Maternal Suicidality and Risk of Suicidality in Offspring: Findings From a Community Study
Abstract
OBJECTIVE: This study evaluated the associations between suicidal ideation and suicide attempts in mothers and various aspects of suicidality in their offspring in a representative community sample. METHOD: Baseline and 4-year follow-up data were used from the Early Developmental Stages of Psychopathology study, a prospective, longitudinal community study of adolescents and young adults. Results are based on 933 adolescents who completed follow-up and for whom direct diagnostic information for the biological mother was available. Suicidal ideation and suicide attempts were assessed in adolescents and mothers with the Munich-Composite International Diagnostic Interview. RESULTS: Compared to offspring of mothers without suicidality, offspring of mothers reporting suicide attempts showed a remarkably higher risk for suicidal thoughts and suicide attempts and a tendency toward suicide attempts at an earlier age. Associations were comparable for male and female offspring. Transmission of maternal suicidality was roughly stable with control for maternal comorbid psychopathology. CONCLUSIONS: The offspring of mothers with suicide attempts are at a markedly increased risk for suicidality themselves and tend to manifest suicide attempts earlier than offspring of mothers without suicidality. Suicidality seems to run in families, independent of depression and other psychopathology.
A number of family studies have reported that suicidality runs in families (1–14). Although familial aggregation may not be interpreted as equivalent to genetic inheritance, results from twin and adoption studies have suggested that there may be an underlying genetic component (15–20). Previous studies further suggest that familial transmission of suicidality seems to be independent of comorbid mental disorders (5, 10–13, 16, 21–23).
However, there are some critical points. First, most of these studies included clinically referred samples. This may be crucial insofar as familial aggregation in treatment samples could be attributable to treatment bias and thus may be limited to a subgroup of severely ill patients in treatment (24). For prevention and intervention, however, it is important to demonstrate that these associations can also be found in representative community samples. Second, for completed suicide, most studies used the psychological autopsy method. Inherent to this approach is the potential recall bias of the informants. To date, only a few studies have addressed the familial transmission of suicidality in nontreatment samples (13, 21, 25, 26). Although the results of these studies support the hypothesis of familial aggregation, there is still uncertainty about the strength of the association in the community. Furthermore, no data are yet available from representative samples concerning the impact of familial suicidality on the age of the first manifestation of suicidality in offspring. Such information would be of major interest from a preventive point of view, since it allows for identifying not only high-risk groups but also high-risk periods that are risk-group specific for the first manifestation of suicidality.
The goal of this report is to increase our understanding of the familial transmission of suicidality by evaluating, based on a representative community sample, the associations between suicidal ideation and suicide attempts in mothers and various aspects of suicidality (frequency of ideation, attempts, and age at onset) in offspring.
Method
Design
Data came from the Early Developmental Stages of Psychopathology study (27, 28), a prospective longitudinal survey collecting data on the prevalence, the incidence, familial and other risk factors, comorbidity, and course of mental disorders in a representative sample of (originally) 3,021 subjects ages 14–24. The study consists of a baseline investigation and two follow-up investigations. The parents of the baseline 14–17-year-olds were additionally assessed in a separate parent survey.
Subjects
The Early Developmental Stages of Psychopathology study builds on a random population sample from the 1994 government population registries of the residents of Munich, with an age range for the sample’s subjects between 14 and 24 years (birth cohorts 1970–1981) at the time of the baseline interview in 1995. Because the study was designed with special interest in the early developmental stages of psychopathology, 14–15-year-olds were sampled at twice the rate of 16–21-year-olds, and 22–24-year-olds were sampled at half this rate. From the total of 4,809 sampled individuals, 4,263 were located and determined to be eligible for the study. From these 4,263 individuals, a total of 3,021 interviews (1,395 subjects ages 14–17, 1,626 subjects ages 18–24) were completed at baseline (response rate: 71%; 50.7% for males and 49.3% for females, all Caucasian). The rate of response for the study sample of 14–17-year-olds (the “younger cohort”) was 74.3%. Two follow-up assessments were completed after the initial baseline investigation, covering an overall period of 3–4 years. The first follow-up study (time 1) was conducted an average of 19.7 months (range=14.3–25.7) after the baseline investigation, and the second follow-up study (time 2) was conducted an average of 41.7 months (range=34.1–49.6) after the baseline investigation. The rate of response for the baseline 14–17-year-olds was 88% at the first follow-up and 84% at the second follow-up. At baseline, most of the respondents were attending school (89%) and living with their parents (98%). About 10% were in job training. The majority was classified as belonging to the middle class (61%). More details about the characteristics of the entire Early Developmental Stages of Psychopathology study sample have been presented (27, 28).
In the parent survey, direct diagnostic interviews were conducted with the parents of the younger cohort to obtain information about early development and familial psychopathology (28). Primarily, the mothers were interviewed. The fathers were interviewed only if the mother was not available (deceased or not located). The parents of 1,053 adolescents were interviewed (in 1,026 cases, the mother; in 27 cases, the father; response rate of 86%). For the current report, the study sample consisted of all adolescents who had completed the second follow-up and whose biological mothers had participated in the parent survey (N=933; 48.9% males and 51.1% females). These adolescents represent the offspring in this report.
Assessment
The adolescents and parents were assessed with the computer-assisted version of the Munich-Composite International Diagnostic Interview (29), an updated version of the World Health Organization Composite International Diagnostic Interview (30). Diagnostic findings, according to the explicit diagnostic criteria of the DSM-IV, were obtained by using the Munich-Composite International Diagnostic Interview/DSM-IV algorithms. The reliability and validity of the Munich-Composite International Diagnostic Interview and its assessment of suicidality, along with descriptions of the interview’s format and coding conventions, have been presented in detail elsewhere (31–33). Briefly, the main findings were as follows. Test-retest reliability of the Munich-Composite International Diagnostic Interview was investigated in a representative sample of community respondents ages 14–24 (N=60). The average time interval between interviews was 38.5 days. Reliability for lifetime DSM-IV diagnosis was high for most disorders (kappa values ranging from 0.56 for any eating disorder to 1.00 for panic disorder) (33). The validity of the Munich-Composite International Diagnostic Interview was investigated by comparing clinical consensus diagnoses in two samples: 104 psychiatric inpatients and outpatients of the Max Planck Institute of Psychiatry (ages 16–65) and 44 subjects from the community who were sampled as part of a pilot study. Kappa values (or Yule’s Y if the base rate was too low), taking the clinicians’ diagnoses as the gold standard, ranged from 0.50 for any somatoform disorder to 0.96 for single major depressive episode (32).
In all assessments, the Munich-Composite International Diagnostic Interview included a separate booklet that included scales and questionnaires to assess psychological constructs. All interviews were administered by highly trained clinical interviewers. Most interviews were carried out in the homes of the adolescents and parents. A detailed overview and characterization of the constructs and assessment methods have been presented (27, 34, 35). At baseline, the lifetime version of the Munich-Composite International Diagnostic Interview was used. At each of the follow-up assessments, the Munich-Composite International Diagnostic Interview’s interval version, which refers to the time period between the last interview and the present, was applied. In the analyses presented here, the complete lifetime status of the subject until time 2 was assessed from the aggregation of information obtained from baseline, time 1, and time 2 interviews.
Assessment of Suicidality
Suicidal ideation was assessed by the depression section of the Munich-Composite International Diagnostic Interview with the following questions (see references 36 and 37):
| 1. | Has there ever been a period of 2 weeks or more when you thought a lot about death—either your own, someone else’s, or death in general? | ||||
| 2. | Has there been a period of 2 weeks or more when you felt like you wanted to die? | ||||
| 3. | Have you ever felt so low that you thought about committing suicide? | ||||
| 4. | Have you ever made a plan as to how you might do it? | ||||
Suicide attempts were assessed with the question, “Have you ever attempted suicide?”
In the Munich-Composite International Diagnostic Interview depression section, only the subjects who acknowledged having had a period of at least 2 weeks with a continuously depressed mood, low energy, or loss of interest (these are the stem questions for major depression) are asked these questions. This applied for the assessment of maternal suicidality as well as to the offspring assessment at baseline and time 1. At time 2, a modification was introduced into the depression section to ensure that all adolescents were asked questions regarding suicidality in their lifetimes by skipping to these questions whenever the stem questions for major depression were denied. All subjects who reported at time 2 that they ever had attempted suicide in their lifetimes were additionally asked for the age of occurrence of the attempt. In case of several attempts, age was acquired for the first, second, and last suicide attempt.
Data Analyses
Data were weighted to adjust for differences in sampling probabilities as well as nonresponse at baseline and time 1 according to age, sex, and geographic location (27). Analyses were performed with the Stata software package (38), and the Huber-White sandwich matrix was applied for robust estimates of confidence intervals in the case of weighted data (39).
Maternal suicide status was the independent variable. Main diagnostic outcomes were the offspring’s cumulative lifetime incidences of pure suicidal ideation and suicide attempts at time 2.
Multinomial logistic regressions with odds ratios were used (40), with subjects without suicidality (i.e., no ideation and no attempts) as the reference group. Subjects with pure suicidal ideation and suicide attempts were compared to those without suicidality—in mothers and offspring, respectively.
The sex and age of the offspring were controlled for in all analyses. The sociodemographic characteristics of the mothers that were related to suicidality as well as maternal anxiety and alcohol use disorders were controlled for in additional analyses to assess to what extent they removed the associations (41). Because suicidality and depression status are confounded by construction of the Munich-Composite International Diagnostic Interview, categories of maternal suicide status were further split into those with and those without major depression. This was done to assess to what extent a diagnosis of major depression was necessary in the mothers for the mother-offspring associations of suicidality. Finally, all associations were tested for interaction with gender of the offspring.
To obtain results allowing a more straightforward interpretation than odds ratios in the risk for incident suicide attempt, we repeated the main analyses using risk ratio regressions (42, 43). For some of the more complicated models, the estimates did not converge for numerical reasons. Regarding the remaining models, the risk ratios were only slightly smaller than the odds ratios because of the low rates of suicide attempts within the groups compared. Therefore, we only reported the odds ratios that could be approximately interpreted as risk ratios here.
Age-specific cumulative lifetime incidence rates of suicide attempts were estimated with the Kaplan-Meier method (44), with age-at-onset information from the offspring. Statistical inferences were based on the stratified Cox model for discrete time (i.e., before testing for differences, different curves in strata defined by birth year cohorts and offspring’s gender are calculated nonparametrically) (44). The interaction term maternal suicide status × age was then added to the model when the proportional hazards assumption was violated (the heterogeneity of hazard ratios across the respondents’ age was tested with so-called Schoenfeld residuals) (45). This allowed us to assess whether the offspring of suicidal mothers have an earlier onset of the outcome under consideration conditional on the outcome being present. Such a model provides hazard ratios for the main effect of maternal suicidality and for the interaction effect with age. A hazard ratio <1 for the interaction term indicates an earlier onset. The age-specific hazard ratio for the difference according to maternal suicidality is given by the equation, hazard ratio (age) = hazard ratio main effect × hazard ratio interaction term to the age.
Results
Lifetime Prevalence of Suicidal Ideation and Suicide Attempts
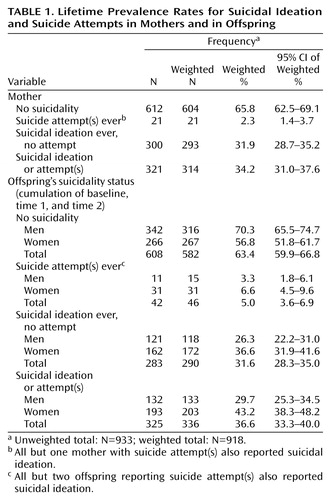
About one-third of the mothers reported lifetime suicidal ideation, whereas the rate of suicide attempts in the mothers was 2.3% (Table 1). Comparably, about one-third of the study sample of adolescents reported suicidal ideation during their lifetimes, and 5.0% reported suicide attempts. Suicidal ideation and suicide attempts were more common in female than in male offspring: suicidal ideation: 36.6% versus 26.3% (odds ratio=1.7, 95% confidence interval [CI]=1.2–2.4), suicide attempts: 6.6% versus 3.3% (odds ratio=2.5, 95% CI=1.1–5.2).
Sociodemographic Characteristics
With regard to suicide status, the mothers did not differ in age (mean age of the mothers without suicidality=46.8 years, SD=5.2; the mothers with suicidal ideation only=46.5 years, SD=5.2; and the mothers with suicide attempts=46.3 years, SD=5.8. However, differences were found regarding current living situation (with partner: 85.3% for the mothers without suicidality, 76.9% for the mothers with suicidal ideation only, and 50.1% for the mothers with suicide attempts), employment status (employed: 75.6% for the mothers without suicidality, 71.4% for the mothers with suicidal ideation only, and 77.9% for the mothers with suicide attempts), and education level (middle/higher education: 71.1% for the mothers without suicidality, 71.6% for the mothers with suicidal ideation only, and 42.2% for the mothers with suicide attempts). The offspring did not differ notably by maternal suicidality in sex (females: 50.3% among the offspring of mothers without suicidality, 53.5% among the offspring of mothers with suicidal ideation only, and 41.8% among the offspring of mothers with suicide attempts) or age distribution at the second follow-up (mean age: 18.7 years [SD=1.2] in the offspring of mothers without suicidality, 18.9 years [SD=1.2] in the offspring of mothers with suicidal ideation only, and 18.7 years [SD=1.0] in the offspring of mothers with suicide attempts).
Mother-Offspring Associations
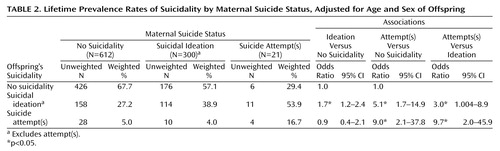
Logistic regression analyses revealed that the risk for suicidal ideation in the offspring was slightly increased if maternal suicidal ideation was present, whereas no association was found between maternal suicidal ideation and suicide attempts in their offspring (Table 2). In contrast, stronger associations were obtained when we examined the associations between suicide attempts in the mothers and suicidal ideation and suicide attempts in the offspring. The odds for suicidal ideation was about five times higher, and the odds for suicide attempts was even nine times higher in the offspring of the mothers who had ever attempted suicide compared to the offspring of the mothers without any suicidality.
Significant differences in risk were found among the offspring of the mothers with suicidal ideation and the offspring of the mothers with suicide attempts, with a higher risk among the offspring of the mothers who reported suicide attempts.
Further analyses revealed that estimates remained relatively stable after we controlled for the mothers’ sociodemographic status. The odds for suicidal ideation in the offspring of the mothers with suicidal ideation, again, was only slightly elevated (odds ratio=1.6, 95% CI=1.1–2.9) and strongly elevated in the offspring of the mothers with suicide attempts (odds ratio=4.4, 95% CI=1.4–13.7) compared with the offspring of mothers without suicidality. The adjusted odds ratio for suicide attempts in the offspring of the mothers with suicidal ideation was 0.8 (95% CI=0.3–1.7), and in the offspring of the mothers with suicide attempts, it increased to 5.4 (95% CI=1.1–26.2).
Controlling for comorbid anxiety and alcohol use disorders in the mothers yielded similar results, with the exception that the association between suicide attempts in the offspring and suicide attempt in the mothers remained only marginally significant, although the point estimate hardly changed (odds ratio=5.5, 95% CI=0.9–33.5, p=0.06).
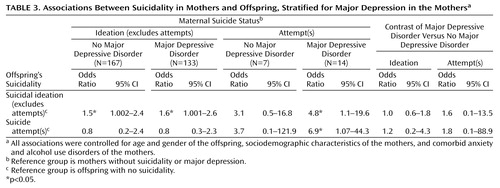
When we stratified maternal suicidal ideation and suicide attempts by maternal major depression status, no differences were found in the associations (Table 3). In the case of suicide attempts, however, the confidence intervals were so broad that nearly nothing can be ruled out.
We expanded the analyses by splitting the category “suicidal thoughts” into those who endorsed the item for suicidal plans and those who did not. There were, however, only 22 offspring and 20 mothers (unweighted) who were classified into that category, and for the combination of mothers and offspring in that category, we found no single case. Therefore, we analyzed only associations between the maternal three-category variable (no suicidality, suicidal ideas only, and suicide attempt) and the offspring four-category variable (no suicidality, suicidal ideas without plans, suicidal ideas with plans, and suicide attempt) and vice versa. The results (available on request from the first author) for the differences between suicidal thoughts with and without suicidal plans revealed no clear and statistically stable pattern. No significant interactions were found for the offspring’s sex for all associations, suggesting similar odds ratios for female and male offspring.
Maternal Suicidality and Age of Offspring’s First Suicide Attempt
Figure 1 shows the offspring’s age-specific probability for first suicide attempt by maternal suicidality status. There was a tendency toward the occurrence of a suicide attempt at an earlier age in the offspring of the mothers who attempted suicide compared to the offspring of mothers without suicidality (hazard ratio for interaction with age=0.6, 95% CI=0.3–1.0, p=0.06; hazard ratio for main effect with this model=4.8, 95% CI=1.1–20.6). No such finding was noted for the mothers who reported suicidal ideation (hazard ratio for interaction=0.9, 95% CI=0.6–1.3; hazard ratio for main effect with this model=0.9, 95% CI=0.4–1.9).
Discussion
The aim of this report was to extend our knowledge of the familial transmission of suicidality by exploring associations between maternal suicidality and suicidal behavior in their children. Notable features of the Early Developmental Stages of Psychopathology study are that 1) it is based on a representative community sample, 2) standardized symptom and diagnostic assessments of suicidal behavior were used, 3) independent diagnostic assessments of mothers and children were carried out, 4) suicidality outcomes in offspring were collected prospectively, and 5) the Early Developmental Stages of Psychopathology study was designed to collect data on a broad range of mental disorders in a representative sample of adolescents and not specifically on suicidality; thus, the questioning of suicidal behavior was embedded in the assessment of general psychopathology so that the threshold for the reporting of suicidal behavior was rather low.
Our study revealed two key findings. First, the risk for suicidal ideation, but not suicide attempts, was only slightly elevated in the presence of maternal suicidal ideation. By contrast, the risk for suicidal ideation and suicide attempts in the offspring was increased when maternal suicide attempts were present. These results are compatible with previous studies suggesting a familial aggregation of suicidality (1, 6, 7, 13, 16, 25). Beyond this confirmation, our findings indicate that different familial associations might exist for suicidal ideation and suicide attempts and that the associations cannot be attributed to differences in the sociodemographic background of the mothers. Second, control for comorbid anxiety and alcohol use disorders in the mothers yielded very similar results, suggesting that mother-offspring associations cannot be explained by maternal psychopathology associated with suicidality. Likewise, stratifying for major depression in the mothers did not reveal significant differences in associations. In confirmation with other studies (5, 13, 16, 25), these results argue for the hypothesis that familial transmission of suicidality seems to be independent of other psychopathology. Genetic mechanisms may, in part, explain the observed associations, as suggested by twin and adoption studies (16, 18–20, 46). For example, Statham et al. (16) demonstrated in a large community sample of monozygotic and dizygotic twin pairs that genetic factors accounted for almost half of the variance concerning suicidal thoughts and behavior. It has also been discussed that familial clustering may be related to impulsiveness, aggressivity, or irritability in families directed inward or outward and stable over time and generations (5, 6, 47). Such behavior seems to be strongly connected with a dysfunction of the serotonergic system (48–50). Currently, the genetic basis of this dysfunction is still unclear (51). In addition, imitation or modeling could play an important role as an explanation for parent-to-child transmission (52–54). Imitation might also explain our finding that maternal suicidal ideation was not associated with suicidal behavior in offspring because suicidal thoughts are not observable, per se, by others. However, the results of studies addressing this issue directly do not support the imitation hypothesis as an explanation for familial transmission (55).
Unlike most other studies, we additionally addressed gender-specific effects in the familial transmission of suicidality. Our findings suggest that familial risk acts similarly in males and females, confirming the findings of Qin et al. (25).
It is noteworthy that we found some indications for suicide attempts occurring at an earlier age in the offspring of the mothers who attempted suicide compared to the offspring of the mothers without suicidality. There was no such finding when the mothers reported suicidal ideation only. Recently, Brent et al. (7) reported a comparable effect specifically for the offspring of mood disorder probands. Despite the postulated continuum from suicidal ideation to suicide attempts (56), this finding provided more support for a threshold model for explaining the development of suicidal behavior in adolescents and young adults (57).
The limitations of our study include the following. First, only mothers were interviewed for the assessment of suicidality in their respective families. The availability of information about suicidality in fathers would, however, probably have resulted in higher associations, provided that the elevated risks are not specific for mothers. Second, not all adolescents had passed through the entire risk period for the onset of suicidal behavior, probably also a source of underestimation. Third, these findings apply only to the subjects followed up to the age of 21. Fourth, the study focused on suicidal ideation and suicide attempts; the extent to which the results generalize to completed suicide remains to be explored. Finally, this report focused exclusively on maternal suicidality. Clearly, the manifestation of suicidality must be seen as a complex interplay of multiple factors (12, 16, 18, 26), and maternal suicidality addresses only one of them. The investigation of the mechanisms through which maternal history of suicidality exerts its influence on offspring was beyond the scope of this report.
In conclusion, our study revealed that the offspring of mothers with suicide attempts are at a markedly increased risk for suicidality themselves. Furthermore, we found that maternal history of suicide attempts tended to predict an earlier onset of first suicide attempt in offspring. Our results provided no evidence against the hypothesis of suicidality running in families, independent of depression and other psychopathology.
Acknowledgment
This work is part of the Early Developmental Stages of Psychopathology study and is funded by the German Ministry of Research and Technology (project numbers 01 EB 9405/6 and 01 EB 9901/6) and the Deutsche Forschungsgemeinschaft (LA 1148/1-1). The principal investigators are Dr. Hans-Ulrich Wittchen and Dr. Roselind Lieb. Current or former staff members of the group are Dr. Kirsten von Sydow, Dr. Gabriele Lachner, Dr. Axel Perkonigg, Dr. Peter Schuster, Dr. Franz Gander, Dipl.-Stat. Michael Höfler, and Dipl.-Psych. Holger Sonntag, as well as Mag. Phil. Esther Beloch, Dr. Martina Fuetsch, Dipl.-Psych. Elzbieta Garczynski, Dipl.-Psych. Alexandra Holly, Dr. Barbara Isensee, Dr. Marianne Mastaler, Dr. Christopher B. Nelson, Dipl.-Inf. Hildegard Pfister, Dr. Victoria Reed, Dipl.-Psych. Andrea Schreier, Dipl.-Psych. Dilek Türk, Dipl.-Psych. Antonia Vossen, Dr. Ursula Wunderlich, and Dr. Petra Zimmermann. Scientific advisers are Dr. Jules Angst (Zurich, Switzerland), Dr. Jürgen Margraf (Basel, Switzerland), Dr. Günther Esser (Potsdam, Germany), Dr. Kathleen Merikangas (NIMH, Bethesda, Md.), Dr. Ron Kessler (Harvard, Boston), and Dr. Jim van Os (Maastricht, the Netherlands).
 |
 |
 |
Presented in part at the 22nd World Congress of the International Association for Suicide Prevention, Stockholm, Sept. 10–14, 2003. Received Jan. 22, 2004; revision received Aug. 10, 2004; accepted Nov. 8, 2004. From the Clinical Psychology and Epidemiology Department and the Clinic, Max Planck Institute of Psychiatry, Munich; and the Clinical Psychology and Psychotherapy Department, Technical University of Dresden, Dresden, Germany. Address correspondence and reprint requests to Dr. Lieb, Max Planck Institute of Psychiatry, Clinical Psychology and Epidemiology Unit, Kraepelinstr. 2, 80804 München, Germany; [email protected] (e-mail).
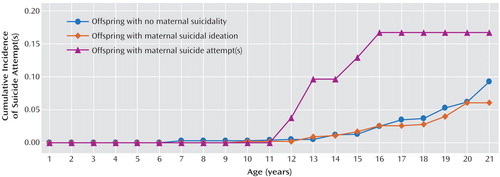
Figure 1. Age at Onset of Suicide Attempt(s) in Offspring by Maternal Suicide Status
1. Murphy GE, Wetzel RD: Family history of suicidal behavior among suicide attempters. J Nerv Ment Dis 1982; 170:86–90Crossref, Medline, Google Scholar
2. Roy A: Family history of suicide. Arch Gen Psychiatry 1983; 40:971–974Crossref, Medline, Google Scholar
3. Shafii M, Carrigan S, Whittinghill JR, Derrick A: Psychological autopsy of completed suicide in children and adolescents. Am J Psychiatry 1985; 142:1061–1064Link, Google Scholar
4. Brent DA, Perper JA, Moritz G, Liotus L, Schweers J, Balach L, Roth C: Familial risk factors for adolescent suicide: a case-control study. Acta Psychiatr Scand 1994; 89:52–58Crossref, Medline, Google Scholar
5. Brent DA, Bridge J, Johnson BA, Connolly J: Suicidal behavior runs in families: a controlled family study of adolescent suicide victims. Arch Gen Psychiatry 1996; 53:1145–1152Crossref, Medline, Google Scholar
6. Brent DA, Oquendo M, Birmaher B, Greenhill L, Kolko D, Stanley B, Zelazny J, Brodsky B, Bridge J, Ellis S, Salazar O, Mann JJ: Familial pathways to early-onset suicide attempt: risk for suicidal behavior in offspring of mood-disordered suicide attempters. Arch Gen Psychiatry 2002; 59:801–807Crossref, Medline, Google Scholar
7. Brent DA, Oquendo M, Birmaher B, Greenhill L, Kolko D, Stanley B, Zelazny J, Brodsky B, Firinciogullari S, Ellis SP, Mann JJ: Peripubertal suicide attempts in offspring of suicide attempters with siblings concordant for suicidal behavior. Am J Psychiatry 2003; 160:1486–1493Link, Google Scholar
8. Pfeffer CR, Normandin L, Kakuma T: Suicidal children grown up: suicidal behavior and psychiatric disorders among relatives. J Am Acad Child Adolesc Psychiatry 1994; 33:1087–1097Crossref, Medline, Google Scholar
9. Malone KM, Haas GL, Sweeney JA, Mann JJ: Major depression and the risk of attempted suicide. J Affect Disord 1995; 34:173–185Crossref, Medline, Google Scholar
10. Gould MS, Fisher P, Parides M, Flory M, Shaffer D: Psychosocial risk factors of child and adolescent completed suicide. Arch Gen Psychiatry 1996; 53:1155–1162Crossref, Medline, Google Scholar
11. Johnson BA, Brent DA, Bridge J, Connolly J: The familial aggregation of adolescent suicide attempts. Acta Psychiatr Scand 1998; 97:18–24Crossref, Medline, Google Scholar
12. Cheng ATA, Chen TH, Chen C-C, Jenkins R: Psychosocial and psychiatric risk factors for suicide. Br J Psychiatry 2000; 177:360–365Crossref, Medline, Google Scholar
13. Runeson B, Åsberg M: Family history of suicide among suicide victims. Am J Psychiatry 2003; 160:1525–1526Link, Google Scholar
14. Roy A, Segal NL: Suicidal behavior in twins: a replication. J Affect Disord 2001; 66:71–74Crossref, Medline, Google Scholar
15. Roy A, Segal NL, Centerwall BS, Robinette DC: Suicide in twins. Arch Gen Psychiatry 1991; 48:29–32Crossref, Medline, Google Scholar
16. Statham DJ, Heath AC, Madden PAF, Bucholz KK, Bierut L, Dinwiddie SH, Slutske WS, Dunne MP, Martin NG: Suicidal behaviour: an epidemiological and genetic study. Psychol Med 1998; 28:839–855Crossref, Medline, Google Scholar
17. Glowinski AL, Bucholz KK, Nelson EC, Fu Q, Madden PAF, Reich W, Heath AC: Suicide attempts in an adolescent female twin sample. J Am Acad Child Adolesc Psychiatry 2001; 40:1300–1307Crossref, Medline, Google Scholar
18. Fu Q, Heath AC, Bucholz KK, Nelson EC, Glowinski AL, Goldberg J, Lyons MJ, Tsuang MD, Jacob T, True MR, Eisen SA: A twin study of genetic and environmental influences on suicidality in men. Psychol Med 2002; 32:11–24Crossref, Medline, Google Scholar
19. Schulsinger F, Kety SS, Rosenthal D, Wender PH: A family study of suicide, in Origin, Prevention and Treatment of Affective Disorders. Edited by Schou M, Strömgren E. London, Academic Press, 1979, pp 277–287Google Scholar
20. Wender PH, Kety SS, Rosenthal D, Schulsinger F, Ortmann J, Lunde L: Psychiatric disorders in the biological and adoptive families of adopted individuals with affective disorders. Arch Gen Psychiatry 1986; 43:923–929Crossref, Medline, Google Scholar
21. Bridge JA, Brent DA, Johnson BA, Connolly J: Familial aggregation of psychiatric disorders in a community sample of adolescents. J Am Acad Child Adolesc Psychiatry 1997; 36:628–636Crossref, Medline, Google Scholar
22. Powell JJ, Geddes J, Deeks J, Goldacre M, Hawton K: Suicide in psychiatric hospital in-patients: risk factors and their predictive power. Br J Psychiatry 2000; 176:266–272Crossref, Medline, Google Scholar
23. Mann JJ, Waternaux C, Haas GL, Malone KM: Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry 1999; 156:181–189Abstract, Google Scholar
24. Kendler KS: Is seeking treatment for depression predicted by a history of depression in relatives? implications for family studies of affective disorder. Psychol Med 1995; 25:807–814Crossref, Medline, Google Scholar
25. Qin P, Agerbo E, Mortensen PB: Suicide risk in relation to family history of completed suicide and psychiatric disorders: a nested case-control study based on longitudinal registers. Lancet 2002; 360:1126–1130Crossref, Medline, Google Scholar
26. Fergusson DM, Beautrais AL, Horwood LJ: Vulnerability and resilience to suicidal behaviours in young people. Psychol Med 2003; 33:61–73Crossref, Medline, Google Scholar
27. Wittchen H-U, Perkonigg A, Lachner G, Nelson CB: Early Developmental Stages of Psychopathology study (EDSP). Eur Addict Res 1998; 4:18–27Crossref, Medline, Google Scholar
28. Lieb R, Isensee B, von Sydow K, Wittchen H-U: The Early Developmental Stages of Psychopathology study (EDSP): a methodological update. Eur Addict Res 2000; 6:170–182Crossref, Medline, Google Scholar
29. Wittchen H-U, Pfister H: DIA-X Interviews. Frankfurt, Germany, Swets-Zeitlinger, 1997Google Scholar
30. World Health Organization: Composite International Diagnostic Interview (CIDI), version 1.0. Geneva, WHO, 1990Google Scholar
31. Lachner G, Wittchen H-U, Perkonigg A, Holly A, Schuster P, Wunderlich U, Türk D, Garczynski E, Pfister H: Structure, content and reliability of the Munich-Composite International Diagnostic Interview (M-CIDI) substance use sections. Eur Addict Res 1998; 4:28–41Crossref, Medline, Google Scholar
32. Reed V, Gander F, Pfister H, Steiger A, Sonntag H, Trenkwalder C, Hundt W, Wittchen H-U: To what degree does the Composite International Diagnostic Interview (CIDI) correctly identify DSM-IV disorders? testing validity issues in a clinical sample. Int J Methods Psychiatr Res 1998; 7:142–155Crossref, Google Scholar
33. Wittchen H-U, Lachner G, Wunderlich U, Pfister H: Test-retest reliability of the computerized DSM-IV version of the Munich-Composite International Diagnostic Interview (M-CIDI). Soc Psychiatry Psychiatr Epidemiol 1998; 33:568–578Crossref, Medline, Google Scholar
34. Höfler M, Lieb R, Perkonigg A, Schuster P, Sonntag, H, Wittchen H-U: Covariates of cannabis use progression in a representative population sample of adolescents: a prospective examination of vulnerability and risk factors. Addiction 1999; 94:1679–1694Crossref, Medline, Google Scholar
35. Wittchen H-U, Lieb R, Schuster P, Oldehinkel T: When is onset? investigations into early developmental stages of anxiety and depressive disorders, in Childhood Onset of “Adult” Psychopathology: Clinical and Research Advances. Edited by Rapoport JL. Washington, DC, American Psychiatric Press, 1999, pp 259–302Google Scholar
36. Wunderlich U, Bronisch T, Wittchen H-U: Comorbidity patterns in adolescents and young adults with suicide attempts. Eur Arch Psychiatry Clin Neurosci 1998; 248:87–95Crossref, Medline, Google Scholar
37. Wunderlich U, Bronisch T, Wittchen H-U, Carter R: Gender differences in adolescents and young adults with suicidal behaviour. Acta Psychiatr Scand 2001; 104:332–339Crossref, Medline, Google Scholar
38. Stata Reference Manual: Release 8.0. College Station, Tex, Stata Corp, 2003Google Scholar
39. Royall RM: Model robust confidence intervals using maximum likelihood estimators. Int Stat Rev 1986; 54:221–226Crossref, Google Scholar
40. McCullagh P, Nelder JA: Generalized Linear Models, 2nd ed. New York, Chapman & Hall, 1989Google Scholar
41. Bronisch T, Wittchen H-U: Suicidal ideation and suicide attempts: comorbidity with depression, anxiety disorders, and substance use disorder. Eur Arch Psychiatry Clin Neurosci 1994; 244:93–98Crossref, Medline, Google Scholar
42. Wacholder S: Binomial regression in GLIM: estimating risk ratios and risk differences. Am J Epidemiol 1986; 123:174–184Crossref, Medline, Google Scholar
43. Greenland S: Additive risk vs additive relative risk models. Epidemiology 1993; 4:32–36Crossref, Medline, Google Scholar
44. Andersen PK, Keiding N: Survival analysis, in Advances in Biometry:50 Years of the International Biometric Society. Edited by Armitage P, David HA. New York, John Wiley & Sons,1996, pp 177–200Google Scholar
45. Grambsch TM, Thernau PM: Proportional hazard tests and diagnostics based on weighted residuals. Biometrika 1994; 81:515–526Crossref, Google Scholar
46. Roy A, Segal NL, Sarchiapone M: Attempted suicide among living co-twins of twin suicide victims. Am J Psychiatry 1995; 152:1075–1076Link, Google Scholar
47. Huesmann LR, Eron LD, Lefkowitz MM, Walder LO: Stability of aggression over time and generations. Dev Psychol 1984; 20:1120–1134Crossref, Google Scholar
48. Mann JJ: The neurobiology of suicide. Nat Med 1998; 4:25–30Crossref, Medline, Google Scholar
49. Mann JJ, Brent DA, Arango V: The neurobiology and genetics of suicide and attempted suicide: a focus on the serotonergic system. Neuropsychopharmacology 2001; 24:467–477Crossref, Medline, Google Scholar
50. Davidson RJ, Putnam KM, Larson CL: Dysfunction in the neural circuitry of emotion regulation—a possible prelude in violence. Science 2000; 289:591–594Crossref, Medline, Google Scholar
51. Arango V, Huang Y, Underwood MD, Mann JJ: Genetics of the serotonergic system in suicidal behavior. J Psychiatr Res 2003; 37:375–386Crossref, Medline, Google Scholar
52. Bandura A, Mischel W: Modification of self-imposed delay of reward through exposure to life and symbolic models. J Pers Soc Psychol 1965; 2:698–705Crossref, Medline, Google Scholar
53. Bandura A: Social learning theory of aggression. J Commun 1978; 28:12–29Crossref, Medline, Google Scholar
54. Schmidtke A, Schaller S: The role of mass media in suicide prevention, in The International Handbook of Suicide and Attempted Suicide. Edited by Hawton K, van Heeringen K. Chichester, UK, John Wiley & Sons, 2000, pp 675–697Google Scholar
55. Brent DA, Moritz G, Bridge J, Perper J, Canobbio R: Long-term impact of exposure to suicide: a three year controlled follow-up. J Am Acad Child Adolesc Psychiatry 1996; 35:646–653Crossref, Medline, Google Scholar
56. Fergusson DM, Lynskey MT: Suicide attempts and suicidal ideation in a birth cohort of 16-year-old New Zealanders. J Am Acad Child Adolesc Psychiatry 1995; 34:1308–1317Crossref, Medline, Google Scholar
57. Bronisch T: The relationship between suicidality and depression. Arch Suicide Res 1996; 2:235–254Crossref, Google Scholar



