D8/17 Expression on B Lymphocytes in Anorexia Nervosa
Abstract
OBJECTIVE: The authors’ goal was to determine whether D8/17, a rheumatic fever susceptibility trait marker, identifies a possible type of anorexia nervosa: pediatric autoimmune neuropsychiatric disorders associated with streptococcus (PANDAS) anorexia nervosa. METHOD: Using immunofluorescence, the authors measured the percentage of D8/17-positive B lymphocytes in the peripheral blood of 16 subjects 7–21 years old who had not had rheumatic fever but who had possible PANDAS anorexia nervosa. The comparison subjects were 17 psychiatric patients with no eating disorder and no PANDAS characteristics. Subjects were considered D8/17 positive if they had 12% or more D8/17+ cells. RESULTS: There were more D8/17-positive individuals among those with PANDAS anorexia nervosa (81%) than among the comparison subjects (12%). The subjects with PANDAS anorexia nervosa had a higher percentage of D8/17+ cells (mean=27.1%, SD=17%) than the comparison subjects (mean=5.3%, SD=7.4%). CONCLUSIONS: A larger study is needed to determine whether D8/17 serves as a marker for susceptibility to a type of anorexia nervosa.
Anorexia nervosa is a serious disorder with a mortality rate among the highest of the psychiatric disorders, poorly understood pathogenesis, and no definitive treatment (1). Clinical and research observations led to the hypothesis that a postinfectious process, similar to that in rheumatic fever, may cause or exacerbate certain cases of anorexia nervosa (2). When the pathogen is group A β-hemolytic streptococcus, these disorders are called pediatric autoimmune neuropsychiatric disorders associated with streptococcus (PANDAS).
Swedo et al. (3) identified a group of children with obsessive-compulsive disorder (OCD) and/or tics who had PANDAS characteristics. These children often expressed the lymphocyte B marker D8/17, apparently a trait marker for susceptibility to rheumatic fever and Sydenham’s chorea (4).
OCD and anorexia nervosa may be related, as evidenced by phenomenology, comorbidity, neurotransmitters, and CNS functional metabolism (5). Many patients with anorexia nervosa have obsessions (about food and weight) and compulsions (overexercise and eating behaviors). This, along with observation of cases of anorexia nervosa whose onset appeared temporally related to infection, led to the hypothesis of a type of anorexia nervosa similar to PANDAS OCD (2).
The purpose of this project was to study the possibility of an infection-triggered type of anorexia nervosa and to determine whether D8/17 identifies PANDAS anorexia nervosa. We hypothesized that patients with PANDAS anorexia nervosa would have more D8/17+ cells than comparison psychiatric patients with no eating disorder or PANDAS characteristics.
Method
D8/17 was measured in 16 subjects with anorexia nervosa who had PANDAS anorexia nervosa characteristics with direct or indirect evidence of a streptococcal infection. D8/17 was also measured in 17 comparison subjects with no eating disorder and no PANDAS anorexia nervosa characteristic. Rheumatic fever and Sydenham’s chorea were ruled out in all subjects by using the Jones criteria (6).
The 16 subjects with PANDAS anorexia nervosa (15 girls and one boy) had a mean age of 14.7 years (SD=2.7, range=11–21). They had the following characteristics of possible PANDAS anorexia nervosa, similar to those in children with PANDAS OCD and tics (3): 1) DSM-IV diagnosis of anorexia nervosa, 2) prepubertal onset of anorexia nervosa (in 10 subjects), 3) acute onset or exacerbation of anorexia nervosa symptoms, 4) possible antecedent or concomitant streptococcal infection, with a temporal relationship to the onset of anorexia nervosa symptoms (as evidenced by clinical history, positive throat culture, and/or positive serological findings of antideoxyribonuclease B titer and/or antistreptolysin O titer), 5) anorexia nervosa symptoms that did not occur exclusively during stress or physical illness, and 6) minor neurological abnormalities.
Four of the subjects with anorexia had comorbid OCD. None had tic disorder, pervasive developmental disorder, or mental retardation. Eleven subjects with anorexia took one to three psychotropic medications; one of these 11 patients took levothyroxine. Five took no medication.
The comparison subjects were 17 psychiatric patients (five girls and 12 boys) with a mean age of 14.3 years (SD=3.0, range=7–19) and no current or past eating disorder, OCD, tics, pervasive developmental disorder, or moderate to severe mental retardation. Chart review revealed no infections before the onset of psychiatric symptoms. DSM-IV principal diagnoses included eight mood disorders, two psychotic disorders, one adjustment disorder, one disruptive behavior disorder, and five attention deficit hyperactivity disorders. Fifteen of the comparison subjects took one to four psychotropic medications. Two took no medication.
Presence of PANDAS anorexia nervosa characteristics in the anorexia nervosa patients and DSM-IV diagnoses in all participants were determined by a child psychiatrist (M.S.S.) and another physician (D.G.K. or H.T.). After complete description of the study to subjects and parents, written informed consent was obtained.
Monoclonal antibody D8/17 is an immunoglobulin M prepared from mice immunized with isolated B lymphocytes from humans with rheumatic fever. D8/17 determination immunofluorescent assay (7) was performed on blood samples by an individual blind to clinical information. Subjects were defined as D8/17 positive if they had 12% or more D8/17+ B cells (7). The percentage of D8/17+ cells (B lymphocytes fluorescing with D8/17 antibody) was obtained by dividing the number of D8/17+ B cells by the total number of CD19+ B cells counted.
Results
There were more D8/17-positive individuals among the subjects with anorexia nervosa (N=13, 81%) than comparison subjects (N=2, 12%) (p<0.0001, Fisher exact test). All but three of the subjects with anorexia were D8/17 positive. The range of D8/17+ B cells among these subjects was 6% to 70%. Two of the 17 comparison subjects had the rheumatic marker. The scores of the D8/17-negative comparison subjects ranged from 1% to 9%. The two D8/17-positive comparison subjects had scores of 12% and 30%. The average percentage of B cells expressing the D8/17 antigen was significantly higher in subjects with anorexia nervosa (mean=27.1%, SD=17.1%) than in comparison subjects (mean=5.3%, SD=7.4%) (t=4.8, df=31, p<0.00002) (Figure 1).
Discussion
Patients with possible PANDAS anorexia nervosa were significantly more likely than psychiatric patients without PANDAS-related characteristics to have peripheral B lymphocytes expressing D8/17. These data suggest that D8/17, a rheumatic fever susceptibility trait marker, may be useful in identifying PANDAS anorexia nervosa. Investigation of this biological marker might lead to improved treatment and preventive strategies for some cases of this serious disorder.
A larger prospective study is needed, with a better-matched comparison group and careful controls for all variables, including evidence of streptococcal infection and the relationship between streptococcal infection and the time of onset of anorexia nervosa symptoms. We know of no completed study showing medication effect on D8/17 level, but this also needs investigation.
Future studies should involve a family-based comparison group because there may be a genetic predisposition to the D8/17-positive phenotype, as evidenced by the report by Khanna et al. (8) of a high number of D8/17+ cells in rheumatic fever patients’ unaffected siblings.
The characteristics of PANDAS anorexia nervosa need to be clarified, and PANDAS anorexia nervosa patients need to be compared with non-PANDAS anorexia nervosa patients. Also, since 25% of the anorexia nervosa subjects had comorbid OCD, the presence of the D8/17 marker may be attributable to OCD rather than anorexia nervosa. However, D8/17 may measure the same thing in anorexia nervosa and OCD; the D8/17 marker for rheumatic fever may identify children with PANDAS, and PANDAS may lead to different symptom manifestations, including OCD or anorexia nervosa. As already noted, anorexia nervosa and OCD may be related (5). Although the diagnostic value of D8/17 remains uncertain, it may provide some insight into the underlying processes in these illnesses.
Received Aug. 7, 2001; revision received Feb. 27, 2002; accepted March 21, 2002. From the Creighton University School of Medicine and Children’s Hospital, Omaha; and the Laboratory of Clinical Microbiology and Immunology, Rockefeller University, New York. Address reprint requests to Dr. Sokol, Eating Disorders Program, Children’s Hospital, 8200 Dodge St., Omaha NE 68114; [email protected] (e-mail). Supported by a grant from Callisto Pharmaceuticals and the Menninger Foundation Child and Family Center. The authors thank Drs. Peter Fonagy and John Sargent, Ms. Andrea Burgett, and the Menninger Library staff.Mr. Houston died in 2002.
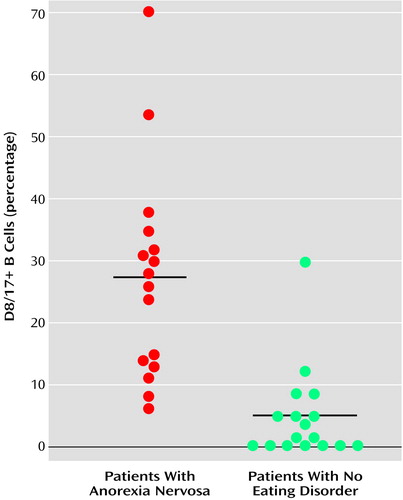
Figure 1. Number of D8/17+ B Cells in Patients With Anorexia Nervosa and Characteristics of Possible Pediatric Autoimmune Neuropsychiatric Disorders Associated With Streptococcus (PANDAS) and in Psychiatric Patients With No Eating Disorder or PANDAS Characteristicsa
aThere was a significant difference between the mean values for the anorexia nervosa patients (27.1%) and the comparison subjects (5.3%) (t=4.8, df=31, p<0.00002).
1. Becker AE, Grinspoon SK, Klibanski A, Herzog DB: Eating disorders. N Engl J Med 1999; 340:1092-1098Crossref, Medline, Google Scholar
2. Sokol MS: Infection-triggered anorexia nervosa in children: clinical description of four cases. J Child Adolesc Psychopharmacol 2000; 10:133-145Crossref, Medline, Google Scholar
3. Swedo SE, Leonard HL, Garvey M, Mittleman B, Allen AJ, Perlmutter S, Dow S, Zamkoff J, Dubbert BK, Lougee L: Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections: clinical description of the first 50 cases. Am J Psychiatry 1998; 155:264-271; correction, 155:578Abstract, Google Scholar
4. Swedo SE, Leonard HL, Mittleman BB, Allen AJ, Rapoport JL, Dow SP, Kanter ME, Chapman F, Zabriskie J: Identification of children with pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections by a marker associated with rheumatic fever. Am J Psychiatry 1997; 154:110-112Link, Google Scholar
5. Jarry JL, Vaccarino FJ: Eating disorders and obsessive-compulsive disorder: neurochemical and phenomenological commonalities. J Psychiatry Neurosci 1996; 121:36-48Google Scholar
6. Special Writing Group of the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease of the Council on Cardiovascular Disease in the Young of the American Heart Association: Guidelines for the diagnosis of rheumatic fever: Jones criteria, 1992 update. JAMA 1992; 268:2069-2073; correction, 1993; 269:476Google Scholar
7. Chapman F, Visvanathan K, Carreno-Manjarrezr R, Zabriskie JB: A flow cytometric assay for D8/17 B cell marker in patients with Tourette’s syndrome and obsessive compulsive disorder. J Immunol Methods 1998; 219:181-186Crossref, Medline, Google Scholar
8. Khanna AK, Buskirk DR, Williams RC Jr, Gibofsky A, Crow MK, Menon A, Fotino M, Reid HM, Poon-King T, Rubinstein P, Zabriskie JB: Presence of a non-HLA B cell antigen in rheumatic fever patients and their families as defined by a monoclonal antibody. J Clin Invest 1989; 83:1710-1716Crossref, Medline, Google Scholar



