact that many patients experienced long periods of untreated initial psychosis, this delay in seeking treatment does not appear to significantly impair subsequent outcome for the average patient with schizophrenia. These results also have implications for the debate about placebo controls in clinical drug trials, the use of “drug holidays,” and the advantages or disadvantages of medication discontinuation or withdrawal (24, 41–43). It appears unlikely that the brief periods of psychosis (lasting several hours to several weeks) that may occur during challenge studies or medication discontinuation will have adverse effects on subsequent symptom severity, psychosocial functioning, or quality of life.
Of course, our findings do not argue against preventive measures for schizophrenia. In fact, future studies should aim toward better understanding of why most patients wait so long before seeking treatment. Interventions to increase the public’s awareness and understanding of this devastating illness and its treatment may help bring patients to seek treatment sooner, and thereby reduce their suffering during the initial psychosis. Such long durations of untreated psychosis are clearly undesirable, since the psychotic experience is usually unpleasant, bewildering, and even painful to the patient and his or her family.
The hypothesis that untreated psychosis may be “biologically toxic” remains unsubstantiated. Clinical outcome studies alone, even those with the most robust methodology, can only provide indirect evidence to support or refute such a hypothesis. To effectively test the “toxic psychosis” hypothesis, biological measures of “toxicity” are likely to be more sensitive than the duration of psychosis. Such biological measures, which may include neuroimaging, neurochemistry, and neuropathology, are needed to provide more direct evidence as to whether untreated psychosis represents an “active morbid process” that is deleterious to outcome in people with schizophrenia.
 |
 |
Presented in part at the International Congress on Schizophrenia Research, Santa Fe, April 17–21, 1999. Received Jan. 13, 1999; revisions received Sept. 17 and Nov. 22, 1999; accepted Dec. 27, 1999. From the Mental Health Clinical Research Center, Department of Psychiatry, University of Iowa College of Medicine. Address reprint requests to Dr. Ho, Department of Psychiatry, 2939 JPP, University of Iowa College of Medicine, 200 Hawkins Dr., Iowa City, IA 52242; [email protected] (e-mail). Supported in part by NIMH grant MH-31593 and Clinical Research Center grant MH-43271; the Nellie Ball Trust Research Fund, Iowa State and Bank Trust Company, Trustee; and NIMH Research Scientist Award MH-00625. The authors thank Stephan Arndt, Ph.D., and Carrie Franciscus, B.S., for assistance in data analysis.
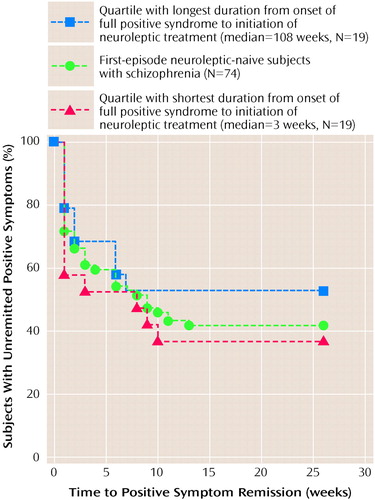
Figure 1. Positive Symptom Remission for Subjects With First-Episode Schizophrenia and for Quartiles With Shortest and Longest Untreated Initial Psychosis Durations
1. Strauss JS, Carpenter WT Jr: Prediction of outcome in schizophrenia, III: five-year outcome and its predictors. Arch Gen Psychiatry 1977; 34:159–163Crossref, Medline, Google Scholar
2. Johnstone EC, Frith CD, Gold A, Stevens M: The outcome of severe acute schizophrenic illnesses after one year. Br J Psychiatry 1979; 134:28–33Crossref, Medline, Google Scholar
3. Moller HJ, von Zerssen D, Werner-Eilert K, Wuschner-Stockheim M: Outcome in schizophrenic and similar paranoid psychoses. Schizophr Bull 1982; 8:99–108Crossref, Medline, Google Scholar
4. McGlashan TH: Predictors of shorter-, medium-, and longer-term outcome in schizophrenia. Am J Psychiatry 1986; 143:50–55Link, Google Scholar
5. Kay SR, Lindenmayer JP: Outcome predictors in acute schizophrenia: prospective significance of background and clinical dimensions. J Nerv Ment Dis 1987; 175:152–160Crossref, Medline, Google Scholar
6. Prudo R, Blum HM: Five-year outcome and prognosis in schizophrenia: a report from the London Field Research Centre of the International Pilot Study of Schizophrenia. Br J Psychiatry 1987; 150:345–354Crossref, Medline, Google Scholar
7. Goldstein JM: Gender differences in the course of schizophrenia. Am J Psychiatry 1988; 145:684–689Link, Google Scholar
8. Westermeyer JF, Harrow M: Course and outcome in schizophrenia, in Handbook of Schizophrenia: Nosology, Epidemiology and Genetics. Edited by Tsuang MT, Simpson JC. Amsterdam, Elsevier, 1988, pp 205–244Google Scholar
9. Breier A, Schreiber JL, Dyer J, Pickar D: National Institute of Mental Health longitudinal study of chronic schizophrenia: prognosis and predictors of outcome. Arch Gen Psychiatry 1991; 48:239–246Crossref, Medline, Google Scholar
10. Loebel AD, Lieberman JA, Alvir JMJ, Mayerhoff DI, Geisler SH, Szymanski SR: Duration of psychosis and outcome in first-episode schizophrenia. Am J Psychiatry 1992; 149:1183–1188Google Scholar
11. Ram R, Bromet EJ, Eaton WW, Pato C, Schwartz JE: The natural course of schizophrenia: a review of first-admission studies. Schizophr Bull 1992; 18:185–207Crossref, Medline, Google Scholar
12. Addington J, Addington D: Premorbid functioning, cognitive functioning, symptoms and outcome in schizophrenia. J Psychiatry Neurosci 1993; 18:18–23Medline, Google Scholar
13. Hwu HG, Tan H, Chen CC, Yeh LL: Negative symptoms at discharge and outcome in schizophrenia. Br J Psychiatry 1995; 166:61–67Crossref, Medline, Google Scholar
14. Szymanski S, Lieberman JA, Alvir JM, Mayerhoff D, Loebel A, Geisler S, Chakos M, Koreen A, Jody D, Kane J, Woerner M, Cooper T: Gender differences in onset of illness, treatment response, course, and biologic indexes in first-episode schizophrenic patients. Am J Psychiatry 1995; 152:698–703Link, Google Scholar
15. Bromet EJ, Jandorf L, Fennig S, Lavelle J, Kovasznay B, Ram R, Tanenberg-Karant M, Craig T: The Suffolk County Mental Health Project: demographic, pre-morbid and clinical correlates of 6-month outcome. Psychol Med 1996; 26:953–962Crossref, Medline, Google Scholar
16. Bailer J, Brauer W, Rey ER: Premorbid adjustment as predictor of outcome in schizophrenia: results of a prospective study. Acta Psychiatr Scand 1996; 93:368–377Crossref, Medline, Google Scholar
17. Thara R, Eaton WW: Outcome of schizophrenia: the Madras longitudinal study. Aust NZ J Psychiatry 1996; 30:516–522Crossref, Medline, Google Scholar
18. Wieselgren IM, Lindstrom E, Lindstrom LH: Symptoms at index admission as predictor for 1–5 year outcome in schizophrenia. Acta Psychiatr Scand 1996; 94:311–319Crossref, Medline, Google Scholar
19. Ho BC, Nopoulos P, Flaum M, Arndt S, Andreasen NC: Two-year outcome in first-episode schizophrenia: predictive value of symptoms for quality of life. Am J Psychiatry 1998; 155:1196–1201Google Scholar
20. Wyatt RJ: The dopamine hypothesis: variations on a theme, in Research in the Schizophrenic Disorders. Edited by Cancro R, Dean SR. Jamaica, NY, Spectrum Publications, 1985, pp 225–247Google Scholar
21. Wyatt RJ: Neuroleptics and the natural course of schizophrenia. Schizophr Bull 1991; 17:325–351Crossref, Medline, Google Scholar
22. Wyatt RJ: Antipsychotic medication and the long-term course of schizophrenia, in Contemporary Issues in the Treatment of Schizophrenia. Edited by Shriqui CL, Nasrallah HA. Washington, DC, American Psychiatric Press, 1995, pp 385–410Google Scholar
23. Wyatt RJ: Early intervention for schizophrenia: can the course of the illness be altered? Biol Psychiatry 1995; 38:1–3Google Scholar
24. Wyatt RJ, Green MF, Tuma AH: Long-term morbidity associated with delayed treatment of first admission schizophrenic patients: a re-analysis of the Camarillo State Hospital data. Psychol Med 1997; 27:261–268Crossref, Medline, Google Scholar
25. Waddington JL, Youssef HA, Kinsella A: Sequential cross-sectional and 10-year prospective study of severe negative symptoms in relation to duration of initially untreated psychosis in chronic schizophrenia. Psychol Med 1995; 25:849–857Crossref, Medline, Google Scholar
26. Scully PJ, Coakley G, Kinsella A, Waddington JL: Psychopathology, executive (frontal) and general cognitive impairment in relation to duration of initially untreated versus subsequently treated psychosis in chronic schizophrenia. Psychol Med 1997; 27:1303–1310Google Scholar
27. Waddington JL, Scully PJ, Meagher D, Quinn J, Murphy P, Kinsella A, Mullaney J: Duration of initially untreated psychosis: cognition and domains of psychopathology in the long-term (abstract). Int J Neuropsychopharmacol 1998; 1:S31Google Scholar
28. Browne S, Clarke M, Gervin M, Waddington JL, Larkin C, O’Callaghan E: Duration of initially untreated psychosis: impact on quality of life at first presentation with schizophrenia (abstract). Int J Neuropsychopharmacol 1998; 1:S32Google Scholar
29. McGorry PD, Edwards J, Mihalopoulos C, Harrigan SM, Jackson HJ: EPPIC: an evolving system of early detection and optimal management. Schizophr Bull 1996; 22:305–326Crossref, Medline, Google Scholar
30. May PR, Tuma AH: Treatment of schizophrenia: an experimental study of five treatment methods. Br J Psychiatry 1965; 111:503–510Crossref, Google Scholar
31. May PR, Tuma AH, Dixon WJ: Schizophrenia—a follow-up study of results of treatment, I: design and other problems. Arch Gen Psychiatry 1976; 33:474–478Crossref, Medline, Google Scholar
32. May PR, Tuma AH, Yale C, Potepan P, Dixon WJ: Schizophrenia—a follow-up study of results of treatment. Arch Gen Psychiatry 1976; 33:481–486Crossref, Medline, Google Scholar
33. May PR, Tuma AH, Dixon WJ, Yale C, Thiele DA, Kraude WH: Schizophrenia: a follow-up study of the results of five forms of treatment. Arch Gen Psychiatry 1981; 38:776–784Crossref, Medline, Google Scholar
34. Lo WH, Lo T: A ten-year follow-up study of Chinese schizophrenics in Hong Kong. Br J Psychiatry 1977; 131:63–66Crossref, Medline, Google Scholar
35. Crow TJ, MacMillan JF, Johnson AL, Johnstone EC: A randomised controlled trial of prophylactic neuroleptic treatment. Br J Psychiatry 1986; 148:120–127Crossref, Medline, Google Scholar
36. Rabiner CJ, Wegner JT, Kane JM: Outcome study of first-episode psychosis, I: relapse rates after one year. Am J Psychiatry 1986; 143:1155–1158Google Scholar
37. Inoue K, Nakajima T, Kato N: A longitudinal study of schizophrenia in adolescence, I: the one- to three-year outcome. Jpn J Psychiatry Neurol 1986; 40:143–151Medline, Google Scholar
38. Fenton WS, McGlashan TH: Sustained remission in drug-free schizophrenic patients. Am J Psychiatry 1987; 144:1306–1309Google Scholar
39. McEvoy JP, Schooler NR, Wilson WH: Predictors of therapeutic response to haloperidol in acute schizophrenia. Psychopharmacol Bull 1991; 27:97–101Medline, Google Scholar
40. Szymanski SR, Cannon TD, Gallacher F, Erwin RJ, Gur RE: Course of treatment response in first-episode and chronic schizophrenia. Am J Psychiatry 1996; 153:519–525Link, Google Scholar
41. Carpenter WT Jr: The risk of medication-free research. Schizophr Bull 1997; 23:11–18Crossref, Medline, Google Scholar
42. Waddington JL, Scully PJ: Untreated psychosis and long-term outcome in schizophrenia (letter). Schizophr Bull 1998; 24:34–35Crossref, Medline, Google Scholar
43. Carpenter WT Jr: Medication-free research and patient safety (letter). Schizophr Bull 1998; 24:35–36Crossref, Google Scholar
44. McGlashan TH, Johannessen JO: Early detection and intervention with schizophrenia: rationale. Schizophr Bull 1996; 22:201–222Crossref, Medline, Google Scholar
45. Strauss JS, Carpenter WT Jr: The prediction of outcome in schizophrenia, I: characteristics of outcome. Arch Gen Psychiatry 1972; 27:739–746Crossref, Medline, Google Scholar
46. Lehman AF, Ward NC, Linn LS: Chronic mental patients: the quality of life issue. Am J Psychiatry 1982; 139:1271–1276Google Scholar
47. Awad AG: Quality-of-life issues in medicated schizophrenic patients, in Contemporary Issues in the Treatment of Schizophrenia. Edited by Shriqui CL, Nasrallah HA. Washington, DC, American Psychiatric Press, 1995, pp 735–747Google Scholar
48. Awad AG: Quality of life rediscovered: implications for clinical outcome and health economics in schizophrenia. J Psychiatry Neurosci 1997; 22:229–230Medline, Google Scholar
49. Lehman AF, Postrado LT, Rachuba LT: Convergent validation of quality of life assessments for persons with severe mental illnesses. Qual Life Res 1993; 2:327–333Crossref, Medline, Google Scholar
50. Sainfort F, Becker M, Diamond R: Judgments of quality of life of individuals with severe mental disorders: patient self-report versus provider perspectives. Am J Psychiatry 1996; 153:497–502Link, Google Scholar
51. Flaum MA, Andreasen NC, Arndt S: The Iowa Prospective Longitudinal Study of Recent-Onset Psychoses. Schizophr Bull 1992; 18:481–490Crossref, Medline, Google Scholar
52. Andreasen NC, Flaum M, Arndt S: The Comprehensive Assessment of Symptoms and History (CASH): an instrument for assessing diagnosis and psychopathology. Arch Gen Psychiatry 1992; 49:615–623Crossref, Medline, Google Scholar
53. Andreasen NC: Psychiatric Status You Currently Have—Baseline Version (PSYCH-BASE). Iowa City, Iowa, University of Iowa, 1989Google Scholar
54. Andreasen NC: Scale for the Assessment of Negative Symptoms (SANS). Iowa City, University of Iowa, 1983Google Scholar
55. Andreasen NC: Scale for the Assessment of Positive Symptoms (SAPS). Iowa City, University of Iowa, 1984Google Scholar
56. Gupta S, Rajaprabhakaran R, Arndt S, Flaum M, Andreasen NC: Premorbid adjustment as a predictor of phenomenological and neurobiological indices in schizophrenia. Schizophr Res 1995; 16:189–197Crossref, Medline, Google Scholar
57. Endicott J, Spitzer RL, Fleiss JL, Cohen J: The Global Assessment Scale: a procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry 1976; 33:766–771Crossref, Medline, Google Scholar
58. Bilder RM, Mukherjee S, Rieder RO, Pandurangi AK: Symptomatic and neuropsychological components of defect states. Schizophr Bull 1985; 11:409–419Crossref, Medline, Google Scholar
59. Liddle PF: The symptoms of chronic schizophrenia: a re-examination of the positive-negative dichotomy. Br J Psychiatry 1987; 151:145–151Crossref, Medline, Google Scholar
60. Arndt S, Alliger RJ, Andreasen NC: The distinction of positive and negative symptoms: the failure of a two-dimensional model. Br J Psychiatry 1991; 158:317–322Crossref, Medline, Google Scholar
61. Miller DD, Arndt S, Andreasen NC: Alogia, attentional impairment, and inappropriate affect: their status in the dimensions of schizophrenia. Compr Psychiatry 1993; 34:221–226Crossref, Medline, Google Scholar
62. Hafner H, Maurer K, Loffler W, Riecher-Rossler A: The influence of age and sex on the onset and early course of schizophrenia. Br J Psychiatry 1993; 162:80–86Crossref, Medline, Google Scholar
63. Angermeyer MC, Klusmann D: The causes of functional psychoses as seen by patients and their relatives, I: the patients’ point of view. Eur Arch Psychiatry Neurol Sci 1988; 238:47–54Crossref, Medline, Google Scholar
64. Angermeyer MC, Klusmann D, Walpuski O: The causes of functional psychoses as seen by patients and their relatives, II: the relatives’ point of view. Eur Arch Psychiatry Neurol Sci 1988; 238:55–61Crossref, Medline, Google Scholar
65. Angermeyer MC, Matschinger H: Relatives’ beliefs about the causes of schizophrenia. Acta Psychiatr Scand 1996; 93:199–204Crossref, Medline, Google Scholar
66. Jorm AF, Korten AE, Jacomb PA, Christensen H, Rodgers B, Pollitt P: “Mental health literacy”: a survey of the public’s ability to recognise mental disorders and their beliefs about the effectiveness of treatment. Med J Aust 1997; 166:182–186Crossref, Medline, Google Scholar
67. Jorm AF, Korten AE, Jacomb PA, Christensen H, Rodgers B, Pollitt P: Public beliefs about causes and risk factors for depression and schizophrenia. Soc Psychiatry Psychiatr Epidemiol 1997; 32:143–148Medline, Google Scholar
68. Rabinowitz J, Bromet EJ, Lavelle J, Severance KJ, Zariello SL, Rosen B: Relationship between type of insurance and care during the early course of psychosis. Am J Psychiatry 1998; 155:1392–1397Google Scholar



