HIV Seroprevalence Among Suicide Victims in New York City, 1991–1993
Abstract
OBJECTIVE: The authors sought to determine the HIV seroprevalence among suicide victims in New York City. METHOD: All suicides of city residents from 1991 through 1993 were studied. The crude proportion of all suicide victims who were HIV positive and the proportion adjusted to the age, gender, and racial/ethnic characteristics of the New York City population were determined. The demographically adjusted proportion was then contrasted with HIV seroprevalence estimates for the New York City general population. HIV-seropositive suicide victims were assessed for pathological findings suggestive of HIV-related illnesses. RESULTS: The crude proportion of all suicide victims who were HIV seropositive was 0.088, and the demographically adjusted proportion was 0.049. Over 90% of all HIV-positive suicide victims were aged 25 to 54 years, and almost 90% were men. Among black and Hispanic men aged 35 to 54 years who committed suicide, the proportion who were HIV seropositive was 0.252—the highest seropositive rate of any demographic group. More than two-thirds of HIV-seropositive suicide victims had no HIV-related pathology or AIDS-indicator conditions at autopsy. CONCLUSIONS: The demographically adjusted proportion of suicide victims who were HIV positive (approximately 0.038 to 0.059), contrasted with the HIV seroprevalence estimates for the New York City general population (approximately 0.014 to 0.032), the absence of HIV-related pathology among suicide victims, and the likelihood that many HIV-positive individuals had other risk factors for suicide, such as substance abuse, suggests that a positive HIV serostatus is associated, at most, with a modest elevation in suicide risk. (Am J Psychiatry 1997; 154:1720–1725)
In 1985 we conducted a study in New York City to determine the risk of suicide among persons with AIDS (1). At the time there were 3,390 known adult cases of AIDS in New York City that had been diagnosed since 1981; more than 90% of those affected were men, and half were white. The HIV serotest had just been devised. We found 12 instances of suicide among persons with AIDS, all of whom were men, aged 22 to 56 years, and most of whom were white—representing a suicide risk 36 times that of men in the general city population of similar age. Subsequent studies also have reported high rates of suicide among persons with AIDS (2–4).
By early 1991, there were 34,822 known cases of AIDS in New York City, and 1%–3% of the city's population was estimated to be infected with HIV (5). At that time, of the population with AIDS, 15% were women, and 65% were nonwhite. The median probability of survival from the date of AIDS diagnosis had increased (6), new drugs increasingly were being used to treat HIV illness at an earlier stage, and the stigma of infection, while persisting, was somewhat reduced. Although there was more hopefulness among many about the prognosis of the disease, there was also an increasing acceptance of “rational” suicide for those with AIDS or other terminal illnesses (7).
Whereas there have been studies of AIDS-related suicides, it is particularly important to understand the demographic and clinical characteristics of suicide among persons who are HIV positive but who may not yet have developed clinical symptoms. This group represents a much larger and healthier population than the subset with AIDS (8). Targeting it for early intervention to prevent suicide could save many years of productive life. While there have been some studies of suicides (9) and nonfatal suicide attempts (10) related to HIV infection, there has been only one systematic, population-based study, which found that HIV-positive individuals did not have a significantly greater risk of suicide in the months following HIV screening (11). However, the study was limited to a population of about 4,000 military service applicants. Thus, we sought to examine the HIV seroprevalence among suicide victims in the general population of New York City at a time when the demographic distribution of the disease was changing, there was renewed hope for treatments and improved prognosis, and there was increasing social acceptance of assisted, self-inflicted fatal poisoning. We also sought to determine whether HIV-positive individuals who committed suicide had HIV-related pathological findings at the time of death. Although there is no population-based enumeration of HIV serostatus as there is for AIDS, a disease that is reportable by law, we also sought to place our estimate of the HIV seroprevalence among suicide victims into a larger context by using estimates of HIV seroprevalence in the general population in New York City.
METHOD
The study was conducted at the Office of the Chief Medical Examiner of New York, which has jurisdiction for all unnatural deaths in New York City. We studied all deaths among New York City residents from 1991 through 1993 that the medical examiner certified as a suicide (ICD-9 code E950-959). Each file from the medical examiner was reviewed for demographic information; the time, date, and location of injury and death; location of the decedent's latest residence; methods of suicide; and autopsy findings.
Autopsies are conducted by full-time forensic pathologists, typically within 24 hours of the pronounced time of death. The autopsies are complete and include examination of the brain, neck organs, and thoracic and abdominal viscera. Autopsies are not conducted in cases of clear-cut suicides in which there are strong family objections to autopsy, usually because of religious reasons. Such cases undergo the usual medicolegal scene investigation, police investigation, and an external examination. In the 3-year study period, 86% of all certified suicide victims underwent a complete autopsy.
Routine HIV blood screening of autopsied cases began at the Office of the Chief Medical Examiner in January 1991. In all autopsied cases, plasma and serum samples are obtained for HIV screening at the New York City Department of Health Laboratory. Initial screening is done in replicate by enzyme-linked immunosorbent assay (ELISA) with confirmation by the Western blot test. Samples that yield a mixed result are considered “inconclusive.” ELISA has been shown to have a sensitivity and specificity approaching 100% in samples from living persons (12), and HIV antibodies can be detected for months after death (13).
The Centers for Disease Control and Prevention (CDC) classification system for HIV disease staging provides for three clinical categories, which are based on the presence or absence of AIDS indicator conditions such as Kaposi's sarcoma and recurrent pneumonia, and for three CD4+ T cell counts (14). The use of autopsy data precludes using the current CDC staging system in an exact manner. For example, enumeration of lymphocyte subsets cannot be reliably made after death; some distinctions between clinical categories A and B, which are based on current physical symptoms at time of death, are not known reliably at autopsy. Nevertheless, mindful of these caveats, we wished to assess whether most HIV-seropositive suicide victims had AIDS-indicator conditions (category C) at the time of death and whether specific types of AIDS-related illnesses were more likely than others to be found at autopsy. Accordingly, for each case we systematically reviewed autopsy findings for all CDC-specified AIDS-indicator conditions.
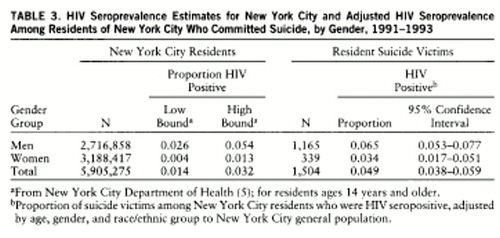
The exact number of residents of New York City who are infected with HIV is unknown. In 1989, the New York City Health Department convened an expert panel on HIV seroprevalence estimates and AIDS projection methodologies (5). This group used a variety of methods including direct calculation, back calculation, ratio comparisons with San Francisco, and serosurveys of pregnant women to derive estimates of HIV seroprevalence in component groups at risk for AIDS, such as men who have sex with men, intravenous drug users, and others not specifically at risk. This yielded low- and high-bound estimates for HIV seroprevalence in the general population of New York City, which were subsequently updated. These estimates were made for men and women and for the population as a whole and were not made for specific demographic strata. Because these seroprevalence estimates are not derived exclusively from serosurvey data and therefore differ in methodology from our serosurvey of suicide victims, we do not present estimates of relative risk. Instead, we present only the upper and lower bounds of the general population estimate and our serosurvey's adjusted proportion among suicide victims, with 95% confidence intervals.
Differences in categorical variables were assessed by using chi-square analysis with a continuity correction. Differences between two means were assessed with a t test. The crude proportion of HIV-positive suicide victims was calculated by dividing the number of HIV-seropositive suicide victims by the total number of suicide victims in a given demographic stratum. Crude proportions were adjusted by age, gender, and race/ethnicity to the New York City general population on the basis of 1990 U.S. census data. Ninety-five percent confidence intervals were calculated about a proportion (15). Statistical significance was defined as a two-tailed alpha of less than 0.05.
RESULTS
Proportion of Suicide Victims Screened for HIV
There were 1,875 suicides among New York City residents during the period 1991 through 1993. Of these, 1,511 (80.6%) were screened for HIV. Compared to those who underwent screenings, nonscreened subjects were more likely to be older (mean=52.1 years, SD=20.7, versus mean=42.2, SD=17.4) (t=9.24, df=1,873, p<0.001), to be white or Asian (percent screened: non-Hispanic white, 72.8% Asian/other, 73.8% non-Hispanic black, 90.4% Hispanic, 94.4%) (χ2=111.1, df=3, p<0.001), and to be women (women screened: 76.2% men screened: 82.0%) (χ2=7.0, df=1, p=0.007). Of the 1,131 suicide victims 25–54 years old, the age group expected to have the highest rate of HIV infection, 955 (84.4%) were screened.
HIV Seroprevalence Among Suicide Victims
Of the 1,511 suicide victims who were screened for HIV, seven had inconclusive test results. Among the remaining 1,504, there were 133 HIV-seropositive subjects, or a crude proportion of 0.088 (95% confidence interval=0.075–0.102).
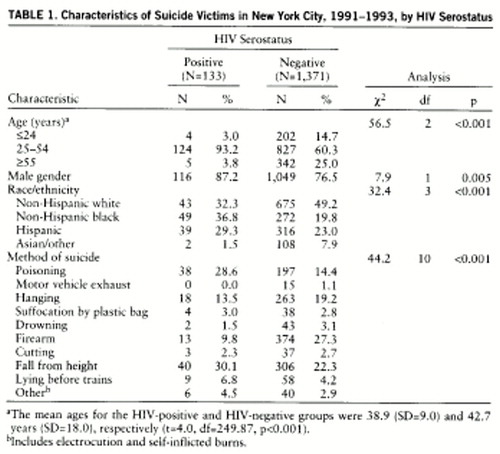
Compared with HIV-negative suicide victims, HIV-positive suicide victims were likely to be men (87.2%), ages 25 to 54 years (93.2%), and non-Hispanic black or Hispanic (66.1%) (table 1). HIV-positive individuals who committed suicide were almost twice as likely to use poisoning as were HIV-negative individuals and one-third as likely to use firearms; the use of other methods was approximately the same.
Men who committed suicide were about twice as likely as women to be HIV positive (odds ratio=2.09; 95% confidence interval=1.24–3.54) (table 2). The HIV seroprevalence rate was highest for those persons aged 25 to 54 years (proportion=0.130, 95% confidence interval=0.109–0.151). The seroprevalence rate for men under age 25 or over age 54 was low (proportion=less than 0.02). The proportion for men under age 25 was 0.022 (95% confidence interval=0.011–0.056); the proportion for men over age 54 was 0.020 (95% confidence interval=0.010–0.046). For women under age 25, as well as for women over age 54, the proportions were 0. Of all racial groups, non-Hispanic blacks had the highest seroprevalence (0.153), followed by Hispanics (0.110), non-Hispanic whites (0.060), and Asians or others (0.018).
Within specific demographic strata, non-Hispanic black and Hispanic men aged 35 to 54 years had the highest proportion who were HIV positive (proportion=0.252, 95% confidence interval=0.190–0.314). White men in this age group were less likely to be HIV positive (proportion=0.127, 95% confidence interval=0.082–0.171). Among women, non-Hispanic blacks and Hispanics aged 25 to 44 years had the highest seroprevalence rate (proportion=0.189, 95% confidence interval=0.100–0.278). In contrast, white women aged 25 to 44 years had one of the lowest seroprevalence rates (proportion=0.030, 95% confidence interval=0.000–0.070). The seroprevalence rates for other specific age-sex-racial strata are available from Dr. Marzuk.
HIV-Related Autopsy Findings
Of the 133 HIV-positive suicide victims who underwent complete autopsy, 39 (29.3%) had HIV-related pathological findings. Eleven individuals had generalized lymphadenopathy without any other findings. Of the 133 cases, 29 had at least one finding suggestive of an AIDS-related illness. The most common AIDS-indicator conditions found at autopsy included pneumonia (N=11), wasting syndrome (N=11), Kaposi's sarcoma (N=4), and mycobacterium tuberculosis (N=3). An important finding was that 94 (70.6%) of the 133 HIV-positive suicide victims had no pathological evidence of an HIV illness at death.
Adjusted HIV Seroprevalence Among Suicide Victims and New York City HIV Seroprevalence Estimates
We also contrasted the proportion of all suicide victims who were HIV positive, demographically adjusted to the New York City general population, for comparison with the high- and low-bound estimates of HIV seroprevalence in the city (table 3). Overall, our estimates for HIV seroprevalence among suicide victims with the 95% confidence intervals fall slightly above the high-bound estimates of HIV seroprevalence in the general population. Our point estimate of 0.049 is approximately twice that of the midpoint of the estimates of the high and low bounds for the New York City population.
DISCUSSION
We found that almost 9% of all suicide victims in New York City in the early 1990s were HIV positive. However, the HIV seroprevalence among suicide victims after demographic adjustment was only moderately higher than the estimates of HIV seroprevalence in the general population of New York City. Although the exact HIV seroprevalence of the general population is unknown, these estimates suggest that a positive HIV serostatus probably represents, at most, a twofold higher risk for suicide than that of the general New York City population. This finding is similar to the twofold higher risk of suicide reported among HIV-seropositive military applicants (11). Among the suicide victims in our study who were HIV positive, about 70% had no HIV-related illness at autopsy. Thus, it is unlikely that pain, physical discomfort, or diminished physical mobility played a role in the majority of suicides among HIV-positive individuals. Since the HIV screening in this study was done at autopsy, some individuals who committed suicide may not have even been aware that they were seropositive. In addition, many individuals who were HIV seropositive undoubtedly had other risks for suicide such as substance abuse and alcoholism (16). Unfortunately, neither the HIV seroprevalence nor the suicide rate among persons with confounding risk factors such as substance abuse is known in the population at large. All of these lines of evidence suggest that a positive HIV serostatus, in itself, could be associated, at most, with a modest elevation in suicide risk.
This finding dampens concerns on several fronts. First, as more Americans become HIV positive, an estimated 897,000 by 1993 (17), our data suggest that it is unlikely that any substantial increase in the suicide rate, due to HIV seroconversion, can be expected. Second, suicide does not appear to be an adverse outcome of HIV serotesting programs. While there had been fears about an increase in the number of suicides following widespread availability of HIV testing (18), this study, indirectly, and others suggest that these fears are largely unfounded (11, 19, 20).
Although we found that HIV serostatus is a weak risk factor for suicide in an overall sense, for some individuals or groups the possibility that a positive HIV status may have served as a psychosocial stressor for suicide cannot be excluded. In some demographic strata the proportion of suicide victims who were HIV positive was high. For example, for black and Hispanic men aged 35 to 54 years, one in four suicide victims was HIV positive, although the HIV seroprevalence in this demographic group in the general population is unknown. Studies of suicide among persons with AIDS have rarely found women with the disease who committed suicide, yet in this study 13% of all HIV-positive suicide victims were women. Women who are HIV positive also appeared to be at higher risk for suicide than men who are seropositive. Comparisons of our demographically specific proportions could not be made with New York City estimates, which are stratified only by gender but not by age or race/ethnicity. Thus, the relative importance of serostatus in contributing to suicide in certain sociodemographic groups clearly requires further exploration.
In recent years, several right-to-die groups have advocated that individuals with AIDS use poisoning as a means of self-inflicted death (7). We found that among suicide victims, those who were HIV positive were twice as likely to use this method as those who were HIV negative. However, more than two-thirds of HIV-positive suicide victims continue to use more violent means such as jumping from a height, hanging, firearms, and other violent methods.
How can the relatively weak association of positive HIV serostatus with suicide risk be reconciled with a much stronger association between clinical AIDS and suicide? AIDS is probably a more potent risk factor than HIV for several reasons. Compared to a serostatus conversion, AIDS is more closely linked to psychiatric illnesses that are themselves risk factors for suicide, such as depression and psychosis (21). The brain, including its serotonergic pathways that have been linked to a propensity for impulsive suicidal behaviors (22), is likely to be much more involved in AIDS through HIV encephalitis and opportunistic infections. Whereas many HIV-seropositive individuals may live for years asymptomatically, the onset of AIDS often involves a marked decline in physical functioning, including decreased mobility, chronic pain, altered sexual functioning, and disfigurement (23)—the same characteristics found in other medical illnesses that have high suicide rates (24). Other stresses of AIDS that have been linked to suicide risk, in general, include unemployment and financial losses; increased dependency on others with subsequent overburdening and dissolution of social support networks; and stigmatization, which may increase as signs of the illness become manifest (10).
The difference in suicide risk between the symptomatic and asymptomatic phases of HIV illness may resemble differences in suicide risk between these phases in other life-threatening illnesses. For example, terminal cancer carries a much higher risk for suicide than the twofold higher risk associated with a cancer diagnosis, in general (24–26). Subjects with Huntington's chorea have a suicide risk seven to 200 times that of the general population (27–29), but surveys (30, 31) of persons at risk for carrying the Huntington's gene suggest that such persons, were they to commit suicide, would do so only after disabling symptoms appeared.
Several methodologic issues warrant comment. First, not all suicide victims were autopsied and tested for HIV. However, over 80% were, and it is unlikely that those who were not would have been more likely to be HIV positive, primarily because nonscreened subjects were somewhat older and less likely to be minorities. Thus, we are reasonably confident that we are not missing a substantial number of HIV-positive suicide victims among the nonscreened cases. In addition, had nonscreened and inconclusive suicide cases been included and been considered HIV negative, the most conservative estimate of HIV seroprevalence among 1,875 cases of suicide would be 7.1%.
Second, a small but substantial minority of those who were HIV positive had AIDS-indicator conditions at autopsy and presumably were symptomatic at death. Our inclusion of these cases in overall seroprevalence figures could artifactually raise the strength of the association of an asymptomatic HIV-positive serostatus with the risk of suicide. We did not exclude this group because the exact number of individuals with AIDS can never be known with certainty in a medical examiner study in which autopsy data neither permit enumeration of T cell counts after death nor provide a complete clinical history in every case. However, even after exclusion of the individuals with known AIDS-indicator conditions, the HIV seroprevalence among suicide victims would be 7%. In addition, most, although not all, symptomatic HIV-related illnesses can be detected in the medical investigation conducted by the medical examiner or at autopsy. Thus, we are reasonably confident that most individuals who were HIV positive and committed suicide were physically asymptomatic at the time of their deaths.
Alternatively, ascertainment bias, i.e., the factors influencing the medical examiner's decision to assign a verdict of suicide, which is inherent in suicide research in general, has added prominence in studies of HIV and suicide (10). In New York City during the study period there were over 2,000 accidental deaths due to drug overdoses, most of which involved heroin and cocaine (32). It is possible that a number of individuals with drug-related deaths who were HIV positive had suicidal intent but were misclassified as accidental deaths. Thus, the HIV seroprevalence among suicide victims that we report may be an underestimate of the true prevalence among individuals whose deaths really were deliberate and self-inflicted.
Finally, we did not attempt to estimate the rates of suicide in the HIV-positive population in New York City. This would be possible only in a population-based study in which HIV serostatus is known for all subjects. Because the actual number of HIV-seropositive individuals in New York City is unknown, we had to use New York City Department of Health estimates. These estimates of HIV seroprevalence, which range from 1.4% to 3.2% for the entire New York City population, are higher than those reported for the nation, as a whole, in a study for 1993 (i.e., 0.47% range=0.46% to 0.62%) of those ages 18–59 years (17). However, New York City is known to have one of the highest case rates of AIDS among all regions of the United States (33).
In summary, of suicide victims among New York City residents, at least one in 11 was HIV seropositive, and the proportion was as high as one in four among black and Hispanic men aged 35 to 54 years. However, when these proportions are demographically adjusted and compared with seroprevalence estimates for the general New York City population, a positive HIV serostatus, in itself, is not a strong risk factor for suicide. Future studies might examine whether available new treatments such as protease inhibitors will provide a hopefulness that further reduces the risk of suicide in those infected with HIV.
 |
 |
 |
Received Feb. 7, 1997; revision received July 7, 1997; accepted July 31, 1997. From the Section of Epidemiology, Department of Psychiatry, and the Department of Public Health, Cornell University Medical College, New York; Office of Chief Medical Examiner, New York; and Department of Forensic Medicine, New York University School of Medicine, New York. Address reprint requests to Dr. Marzuk, Department of Psychiatry, Box 147, The New York Hospital-Cornell Medical Center, 525 East 68th St., New York, NY 10021. Supported by grant DA-06534 from the National Institute on Drug Abuse and by the Reader's Digest Foundation.
1. Marzuk PM, Tierney H, Tardiff K, Gross EM, Morgan EB, Hsu MA, Mann JJ: Increased risk of suicide in persons with AIDS. JAMA 1988; 259:1333–1337Google Scholar
2. Kizer KW, Green M, Perkins CI, Doebbert G, Hughes MJ: AIDS and suicide in California (letter). JAMA 1988; 260:1881Crossref, Medline, Google Scholar
3. Plott RT, Benton SD, Winslade WJ: Suicide of AIDS patients in Texas: a preliminary report. Tex Med 1989; 85:40–43Medline, Google Scholar
4. Coté TR, Biggar RJ, Dannenberg AL: Risk of suicide among persons with AIDS: a national assessment. JAMA 1992; 268:2066–2068Google Scholar
5. New York City Department of Health: Report of the Expert Panel on HIV Seroprevalence Estimates and AIDS Case Projection Methodologies. New York, Department of Health, 1989; updated December 1992 by Health Systems Agency of New York CityGoogle Scholar
6. Lemp GF, Payne SF, Neal D, Temelso T, Rutherford GW: Survival trends for patients with AIDS. JAMA 1990; 263:402–406Crossref, Medline, Google Scholar
7. Kolata G: AIDS patients seek solace in suicide but many risk added pain in failure. New York Times, June 14, 1994, p C1Google Scholar
8. Marzuk PM: Suicidal behavior and HIV illness. Int Rev Psychiatry 1991; 3:365–371Crossref, Google Scholar
9. Rajs J, Fugelstad A: Suicide related to human immunodeficiency virus infection in Stockholm. Acta Psychiatr Scand 1992; 85:234–239Crossref, Medline, Google Scholar
10. Gala C, Pergami A, Catalan J, Riccio M, Durbano F, Musicco M, Baldeweg T, Invernizzi G: Risk of deliberate self-harm and factors associated with suicidal behavior among asymptomatic individuals with HIV infection. Acta Psychiatr Scand 1992; 86:70–75Crossref, Medline, Google Scholar
11. Dannenberg AL, McNeil JG, Brundage JF, Brookmeyer R: Suicide and HIV infection: mortality follow-up of 4147 HIV-seropositive military service applicants. JAMA 1996; 276:1743–1746Google Scholar
12. Davey RT Jr, Lane HC: Laboratory methods in the diagnosis and prognostic staging of infection with human immunodeficiency virus type 1. Rev Infectious Dis 1990; 12:912–930Crossref, Medline, Google Scholar
13. Puschel K, Lieske K, Hashimoto Y, Karch H, Laufs R, Racz P, Janssen W: HIV-infection in forensic autopsy cases, in Drug Addiction and AIDS. Edited by Loimer N, Schmid R, Springer A. Vienna, Springer-Verlag, 1991, pp 89–96Google Scholar
14. 1993 revised classification system for HIV infection and expanded surveillance case definition for AIDS among adolescents and adults. MMWR Morb Mortal Wkly Rep 1992; 41(RR-17):1–19Google Scholar
15. Armitage P, Berry G: Statistical Methods in Medical Research. Oxford, England, Blackwell Scientific, 1987Google Scholar
16. Marzuk PM, Mann JJ: Suicide and substance abuse. Psychiatr Annals 1988; 18:639–645Google Scholar
17. Rosenberg PS: Scope of the AIDS epidemic in the United States. Science 1995; 270:1372–1375Google Scholar
18. Pierce C: Underscore urgency of HIV counseling. Clin Psychiatry News, Oct 1987, pp 1, 29Google Scholar
19. Perry S, Jacobsberg L, Fishman B: Suicidal ideation and HIV testing. JAMA 1990; 263:679–682Crossref, Medline, Google Scholar
20. Van Haastrecht HJA, Mientjes GHC, van den Hock AJAR, Coutinho RA: Death from suicide and overdose among drug injectors after disclosure of first HIV test result. AIDS 1994; 8:1721–1725Google Scholar
21. Perry SW: Organic mental disorders caused by HIV: update on early diagnosis and treatment. Am J Psychiatry 1990; 147:696–710Link, Google Scholar
22. Mann JJ, Stanley M (eds): Psychobiology of Suicidal Behavior. Ann NY Acad Sci 1986; 486(suppl)Google Scholar
23. Miller D, Riccio M: Nonorganic psychiatric and psychosocial syndromes associated with HIV-1 infection and disease. AIDS 1990; 4:381–388Crossref, Medline, Google Scholar
24. Marzuk PM: Suicide and terminal illness. Death Studies 1994; 18:497–512Crossref, Google Scholar
25. Fox BH, Stanek EJ, Boyd SC, Flannery ST: Suicide rates among cancer patients in Connecticut. J Chronic Dis 1982; 35:85–100Crossref, Google Scholar
26. Storm HH, Christensen N, Jensen O: Suicides among Danish patients with cancer, 1971–1986. Cancer 1992; 69:1507–1512Google Scholar
27. Dewhurst K, Oliver JE, McKnight AL: Sociopsychiatric consequences of Huntington's disease. Br J Psychiatry 1970; 116:255–258Crossref, Medline, Google Scholar
28. Farrer LA: Suicide and attempted suicide in Huntington disease: implications for preclinical testing of persons at risk. Am J Med Genet 1986; 24:305–311Crossref, Medline, Google Scholar
29. Hayden MR, Ehrlich F, Parker H, Ferera SJ: Social perspectives in Huntington's chorea. South Afr Med J 1980; 58:201–203Medline, Google Scholar
30. Kessler S: Psychiatric implications of presymptomatic testing for Huntington's disease. Am J Orthopsychiatry 1987; 57:212–219Crossref, Medline, Google Scholar
31. Mastromauro C, Myers RH, Berkman B: Attitudes toward presymptomatic testing in Huntington's disease. Am J Med Genet 1987; 26:271–282Crossref, Medline, Google Scholar
32. Tardiff K, Marzuk PM, Leon AC, Hirsch CS, Stajic M, Portera L, Hartwell N: Accidental fatal drug overdoses in New York City, 1990–1992. Am J Drug Alcohol Abuse 1996; 22:135–146Crossref, Medline, Google Scholar
33. Division of HIV/AIDS Prevention, National Center for Prevention Services, Centers for Disease Control: First 500,000 AIDS cases—United States, 1995. MMWR Morb Mortal Wkly Rep 1995; 44:849–853Medline, Google Scholar



