Peripubertal Suicide Attempts in Offspring of Suicide Attempters With Siblings Concordant for Suicidal Behavior
Abstract
OBJECTIVE: The authors sought to determine 1) whether the risk for familial transmission of suicidal behavior is greater with increased family loading for suicide attempts, and 2) whether the transmission of suicidal behavior is mediated by impulsive aggression. METHOD: A reanalysis of a high-risk study compared the offspring of three mood disorder proband groups: suicide attempters with a sibling who also attempted suicide (N=19), suicide attempters whose siblings never made a suicide attempt (N=73), and nonsuicidal probands whose siblings also never engaged in suicidal behavior (N=73). Probands and offspring were assessed with respect to psychopathology, suicide attempt history, impulsive aggression, and exposure to familial adversity. RESULTS: Offspring of suicide attempters with siblings concordant for suicidal behavior showed a higher risk of suicide attempt than did offspring of nonsuicidal probands and had an earlier age at onset of suicidal behavior than offspring of suicide attempters with siblings discordant for suicidal behavior. Probands from sibling pairs concordant for suicidal behavior and their offspring reported greater lifetime impulsive aggression compared with each of the other two proband/offspring groups. In the offspring, impulsive aggression was the most powerful predictor of early age at first suicide attempt. CONCLUSIONS: Familial loading for suicide attempts may affect rates of transmission as well as age at onset of suicidal behavior, and its effect may be mediated by the familial transmission of impulsive aggression.
Suicide and suicidal behavior are familial. Adoption, twin, and family studies have shown that first-degree relatives of suicide victims and attempters are at higher risk for suicidal behavior (1). While the familial transmission of suicidal behavior is partly mediated by the transmission of psychiatric disorders (2, 3), there is up to a 4–6-fold greater risk of suicidal behavior in first-degree relatives of suicide attempters or completers even after controlling for the familial transmission of psychiatric disorder (2–13). Impulsive aggressive traits appear to be part of a diathesis for suicidal behavior and may mediate the familial transmission of suicidal behavior (8, 9, 12, 14, 15).
We recently demonstrated familial transmission of suicidal behavior in the offspring of mood disorder probands who attempted suicide (16). The familial transmission of suicidal behavior was related, in part, to the familial transmission of sexual abuse and of impulsive aggression. In this report, we extend our findings of familial transmission of suicidal behavior by examining the relationship between family loading for suicidal behavior and familial transmission of suicidal behavior. We compared three proband groups, all adults with a history of a mood disorder separated on the basis of suicide attempt history and family loading for suicidal behavior: 1) suicide attempters with a sibling who also attempted suicide, 2) suicide attempters whose siblings never made a suicide attempt, and 3) nonsuicidal probands whose siblings also never engaged in suicidal behavior. We posited that the offspring of parents with the greatest loading for suicidal behavior would have the highest morbid risk for familial transmission of suicidal behavior and that the familial transmission of suicidal behavior would be mediated partly by higher impulsive aggression in probands and offspring.
Method
Subjects
The study group consisted of nonpsychotic mood disorder probands who had or had not attempted suicide and their offspring. Subjects with mood disorder secondary to substance abuse or medical illness were excluded. Suicide attempt was defined as a self-destructive act with at least some intent to die. Attempters had made an attempt that resulted in at least moderate medical damage requiring medical attention according to the Medical Damage or Lethality Rating Scale (17). Nonattempters had no lifetime history of suicide attempt. The subjects were a consecutive study group recruited from inpatient units in New York (New York State Psychiatric Institute and Payne Whitney Clinic) and Pittsburgh (Western Psychiatric Institute and Clinic and St. Francis Hospital). A previous study reported on 299 offspring of 136 probands (18). The rates of agreement to participate in this study for probands and offspring were 86% and 88%, respectively. This project was approved by and conducted in accordance with the institutional review boards of the University of Pittsburgh and the New York State Psychiatric Institute/Columbia University Department of Psychiatry. Adult subjects were recruited after the procedures were fully explained and written informed consent was obtained. Children were recruited after their written assent and written consent from parents were obtained.
Probands were divided into three groups, stratified on the basis of family loading for suicide attempts in the proband generation: suicide attempters with siblings concordant for suicidal behavior, suicide attempters with siblings discordant for suicidal behavior, and nonsuicidal probands whose siblings also had never attempted suicide. Probands who had no siblings (N=13) and nonsuicidal probands who had a sibling who attempted or completed suicide (N=2) were excluded from these analyses. At a follow-up evaluation, five nonsuicidal probands were subsequently found to have attempted suicide. None of these five subjects had siblings concordant for suicidal behavior. Analyses conducted with these five subjects reclassified did not change the results; therefore we report the data with subjects based on their classification at intake into the study.
Assessment
All subjects over age 18 were assessed for the presence of lifetime and current DSM-IV psychiatric disorders with the Structured Clinical Interview for DSM-IV (SCID-I) (15, 19). Biological co-parents not directly interviewed were assessed with the Family History Research Diagnostic Criteria (20)—modified to reflect DSM-IV criteria—reported by either the proband or another biological relative (20). Offspring between the ages of 10–17 years were assessed regarding axis I disorders with the Schedule for Affective Disorders and Schizophrenia for School-Age Children—Present and Lifetime Version (K-SADS-PL) (21). History of suicidal behavior was assessed with the Columbia University Suicide History Form, the Medical Damage Lethality Rating Scale, and the Beck Suicide Intent Scale for the current and most severe attempts in probands and in all offspring 10 and older (17, 22). Personality disorders were diagnosed with the Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II) (23) for all subjects over age 14. Aggression was rated in all subjects with the 11-item Brown-Goodwin Lifetime History of Aggression (24). Impulsive aggression was assessed by the Buss-Durkee Hostility Inventory (25) in all subjects over age 14. In youth aged 10–13, the downward extension of the Buss-Durkee Hostility Inventory, the Children’s Hostility Inventory (26) was used. In subjects over 18 years of age, impulsivity was assessed with the Barratt Impulsivity Scale (27). In subjects aged 10–17 years, the 5-item impulsivity subscale of the Iowa Conners Parent Physical Report (28) was used. In subjects over age 18, physical and sexual abuse history were assessed by using a series of screening questions from our demographic questionnaire and from the posttraumatic stress disorder (PTSD) section of the SCID-I. Reliability of a self-report questionnaire (29) with the initial assessment was moderate for physical abuse (kappa=0.41, SE=0.11) and high for sexual abuse (kappa=0.74, SE=0.11). For youth age 10–17, a history of physical and sexual abuse was assessed by using the Psychosocial Schedule (30), an interview with the parent and child about home and family environment.
Diagnostic Procedure
All interviewers were at least master’s-level clinicians or psychiatric nurses who received extensive training in the administration of semistructured interviews. Assessments of offspring and of probands were conducted blind to each other. Best-estimate diagnoses were made by consensus and used all available data sources in diagnostic consensus conferences. Discrepancies between informants were resolved by reinterview of both informants until consensus could be obtained. Within and cross-site reliability on the SCID-I and SCID-II, K-SADS-PL, suicide history, and the Brown-Goodwin Lifetime History of Aggression were high (intraclass correlation coefficients=0.82–0.98, kappas=0.86–0.95).
Data Analysis
The data from the two sites were pooled, since there were no site-by-risk factor-by-familial transmission interactions. Differences between the three proband and offspring groups were compared by using chi-square and t tests. Lethality, intent, age at onset of mood disorder, and age at onset of suicidal behavior were compared in probands and offspring by using t tests and appropriate nonparametric tests. Logistic regression was used to identify the most parsimonious set of variables that 1) differentiated sibling-concordant and sibling-discordant suicide attempters and their offspring and 2) was related to familial transmission of suicide attempt. The morbid risk and time to first attempt were compared among the offspring of the three groups by using Kaplan-Meier estimates and by Cox regression, with baseline differences between groups entered as covariates.
Results
Comparison of Proband Groups
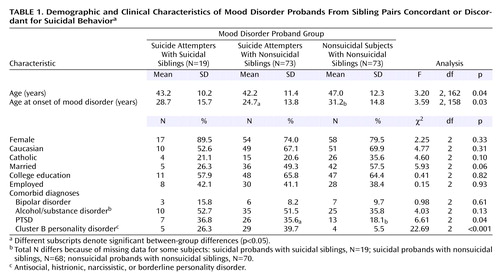
The probands were in their mid-40s and mostly female (Table 1). All three groups had an age at onset of mood disorder around the age of 30. Pairwise comparison showed that age at onset was younger in the suicidal probands with nonsuicidal siblings than in the nonsuicidal probands. The rate of bipolar disorder or comorbid alcohol/substance abuse did not differ in the three groups. Both suicide attempter groups had higher rates of PTSD and cluster B personality disorders than did the nonsuicidal probands.
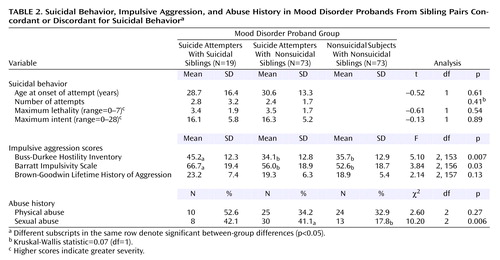
As hypothesized, suicidal probands with siblings concordant for suicidal behavior showed higher levels of impulsivity on the Barratt Impulsivity Scale and higher levels of impulsive aggression on the Buss-Durkee Hostility Inventory than each of the other proband groups (Table 2). A reported history of sexual abuse was more common in both suicide attempter proband groups compared with the nonsuicidal probands. There were no group differences for physical abuse.
The prevalence of suicidal behavior among first-degree relatives of the three proband groups appeared to be highest in the suicide attempters with siblings concordant for suicidal behavior (10%, compared with 3% and 6% in the suicide attempters with siblings discordant for suicidal behavior and nonsuicidal probands, respectively). The difference, however, was not significant (p=0.14, Fisher’s exact test).
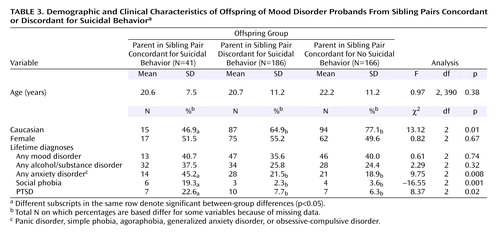
Comparison of Offspring
All subjects in the offspring groups were in late adolescence at the time of evaluation (Table 3). The offspring of probands in the two suicide attempter groups were less likely to be Caucasian. The three groups had similar rates of mood disorders and alcohol/substance abuse but different rates of anxiety, social phobia, and PTSD. Post hoc comparisons showed higher rates of anxiety, social phobia, and PTSD in the offspring of suicide attempters with siblings concordant for suicidal behavior than offspring of the other two proband groups.
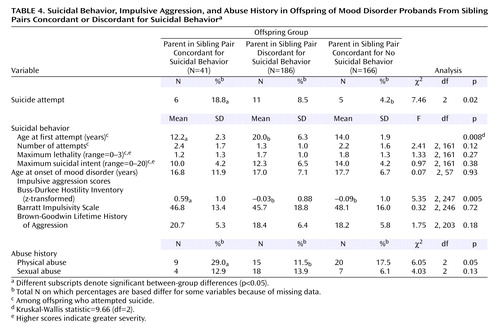
The rates of suicide attempts were different across the three offspring groups, with a significant pairwise difference between offspring of sibling-concordant suicidal probands versus offspring of sibling-discordant suicidal probands (18.8% versus 4.2%) (χ2=7.90, df=1, p=0.005) (Table 4). The morbid risk for suicide attempt was similar in the offspring of the two suicide attempter groups (mean=0.18 [SE=0.07] and 0.20 [SE=0.06]), but the age at first suicide attempt was about 8 years earlier in the offspring of sibling-concordant versus sibling-discordant suicidal probands (generalized Wilcoxon χ2=6.27, df=1, p=0.01). The morbid risk of attempt was much greater in the offspring of sibling-concordant suicide attempters than in the offspring of nonsuicidal probands (mean=0.18 [SE=0.07] versus 0.05 [SE=0.02], respectively) (Wilcoxon χ2=7.46, df=1, p=0.006) (Figure 1). However, there was no significant difference in the age at onset of suicidal behavior for offspring of sibling-concordant suicide attempters versus offspring of nonsuicidal probands (Mann-Whitney U=6.5, p=0.51). Suicide attempt followed onset of the mood disorder by a median of 1 year (mean=0.33, SD=5.0) in offspring of sibling-concordant suicide attempters, 2 years (mean=5.0, SD=7.6) in the offspring of sibling-discordant suicide attempters, and 1.5 years (mean=0.5, SD=2.3) in the offspring of nonsuicidal probands.
The ages at first suicide attempt and onset of mood disorders were earlier in the offspring than in probands (Mann-Whitney U=31.50, p=0.003; Mann Whitney U=285.0, p=0.02). Neither lethality nor number of lifetime suicide attempts differentiated offspring of sibling-concordant suicide attempters from offspring of sibling-discordant suicide attempters. However, the maximum medical damage and suicide intent were lower in the offspring than in the proband parents (medical damage: t=4.57, df=107, p<0.0001; suicide intent: t=3.37, df=107, p=0.0005).
Suicidal probands with siblings concordant for suicidal behavior appeared to be more likely to have at least one sibling with a mood disorder (58%) than suicidal probands with nonsuicidal siblings (36%) and nonsuicidal probands (29%), although this was not statistically significant (χ2=5.6, df=2, p=0.06). In addition, the sibling pairs concordant for suicidal behavior were more likely to have at least one first-degree relative with a mood disorder (89% versus 45% versus 51%) (χ2=12.1, df=2, p=0.002).
Offspring of probands in sibling pairs concordant for suicidal behavior had higher levels of impulsive aggression than did the other two offspring groups. There were no group differences in impulsivity on either the Barratt Impulsivity Scale or the Conners impulsivity subscale. There were no differences in the rates of reported childhood sexual abuse among the three groups, but the rates of reported physical abuse were higher in the offspring of sibling-concordant suicidal probands than sibling-discordant suicidal probands.
Logistic and Cox Regressions
Proband and offspring variables that differentiated the sibling-concordant suicide attempter group from the other two groups were entered into a logistic regression. Only offspring impulsive aggression survived this logistic regression (odds ratio=2.0, 95% confidence interval [CI]=1.0–4.0; Wald χ2=4.12, df=1, p=0.04). Offspring impulsive aggression and proband concordance status were entered into a Cox regression predicting age at first offspring suicide attempt. Only offspring impulsive aggression was significant (odds ratio=2.2, 95% CI=1.3–3.8; Wald χ2=8.85, df=1, p=0.003), whereas proband concordance status, which was significantly associated with offspring attempt in the univariate analysis (odds ratio=2.9, 95% CI=1.1–7.3; Wald χ2=4.78, df=1, p<0.03), now escaped statistical significance (odds ratio=2.1, 95% CI=0.8–6.1; Wald χ2=1.77, df=1, p=0.18). This supports our hypothesis of impulsive aggression mediating the relationship between sibling-pair concordance for suicide attempt status and early-onset offspring suicide attempt.
Discussion
In this study, we found that greater familial loading for suicidal behavior in the proband generation was associated with 1) a greater risk of suicidal behavior and earlier age at first suicide attempt in offspring as well as 2) greater impulsive aggression in both parents and offspring. Offspring impulsive aggression was related to risk for suicide attempt and earlier age at first attempt. The seriousness of the suicidal behavior, as measured by lethality and number of attempts, was similar in the offspring of sibling-concordant and sibling-discordant suicidal probands. Offspring were younger at the time of their first suicide attempt and first episode of major mood disorder than their proband parents and had lower intent and lethality of suicidal behavior.
Greater familial loading for suicidal behavior was associated with a higher risk of suicide attempt among offspring. Offspring of suicide attempters with a sibling concordant for suicidal behavior were at highest risk for suicide attempt, offspring of suicide attempters with nonsuicidal siblings were intermediate, and offspring of nonsuicidal probands had the lowest risk for attempt. This dose-response relationship between familial loading for suicidal behavior and risk for offspring attempt further supports the conclusion that suicidal behavior is familially transmitted (2–18).
Familial loading for suicidal behavior was also associated with earlier age at onset of suicidal behavior. Specifically, the offspring of sibling-concordant suicide attempters showed the earliest age at onset of suicidal behavior—a full 8 years on average before the first suicide attempt by offspring of suicide attempters with nonsuicidal siblings. However, the few offspring of nonsuicidal probands who made suicide attempts also had their first attempt at a relatively early age. Thus, there are other explanations for early age at first suicide attempt besides familial loading for suicidal behavior.
The single most powerful predictor for familial transmission of suicidal behavior and of early first attempt in offspring was impulsive aggression in offspring. Impulsive aggression was highest in the suicide attempters with siblings concordant for suicidal behavior and in their offspring. Thus, it is likely that familial transmission of early-onset suicidal behavior is related to the transmission of impulsive aggression. Previous studies have shown a relationship between impulsive aggression in probands and families and familial loading for suicidal behavior (1, 8, 9, 12, 14, 16, 31). Impulsive aggression has been consistently implicated in the phenomenology and neurobiology of suicidal behavior (1, 32). However, there are multiple pathways to impulsive aggression and to early-onset suicidal behavior, such as by a history of sexual or physical abuse (33). The offspring of the nonsuicidal probands who themselves attempted suicide had a particularly high rate of physical or sexual abuse (three of five subjects), which might have accounted for their early first suicide attempt, as has been reported in other studies (33–35).
Since mood disorder preceded suicide attempt in offspring, factors that lead to an earlier age at onset of mood disorder might thereby lower the age at first suicide attempt. Familial loading for mood disorders is related to earlier age at onset of mood disorder (36). The sibling-concordant suicide attempter group did have the highest loading of mood disorder in proband first-degree relatives, but this did not account for an earlier age at first suicide attempt in offspring. This may be because the familial loading for mood disorder was already so high in all three proband groups.
We have identified factors related to predicting early onset of mood disorder (unpublished 2002 study of D. Brent et al.), namely impulsive aggression in offspring, physical abuse in offspring, and offspring comorbid anxiety. Impulsive aggression predicts early onset of both mood disorder and suicidal behavior. Thus, transmission of impulsive aggression may influence onset of suicidal acts by increasing the propensity to act on powerful feelings and by earlier onset of a major depressive episode.
Comorbid anxiety was more common in the offspring of the sibling-concordant suicide attempters. However, after impulsive aggression was controlled, anxiety did not predict earlier age at first suicide attempt. Anxiety disorders are often a precursor of mood disorders and in our study may herald the onset of major depression, which in turn leads to suicidal acts (37–39).
In our previous report, we found that the familial transmission of suicidal behavior was mediated by the familial transmission of sexual abuse (16). However, there were no differences in the rates of sexual abuse between either the sibling-concordant and sibling-discordant suicide attempters or their respective offspring groups. There was a higher rate of physical abuse in the offspring of sibling-concordant suicide attempters, but in this study group, physical abuse was not related to the familial transmission of suicide attempt. Other studies have recognized the deleterious effects of physical abuse but also find that a suicide attempt history is more closely related to sexual rather than physical abuse (40). Thus, the earlier age at onset of suicidal behavior in offspring of sibling-concordant suicidal probands was not related to a history of abuse in the probands or the offspring but was related to the severity of impulsive aggressive traits in the offspring. However, other studies have reported a relationship between sexual abuse and early onset of suicidal behavior and with impulsive aggression (33–35, 41).
The age at first suicide attempt was much earlier in the offspring than in probands, and the maximum lethality and intent were much lower in the offspring than in probands. This could be an artifact of recall bias, in which probands have failed to accurately recall their earlier, less serious suicide attempts. Alternatively, the offspring of attempters may have greater familial loading for suicidal behavior than their parents and consequently have an earlier age at first attempt. Offspring of both suicide attempter groups had first attempts of similarly low intent and lethality, despite the older age at onset in the offspring of the sibling-discordant suicidal probands. Suicidal behavior may begin early in life with relatively low intent and lethality and increase in crescendo-like fashion with age. This is consistent with studies that have compared older and younger suicidal subjects as well as studies that have followed suicide attempters longitudinally (42–46).
These results support the utility of collecting concordant sibling pairs for the genetic study of suicidal behavior as well as for the role of impulsive aggression as an “endophenotype” for suicidal behavior. Future studies that examine siblings concordant for suicide attempts may shed light on the genetics of suicidal behavior and of impulsive aggression.
This study should be viewed in the context of its limitations. Most of the probands and offspring who attempted suicide were female, so this study is most informative about female-to-female transmission of suicidal behavior. The proband group was restricted to those with mood disorders, particularly major depressive disorder, which has the benefit of increasing homogeneity but therefore does not address the familial transmission of suicidal behavior in the context of other psychiatric disorders, including bipolar disorder. The probands were recruited from inpatient facilities, where the disorders are more severe rather than representative. While a sibling-concordant suicide attempt group implies greater family-genetic loading for suicidal behavior, a greater risk of suicidal behavior in the proband generation could be due to a shared adverse family environment, such as abuse or neglect. Additionally, the familial transmission of suicidal behavior could be explained by imitation. Previous studies of twins and of parent-child pairs have looked at the wide variability between the twins of relative attempts and concluded that imitation is not a major explanation of the familial transmission of suicidal behavior (18). Nevertheless, even within the context of these limitations, our results are consistent with findings from both referred and nonreferred patient groups and support further investigation of genetic traits related to suicidal behavior.
The strikingly early age at onset of suicidal behavior in the offspring of mood disordered suicide attempters with siblings concordant for suicidal behavior suggests risk factors that can be targets of early prevention. Replication of this study and early treatment and prevention studies are the next steps.
 |
 |
 |
 |
Received Sept. 26, 2002; revision received Jan. 8, 2003; accepted Jan. 21, 2003. From the Western Psychiatric Institute and Clinic, Pittsburgh; and the New York State Psychiatric Institute, New York. Reprints are not available. Address correspondence to Dr. Brent, Western Psychiatric Institute and Clinic, 3811 O’Hara St., Suite 112, Pittsburgh, PA 15213; [email protected] (e-mail). Supported by NIMH grants MH-56612, MH-56390, MH-55123, and MH-62185. The authors thank Ms. Stephanie Costa for manuscript preparation and Dr. Satish Iyengar for statistical consultation.
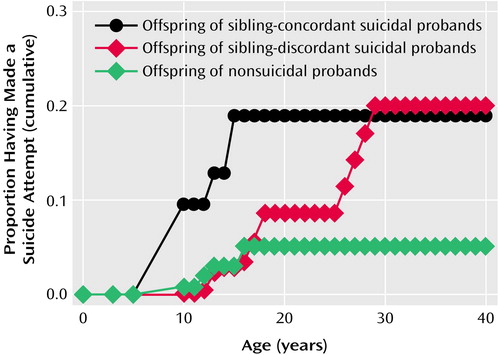
Figure 1. Suicide Attempts Over Time Among Offspring of Mood Disorder Probands From Sibling Pairs Concordant or Discordant for Suicidal Behavior
1. Mann JJ, Brent DA, Arango V: The neurobiology and genetics of suicide and attempted suicide: a focus on the serotonergic system. Neuropsychopharmacology 2001; 24:467–477Crossref, Medline, Google Scholar
2. Egeland JA, Sussex JN: Suicide and family loading for affective disorders. JAMA 1985; 254:915–918Crossref, Medline, Google Scholar
3. Wender PH, Kety SS, Rosenthal D, Schulsinger F, Ortmann J, Lunde I: Psychiatric disorders in the biological and adoptive families of adopted individuals with affective disorders. Arch Gen Psychiatry 1986; 43:923–929Crossref, Medline, Google Scholar
4. Schulsinger F, Kety SS, Rosenthal D, Wender PH: A family study of suicide, in Origin, Prevention and Treatment of Affective Disorders. Edited by Schou M, Stromgren E. London, Academic Press, 1979, pp 277–287Google Scholar
5. Roy A: Family history of suicide. Arch Gen Psychiatry 1983; 40:971–974Crossref, Medline, Google Scholar
6. Roy A, Segal NL, Centerwall BS, Robinette D: Suicide in twins. Arch Gen Psychiatry 1991; 48:29–32Crossref, Medline, Google Scholar
7. Malone KM, Haas GL, Sweeney JA, Mann JJ: Major depression and the risk of attempted suicide. J Affect Disord 1995; 34:173–185Crossref, Medline, Google Scholar
8. Garfinkel BD, Froese A, Hood J: Suicide attempts in children and adolescents. Am J Psychiatry 1982; 139:1257–1261Link, Google Scholar
9. Linkowski P, de Maertelaer V, Mendlewicz J: Suicidal behaviour in major depressive illness. Acta Psychiatr Scand 1985; 72:233–238Crossref, Medline, Google Scholar
10. Tsuang MT: Risk of suicide in the relatives of schizophrenics, manics, depressives, and controls. J Clin Psychiatry 1983; 44:396–400Medline, Google Scholar
11. Cheng AT, Chen THH, Chen CC, Jenkins R: Psychosocial and psychiatric risk factors for suicide: case-control psychological autopsy study. Br J Psychiatry 2000; 177:360–365Crossref, Medline, Google Scholar
12. Brent DA, Bridge J, Johnson BA, Connolly J: Suicidal behavior runs in families: a controlled family study of adolescent suicide victims. Arch Gen Psychiatry 1996; 53:1145–1152Crossref, Medline, Google Scholar
13. Gould MS, Fisher P, Parides M, Flory M, Shaffer D: Psychosocial risk factors of child and adolescent completed suicide. Arch Gen Psychiatry 1996; 53:1155–1162Crossref, Medline, Google Scholar
14. Johnson BA, Brent DA, Bridge J, Connolly J, Matta J, Constantine D, Rather C, White T: The familial aggregation of adolescent suicide attempts. Acta Psychiatr Scand 1998; 97:18–24Crossref, Medline, Google Scholar
15. Pfeffer CR, Normandin L, Tatsuyuki K: Suicidal children grow up: suicidal behavior and psychiatric disorders among relatives. J Am Acad Child Psychiatry 1994; 33:1087–1097Crossref, Google Scholar
16. Brent DA, Oquendo MA, Birmaher B, Greenhill L, Kolko DJ, Stanley B, Zelazny J, Brodsky BS, Bridge J, Ellis SP, Salazar O, Mann JJ: Familial pathways to early-onset suicide attempts: a high-risk study. Arch Gen Psychiatry 2002; 59:801–807Crossref, Medline, Google Scholar
17. Mann JJ, McBride PA, Brown RP, Linnoila M, Leon AC, DeMeo M, Mieczkowski T, Myers JE, Stanley M: Relationship between central and peripheral serotonin indexes in depressed and suicidal psychiatric inpatients. Arch Gen Psychiatry 1992; 49:442–446Crossref, Medline, Google Scholar
18. Statham DJ, Heath AC, Madden PAF, Bucholz KK, Bierut L, Dinwiddie SH, Slutske WS, Dunne MP, Martin NG: Suicidal behaviour: an epidemiological and genetic study. Psychol Med 1998; 28:839–855Crossref, Medline, Google Scholar
19. First MB, Spitzer RL, Gibbon M, Williams JB: Structured Clinical Interview for DSM-IV Axis I Disorders, version 2.0 (SCID-I). New York, New York State Psychiatric Institute, Biometrics Research, 1996Google Scholar
20. Andreasen NC, Endicott J, Spitzer RL, Winokur G: The family history method using diagnostic criteria: reliability and validity. Arch Gen Psychiatry 1977; 34:1229–1235Crossref, Medline, Google Scholar
21. Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N: Schedule for Affective Disorders and Schizophrenia for School-Age Children—Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 1997; 36:980–988Crossref, Medline, Google Scholar
22. Beck AT, Schuyler D, Herman I: Development of suicidal intent scales, in The Prediction of Suicide. Edited by Beck AT, Lettieri DJ, Resnick HLP. Bowie, Md, Charles Press, 1974, pp 45–55Google Scholar
23. First MB, Gibbon M, Spitzer RL, Williams JB, Benjamin L: Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II): User’s Guide. Washington, DC, American Psychiatric Press, 1997Google Scholar
24. Brown GL, Goodwin FK: Human aggression and suicide. Suicide Life Threat Behav 1986; 16:223–243Crossref, Medline, Google Scholar
25. Buss AH, Durkee A: An inventory for assessing different kinds of hostility. J Consult Psychol 1957; 21:343–349Crossref, Medline, Google Scholar
26. Kazdin AE, Rodgers A, Colbus D, Siegel T: Children’s Hostility Inventory: measurement of aggression and hostility in psychiatric inpatient children. J Clin Child Psychol 1987; 16:320–328Crossref, Google Scholar
27. Barratt ES: Factor analysis of some psychometric measures of impulsiveness and anxiety. Psychol Rep 1965; 16:547–554Crossref, Medline, Google Scholar
28. Pelham WE, Milich R, Murphy DA, Murphy HA: Normative data on the IOWA Conners Teacher Rating Scale. J Clinical Child Psychiatry 1989; 18:259–262Crossref, Google Scholar
29. Wagner AW, Linehan MM: Relationship between childhood sexual abuse and topography of parasuicide among women with borderline personality disorder. J Personal Disord 1994; 8:1–9Crossref, Google Scholar
30. Lukens E, Puig-Antich J, Behn J, Goetz R, Tabrizi M, Davies M: Reliability of the Psychosocial Schedule for School-Age Children. J Am Acad Child Psychiatry 1983; 22:29–39Crossref, Medline, Google Scholar
31. Mitterauer B: A contribution to the discussion of the role of the genetic factor in suicide, based on five studies in an epidemiologically defined area (Province of Salzburg, Austria). Compr Psychiatry 1990; 31:557–565Crossref, Medline, Google Scholar
32. Mann JJ, Waternaux C, Haas GL, Malone KM: Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry 1999; 156:181–189Abstract, Google Scholar
33. Brodsky BS, Oquendo M, Ellis SP, Haas GL, Malone KM, Mann JJ: The relationship of childhood abuse to impulsivity and suicidal behavior in adults with major depression. Am J Psychiatry 2001; 158:1871–1877Link, Google Scholar
34. Kaplan ML, Asnis GM, Lipschitz DS, Chorney P: Suicidal behavior and abuse in psychiatric outpatients. Compr Psychiatry 1995; 36:229–235Crossref, Medline, Google Scholar
35. Molnar BE, Berkman LF, Buka SL: Psychopathology, childhood sexual abuse and other childhood adversities: relative links to subsequent suicidal behavior in the US. Psychol Med 2001; 31:965–977Crossref, Medline, Google Scholar
36. Kovacs M, Devlin B: Internalizing disorders in childhood. J Child Psychol Psychiatry 1998; 39:47–63Crossref, Medline, Google Scholar
37. Stein MB, Torgrud LJ, Walker JR: Social phobia symptoms, subtypes, and severity: findings from a community survey. Arch Gen Psychiatry 2000; 57:1046–1052Crossref, Medline, Google Scholar
38. Breslau N, Schultz L, Peterson E: Sex differences in depression: a role for preexisting anxiety. Psychiatry Res 1995; 58:1–12Crossref, Medline, Google Scholar
39. Hayward C, Varady S, Albano AM, Thienemann ML, Henderson L, Schatzberg A: Cognitive-behavioral group therapy for social phobia in female adolescents: results of a pilot study. J Am Acad Child Adolesc Psychiatry 2000; 39:721–726Crossref, Medline, Google Scholar
40. Brown J, Cohen P, Johnson JG, Smailes EM: Childhood abuse and neglect: specificity of effects on adolescent and young adult depression and suicidality. J Am Acad Child Adolesc Psychiatry 1999; 38:1490–1496Crossref, Medline, Google Scholar
41. Fergusson DM, Horwood LJ, Lynskey MT: Childhood sexual abuse and psychiatric disorder in young adulthood, II: psychiatric outcomes of childhood sexual abuse. J Am Acad Child Adolesc Psychiatry 1996; 35:1365–1374Crossref, Medline, Google Scholar
42. Groholt B, Ekeberg O, Wichstrom L, Haldorsen T: Suicide among children and younger and older adolescents in Norway: a comparative study. J Am Acad Child Adolesc Psychiatry 1998; 37:473–481Crossref, Medline, Google Scholar
43. Rich CL, Young D, Fowler RC: San Diego suicide study, I: young vs old subjects. Arch Gen Psychiatry 1986; 43:577–582Crossref, Medline, Google Scholar
44. Brent DA, Baugher M, Bridge J, Chen J, Beery L: Age and sex-related risk factors for adolescent suicide. J Am Acad Child Adolesc Psychiatry 1999; 38:1497–1505Crossref, Medline, Google Scholar
45. Conwell Y, Brent D: Suicide and aging, I: patterns of psychiatric diagnoses. Int Psychogeriatr 1995; 7:149–164Crossref, Medline, Google Scholar
46. Pierce DW: The predictive validation of a suicide intent scale: a five year follow-up. Br J Psychiatry 1981; 139:391–396Crossref, Medline, Google Scholar



