Physical Aggression in Dementia Patients and Its Relationship to Depression
Abstract
OBJECTIVE: The goal of this study was to determine the frequency of physically aggressive behavior in community-residing patients with dementia and its relationship to depression. METHOD: A consecutive series of 541 patients with DSM-IV-defined dementia underwent comprehensive neuropsychiatric evaluation and were rated on the Cornell Scale for Depression in Dementia, the Mini-Mental State, the Psychogeriatric Dependency Rating Scale, and the General Medical Health Rating. RESULTS: Physically aggressive behavior was exhibited by 79 patients in the 2 weeks before evaluation. Aggressive behavior was closely associated with moderate to severe depression, male gender, and greater impairment in activities of daily living, even after adjustment for delusions, hallucinations, sleep disturbance, and severity of cognitive impairment. After adjustment for depression, gender, and impairment in activities of daily living, there was no association between physically aggressive behavior and the presence of either delusions or hallucinations. CONCLUSIONS: A substantial minority of patients with dementia exhibit physically aggressive behavior, and this aggression is strongly linked with the presence of depressive symptoms. It is possible that the identification and treatment of depression in dementia may be a means of preventing and managing physically aggressive behavior.
Dementia is a major and increasing public health problem in the United States. An important clinical problem for dementia patients and their caregivers is the noncognitive mental and behavioral disturbances that afflict between 70% and 80% of patients over the course of illness (1). Arguably, the most serious such disturbance is physically aggressive behavior. For dementia patients residing in the community, such behavior has several adverse consequences, including injury, mental suffering, hospitalization, and earlier admission to an institutional setting, such as a nursing home (1, 2). Physically aggressive behavior also affects caregivers of dementia patients, leading to chronic mental distress, depression, injury, and patient abuse (3, 4).
The frequency and clinical correlates of physically aggressive behavior in community-residing dementia patients have been assessed in several studies (5–18). The only population-based investigation indicated a 1-year prevalence of 18% (6). Most studies of clinical samples have shown that 15%–20% of the patients exhibited physical aggression in the last month, with as many as 45% having been physically aggressive in the past year (7). Multiple correlates and risk factors for physically aggressive behavior have been described. They include male gender (6, 9), more severe dementia (7, 9, 14, 17), “psychosis,” delusions, or hallucinations (10, 11, 18), earlier age at dementia onset (13), wandering (13), underlying medical illnesses (15), caregiver depression (16), limited space in living arrangements (16), and sleep disorder (13). However, these associations have not been supported universally. For example, some studies suggest that male gender (10), delusions 12, (17), and more severe dementia (9) are not risk factors for physical aggression.
The preceding research has several limitations. Most studies have examined only a small number of risk factors for physically aggressive behavior. Others have focused on aggressive behavior in the elderly in general and not in dementia patients specifically. Also, studies have used varying definitions of physically aggressive behavior, have typically focused on Alzheimer’s disease but not other types of dementia, and have had too few subjects to adequately investigate interrelationships between correlates of aggression. Other studies have had design limitations, such as the use of chart review or of nonstandardized assessment of psychopathology.
Depressive syndromes, both major and minor forms, are important psychopathologic accompaniments of dementia, afflicting as many as 50% of patients with dementia residing in the community (19, 20). Depressive features are associated with “agitation” and psychosis (19) and may mediate the relationship between other forms of psychopathology and aggressive behavior. Such a mediating role might explain contradictory findings of prior studies. To our knowledge, only one study (10) has assessed the relationship between depression and physically aggressive behavior, and it showed no association between the two.
In this study we investigated the frequency and cross-sectional correlates of physically aggressive behavior in community-residing patients with dementia. We were particularly interested in the relationship between aggressive behavior and depression. The study group was a series of patients who met the DSM-IV diagnostic criteria for dementia. We used standardized definitions of physically aggressive behavior, dementia-associated depression, and other psychopathology.
METHOD
Participants and Design
The study participants were a consecutive series of 541 community-residing patients with dementia who were referred for evaluation to the Johns Hopkins Neuropsychiatry and Memory Group over 2 years. Data were collected as part of routine clinical care. All patients who met the DSM-IV criteria for dementia were included in the study. This was a cross-sectional, case-control investigation.
Procedure
All participants underwent comprehensive neuropsychiatric examinations according to previously published methods (19, 20). These included history, neurological examination, mental status examination, brain imaging, ECG, chest X-rays, and laboratory assessment (chemistries, complete blood count, liver tests, thyroid tests, rapid plasma reagin test for syphilis, urinalysis, and measurement of electrolytes, serum B12, serum folate, and sedimentation rate). Psychiatric diagnoses based on DSM-IV criteria were made by experienced geriatric psychiatrists using input from family members, caregivers, and primary care physicians. In accordance with consensus clinical criteria, the psychiatrists classified the type of dementia as possible or probable Alzheimer’s disease (21), possible or probable vascular dementia (22), or “other” (not meeting the criteria for either of the other types).
The psychiatrists were also asked to specify whether the participants had sleep disturbances according to DSM-IV criteria and whether they suffered from delusions or hallucinations according to DSM-IV glossary definitions. The participants were rated concurrently on the Cornell Scale for Depression in Dementia (23), a quantitative measure of depressive symptoms incorporating information from patient examination, observation, and caregiver interview. These ratings are independent of the presence or absence of physically aggressive behavior, although ratings of mood-congruent delusions are made. In dementia patients, scores higher than 12 on the Cornell Scale for Depression in Dementia are highly suggestive of a psychiatrist-ascertained major depressive episode (19, 23).
The study participants were also rated on the following: 1) the Mini-Mental State (24) to quantify the severity of dementia, 2) the activities of daily living subscale of the Psychogeriatric Dependency Rating Scale (25), and 3) the General Medical Health Rating (19). The General Medical Health Rating was designed at the Johns Hopkins Neuropsychiatry and Memory Group to rate the status of general medical health in patients with dementia by means of a standardized process. Ratings of “excellent,” “good,” “fair,” and “poor” are possible. The interrater reliability of the General Medical Health Rating was studied by using ratings for 50 patients with dementia. Of these, 48% lived in the community, 32% lived in assisted living facilities, and 20% lived in nursing homes. These patients had a mean age of 80.3 years (SD=8.1), 70% were female, 80% had Alzheimer’s disease, 10% had vascular dementia, and 10% had other dementias. They were rated independently on the General Medical Health Rating by a geriatric psychiatrist and a nurse. The scale’s estimated reliability was excellent (kappa=0.91).
Definition of Physically Aggressive Behavior
The literature was reviewed to identify reported definitions of physically aggressive behavior in dementia patients or other elderly patients. The most widely used definitions found were those of Patel and Hope (26) and of Cohen-Mansfield et al. (27) (developed for elderly nursing home residents). Given its broader scope, the definition proposed by Patel and Hope was used, after slight modification. Thus, physically aggressive behavior was defined as “an overt act involving delivery of a noxious stimulus to another person which was clearly not accidental.” The presence of physically aggressive behavior in the 2 weeks before evaluation was assessed so as to be in line with the time definitions used in the Psychogeriatric Dependency Rating Scale, on which participants were already being rated.
Analyses
One purpose of the study was to obtain a frequency estimate of physically aggressive behavior in community-residing dementia patients in the last 2 weeks. This estimate is reported. A second intent of the study was to compare aggressive and nonaggressive dementia patients on a series of variables. We present and contrast aggressive and nonaggressive patients on sociodemographic characteristics (age, gender, race, education); general medical health (General Medical Health Rating); identity of primary caregiver; dementia characteristics (type, severity of cognitive impairment, severity of impairment in activities of daily living); and dementia-associated psychopathology (severity of depressive symptoms, delusions, hallucinations, sleep disorder).
A final purpose of the study was to investigate the relationship between depression and physically aggressive behavior, after adjustment for other important variables. We defined moderate–severe depression as a score higher than 12 on the Cornell Scale for Depression in Dementia and compared patients with depression to those without (i.e., having a score of 12 or less). A series of bivariate and multivariate logistic regression models were estimated to quantify the relationship between physically aggressive behavior and depression and the associations between aggressive behavior and other variables. The dependent variable was the presence or absence of aggressive behavior, and the independent variable was depression or one (or more) of the other variables. In secondary analyses, the score on the Cornell Scale for Depression in Dementia was used as a continuous measure in place of moderate–severe depression in otherwise identical regression models. The findings were similar, and so the results from the initial analyses only are reported.
RESULTS
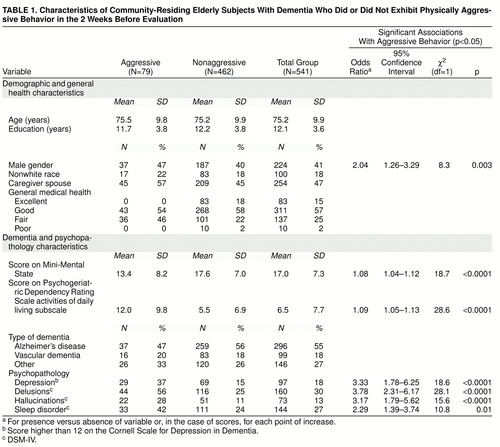
Among the 541 dementia patients examined, 79 (15%) had exhibited physically aggressive behavior during the 2 weeks before the evaluation. table 1 contains data on the total group of study participants, those who had not exhibited aggressive behavior in the past 2 weeks, and those who had exhibited aggressive behavior in the last 2 weeks. The relationship between each of these variables and the likelihood of physically aggressive behavior was explored in bivariate logistic regression models with physically aggressive behavior as the dependent variable. Results are included in the table only for the variables with statistically significant associations with aggressive behavior (p<0.05). As expected, participants with moderate–severe depression (score higher than 12 on the Cornell Scale for Depression in Dementia) were more likely to be physically aggressive. In addition, men were twice as likely as women to be aggressive. Participants with more severe dementia (lower Mini-Mental State score) or greater impairment in activities of daily living (higher score on the Psychogeriatric Dependency Rating Scale subscale for activities of daily living) were also more likely to be aggressive. Those with delusions, hallucinations, or sleep disorder were also more likely to be aggressive.
None of the other variables assessed had a significant association with physically aggressive behavior in the bivariate regression models (in all cases, p>0.06). Thus, aggressive behavior did not appear to be related to education, identity of caregiver, or status of general medical health. Patients with Alzheimer’s disease, those with vascular dementia, and those with other types of dementia were all equally likely to exhibit aggressive behavior.
In the multivariate logistic regressions, we first included all variables significant in the bivariate models: moderate–severe depression, gender, Mini-Mental State score, score on the activities of daily living subscale of the Psychogeriatric Dependency Rating Scale, delusions, hallucinations, and sleep disturbance. In this model, depression (odds ratio=2.41 for depressed versus nondepressed, χ2=5.8, df=1, p=0.02), gender (odds ratio=3.06 for men versus women, χ2=10.0, df=1, p=0.002), and greater impairment in activities of daily living (odds ratio=1.06 for each point increase in score, χ2=6.0, df=1, p=0.01) each retained a significant association with physically aggressive behavior. None of the other variables was significantly associated with physically aggressive behavior (in all cases, p>0.09). A final model was estimated that included only depression (odds ratio=2.73, χ2=9.0, df=1, p=0.003), gender (odds ratio=2.47, χ2=7.7, df=1, p=0.006), and score on the activities of daily living subscale of the Psychogeriatric Dependency Rating Scale (odds ratio=1.09, χ2=18.8, df=1, p<0.0001).
DISCUSSION
In this large consecutive series of patients with dementia, we found the frequency of physically aggressive behavior in the past 2 weeks to be 15%. Patients with more depressive symptoms, those with greater impairment in activities of daily living, and those who were men were the most likely to exhibit aggressive behavior. This maybe an overestimation of the true prevalence of aggressive behavior in the community, since such behaviors probably increase the likelihood of referral to a clinical setting. However, the estimate is in accord with those in most other studies on the issue (5–18). There is wide agreement that physical aggression is not exhibited by the great majority of dementia patients residing in the community.
To our knowledge, the association between depression and physically aggressive behavior in dementia has not been reported previously. We know of only one other published report of a study of the relationship between aggressive behavior and depression, and it showed no association between the two (10). However, the investigators in that study used a less systematic quantification of depressive symptoms and a broader definition of aggression. Furthermore, the number of subjects was much smaller, so that the failure to detect a relationship between aggressive behavior and depression may have been due to type II error. It is interesting that after we adjusted for depression and other significant variables in the multivariate regression model, other types of psychopathology, such as delusions, hallucinations, and sleep disorder, were no longer significantly associated with physically aggressive behavior.
Given that major and minor depression affect almost 50% of patients with Alzheimer’s disease (19) and since substantial numbers of patients with other forms of dementia suffer from depressive symptoms (20), the identification and treatment of depression in dementia patients is an important approach to managing physical aggression. Several treatments are available for depression in dementia, including antidepressant medications (28, 29), behavioral treatments (30), and ECT (V. Rao and C.G. Lyketsos, unpublished).
Impairment in activities of daily living in demented patients is associated with depression (19). Moreover, as we report here, physically aggressive behavior is related to both depression and impairment in activities of daily living. Thus, it is possible that for some patients impairment in activities of daily living is the primary problem leading to both aggressive behavior and depressive symptoms, such as dysphoria, anger, and low frustration tolerance. For these latter patients, the best interventions for treating both the depressive symptoms and the physically aggressive behavior would be ones that help patients adapt to their impairment in activities of daily living.
This work confirms that of others (6, 9) suggesting that male gender is important to the development of aggression in dementia patients. This is not unexpected since men are more likely than women to be aggressive overall (31). Several mechanisms, including hormonal and cultural factors, might be involved. The possibility that androgens, testosterone specifically, play a role in the development of aggression in dementia patients has received some support from reports in the literature that aggressive men with dementia become less aggressive with antiandrogen therapy using leuprolide (32) or progestins (33).
The relationship between greater impairment in activities of daily living and physical aggression, present even after adjustment for severity of dementia, suggests that a substantial proportion of physically aggressive behavior may occur while caregivers are providing assistance with activities of daily living. This relationship between aggressive behavior and efforts to provide assistance with activities of daily living is a common problem in nursing homes (34). Whether the functional decline is due to dementia or general medical impairment (both of which are likely involved), the provision of assistance with basic daily living activities to dementia patients can lead to aggressive behavior, particularly if caregivers are inexperienced or themselves impaired. Therefore, one avenue for managing aggressive behavior in dementia patients is to identify the instances of aggressive behavior that occur during daily care and to teach caregivers at home better approaches to daily care. Additionally, since impairment in activities of daily living is itself associated with depression (19), it is occasionally possible that both physically aggressive behavior and impairment in activities of daily living are due to depression. Therefore, some patients with physically aggressive behavior might also show improvements in activities of daily living if their depression is identified and treated.
Our finding that the relationship between delusions or hallucinations and aggressive behavior is no longer significant after adjustment for depression and other variables builds on others’ work showing links between these mental phenomena and physically aggressive behavior (10, 11, 18). The latter studies relating physical aggression to psychosis did not account for the relationship between psychosis and depression. We propose that the association of delusions and hallucinations with physically aggressive behavior, observed in this study in the bivariate analyses, is mediated in part by the presence of depression. However, we do not wish to downplay the importance of delusions and hallucinations in the development of aggression. Good clinical care of dementia patients requires the identification and treatment of depression, sleep disorders, delusions, and hallucinations, since there is anecdotal evidence that this leads to reductions in aggression.
While the relationships between physically aggressive behavior and multiple variables were examined in this study, much of the variance in aggressive behavior is still unexplained. Thus, there are many other factors involved in its development. These factors may be intertwined with depression, male gender, and impairment in activities of daily living. One important such variable is location of the brain involvement of the dementing disease, regardless of cause. Patients in whom the dementing disease leads to imbalances of important neurotransmitter systems are more likely to exhibit physically aggressive behavior. For example, pathologic studies have shown that damage to the serotonergic system (35), relative preservation of the dopaminergic system (36), and a higher number of α2 adrenergic receptors in the cerebellum (37) are associated with aggression in dementia.
It is important to appreciate that aggression in dementia patients is best approached as a nonspecific symptom. In clinical settings it is critical to evaluate systematically all patients who are aggressive. Such an evaluation (for example, as proposed in reference 1) must first define the aggression exhibited by each patient and its temporal characteristics. This is followed by a review of the history, examination of the patient (both physical and mental status), necessary laboratory studies, and then a review of potential contributors to aggression. As we demonstrate in this research, depressive symptoms and interactions during activities of daily living appear to be important contributors to aggression that must be treated or managed. Additionally, other coexisting psychopathology must be treated as well. Investigations are also necessary to rule out any relationship between aggression and an active general medical condition, such as a urinary tract infection, or the use of an excessive number of medications.
A few limitations of this study must also be considered. First, this is a consecutive series of a clinical sample. While this sampling method may limit our ability to estimate the prevalence of physically aggressive behavior in community-residing patients with dementia, there is no reason to expect that it would affect the relationship between aggression and depression or other variables. Second, we did not examine an exhaustive set of variables that might have been associated with aggression. In particular, caregiver variables were not adequately assessed. Third, we did not collect further details on the physically aggressive behavior exhibited, such as its severity or frequency, which might have been important in further understanding the correlates of aggression in the sample. Fourth, this was a cross-sectional study, which limits our ability to make causal inferences. Finally, while we have shown a relationship between aggression and depression, we cannot be confident that treatment and resolution of depression would lead to resolution of the aggression.
Received Feb. 19, 1998; revision received June 2, 1998; accepted July 9, 1998. From the Neuropsychiatry and Memory Group, Department of Psychiatry and Behavioral Sciences, School of Medicine, The Johns Hopkins University; and Copper Ridge, Sykesville, Md. Address reprint requests to Dr. Lyketsos, Osler 320, The Johns Hopkins Hospital, 600 North Wolfe St., Baltimore, MD 21287; [email protected] (e-mail). Supported in part by NIMH grant MH-56511. The authors thank Betty Burgeois for typing the manuscript.
 |
1. Lyketsos CG, Steele C, Steinberg M: Behavioral disturbances in dementia, in Reichel’s Care of the Aged. Edited by Gallo JJ. Philadelphia, Williams & Wilkins (in press)Google Scholar
2. Mega MS, Cummings JL, Fiorello T, Gornbein J: The spectrum of behavioral change in Alzheimer’s disease. Neurology 1996; 46:130–135Crossref, Medline, Google Scholar
3. Rabins PV, Mace NL, Lucas MJ: The impact of dementia on the family. JAMA 1982; 248:333–335Crossref, Medline, Google Scholar
4. O’Donnell BF, Drachman DA, Barnes HJ, Peterson KE, Swearer JM, Lew RA: Incontinence and troublesome behaviors predict institutionalization in dementia. J Geriatr Psychiatry Neurol 1992; 5:45–52Crossref, Medline, Google Scholar
5. Gibbons P, Gannon M, Wrigley M: A study of aggression among referrals to a community-based psychiatry of old age service. Int J Geriatr Psychiatry 1997; 12:384–388Crossref, Medline, Google Scholar
6. Burns A, Jacoby R, Levy R: Psychiatric phenomena in Alzheimer’s disease, IV: disorders of behavior. Br J Psychiatry 1990; 157:86–94Crossref, Medline, Google Scholar
7. Ryden MB: Aggressive behavior in persons with dementia who live in the community. Alzheimer Dis Assoc Disord 1988; 2:342–355Crossref, Medline, Google Scholar
8. Shah AK: Aggressive behavior among patients referred to a psychogeriatric service. Med Sci Law 1993; 32:144–150Google Scholar
9. Eastley R, Wilcock GK: Prevalence and correlates of aggressive behaviors occurring in patients with Alzheimer’s disease. Int J Geriatr Psychiatry 1997; 12:484–487Crossref, Medline, Google Scholar
10. Aarsland D, Cummings JL, Yener G, Miller B: Relationship of aggressive behavior to other neuropsychiatric symptoms in patients with Alzheimer’s disease. Am J Psychiatry 1996; 153:243–247Link, Google Scholar
11. Deutsch LH, Bylsma FW, Rovner BW, Steele C, Folstein MF: Psychosis and physical aggression in probable Alzheimer’s disease. Am J Psychiatry 1991; 148:1159–1163Link, Google Scholar
12. Mendez MF, Martin RJ, Smyth KA, Whitehouse PJ: Psychiatric symptoms associated with Alzheimer’s disease. J Neuropsychiatry Clin Neurosci 1990; 2:28–33Crossref, Medline, Google Scholar
13. Tsai SJ, Hwang JP, Yang CH, Liu KM: Physical aggression and associated factors in probable Alzheimer’s disease. Alzheimer Dis Assoc Disord 1996; 10:82–85Crossref, Medline, Google Scholar
14. Hamel M, Gold DP, Andres D, Reis M, Dastoor D, Grauer H, Bergman H: Predictors and consequences of aggressive behavior by community based dementia patients. Gerontologist 1990; 30:206–211Crossref, Medline, Google Scholar
15. Malone ML, Thompson L, Goodwin JS: Aggressive behaviors among the institutionalized elderly. J Am Geriatr Soc 1993; 41:853–856Crossref, Medline, Google Scholar
16. Paveza GJ, Cohen D, Eisdorfer C, Freels S, Semla T, Ashford JW, Gorelick P, Hirshman R, Luchins D, Levy P: Severe family violence and Alzheimer’s disease: prevalence and risk factors. Gerontologist 1992; 32:493–497Crossref, Medline, Google Scholar
17. Swearer JM, Drachman DA, O’Donnell BF, Mitchell AL: Troublesome and disruptive behaviors in dementia. J Am Geriatr Soc 1988; 36:784–790Crossref, Medline, Google Scholar
18. Gilley DW, Wilson RS, Beckett LA, Evans DA: Psychotic symptoms and physically aggressive behavior in Alzheimer’s disease. J Am Geriatr Soc 1997; 45:1074–1079Crossref, Medline, Google Scholar
19. Lyketsos CG, Baker L, Warren A, Steele C, Brandt J, Steinberg M, Kopunek S, Baker A: Major and minor depression in Alzheimer’s disease: prevalence and impact. J Neuropsychiatry Clin Neurosci 1997; 9:556–561Crossref, Medline, Google Scholar
20. Payne JL, Lyketsos CG, Baker L, Warren A, Steele C, Brandt J, Steinberg M, Kopunek S, Baker A: The relationship of cognitive and functional impairment to depressive features in Alzheimer’s disease and other dementias. J Neuropsychiatry Clin Neurosci (in press)Google Scholar
21. McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM: Clinical diagnosis of Alzheimer"s disease: report of the NINCDS-ADRDA Work Group under the auspices of the Department of Health and Human Services Task Force on Alzheimer"s Disease. Neurology 1984; 34:939–944Crossref, Medline, Google Scholar
22. NINDS/AIREN International Workshop: Vascular dementia: diagnostic criteria for research studies. Neurology 1993; 43:250–260Crossref, Medline, Google Scholar
23. Alexopoulos GS, Abrams RC, Young RC, Shamoian CA: Cornell Scale for Depression in Dementia. Biol Psychiatry 1988; 23:271–284Crossref, Medline, Google Scholar
24. Folstein MF, Folstein SE, McHugh PR: “Mini-Mental State”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975; 12:189–198Crossref, Medline, Google Scholar
25. Wilkinson IM, Graham-White J: Psychogeriatric dependency rating scales (PGDRS): a method of assessment for use by nurses. Br J Psychiatry 1980; 137:558–565Crossref, Medline, Google Scholar
26. Patel V, Hope T: Aggressive behavior in elderly people with dementia: a review. Int J Geriatr Psychiatry 1993; 8:457–472Crossref, Google Scholar
27. Cohen-Mansfield J, Werner P, Marx MS: An observational study of agitation in agitated nursing home residents. Int Psychogeriatr 1989; 1:153–165Crossref, Medline, Google Scholar
28. Reifler BV, Teri L, Raskind M, Veith R, Barnes R, White E, McLean P: Double-blind trial of imipramine in Alzheimer’s disease patients with and without depression. Am J Psychiatry 1989; 146:45–49Link, Google Scholar
29. Petracca G, Teson A, Chemerinski E, Leiguarda R, Starkstein SE: A double-blind placebo-controlled study of clomipramine in depressed patients with Alzheimer’s disease. J Neuropsychiatry Clin Neurosci 1996; 8:270–275Crossref, Medline, Google Scholar
30. Teri L: Behavioral treatment of depression in patients with dementia. Alzheimer Dis Assoc Disord 1994; 8(suppl 3):66–74Google Scholar
31. Birkett DP: Violence in geropsychiatry. Psychiatr Annals 1997; 27:752–756Crossref, Google Scholar
32. Ott BR: Leuprolide treatment of sexual aggression in a patient with dementia and the Kluver-Bucy syndrome. Clin Neuropharmacol 1995; 18:443–447Crossref, Medline, Google Scholar
33. Kyomen HH, Nobel KW, Wei JY: The use of estrogen to decrease aggressive physical behavior in elderly men with dementia. J Am Geriatr Soc 1991; 39:1110–1112Crossref, Medline, Google Scholar
34. Farrell Miller M: Physical aggressive resident behavior during hygienic care. J Gerontol Nurs 1997; 23:24–39Crossref, Medline, Google Scholar
35. Procter AW, Francis PT, Stratmann GC, Bowen DM: Serotonergic pathology is not widespread in Alzheimer patients without prominent aggressive symptoms. Neurochem Res 1992; 17:917–922Crossref, Medline, Google Scholar
36. Victoroff J, Zarow C, Mack WJ, Hsu E, Chui HC: Physical aggression is associated with preservation of substantia nigra pars compacta in Alzheimer’s disease. Arch Neurol 1996; 53:428–434Crossref, Medline, Google Scholar
37. Russo-Neustadt A, Cotman CW: Adrenergic receptors in Alzheimer’s disease brain: selective increases in the cerebella of aggressive patients. J Neurosci 1997; 17:5573–5580Crossref, Medline, Google Scholar



