Association of Recurrent Suicidal Ideation With Nonremission From Acute Mixed Mania
Abstract
Objective:The authors’ goal was to examine suicidality in relation to acute symptom remission in inpatients with mixed and pure bipolar disorder.Method:Using chart review of 184 adult inpatients with bipolar I disorder, the authors assessed patients’ past and current suicidality, other psychopathology, treatment, and remission.Results:Past, current, and recurrent suicidality were significantly more common among patients with mixed mania than among those with pure mania. The probability of remission declined by 49% for every suicide attempt made before the index manic episode. Mixed mania, multiple previous hospitalizations, and previous suicide attempts were significantly associated with current suicidality.Conclusions:Suicidality is linked with mixed manic states and may be a clinical marker for recurrent dysphoric mania. Multiple suicide attempts are associated with nonremission from mixed manic episodes. Am J Psychiatry 1998; 155: 1753-1755
Reports have suggested that suicidality is more common among patients with bipolar disorder who have mixed mania than among those who have pure mania (1, 2). It is unknown whether suicidality in mania may be prognostically or pathognomonically important for mixed states. The clinical significance of suicidality during mania with subsyndromal depression also remains unknown. The goals of this study were 1) to determine frequency of current suicidal ideation and previous suicide attempts for inpatients with mixed and pure mania and 2) to compare acute remission rates for suicidal and nonsuicidal patients with bipolar disorder.
METHOD
We reviewed consecutive charts for 253 inpatients with acute mania at the Payne Whitney Clinic, New York Hospital, from 1991 to 1995. The study group included 184 patients who unequivocally met DSM-III-R criteria for bipolar I mania and who had no evidence of past or current schizophrenia or schizoaffective disorder, primary substance abuse or dependence, or primary personality disorder. Additionally, we required that patients remained hospitalized for 2 weeks or longer and received lithium, carbamazepine, or divalproex.
We used a standardized protocol described elsewhere (3) to obtain data on affective or psychotic symptoms, substance abuse or dependence, and treatment from intake records, progress notes, and discharge summaries. We rated overall severity, according to hospital records, at baseline and weekly thereafter using the Clinical Global Impression (CGI) severity scale. Remission was defined by a CGI severity score of 2 or lower (indicating that the subject was borderline mentally ill) for 1 week or longer.
We used the Cincinnati criteria (4) to make distinctions between pure and mixed manic episodes. Patients with mixed mania met full DSM-III-R criteria for a bipolar I manic episode and had two or more prominent depressive features other than current suicidality. Symptoms that could be either manic or depressive in nature (e.g., insomnia, poor concentration), when ambiguous, were excluded as defining of mixed mania. Episodes with fewer than two prominent depressive symptoms were rated as purely manic.
On hospitalization, admitting psychiatrists interviewed and rated each patient systematically for current or recent suicidal ideation, attempts, and past attempts using a standardized hospital intake form. Suicidal ideation or attempts in the hospital were regularly documented by treating psychiatrists for each patient throughout the index episode. Additional information on previous suicide attempts was culled from chart notes. Complete data on previous suicide attempts were available for 163 of the 184 patients with bipolar disorder. Patients were judged to have made a suicide attempt if they displayed behaviors that involved suicidal intention and a potential for lethality or significant self-harm.
Approval was obtained to conduct the research protocol through the Committee on Human Rights of Cornell University Medical College.
Dichotomous variables were analyzed by using chi-square analysis or Fisher’s exact test. Group mean differences were compared by using the Mann-Whitney U test. To examine associations between relevant independent variables and 1) suicidality at index episode or 2) remission from the index manic episode, logistic regression analyses were conducted, from which Wald chi-square statistics and odds ratios with 95% confidence intervals were derived. Two-tailed alpha levels of 0.05 were used for all statistical tests.
RESULTS
Seventy-seven (41.8%) of the 184 patients met criteria for pure mania and 107 (58.2%) for mixed mania. The mean age for the total study group was 40.4 years (SD=15.3); 99 (53.8%) were women; 133 (72.3%) were white; and 131 (71.2%) were psychotic (i.e., had delusions and/or hallucinations) during the index episode. Patients with pure mania had greater CGI baseline severity scores than patients with mixed mania (Mann-Whitney U=2308.5, N=183, p<0.001). Patients with mixed and pure mania did not differ in age (Mann-Whitney U=3972.5, N=183, p=0.79), sex (χ2=0.73, df=1, p=0.39), number of previous hospitalizations (Mann-Whitney U=3174.0, N=176, p=0.10), age at onset of illness (Mann-Whitney U=3631.5, N=174, p=0.94), lifetime duration of illness (Mann-Whitney U=3637.5, N=174, p=0.95), or psychosis (χ2=0.09, df=1, p=0.77).
Thirty-nine (23.9%) of the 163 patients with bipolar disorder who had complete pre-index-episode suicide ratings had made one or more previous suicide attempts. For the full study group of 184 patients, 63 (34.2%) had suicidal ideation or attempts during the index episode. Fifty-eight (92.1%) of these 63 patients had suicidal ideation without attempts; four (6.3%) made an attempt during the current episode; and one (1.6%) had current suicidal ideation with unknown attempts during the index episode. The 63 ideators or attempters during the index episode were combined and classified as suicidal during the index episode because of the small number of attempters relative to ideators.
During the index episode, 62 (57.9%) of the 107 patients with mixed mania were suicidal, compared with one (1.3%) of the 77 patients with pure mania (χ2=63.8, df=1, p<0.001). Suicide attempts before the index episode were also more common among patients with current mixed mania (33 [36.7%] of 90 patients) than among those with pure mania (six [8.2%] of 73 patients) (χ2=17.9, df=1, p<0.001).
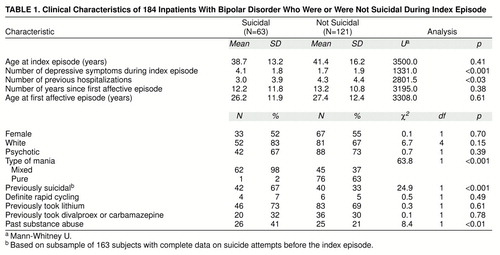
Table 1 compares features of suicidal and nonsuicidal patients with bipolar disorder during the index episode. Currently suicidal patients with bipolar disorder had significantly more depressive symptoms (other than suicidality), substance abuse, previous hospitalizations, and previous suicide attempts. Suicidality during the index episode was evident among 66.7% (26 of 39) previous suicide attempters, compared with 23.4% (29 of 124) subjects who had not attempted suicide.
Twenty-six (78.8%) of the 33 patients with mixed mania who had made previous suicide attempts were again suicidal during the index episode, compared with 28 (49.1%) of the 57 patients with mixed mania who had not made a suicide attempt (χ2=7.7, df=1, p<0.01). In contrast, among patients with pure mania, none of the six previously suicidal and only one (1.5%) of the 67 previously nonsuicidal patients were currently suicidal (p=1.0, Fisher’s exact test, two-tailed).
To examine the strength of association of seven hypothesized clinical correlates of suicidality at index episode, we conducted logistic regression on 153 of the 163 patients with complete data on previous suicide attempts who also had complete data on all other regression variables. Current suicidality was more common among 1) patients with mixed mania than those with pure mania (Wald χ2=11.10, df=1, p<0.001, odds ratio=0.02, 95% confidence interval=0.002–0.210), 2) pre-index-episode suicide attempters (Wald χ2=6.39, df=1, p<0.02, odds ratio=3.71, 95% confidence interval=1.335–9.534), and 3) previously hospitalized patients (Wald χ2=3.85, df=1, p<0.05, odds ratio=0.90, 95% confidence interval=0.811–1.000). Nonsignificant variables included sex (Wald χ2=0.47, df=1, p=0.49, odds ratio=1.39, 95% confidence interval=0.540–3.590), baseline severity (Wald χ2=0.05, df=1, p=0.82, odds ratio=0.94, 95% confidence interval=0.561–1.579), number of current depressive symptoms (Wald χ2=0.55, df=1, p=0.46, odds ratio=1.12, 95% confidence interval=0.828–1.521), and substance abuse (Wald χ2=1.44, df=1, p=0.23, odds ratio=1.79, 95% confidence interval=0.691–4.643).
A separate logistic regression (N=108) examined the association between remission and suicidality at index episode. For every suicide attempt made before the index episode, the likelihood of remission declined 49% (Wald χ2=4.63, df=1, p<0.05, odds ratio=0.51, 95% confidence interval=0.261–0.939), and for every week needed to achieve a therapeutic serum level of any mood stabilizer (i.e., ≥0.8 meq/liter of lithium; ≥50 mmol/liter of divalproex; ≥8 mmol/liter of carbamazepine), the likelihood of remission declined 36% (Wald χ2=7.45, df=1, p<0.01, odds ratio=0.64, 95% confidence interval=0.470–0.883). Nonsignificant variables included mixed or pure mania (Wald χ2=0.85, df=1, p=0.36, odds ratio=0.54, 95% confidence interval=0.146–2.003), sex (Wald χ2=2.07, df=1, p=0.15, odds ratio=2.30, 95% confidence interval=0.738–7.190), substance abuse (Wald χ2=1.01, df=1, p=0.32, odds ratio=0.55, 95% confidence interval=0.171–1.767), baseline severity (Wald χ2=1.92, df=1, p=0.17, odds ratio=0.63, 95% confidence interval=0.325–1.214), psychosis (Wald χ2=0.44, df=1, p=0.51, odds ratio=0.61, 95% confidence interval=0.14–2.61), and previous hospitalizations (Wald χ2=0.24, df=1, p=0.63, odds ratio=0.97, 95% confidence interval=0.839–1.111). No differences were observed between medication groups and remission (Wald χ2=0.36, df=1, p=0.83).
DISCUSSION
The present findings, although limited by the retrospective research design, are consistent with previous reports suggesting that suicidality is more common among patients with bipolar disorder who have mixed mania than among those with pure mania (1, 2). Moreover, previous suicide attempts were strongly associated with current suicidality for patients with mixed mania but not those with pure mania. Additionally, the extent of previous suicidality was strongly associated with acute nonremission. Multiple previous suicide attempts may reflect more severe lifetime illness and affective unpredictability. Patients with mixed mania, in particular, may be especially at risk for nonrecovery, treatment failure, comorbid illnesses, and poor outcome (5). These features, perhaps even more than current suicidality, may collectively predispose patients with mixed mania to demoralization and treatment failure.
The association between suicidality at index episode and number of depressive symptoms was not significant when controlled for. Rather, only the presence of mixed mania per se, combined with a history of previous suicidality and multiple past hospitalizations, significantly predicted suicidal ideation or attempts during the index episode. These findings support previous studies suggesting that suicidality correlates with the extent of depressive features in mixed mania ((2), but this association may be less robust than is the link between suicidality and dysphoria during acute mania. Moreover, although suicidal patients with bipolar disorder had more substance abuse, higher baseline severity, more previous hospitalizations, and more depressive symptoms than nonsuicidal patients with bipolar disorder, these variables did not predict nonremission when controlled for.
Our results question the stringent criteria by which DSM-IV defines mixed mania, where a full manic and simultaneous full major depressive syndrome are required to classify a mixed state. When mixed mania was defined by only two depressive symptoms other than suicidality, plus a full manic episode, suicidality was more prevalent among patients with mixed mania than among those with bipolar disorder with one or no depressive features. This suggests that significant depression and suicide risk merit identification in a broader subgroup of manias with subsyndromal depression.
The data suggest a vulnerability to recurrent suicidality among dysphoric patients with mania, raising the possibility that dysphoric mania with suicidality recurs as a distinct phenomenon for some patients with bipolar disorder. Prospective longitudinal studies are needed to confirm this speculation about the nature of recurrent mixed versus pure mania.
Presented, in part, at the 150th annual meeting of the American Psychiatric Association, San Diego, May 17–22, 1997, and the Second International Conference on Bipolar Disorders, Pittsburgh, June 19–21, 1997 Received Oct. 29, 1997; ; revisions received March 31 and June 12, 1998; accepted Aug. 4, 1998. From the Bipolar Disorders Research Clinic, Payne Whitney Clinic, New York and Presbyterian Hospital; and the Weill Medical College of Cornell University, New York. Address reprint requests to Dr. Goldberg, Payne Whitney Clinic, New York Hospital, 525 E. 68th St., New York, NY 10021. Supported by a grant from Abbott Laboratories, Abbott Park, Ill.; by a fund established in the New York Community Trust by DeWitt-Wallace; and by funds from the Pritzker Depression Network.The authors thank Amy Kossoy, B.S., for assistance with data collection.
 |
1. Dilsaver SC, Chen Y-W, Swann AC, Shoaib AM, Krajewski KJ: Suicidality in patients with pure and depressive mania. Am J Psychiatry 1994; 151:1312–1315Link, Google Scholar
2. Strakowski SM, McElroy SL, Keck PE Jr, West SA: Suicidality among patients with mixed and manic bipolar disorder. Am J Psychiatry 1996; 153:674–676Link, Google Scholar
3. Goldberg JF, Garno JL, Leon AC, Kocsis JH, Portera L: Rapid titration of mood stabilizers predicts remission from mixed or pure mania in bipolar patients. J Clin Psychiatry 1998; 59:151–158Crossref, Medline, Google Scholar
4. McElroy SL, Keck PE Jr, Pope HG Jr, Hudson JI, Faedda GL, Swann AC: Clinical and research implications of the diagnosis of dysphoric or mixed mania or hypomania. Am J Psychiatry 1992; 149:1633–1644Link, Google Scholar
5. Keller MB, Lavori PW, Coryell W, Endicott J, Mueller TI: Bipolar I: a five-year prospective follow-up. J Nerv Ment Dis 1993; 181:238–245Crossref, Medline, Google Scholar



