Clinical and Theoretical Implications of 5-HT2 and D2 Receptor Occupancy of Clozapine, Risperidone, and Olanzapine in Schizophrenia
Abstract
OBJECTIVE: Dopamine D2 receptor occupancy measurements provide a valid predictor of antipsychotic response, extrapyramidal side effects, and elevation of prolactin levels. The new antipsychotics clozapine, risperidone, and olanzapine obtain antipsychotic response with few extrapyramidal side effects and little prolactin elevation. The purpose of this study was to compare the D2 and serotonin 5-HT2 receptor occupancies of these drugs in patients receiving multiple-dose, steady-state regimens. METHOD: Forty-four patients with schizophrenia (16 taking risperidone, 2–12 mg/day; 17 taking olanzapine, 5–60 mg/day; and 11 taking clozapine, 75–900 mg/day) had their D2 and 5-HT2 occupancies determined with the use of [11C]raclopride and [18F]setoperone, respectively, and positron emission tomography imaging. RESULTS: Clozapine showed a much lower D2 occupancy (16%–68%) than risperidone (63%–89%) and olanzapine (43%–89%). Risperidone and olanzapine gave equal D2 occupancies at doses of 5 and 20 mg/day, respectively. All three drugs showed greater 5-HT2 than D2 occupancy at all doses, although the difference was greatest for clozapine. CONCLUSIONS: Clozapine, at doses known to be effective in routine clinical settings, showed a D2 occupancy clearly lower than that of typical antipsychotics, while risperidone and olanzapine at their usual clinical doses gave the same level of D2 occupancy as low-dose typical antipsychotics. The results also suggest that some previous clinical comparisons of antipsychotics may have been confounded by different levels of D2 occupancy. Clinical comparisons of these drugs, matching for D2 occupancy, may provide a better measure of their true “atypicality” and will help in understanding the contribution of non-D2 receptors to antipsychotic effects.
Every known antipsychotic blocks dopamine D2 receptors. While this does not prove a causal relationship between D2 blockade and antipsychotic response, the association between the two is undeniable. Thus, it is of obvious interest to compare the relative D2 receptor occupancies of the available antipsychotics. Farde and colleagues (1) proposed that one needs a “threshold” of D2 occupancy to induce antipsychotic response. Prospective studies have largely confirmed this notion, although it is unclear whether this threshold is 60% or 70% and whether the threshold for inducing response is the same as the one for maintaining it (2, 3). Nonetheless, there is a mechanism of antipsychotic response that relies on D2 occupancy alone (4). Furthermore, it has been noted that as D2 occupancy increases, especially as it rises above 80%, the incidence of extrapyramidal side effects increases (1). Elevation of prolactin levels may also show a threshold relationship with respect to D2 occupancy (5, 6, and unpublished data from our laboratory). While D2 occupancy may be necessary for response, it is not always sufficient, as there are patients who do not respond despite adequate D2 occupancy (7). However, it would be fair to claim that D2 occupancy provides a reliable (and perhaps the best) pharmacological predictor of response to antipsychotic medication, extrapyramidal side effects, and elevation of prolactin levels.
There are now several antipsychotics that have a lower propensity than typical antipsychotics to cause extrapyramidal side effects and prolactin elevation: clozapine, risperidone, olanzapine, sertindole, and quetiapine (8–12). The first three have been used most extensively in patients and are the focus of this study. Given the relevance of D2 occupancy for response to antipsychotics, extrapyramidal side effects, and prolactin elevation, it is of obvious interest how these antipsychotics compare on this index. The main purpose of this study was to compare the D2 occupancy of these three drugs in patients receiving multiple-dose, steady-state regimens of the drugs across their usual range of clinical use.
It has been suggested that drugs may demonstrate atypical clinical features (i.e., low extrapyramidal side effects and prolactin elevation) if they have at least a 10 times higher affinity for serotonin 5-HT2 receptors than D2 receptors in vitro (13, 14). In patients this translates into a preferential occupancy of 5-HT2 receptors as opposed to D2 receptors (15). Clozapine, risperidone, and olanzapine all show a higher affinity for 5-HT2 receptors than D2 receptors in vitro, but the amount by which 5-HT2 exceeds D2 is unclear. In animal tissue or cloned human receptors, clozapine shows a much higher 5-HT2/D2 ratio (20 times higher affinity for 5-HT2 than for D2) than either risperidone (11 times) or olanzapine (12 times) (16). On the other hand, occupancy measurements in rats following subcutaneous injection showed that risperidone had the highest 5-HT2/D2 affinity ratio (19 times) as compared with clozapine (5.1 times) and olanzapine (7.5 times) (16). Therefore, a second purpose of this study was to systematically compare the 5-HT2 occupancies and the 5-HT2/D2 occupancy ratios in patients.
Several previous reports have presented data on one or two of these antipsychotics separately. However, these studies used different imaging modalities (positron emission tomography [PET; 17–21] or single photon emission computed tomography [SPECT; 22, 23]); different radioligands ([11C]raclopride [17–20], [11C]- NMSP [21], or [123I]IBZM [22, 23]); and different image analysis models (cerebellum as reference [17–21] or frontal cortex as reference [22, 23]). As a result, it is not valid to compare the occupancy of, say, risperidone obtained with [123I]IBZM SPECT to that of clozapine derived by using [11C]NMSP PET. It is essential, when comparing drugs, that the data be obtained on all of the drugs in the same fashion. Furthermore, dose of a drug is a central determinant of its receptor occupancy, and some previous studies have compared occupancies without adequately controlling for dose (23). Any systematic comparison across drugs must compare not just the occupancy but also the dose-occupancy relationships over the clinically relevant dose range. To provide the first such comparison, we present data on the relation between dose, plasma level, and 5-HT2 and D2 occupancies in 44 patients with schizophrenia who were receiving a wide range of steady-state doses of clozapine, risperidone, and olanzapine.
METHOD
The procedures for this study were approved by the Human Subjects Review Committee of the University of Toronto. Patients participated after receiving detailed written information about the study and signing a consent document. Patients receiving ongoing treatment in our inpatient and outpatient clinic were recruited over a period of 4 years. We studied 44 patients (36 male and eight female) aged 19–54 years; 43 had a DSM-IV diagnosis of schizophrenia, and one had a diagnosis of atypical psychosis. Sixteen patients were receiving risperidone (2–12 mg/day), 17 were receiving olanzapine (5–60 mg/day), and 11 were receiving clozapine (75–900 mg/day). The patients were not randomly assigned to the three drugs, and the limitations of this are discussed later. Most of the patients were chosen from a clinic population so as to provide a representative range of doses for each drug, which is a sufficient study design for obtaining the in vivo 5-HT2/D2 profile of the three drugs in patients. However, because of inadequate prospective control over drug and dose assignment and the fact that patients were in various degrees of remission at the time of scanning, the design was limited in its ability to obtain reliable associations between receptor occupancy and clinical outcome. Nonetheless, to ensure a valid comparison of the action of the three drugs on the receptors, the patients in this report conformed to the following criteria.
1. All patients were on multiple-dose, steady-state levels (at least 5 days on the particular dose) of the medication for which they were assessed.
2. All patients were free of any confounding major medical or neurological illness. None of the patients had received any depot antipsychotics in the year before this PET examination, and none had received any other antipsychotics for a minimum of 14 days before the PET examination. None of the patients had concurrent substance abuse or substance dependence (nicotine excepted).
3. Patients were not receiving any other psychotropic medication that might confound the findings for D2 occupancy, with the exception of benzodiazepines and/or an antiparkinsonian agent, as indicated in table 1. It has been shown that the addition of lorazepam does not alter the measurement of D2 occupancy with [11C]raclopride (24).
4. All patients received a scan for dopamine D2 receptors, and most received a scan for serotonin 5-HT2 receptors. All patients had their [11C]raclopride PET examinations done 12–13 hours after their last nightly drug dose (the usual scan start was at 9:00 a.m.). The [18F]setoperone PET examination for 5-HT2 receptors, if done, followed the [11C]raclopride examination on the same day and started 14–15 hours after the last nightly drug dose.
PET data on some of the patients have appeared in previous reports (19, 20); these patients are identified in table 1. To carry out a systematic comparison, data on all of the subjects in the study were analyzed (those reported before were reanalyzed) with the methods described below, and all patient data were compared with the same baseline data to eliminate any across-drug bias. As a result, there may be a slight variation in the occupancy reported here and that reported before.
The PET scans to estimate D2 occupancy were obtained after the injection of 10 mCi of high specific activity [11C]raclopride (300–1600 Ci/mmol) according to a bolus-plus-infusion protocol. The scanning methods used have been described in a previous report in this journal (2). The pertinent aspects are the following. Striatal and cerebellar regions of interest were drawn on two contiguous PET slices on a composite PET image with reference to a coregistered magnetic resonance imaging (MRI) scan (GE Signa 1.5-T scanner; T2-weighted spin-echo sequence coregistered to the PET scan with a surface-matching algorithm). An estimate of the D2 binding potential (D2 BP) of raclopride (which represents the Bmax/Kd of [11C]- raclopride for D2 receptors, where Bmax is the total number of receptors available to a ligand, and Kd is the affinity of the ligand for the receptors) was obtained from the ratio of the striatum to the cerebellum during the 30- to 75- minute interval, a period of prolonged pseudo equilibrium afforded by the bolus-plus-infusion protocol. As used in our laboratory, this method yields a test-retest standard deviation of 6% and has been standardized to have an interrater and intrarater reliability, as measured by the intraclass correlation coefficient (ICC-III), of >0.95.
To estimate receptor occupancy, we used an age-corrected baseline value derived from a pool of 16 normal subjects and 12 antipsychotic-naive patients with schizophrenia. Since the illness had no statistically discernible effect on D2 receptors as measured with [11C]raclopride in this sample (F=0.66, df=1, 25, p=0.42) and in a previous report by others (25), data from the antipsychotic-naive patients and normal subjects were pooled to provide a more robust effect of age on D2 binding potential. Drug-induced D2 receptor occupancy was determined as (D2 BPBase–D2 BPDrug)/(D2 BPBase), where D2 BPBase is the age-corrected D2 baseline binding potential, and D2 BPDrug is the D2 binding potential for patients taking the antipsychotic drug. The absence of the patient’s own baseline values introduces a potential error; the error as calculated on the basis of variance in the data from antipsychotic-naive persons is expected to vary from 0% to 9% for patients with 50% occupancy and from 0% to 4% for patients with 80% occupancy (26).
The 5-HT2 scans were obtained with the use of a bolus injection of 5 mCi of high specific activity [18F]setoperone (360–6210 Ci/mmol), according to the method developed and standardized by Blin et al. (27, 28). The 5-HT2 occupancy was determined in the prefrontal cortex regions of interest drawn on the [18F]setoperone scan with reference to a coregistered MRI (as described above). An index of the 5-HT2 receptors was obtained from the prefrontal cortex/cerebellar ratio over the 65- to 90-minute time period. The cerebellum is practically devoid of 5-HT2 receptors (29), and studies in baboons as well as humans report no displaceable [18F]setoperone binding in this region (27, 28, 30). It can be shown that at a time when the binding of the radioligand is at pseudo equilibrium, the prefrontal/cerebellum ratio represents 5-HT2 BP + 1 (31). The details of this method as applied here have been described elsewhere (32). We have shown that this method yields an average test-retest deviation of 6%–7% and an acceptably high interrater reliability (ICC-III >0.95) (32).
Since these patients were already receiving treatment, it was not possible to measure their baseline 5-HT2 binding potential. In the absence of this baseline, we used the age-corrected 5-HT2 binding potential obtained from 11 antipsychotic-free patients with schizophrenia and 26 age-matched normal subjects. The pooling of normal subjects and patients results in a more robust age-corrected regression and is justified because there was neither a main effect of diagnosis (F=1.20, df=1, 33, p=0.28) nor a significant effect of diagnosis on the age regression (F=0.59, df=1, 33, p=0.45) (33). Occupancy was calculated in the same way as for dopamine D2 occupancy.
The patients had blood drawn at the time of the D2 PET scan; the samples were analyzed in batches by drug. Clozapine plasma levels were measured by means of high-performance liquid chromatography with electrochemical detection by a method based on previously published techniques (34). Risperidone plasma levels were measured by means of a radioimmunoassay for the active moiety, which reflects both risperidone and 9-OH risperidone, by the Janssen Research Foundation, Beerse, Belgium (35). Olanzapine plasma levels were measured by means of high-performance liquid chromatography with electrochemical detection by BAS Analytics (West Lafayette, Ind.).
Since the patients were, by design, taking the drugs at different dose and plasma levels, a direct comparison of the occupancies without reference to dose is not very informative. To provide a valid comparison, we characterized the dose-occupancy relationship for each drug and compared these profiles across the three drugs. The expected relationship between a drug level and occupancy of the receptors should conform to a rectangular hyperbola, assuming bimolecular (drug-receptor) interactions and negligible occupancy by the endogenous ligand. A rectangular hyperbola, in this context, is defined by  , where %Occ is the observed occupancy, Occmax is the theoretically maximum occupancy for that particular drug, DConc is the amount of the drug (expressed either as dose or plasma level), and ED50 is a constant equivalent to the amount of the drug required to occupy 50% of Occmax. If there is reason to believe that all of the [11C]raclopride can be displaced by the drug in question, Occmax can be replaced by 100 in equation 1. In its truest form, DConc should represent the concentration of the drug in the synapse. Since there is no easy way to measure the synaptic concentration of the drug in patients, one can use dose and plasma level as functional surrogates. However, it should be kept in mind that dose and plasma level only indirectly reflect synaptic concentrations. Noncompliance with the medication regimen or changes in metabolism may lead to different plasma levels for a given dose, and there may be significant differences in the levels of the freely available drug in the synapse if there is a change in protein binding. The observed receptor occupancy was related to the administered dose and measured plasma level with the use of equation 1 implemented in SPSS for Windows (SPSS Inc., Chicago).
, where %Occ is the observed occupancy, Occmax is the theoretically maximum occupancy for that particular drug, DConc is the amount of the drug (expressed either as dose or plasma level), and ED50 is a constant equivalent to the amount of the drug required to occupy 50% of Occmax. If there is reason to believe that all of the [11C]raclopride can be displaced by the drug in question, Occmax can be replaced by 100 in equation 1. In its truest form, DConc should represent the concentration of the drug in the synapse. Since there is no easy way to measure the synaptic concentration of the drug in patients, one can use dose and plasma level as functional surrogates. However, it should be kept in mind that dose and plasma level only indirectly reflect synaptic concentrations. Noncompliance with the medication regimen or changes in metabolism may lead to different plasma levels for a given dose, and there may be significant differences in the levels of the freely available drug in the synapse if there is a change in protein binding. The observed receptor occupancy was related to the administered dose and measured plasma level with the use of equation 1 implemented in SPSS for Windows (SPSS Inc., Chicago).
RESULTS
For all three drugs, increasing doses led to increasing plasma levels, consistent with expectations and affirming reasonable compliance (table 1). A simple comparison of the occupancies shows that clozapine had a significantly lower D2 occupancy than risperidone and olanzapine (main analysis of variance, F=13.05, df=2, 39, p<0.001; post hoc comparison with risperidone: p<0.001; with olanzapine: p<0.001), which were themselves indistinguishable (Tukey’s honestly significant difference post hoc test, risperidone versus olanzapine: p=0.80).
The D2 occupancies in response to increasing doses and plasma levels are presented in figure 1 and figure 2. In each case, a rectangular hyperbola provided a better fit (i.e., explained a greater degree of variance) than a simple linear fit. The parameters for the curves relating occupancy to dose were as follows: for risperidone, Occmax=91%, ED50=0.8 mg/day, with 77% variance explained; for olanzapine, Occmax=92%, ED50=3.2 mg/day, with 81% variance explained; for clozapine, Occmax=71%, ED50=112 mg/day, with 55% variance explained. The parameters for the curves relating occupancy to plasma level were as follows: for risperidone, Occmax=88%, ED50=3.2 ng/ml, with 59% variance explained; for olanzapine, Occmax=90%, ED50=6.4 ng/ml, with 84% variance explained; for clozapine, Occmax=68%, ED50=88 mg/day, with 18% variance explained. It is important to note that clozapine does not saturate the D2 receptors, and the theoretical maximum occupancy (Occmax) is 68%–71%. This is in contrast to risperidone and olanzapine, where we observed occupancies of up to 83% and where Occmax was 91% and 92%, respectively.
Curves relating dose and occupancy for risperidone and olanzapine had the same shape (a near-saturating rectangular hyperbola) and differed only in the dose axis. The amount of drug required to occupy 50% of the available D2 receptors is 3.2 mg/day for olanzapine and 0.8 mg/day for risperidone if the equation is fitted with two parameters (and 4.5 versus 1.2 mg/day if Occmax is assumed to be 100%). This suggests that D2-occupancy-equipotent doses of risperidone and olanzapine are in the ratio of 5:20 mg/day.
All three drugs showed a preferential occupancy of 5-HT2 receptors versus D2 receptors and the ability to completely occupy 5-HT2 receptors, as measured by [18F]setoperone (figure 1 and figure 2). The lowest doses tested—75 mg/day of clozapine, 2–4 mg/day of risperidone, and 5–10 mg/day of olanzapine—all led to more than 95% occupancy of frontal 5-HT2 receptors in most patients. It should be noted that once occupancy goes beyond 90%, the signal available for analysis is less than 10%, and the precision of data beyond this point is limited. Since there were few patients who had midrange 5-HT2 occupancies, it is not valid to try to fit the data to rectangular-hyperbola relationships. Nonetheless, clozapine possesses a greater degree of separation between its 5-HT2 and D2 occupancies than either risperidone or olanzapine (F=12.67, df=2, 25, p<0.0002; clozapine was different at p<0.05, according to Tukey’s post hoc unequal-N test, while risperidone and olanzapine were not different, p>0.10 ).
DISCUSSION
The data show that clozapine differs from risperidone and olanzapine in its D2 occupancy profile. Risperidone and olanzapine have similar profiles but differ in potency. All three of the antipsychotics are complete blockers of 5-HT2 receptors, although clozapine shows the greatest difference between its 5-HT2 and D2 occupancies. We discuss how these findings relate to previous published work, discuss the limitations of our results, and then present the implications of these findings for comparisons between antipsychotics.
Differences in ligand selection, imaging modality, and analysis procedures make comparisons of numbers obtained by different centers difficult. Therefore, our results are best compared with those reported by groups that have data, at least on one of the two receptors, on all three drugs. Pilowsky et al. (23) compared the D2 occupancies of clozapine, risperidone, and olanzapine using IBZM SPECT imaging. They concluded that the D2 occupancy of olanzapine is statistically indistinguishable from that of clozapine and that the D2 occupancy of risperidone is higher than that of both clozapine and olanzapine. Our data disagree with regard to olanzapine. The Pilowsky et al. study had several limitations. First, the spatial resolution, quantification, and signal/noise characteristics of IBZM SPECT imaging are inferior to those of [11C]raclopride PET. Second, their study had a smaller total number of subjects (N=22, versus N=44 in this study), a restricted dose range (10–20 mg/day for olanzapine, while we report on 5–60 mg/day), and fewer subjects taking olanzapine (six, while we report on 17). Third, Pilowsky et al. compared the occupancies without reference to the dose of the drug—the average dose for olanzapine patients was 12.5 mg/day, while that for risperidone patients was 8.7 mg/day, a confounding factor that might explain their finding of a lower occupancy for olanzapine and a higher one for risperidone (see below). Finally, they found no relation between dose and occupancy, questioning the internal consistency of the data. The present study overcomes these limitations.
The Karolinska PET group has provided data on a series of patients taking 125–600 mg/day of clozapine (18), four patients taking 6 mg/day of risperidone (17), and three normal control subjects taking a single dose of 10 mg/day of olanzapine (36). Our data on clozapine confirm theirs. We observed a maximal D2 occupancy of 68%, and Nordstr�m et al. (18) reported 67%; the theoretical maximum occupancy when plasma levels were related to D2 occupancy was 68% in our study and 61% in theirs. Farde et al. (17) reported that 6 mg/day of risperidone led to 75%–80% D2 occupancy; our data show an average of 79% (range=73%–85%). Finally, on the basis of their study of single-dose olanzapine in normal volunteers, these investigators predicted that 10 mg/day of olanzapine should lead to 70% D2 occupancy (36), which is consistent with our observed average of 72% (range=66%–75%). Thus, our results are consistent with previous PET data and provide a more valid basis for comparison of the D2 occupancies of the three drugs.
In addition, we made a comparison of the 5-HT2 and D2 occupancies of these drugs, which has never been reported before. It has been reported previously that low doses of clozapine lead to complete saturation of the 5-HT2 receptors (18). The new finding here is that risperidone and olanzapine also completely block 5-HT2 receptors. The results refute the findings of the occupancy studies in rats done by Schotte et al. (16) in which risperidone showed a greater separation of 5-HT2 and D2 occupancies. In our data, clozapine showed the greatest separation, with risperidone and olanzapine being similar.
Our study is not without its limitations. An important one is that the subjects were not randomly assigned to the drugs and to different doses of each drug. Since clozapine is used in patients who do not respond satisfactorily to other typical and atypical antipsychotics, there is a systematic selection bias here. While, clearly, a prospective randomized assignment to the three drugs would have been preferable, no study has yet been able to achieve this. Furthermore, while the clozapine patients do represent a more treatment-refractory group, there are no data to suggest that D2 occupancy varies systematically as a function of lack of response; in fact, a previous study suggested that responders and nonresponders do not differ in D2 occupancy (7). [11C]raclopride provides only striatal D2 occupancy. The exact site of antipsychotic response is not known, but it is speculated that the mesolimbic D2 receptors may be crucial. However, it is worth noting that a recent study comparing striatal to mesolimbic D2 occupancy, using [11C]raclopride and [11C]FLB (37), found no significant regional differences in D2 occupancy between the striatum and the temporal cortex. It should be pointed out that preferential mesolimbic D2 blockade is not a necessary precondition for mesolimbic selectivity. While there was no evidence for limbic selectivity of receptor blockade for any typical or atypical antipsychotics in ex vivo animal receptor occupancy studies (16), there is clear evidence for preferential functional antagonism of the limbic as opposed to the striatal dopamine system with several of the atypical antipsychotics (38).
Another limitation of our work, as of all the previous studies, is that the individual’s own pretreatment binding potential was not available; therefore, the estimate of occupancy carries an inherent error. However, this error is likely to be small and randomly distributed (39). Furthermore, since the main focus of this study was the difference between the three drugs, all compared with the same baseline values, any such error is unlikely to account for the observed pattern of differences. Finally, it has been demonstrated in animals (40 and suggested in humans (5) that antipsychotics lead to an up-regulation of dopamine D2 receptors. If so, a pretreatment baseline D2 value may result in a lower estimate of D2 occupancy. However, most animal data show that clozapine does not result in receptor up-regulation (40, 41), while the situation with respect to olanzapine and risperidone is not clear. Even if up-regulation occurs, it is more likely with risperidone and olanzapine than with clozapine, and this would have decreased, rather than increased, our chances of finding the difference we report.
What do these results tell us about the pharmacological mechanisms of antipsychotic action? Farde and colleagues (1) have suggested that one needs a threshold of D2 receptor occupancy to obtain a satisfactory antipsychotic response. This threshold lies in the range of 65%–70% (2, 4). It is interesting, then, that both risperidone and olanzapine become effective antipsychotics only at doses which cross these levels of D2 occupancy. Doses of risperidone and olanzapine that do not reach these levels (i.e., <2 mg/day of risperidone and <10 mg/day of olanzapine) are not reliably antipsychotic in most clinical situations. Clozapine, on the other hand, is able to obtain an antipsychotic response with levels of D2 occupancy (usually 30%–60%) that would be insufficient to cause antipsychotic response by themselves (4). Thus, clozapine does not call on the typical D2 occupancy mechanism for inducing antipsychotic response; risperidone and olanzapine do. This raises the possibility that despite some similarities in their receptor profile in vitro, the fundamental mechanism of response of clozapine may be different from that of olanzapine and risperidone in patients. While this question can ultimately be resolved only in a clinical arena in crossover studies, the data on D2 occupancy provide a rationale for why patients who do not respond to risperidone/olanzapine may respond to clozapine and the other way around.
The 5-HT2 receptor data show that all of these drugs are potent antagonists at that receptor. The fact that clozapine saturates 5-HT2 receptors at such a low dose and that one continues to see an increasing response to clozapine in doses up to 350–400 mg/day (42) makes it unlikely that 5-HT2 is the primary source of the antipsychotic effect of clozapine. A similar conclusion was reached by Trichard et al. (43) in their study of chlorpromazine and clozapine. It does not rule out the possibility that high levels of 5-HT2 blockade may modulate or enhance the ability of D2 blockade to induce response or to delay the onset of D2-related side effects (14, 15). However, any benefit provided by a mixed 5-HT2/D2 model must express itself in a narrow range. Patients taking risperidone and olanzapine who have high D2 occupancies experience extrapyramidal side effects and prolactin elevation despite a concomitantly high 5-HT2 occupancy (19,20).
These findings also raise interesting questions regarding the comparison of risperidone and olanzapine with each other and with typical antipsychotics. All of the currently published “pivotal” studies that have compared olanzapine and risperidone with the reference drug haloperidol have used 10–20 mg/day of haloperidol (9, 10, 44). Thus, doses of olanzapine and risperidone that lead to 70%–80% D2 occupancy have been compared with doses of haloperidol that result in more than 90% D2 occupancy (3, 19). It is increasingly being realized that the optimal dose of haloperidol for treatment of most patients may be less than 6 mg/day, while higher doses may result in greater extrapyramidal side effects without extra efficacy (45). Since extrapyramidal side effects can also influence measurement of negative symptoms (46), this raises an interesting question: would risperidone/olanzapine demonstrate superior benefits for extrapyramidal side effects, prolactin levels, and negative symptoms if they were compared with a typical antipsychotic that has the same D2 occupancy? Such D2-occupancy-matched studies will be very valuable for discerning the true components of atypicality.
These data are also of interest in interpreting the comparison between risperidone and olanzapine. In a recently published trial (47), olanzapine, 17.2 mg/day, was compared with risperidone, 7.2 mg/day, and risperidone showed a higher propensity for extrapyramidal side effects and prolactin elevation. According to the equations derived from our data, the study compared an average of 77%–79% D2 occupancy induced by olanzapine with an average of 82%–86% D2 occupancy induced by risperidone. Because both extrapyramidal side effects and prolactin elevation are related to the amount of D2 occupancy, and because as occupancy rises beyond 80%, extrapyramidal side effects become more prominent (1), this raises the question of whether the higher incidence of extrapyramidal side effects/prolactin elevation with risperidone is a function of the choice of dose (and resulting D2 occupancy) rather than a qualitative difference between the two drugs. On the other hand, since the design of the Tran et al. study (47) permitted a clinical titration of the dose, it could also be true that olanzapine is able to muster a greater clinical response with a slightly lower level of D2 occupancy (possibly because of the synergism of its multiple-receptor-blocking profile), and that if D2-equipotent doses of risperidone and olanzapine were compared (e.g., 4–5 mg of risperidone versus 17.2 mg of olanzapine), risperidone might have lower extrapyramidal side effects/prolactin elevation, but olanzapine might then show superior efficacy.
In conclusion, this study provides the first systematic comparison of the D2 and 5-HT2 receptor occupancies of the three most commonly used atypical antipsychotics. Clozapine is able to induce an antipsychotic response with a D2 occupancy lower than that of typical antipsychotics, and this may explain its freedom from extrapyramidal side effects and prolactin elevation. Risperidone and olanzapine become effective antipsychotics only when their D2 occupancy is in the range obtained by low-dose typical antipsychotics (2, 3). They occupy equal numbers of D2 receptors when used in the dose ratio of 1:4 mg/day, respectively. All three drugs saturate the 5-HT2 receptors at subtherapeutic doses, suggesting that 5-HT2 occupancy alone is an unlikely explanation for their antipsychotic effects. The data also have implications for clinical comparison studies. Most studies comparing atypical antipsychotics with haloperidol have compared doses of risperidone/olanzapine that give 65%–80% D2 occupancy with doses of haloperidol that give more than 90% D2 occupancy. This may have biased these comparisons to produce higher extrapyramidal side effects and prolactin elevation with haloperidol. D2-occupancy-matched trials of atypical antipsychotics versus haloperidol and atypical versus atypical antipsychotics would be more informative with regard to the true superiority of one drug over another and would also help in distinguishing the clinical role of receptors other than D2.
Received April 6, 1998; revision received July 29, 1998; accepted Aug. 10, 1998. From the Schizophrenia Division and PET Centre, The Clarke Institute of Psychiatry, Department of Psychiatry, University of Toronto; and the Rotman Research Institute, Baycrest Centre, University of Toronto. Address reprint requests to Dr. Kapur, PET Centre, The Clarke Institute of Psychiatry, 250 College St., Toronto, ON, Canada M5T 1R8; [email protected] (e-mail). Supported by an award from the Medical Research Council of Canada to Dr. Kapur. Astra Arcus, A.B., provided the precursor used in the synthesis of [11C]raclopride, and Janssen-Cilag (France) provided the precursor for the radiochemical synthesis of [18F]setoperone. Some of the data in this report were collected with the support of Janssen Pharmaceutica, Inc. (makers of risperidone) and Eli Lilly & Co. (makers of olanzapine). The authors thank Erin Toole, Doug Hussey, Kevin Cheung, and Terry Bell for technical assistance; Dr. Alan Wilson, Dr. Jean DaSilva, Armando Garcia, and Li Jin for radiochemical synthesis; and Dr. Sylvain Houle for interpretation of PET data.
 |
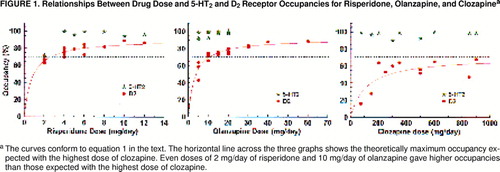
FIGURE 1. Relationships Between Drug Dose and 5-HT2 and D2 Receptor Occupancies for Risperidone, Olanzapine, and Clozapinea
aThe curves conform to equation 1 in the text. The horizontal line across the three graphs shows the theoretically maximum occupancy expected with the highest dose of clozapine. Even doses of 2 mg/day of risperidone and 10 mg/day of olanzapine gave higher occupancies than those expected with the highest dose of clozapine.
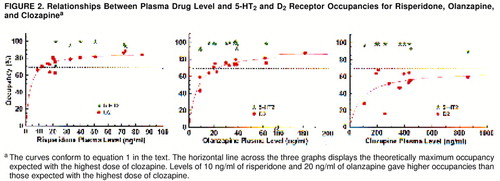
FIGURE 2. Relationships Between Plasma Drug Level and 5-HT2 and D2 Receptor Occupancies for Risperidone, Olanzapine, and Clozapinea
aThe curves conform to equation 1 in the text. The horizontal line across the three graphs displays the theoretically maximum occupancy expected with the highest dose of clozapine. Levels of 10 ng/ml of risperidone and 20 ng/ml of olanzapine gave higher occupancies than those expected with the highest dose of clozapine.
1. Farde L, Nordstrom AL, Wiesel FA, Pauli S, Halldin C, Sedvall G: Positron emission tomographic analysis of central D1 and D2 dopamine receptor occupancy in patients treated with classical neuroleptics and clozapine: relation to extrapyramidal side effects. Arch Gen Psychiatry 1992; 49:538–544Crossref, Medline, Google Scholar
2. Kapur S, Remington G, Jones C, Wilson A, DaSilva J, Houle S, Zipursky R: High levels of dopamine D2 receptor occupancy with low-dose haloperidol treatment: a PET study. Am J Psychiatry 1996; 153:948–950Link, Google Scholar
3. Nyberg S, Farde L, Halldin C, Dahl M-L, Bertilsson L: D2 dopamine receptor occupancy during low-dose treatment with haloperidol decanoate. Am J Psychiatry 1995; 152:173–178Link, Google Scholar
4. Nordstrom AL, Farde L, Wiesel FA, Forslund K, Pauli S, Halldin C, Uppfeldt G: Central D2-dopamine receptor occupancy in relation to antipsychotic drug effects—a double-blind PET study of schizophrenic patients. Biol Psychiatry 1993; 33:227–235Crossref, Medline, Google Scholar
5. Baron JC, Martinot JL, Cambon H, Boulenger JP, Poirier MF, Caillard V, Blin J, Huret JD, Loc’h C, Maziere B: Striatal dopamine receptor occupancy during and following withdrawal from neuroleptic treatment: correlative evaluation by positron emission tomography and plasma prolactin levels. Psychopharmacology (Berl) 1989; 99:463–472Crossref, Medline, Google Scholar
6. Schlegel S, Schlosser R, Hiemke C, Nickel O, Bockisch A, Hahn K: Prolactin plasma levels and D-2-dopamine receptor occupancy measured with IBZM-SPECT. Psychopharmacology (Berl) 1996; 124:285–287Crossref, Medline, Google Scholar
7. Wolkin A, Barouche F, Wolf AP, Rotrosen J, Fowler JS, Shiue C-Y, Cooper TB, Brodie JD: Dopamine blockade and clinical response: evidence for two biological subgroups of schizophrenia. Am J Psychiatry 1989; 146:905–908Link, Google Scholar
8. Kane JM, Freeman HL: Towards more effective antipsychotic treatment. Br J Psychiatry 1994; 165:22–31Crossref, Medline, Google Scholar
9. Marder SR, Meibach RC: Risperidone in the treatment of schizophrenia. Am J Psychiatry 1994; 151:825–835Link, Google Scholar
10. Tollefson GD, Beasley CM Jr, Tran PV, Street JS, Krueger JA, Tamura RN, Graffeo KA, Thieme ME: Olanzapine versus haloperidol in the treatment of schizophrenia and schizoaffective and schizophreniform disorders: results of an international collaborative trial. Am J Psychiatry 1997; 154:457–465Link, Google Scholar
11. Zimbroff DL, Kane JM, Tamminga CA, Daniel DG, Mack RJ, Wozniak PJ, Sebree TB, Wallin BA, Kashkin KB, Sertindole Study Group: Controlled, dose-response study of sertindole and haloperidol in the treatment of schizophrenia. Am J Psychiatry 1997; 154:782–791Link, Google Scholar
12. Arvanitis LA, Miller BG, Seroquel Trial 13 Study Group: Multiple fixed doses of “Seroquel” (quetiapine) in patients with acute exacerbation of schizophrenia: a comparison with haloperidol and placebo. Biol Psychiatry 1997; 42:233–246Crossref, Medline, Google Scholar
13. Meltzer HY, Matsubara S, Lee JC: The ratios of serotonin-2 and dopamine-2 affinities differentiate atypical and typical antipsychotic drugs. Psychopharmacol Bull 1989; 25:390–392Medline, Google Scholar
14. Meltzer HY, Matsubara S, Lee JC: Classification of typical and atypical antipsychotic drugs on the basis of dopamine D-1, D-2 and serotonin-2 pKi values. J Pharmacol Exp Ther 1989; 251:238–246Medline, Google Scholar
15. Kapur S: A new framework for investigating antipsychotic action in humans: lessons from PET imaging. Mol Psychiatry 1998; 3:135–140Crossref, Medline, Google Scholar
16. Schotte A, Janssen PFM, Gommeren W, Luyten WHML, VanGompel P, Lesage AS, DeLoore K, Leysen JE: Risperidone compared with new and reference antipsychotic drugs: in vitro and in vivo receptor binding. Psychopharmacology (Berl) 1996; 124:57–73Crossref, Medline, Google Scholar
17. Farde L, Nyberg S, Oxenstierna G, Nakashima Y, Halldin C, Ericsson B: Positron emission tomography studies on D-2 and 5-HT2 receptor binding in risperidone-treated schizophrenic patients. J Clin Psychopharmacol 1995; 15:S19–S23Google Scholar
18. Nordstr�m A-L, Farde L, Nyberg S, Karlsson P, Halldin C, Sedvall G: D1, D2, and 5-HT2 receptor occupancy in relation to clozapine serum concentration: a PET study of schizophrenic patients. Am J Psychiatry 1995; 152:1444–1449Link, Google Scholar
19. Kapur S, Remington G, Zipursky RB, Wilson AA, Houle S: The D2 dopamine receptor occupancy of risperidone and its relationship to extrapyramidal symptoms: a PET study. Life Sci 1995; 57:PL103–PL107Google Scholar
20. Kapur S, Zipursky RB, Remington G, Jones C, DaSilva J, Wilson AA, Houle S: 5-HT2 and D2 receptor occupancy of olanzapine in schizophrenia: a PET investigation. Am J Psychiatry 1998; 155:921–928Link, Google Scholar
21. Goyer PF, Berridge MS, Morris ED, Semple WE, Compton-Toth BA, Schulz SC, Wong DF, Miraldi F, Meltzer HY: PET measurement of neuroreceptor occupancy by typical and atypical neuroleptics. J Nucl Med 1996; 37:1122–1127Medline, Google Scholar
22. Kufferle B, Brucke T, Topitz-Schratzberger A, Tauscher J, Gossler R, Vesely C, Asenbaum S, Podreka I, Kasper S: Striatal dopamine-2 receptor occupancy in psychotic patients treated with risperidone. Psychiatry Res Neuroimaging 1996; 68:23–30Crossref, Medline, Google Scholar
23. Pilowsky LS, Busatto GF, Taylor M, Costa DC, Sharma T, Sigmundsson T, Ell PJ, Nohria V, Kerwin RW: Dopamine D-2 receptor occupancy in vivo by the novel atypical antipsychotic olanzapine—a I-123 IBZM single photon emission tomography (SPET) study. Psychopharmacology (Berl) 1996; 124:148–153Crossref, Medline, Google Scholar
24. Hietala J, Kuoppamaki M, Nagren K, Lehikoinen P, Syvalahti E: Effects of lorazepam administration on striatal dopamine D-2 receptor binding characteristics in man—a positron emission tomography study. Psychopharmacology (Berl) 1997; 132:361–365Crossref, Medline, Google Scholar
25. Farde L, Wiesel FA, Stone-Elander S, Halldin C, Nordstrom AL, Hall H, Sedvall G: D2 dopamine receptors in neuroleptic-naive schizophrenic patients. Arch Gen Psychiatry 1990; 47:213–219Crossref, Medline, Google Scholar
26. Kapur S, Zipursky R, Jones C, Remington G, Wilson A, DaSilva J, Houle S: The D2 receptor occupancy profile of loxapine determined using PET. Neuropsychopharmacology 1996; 15:562–566Crossref, Medline, Google Scholar
27. Blin J, Pappata S, Kiyosawa M, Crouzel C, Baron JC: [18F]Setoperone: a new high-affinity ligand for positron emission tomography study of the serotonin-2 receptors in baboon brain in vivo. Eur J Pharmacol 1988; 147:73–82Crossref, Medline, Google Scholar
28. Blin J, Sette G, Fiorelli M, Bletry O, Elghozi JL, Crouzel C, Baron JC: A method for the in vivo investigation of the serotonergic 5-HT2 receptors in the human cerebral cortex using positron emission tomography and 18F-labeled setoperone. J Neurochem 1990; 54:1744–1754Crossref, Medline, Google Scholar
29. Pazos A, Probst A, Palacios JM: Serotonin receptors in the human brain, IV: autoradiographic mapping of serotonin-2 receptors. Neuroscience 1987; 21:123–139Crossref, Medline, Google Scholar
30. Petit-Taboue MC, Landeau B, Osmont A, Tillet I, Barre L, Baron JC: Estimation of neocortical serotonin-2 receptor binding potential by single-dose fluorine-18-setoperone kinetic PET data analysis. J Nucl Med 1996; 37:95–104Medline, Google Scholar
31. Mazoyer B: Investigation of the dopamine system with positron emission tomography: general issues in modelling, in Brain Dopaminergic Imaging With Positron Emission Tomography. Edited by Baron JC. Dordrecht, The Netherlands, Kluwer Academic, 1991, pp 65–83Google Scholar
32. Kapur S, Jones C, DaSilva J, Wilson A, Houle S: Reliability of a simple non-invasive method for the evaluation of 5-HT2 receptors using [18F]-setoperone PET imaging. Nucl Med Commun 1997; 18:395–399Crossref, Medline, Google Scholar
33. Lewis R, Kapur S, Jones C, DaSilva J, Brown GM, Wilson AA, Houle S, Zipursky RB: Serotonin 5-HT2 receptors in schizophrenia: a PET study using [18F]setoperone in neuroleptic-naive patients and normal subjects. Am J Psychiatry 1999; 156:72–78Link, Google Scholar
34. Lovdahl MJ, Perry PJ, Miller DD: The assay of clozapine and N-desmethylclozapine in human plasma by high-performance liquid chromatography. Ther Drug Monit 1991; 13:69–72Crossref, Medline, Google Scholar
35. Huang ML, Van Peer A, Woestenborghs R, De Coster R, Heykants J, Jansen AA, Zylicz Z, Visscher HW, Jonkman JH: Pharmacokinetics of the novel antipsychotic agent risperidone and the prolactin response in healthy subjects. Clin Pharmacol Ther 1993; 54:257–268Crossref, Medline, Google Scholar
36. Nyberg S, Farde L, Halldin C: A PET study of 5-HT2 and D-2 dopamine receptor occupancy induced by olanzapine in healthy subjects. Neuropsychopharmacology 1997; 16:1–7Crossref, Medline, Google Scholar
37. Farde L, Suhara T, Nyberg S, Karlsson P, Nakashima Y, Hietala J, Halldin C: A PET study of [C-11]FLB 457 binding to extrastriatal D-2-dopamine receptors in healthy subjects and antipsychotic drug-treated patients. Psychopharmacology (Berl) 1997; 133:396–404Crossref, Medline, Google Scholar
38. Arnt J, Skarsfeldt T: Do novel antipsychotics have similar pharmacological characteristics? a review of the evidence. Neuropsychopharmacology 1998; 18:63–101Crossref, Medline, Google Scholar
39. Kapur S, Zipursky R, Remington G, Jones C, McKay G, Houle S: PET evidence that loxapine is an equipotent blocker of 5-HT2 and D2 receptors: implications for the treatment of schizophrenia. Am J Psychiatry 1997; 154:1525–1529Link, Google Scholar
40. Burt DR, Creese I, Snyder SH: Antischizophrenic drugs: chronic treatment elevates dopamine receptor binding in brain. Science 1977; 196:326–328Crossref, Medline, Google Scholar
41. Lidow MS, Goldman-Rakic PS: Differential regulation of D2 and D4 dopamine receptor mRNAs in the primate cerebral cortex vs neostriatum: effects of chronic treatment with typical and atypical antipsychotic drugs. J Pharmacol Exp Ther 1997; 283:939–946Medline, Google Scholar
42. VanderZwaag C, McGee M, McEvoy JP, Freudenreich O, Wilson WH, Cooper TB: Response of patients with treatment-refractory schizophrenia to clozapine within three serum level ranges. Am J Psychiatry 1996; 153:1579–1584Link, Google Scholar
43. Trichard C, Paill�re-Martinot M-L, Attar-Levy D, Recassens C, Monnet F, Martinot J-L: Binding of antipsychotic drugs to cortical 5-HT2A receptors: a PET study of chlorpromazine, clozapine, and amisulpride in schizophrenic patients. Am J Psychiatry 1998; 155:505–508Link, Google Scholar
44. Chouinard G, Jones B, Remington G, Bloom D, Addington D, MacEwan GW, Labelle A, Beauclair L, Arnott W: A Canadian multicenter placebo-controlled study of fixed doses of risperidone and haloperidol in the treatment of chronic schizophrenic patients. J Clin Psychopharmacol 1993; 13:25–40Crossref, Medline, Google Scholar
45. Bollini P, Pampallona S, Orza MJ, Adams ME, Chalmers TC: Antipsychotic drugs: is more worse? a meta-analysis of the published randomized control trials. Psychol Med 1994; 24:307–316Crossref, Medline, Google Scholar
46. Carpenter WT Jr, Heinrichs DW, Wagman AMI: Deficit and nondeficit forms of schizophrenia: the concept. Am J Psychiatry 1988; 145:578–583Link, Google Scholar
47. Tran PV, Hamilton SH, Kuntz AJ, Potvin JH, Andersen SW, Beasley C, Tollefson GD: Double-blind comparison of olanzapine versus risperidone in the treatment of schizophrenia and other psychotic disorders. J Clin Psychopharmacol 1997; 17:407–418Crossref, Medline, Google Scholar