Major Depression in Individuals With a History of Childhood Physical or Sexual Abuse: Relationship to Neurovegetative Features, Mania, and Gender
Abstract
Objective:Numerous studies have linked childhood trauma with depressive symptoms over the life span. However, it is not known whether particular neurovegetative symptom clusters or affective disorders are more closely linked with early abuse than are others. In a large community sample from Ontario, the authors examined whether a history of physical or sexual abuse in childhood was associated with particular neurovegetative symptom clusters of depression, with mania, or with both.Method:The World Health Organization Composite International Diagnostic Interview was used to assess 8,116 individuals aged 15–64 years. Each subject was asked about early physical and sexual abuse experiences on a structured supplement to the interview. Six hundred fifty-three cases of major depression were identified. Rates of physical and sexual abuse in depressive subgroups defined by typical and reversed neurovegetative symptom clusters (i.e., decreased appetite, weight loss, and insomnia versus increased appetite, weight gain, and hypersomnia, respectively) and by the presence or absence of lifetime mania were compared by gender.Results:A history of physical or sexual abuse in childhood was associated with major depression with reversed neurovegetative features, whether or not manic subjects were included in the analysis. A strong relationship between mania and childhood physical abuse was found. Across analyses there was a significant main effect of female gender on risk of early sexual abuse; however, none of the group-by-gender interactions predicted early abuse.Conclusions:These results suggest an association between early traumatic experiences and particular symptom clusters of depression, mania, or both in adults. Am J Psychiatry 1998; 155: 1746-1752
Major depression is a significant health problem with very high prevalence rates, high rates of chronicity, and substantial morbidity and mortality (1–5). Research on the etiology of depression is hampered by the heterogeneous nature of this disorder. The myriad of research approaches used to study depression has also been problematic, with a tendency to separate psychosocial/life events research from biological research. The development of models that link life experiences, neurodevelopment, and psychopathology (6, 7) has been a major step forward in this regard.
To further assess and refine etiological models of mood disorders that integrate life events and neurodevelopment, it would be important to examine whether particular experiences in early development lead to unique expressions of psychopathology over the life span. While there is now a large body of evidence that childhood physical and sexual abuse are significant risk factors for depression in all age groups (8–24), it is not known whether particular symptom clusters or subtypes of depression are more closely linked with early abuse than are others. It might be that early trauma produces adaptive changes in the CNS in a way that promotes some but not all depressive subtypes. Given the heterogeneity of major depression, linking early trauma to particular expressions of this disorder would be a substantial step forward, helping to refine our theoretical understanding of how psychosocial stress might be translated into affective disturbance, helping to identify high-risk individuals, and thus improving our ability to treat depression over time.
The overall goal of the current project was to use a large community epidemiological study to explore whether childhood physical and/or sexual abuse is associated with particular symptom clusters of major depression, with mania, or with both in individuals aged 15–64 years. We chose to focus on neurovegetative symptoms related to eating behavior and sleep and on manic depression, as there is considerable evidence that these dimensions have theoretical and clinical relevance and may reflect unique biological processes based on epidemiology, course of illness, and treatment response (25dash;27 and DSM-IV). The particular depressive subgroups we examined were defined by typical neurovegetative symptoms (decreased appetite, weight loss, insomnia) or reversed neurovegetative symptoms (increased appetite, weight gain, hypersomnia) and by the presence or absence of lifetime mania. The specific questions we sought to examine were as follows. 1) Is childhood physical and/or sexual abuse associated with a particular neurovegetative pattern, or patterns, of depression in later years? 2) Does having one or more lifetime episodes of depression with typical features predict a history of childhood abuse? 3) Does having one or more lifetime episodes of depression with reversed features predict a history of childhood abuse? 4) Is bipolar depression associated with childhood abuse?
On the basis of the higher prevalence rates of depression in females (28) and the different patterns of both depression and early abuse in females compared with males (28,29), gender was used as a grouping variable throughout the study.
METHOD
This study was a secondary analysis of data from the Mental Health Supplement to the Ontario Health Survey, a community survey of 9,953 residents of Ontario, Canada, conducted in 1990–1991. This supplement was designed to assess the prevalence of major psychiatric disorders and associated risk factors, health care utilization, and disability. A stratified, multistage sampling design was used (30). The province was divided into a number of enumeration areas, and households were sampled from each area. One individual, aged 15 years or older, was randomly selected from each household to be the respondent. Individuals living in institutions or on native reserves were excluded. A response rate of 76.5% was achieved. Because subjects over the age of 64 were administered a shortened version of the original questionnaire, they were not included in the current study. The overall sample from which our subjects were identified thus included 8,116 respondents aged 15–64 years.
Because this was a project funded by the provincial government and implemented by Statistics Canada (equivalent to the U.S. Census Bureau), standard provincial and federal procedures were followed for informing participants about the study. Before interviewer contact, an official letter was sent to each prospective respondent that described the nature of the project, the fact that participation was voluntary, and the federal legislation which protected confidentiality.
The Mental Health Supplement questionnaire has a number of components, including a diagnostic instrument, a series of measures to assess disability, a set of questions to measure service utilization, and basic demographic information. Individuals were interviewed face-to-face for 1–2 hours by specially trained lay interviewers. The diagnostic instrument we used, the World Health Organization Composite International Diagnostic Interview, is a structured interview based on the National Institute of Mental Health Diagnostic Interview Schedule and the Present State Examination and has good reliability and validity (31). The version used here, the UM-Composite International Diagnostic Interview, had been modified and further field tested (32). Major diagnoses surveyed included anxiety disorders, affective disorders, eating disorders, psychotic disorders, substance abuse, and antisocial personality disorder, according to the DSM-III-R criteria. The Composite International Diagnostic Interview systematically records the symptoms of each potential disorder, and both current and lifetime diagnoses are delineated.
Childhood abuse was assessed with the use of a self-report questionnaire developed specifically for the Mental Health Supplement (29). The questionnaire consisted of seven questions related to physical abuse and four related to sexual abuse (appendix 1). The sexual abuse questions were derived from the National Population Survey, a Canadian survey on sexual abuse described elsewhere (33). During the administration of the Composite International Diagnostic Interview, respondents were asked to complete the self-report questionnaire and place it in a sealed envelope coded with only an identification number for confidentiality.
Analysis
Only subjects in the 15- to 64-year age range who met the criteria for current or lifetime major depression were included in the current analysis. As an initial step to examine possible associations between neurovegetative patterns of depression and childhood abuse, each depressed subject was assigned to one of four neurovegetative groups as follows (34).
| 1. | Subjects in the typical-symptom group positively endorsed each of the three items “decreased appetite,” “weight loss,” and “insomnia (initial, middle, or late)” on the Composite International Diagnostic Interview section for major depression (current or lifetime). | ||||
| 2. | Subjects in the reversed-symptom group positively endorsed each of the three items “increased appetite,” “weight gain,” and “hypersomnia” on the Composite International Diagnostic Interview section for major depression (current or lifetime). | ||||
| 3. | Subjects in the neither-symptom group had major depressive episodes, current or lifetime, but did not meet the criteria for either the typical- or the reversed-symptom group. | ||||
| 4. | Subjects in the fluctuating-symptom group experienced both typical and reversed major depressive episodes over time and met the criteria for both the typical- and reversed-symptom groups. | ||||
The rationale for including four as opposed to two depressive subgroups based on neurovegetative symptoms was our recent finding that in this community sample, many of the differences across these four groups were due to the unique characteristics of the neither-symptom and fluctuating-symptom groups (34). The fluctuating-symptom group accounted for one-third of all individuals with a lifetime history of depression with reversed features and had particularly high levels of mania, panic attacks, substance abuse, bulimia, antisocial features, and health care utilization, consistent with a high degree of mood dysregulation and overall psychopathology in this group. The neither-symptom group was the largest of the four groups and had the lowest rate of serious psychopathology.
To limit the number of independent variables in the analysis, the item asking whether the subject had ever been slapped or spanked was eliminated on the basis of extremely high positive endorsement rates in all identified subgroups. The item asking whether the subject had ever been choked, burned, or scalded was endorsed extremely rarely and was excluded on this basis. This left five physical abuse and four sexual abuse variables for subsequent analyses. For the five physical abuse variables, each item was scored 3 (often) to 0 (never), and a physical abuse total score of 0–15 was calculated by summing the scores across the five items. The sexual abuse items were dichotomized into responses of yes (score=1) or no (score=0) on the questionnaire itself, creating a sexual abuse total score ranging from 0 to 4 for a given subject. For each analysis, when incomplete data made it impossible to assign a group for a given subject, the subject’s data were removed from this step. This led to some differences in sample sizes across analyses.
Statistical Procedures
To assess possible associations between subtypes of depression and childhood abuse experiences, the four key study questions were analyzed as described below. For each question, two main analyses were completed, one in which the physical abuse total scores were used as the dependent variable and another in which the sexual abuse total scores were used. Gender was used as a grouping variable for all analyses.
| 1. | Do the four depressive subgroups, as defined by neurovegetative symptoms, exhibit different rates of childhood physical and/or sexual abuse? Subjects in each of the four neurovegetative subgroups of depression were compared by using a 4 (neurovegetative group) by 2 (gender) analysis of variance (ANOVA). Post hoc tests were done by using Tukey’s test of honestly significant difference. | ||||
| 2. | Does having one or more episodes of depression with typical features over the lifetime predict a history of childhood abuse? Subjects in the typical-symptom and fluctuating-symptom groups were combined (group with typical episodes) and compared with individuals in the reversed-symptom and neither-symptom groups combined (group without typical episodes) by means of a 2 (group) by 2 (gender) ANOVA. | ||||
| 3. | Does having one or more episodes of depression with reversed features over the lifetime predict a history of childhood abuse? Subjects in the reversed-symptom and fluctuating-symptom groups were combined (group with reversed episodes) and compared with individuals in the typical-symptom and neither-symptom groups combined (group without reversed episodes) by means of a 2 (group) by 2 (gender) ANOVA. | ||||
| 4. | Is bipolar depression associated with early abuse? For this step, subjects were designated as with or without mania (current or lifetime) and compared by means of a 2 (group) by 2 (gender) ANOVA; the four neurovegetative groups were not differentiated at this step. | ||||
To correct for multiple comparisons, the level of significance for all analyses was set at p<0.01.
RESULTS
Patient Characteristics
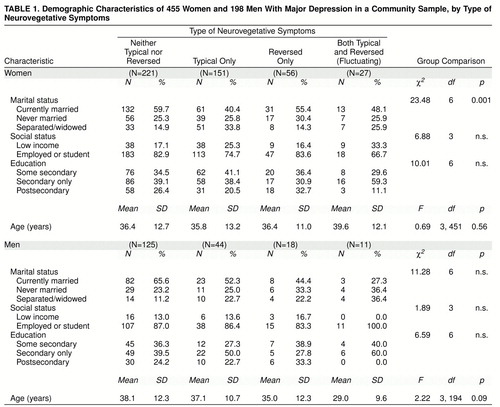
Of the total sample of 8,116 individuals, 653 (8.0%) met the criteria for major depression, current or lifetime. With respect to neurovegetative subgroups, 346 (53.0%) were classified as having neither typical nor reversed symptoms, 195 (29.9%) as having typical symptoms only, 74 (11.3%) as having reversed symptoms only, and 38 (5.8%) as having both types of symptoms (fluctuating) (34). Table 1 summarizes the demographic characteristics of the four neurovegetative subgroups by gender. The only significant difference across the neurovegetative subgroups was in the marital status of female subjects. A detailed summary of the characteristics of each of the four subgroups with respect to demographics, comorbidity, disability, and health care utilization, is available in a previous report (34).
Sixty-three subjects with a history of depression also met the criteria for an episode of mania, 562 did not, and 28 had incomplete or missing data for this section of the Composite International Diagnostic Interview.
Early Abuse and Neurovegetative Patterns of Depression
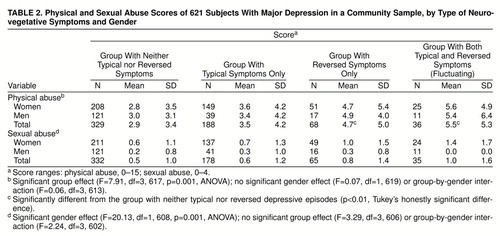
On question 1 (table 2), for physical abuse, the main effect of neurovegetative group was significant, while the main effect of gender and the group-by-gender interaction were nonsignificant. Post hoc tests comparing the individual groups revealed significant differences between the reversed-symptom and neither-symptom groups and between the fluctuating-symptom and neither-symptom groups. For sexual abuse, there was a significant main effect of female gender.
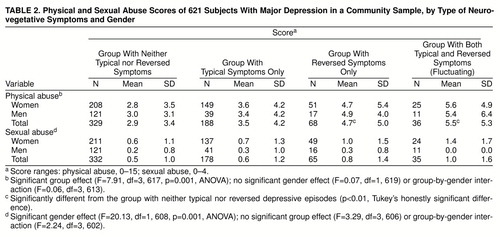
On question 2 regarding typical depressive episodes (table 3), for both physical abuse and sexual abuse, the main effect of group and the group-by-gender interaction were nonsignificant. There was a significant main effect of female gender for sexual abuse.
On question 3 regarding reversed depressive episodes (table 4), a significant main effect of group was found for both physical and sexual abuse; the data indicate higher abuse scores among individuals with a history of a reversed-symptom depressive episode. There was a main effect of female gender for sexual abuse. Both of the group-by-gender interactions were nonsignificant.
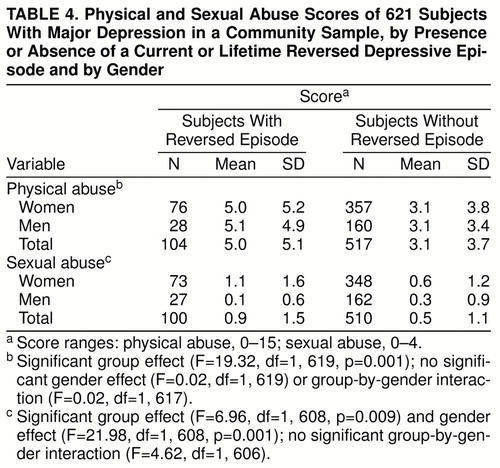
Early Abuse in Bipolar Depression
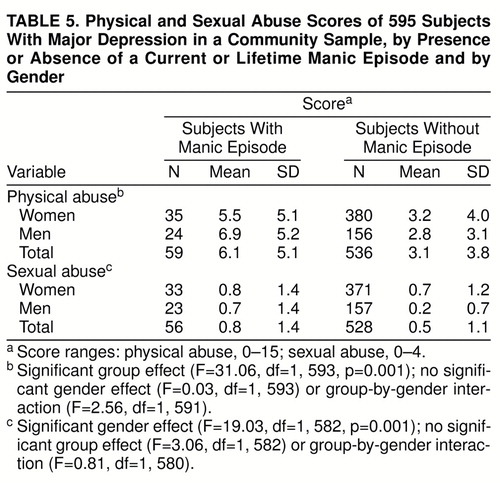
On question 4 (table 5), for physical abuse, the results indicate a strong main effect of group, but not of gender, suggesting that individuals with a lifetime history of major depression and mania have a significantly greater rate of childhood physical abuse than do other depressed subjects. The interaction of group and gender was nonsignificant. For sexual abuse, the main effect of female gender was significant.
Early Abuse in Nonmanic Depression With Reversed Features
To extend the results described above, we decided to add a fifth question post hoc, i.e., when only depressed subjects without a history of a manic episode are considered, is having one or more episodes of depression with reversed features associated with childhood abuse? We hoped to remove the data of subjects with probable anergic bipolar depression (35) in this analysis, creating a more homogeneous “nonmanic” group with reversed features.
With respect to physical abuse, a strong main effect of group was once again found (F=15.74, df=1, 534, p<0.001), indicating that depression with reversed features is associated with early traumatic experiences independent of lifetime mania. For sexual abuse, removal of manic patients’ data accentuated the differences between the groups with and without reversed-symptom episodes (F=15.72, df=1, 526, p<0.001) despite the decrease in sample size. The main effect of female gender was significant for sexual abuse (F=20.21, df=1, 526, p<0.001); the group-by-gender interactions were nonsignificant.
DISCUSSION
The current study is the first to assess the relationship between childhood abuse and particular expressions of major depression in later years. We found that for both men and women, having a childhood history of either physical or sexual abuse was associated with a higher risk of depressive episodes with reversed neurovegetative features, whether or not individuals with mania were considered. A strong relationship between mania and childhood physical abuse was also found. These are novel findings and suggest a potential focus for future work on the transduction of early stress into affective disturbances over the life span. Clinically, the current findings validate the subtyping of depression based on symptom profiles and help to identify a subgroup of individuals who are more likely to require a multifaceted treatment approach. The results may also help explain why many depressed patients with reversed symptoms have a particularly chronic course (27, 36–38). Given the personal and societal costs of affective disorders (1–5), these results emphasize the need for early identification and intervention for children and adolescents at high risk for abuse.
Reversed Neurovegetative Features of Depression and Early Trauma
The most striking finding in this study was a strong relationship between early traumatic experiences and depression with reversed neurovegetative features. This finding was not simply attributable to reversed symptoms in the context of manic depression, since removal of data on manic subjects actually accentuated this association. This finding was also not solely attributable to severity of psychopathology, since having an episode of typical depressive symptoms was not associated with increased rates of abuse, even in comparison with the neither-symptom group; typical symptoms of depression are generally associated with a high degree of psychiatric morbidity (27).
Understanding the long-term vulnerability factors that promote depression over the life span is a high priority for both researchers and clinicians. Models of affective disorders that link stressful life experiences, neurodevelopment, and psychopathology (6, 7) have been a major step forward in this regard. The current findings, by linking a set of early experiences to particular expressions of psychopathology in later years, provide at least preliminary support for such models. Prior research showing that depression with reversed features had an early age at onset (37–42) and frequent exacerbations (27, 36–38) is also highly congruent with these models.
Why might early trauma predispose more to reversed neurovegetative symptoms than to other expressions of depression? While it is premature to speculate pending further research, there is a large body of work with animals indicating that early experience can have a profound effect on the development and expression of neurobiological systems and the behaviors they mediate (43–46). This work may extend to human psychiatric populations, including individuals with a history of child abuse (47). More research is needed to explore the possible links between early trauma, particular biological and/or psychological markers, and the clinical expression of depression over the life span.
Manic Depression and Early Trauma
In trying to understand the nature of the relationship between early trauma and manic depression in particular, a number of sociological and pathophysiological issues must be considered. In families with one or more parents with bipolar disorder, one must consider the combined effects of genetic loading for psychopathology and the likelihood of abuse based on parental illness and/or a disruptive family environment. In light of recent reports of very high comorbidity rates for attention deficit disorder with hyperactivity and adolescent mania (25, 48–51), one possible interpretation of the current data is that many children who later develop bipolar disorder act in an impulsive manner that could promote harsh discipline and physical abuse from caregivers (52, 53). It is possible that early trauma is associated with exaggerated cycles of high and low arousal that contribute to mood instability over time by permanently changing brain physiology (6, 54–56). Whatever the direction of causality linking physical abuse to mania, the current results strongly support the need for early identification and intervention in this high-risk group.
Limitations of the Study
A number of methodological limitations merit consideration. While our use of a community-based sample may have helped avoid the bias inherent in clinic-based research, all of the information gathered was based on retrospective reporting, a potential problem for lifetime diagnoses and for the disclosure of information regarding abuse. However, a recent review by Rutter and Maughan (57) suggests that retrospective self-reports regarding abuse are more likely to be biased toward underreporting than exaggeration.
The choice of diagnostic instrument may be problematic. Of particular relevance to the current study, the Composite International Diagnostic Interview is limited by its failure to diagnose either bipolar II disorder or cyclothymia. If many individuals with reversed neurovegetative symptoms do in fact fall into this “soft bipolar” subcategory (58), the current data would likely underestimate the link between early trauma and bipolar-spectrum mood disorders.
Notwithstanding these potential limitations, the current project is the first to link early abusive experiences to particular neurovegetative symptoms of depression and/or mania in adults. Much work is needed to replicate these findings and to work out the developmental pathways that connect early traumatic experiences to particular symptom patterns over time. In future work in this area, it will be important to consider intervening variables, such as social class and support systems, and whether particular types of abuse lead to unique expressions of depression.
At a clinical level, our data emphasize the importance of routine inquiry regarding early trauma and specific neurovegetative symptom clusters in the assessment of depressive illness. This approach may help clinicians identify patients more likely to require multimodal treatment strategies and thus help decrease the morbidity associated with mood disorders over the life span.
APPENDIX 1. Physical and Sexual Abuse Items on the Self-Report Questionnaire Addendum to the Ontario Health Survey
When you were growing up, how often did any adult do any of the things on this list to you?
Pushed, grabbed, or shoved you
Threw something at you
Slapped or spanked you
Kicked, bit, or punched you
Hit you with something
Choked, burned, or scalded you
Physically attacked you in some other way
When you were growing up, did any adult ever do any of these things to you against your will?
Exposed themselves to you more than once
Threatened to have sex with you
Touched the sex parts of your body
Tried to have sex with you or sexually attacked you
Answer: often, sometimes, rarely, or never.
Answer: yes or no.
Received Sept. 9, 1997; revisions received April 8 and May 28, 1998; accepted June 26, 1998. From the Clarke Division of the Centre for Addiction and Mental Health and the Department of Psychiatry, University of Toronto; and the Centre de Recherche Fernand-Seguin, Hôpital Louis-H. Lafontaine, Department of Psychiatry, University of Montreal. Address reprint requests to Dr. Levitan, Clarke Division of CAMH, Room 1135, 250 College St., Toronto, Ont., Canada M5T 1R8.
 |
 |
 |
 |
 |
1. Regier DA, Boyd JH, Burke JD Jr, Rae DS, Myers JK, Kramer M, Robins LN, George LK, Karno M, Locke BZ: One-month prevalence of mental disorders in the United States: based on five Epidemiologic Catchment Area sites. Arch Gen Psychiatry 1988; 45:977–986Crossref, Medline, Google Scholar
2. Wells KB, Stewart A, Hays RD, Burnam MA, Rogers W, Daniels M, Berry S, Greenfield S, Ware J: The functioning and well-being of depressed patients: results from the Medical Outcomes Study. JAMA 1989; 262:914–919Crossref, Medline, Google Scholar
3. Fawcett J, Scheftner W, Clark D, Hedeker D, Gibbons R, Coryell W: Clinical predictors of suicide in patients with major affective disorders: a controlled prospective study. Am J Psychiatry 1987; 144:35–40Link, Google Scholar
4. Klerman GL, Weissman MM: The course, morbidity, and costs of depression. Arch Gen Psychiatry 1992; 49:831–834Crossref, Medline, Google Scholar
5. Keller MB, Lavori PW, Mueller TI, Endicott J, Coryell W, Hirschfeld RMA, Shea MT: Time to recovery, chronicity, and levels of psychopathology in major depression: a five-year prospective follow-up of 431 subjects. Arch Gen Psychiatry 1992; 49:809–816Crossref, Medline, Google Scholar
6. Post RM: Transduction of psychosocial stress into the neurobiology of recurrent affective disorder. Am J Psychiatry 1992; 149:999–1010Link, Google Scholar
7. Duman RS, Heninger, GR, Nestler EJ: A molecular and cellular theory of depression. Arch Gen Psychiatry 1997; 54:597–606Crossref, Medline, Google Scholar
8. Green A: Core affective disturbance in abused children. J Am Acad Psychoanal 1981; 9:435–446Crossref, Medline, Google Scholar
9. Kazdin AE, Moser J, Colbus D, Bell R: Depressive symptoms among physically abused and psychiatrically disturbed children. J Abnorm Psychol 1985; 94:298–307Crossref, Medline, Google Scholar
10. Browne A, Finkelhor D: Impact of child sexual abuse: a review of the research. Psychol Bull 1986; 99:66–77Crossref, Medline, Google Scholar
11. Allen DM, Tarnowski KJ: Depressive characteristics of physically abused children. J Abnorm Child Psychol 1989; 17:1–11Crossref, Medline, Google Scholar
12. Briere JN: Child Abuse Trauma. London, Sage Publications, 1992, pp 17–78Google Scholar
13. Rosenthal PA, Rosenthal S: Suicidal behavior by preschool children. Am J Psychiatry 1984; 141:520–525Link, Google Scholar
14. Kashani JH, Carlson GA: Seriously depressed preschoolers. Am J Psychiatry 1987; 144:348–350Link, Google Scholar
15. Sedney MA, Brooks B: Factors associated with a history of childhood sexual experience in a non-clinical female population. J Am Acad Psychiatry 1984; 23:215–218Crossref, Medline, Google Scholar
16. Bryer JB, Nelson BA, Miller JB, Krol PA: Childhood sexual and physical abuse as factors in adult psychiatric illness. Am J Psychiatry 1987; 144:1426–1430Link, Google Scholar
17. Mullen PE, Romans-Clarkson SE, Walton VA, Herbison CP: Impact of sexual and physical abuse on women’s mental health. Lancet 1988; 1:841–845Crossref, Medline, Google Scholar
18. Brown BE, Garrison CJ: Patterns of symptomatology of adult women incest survivors. West J Nurs Res 1990; 12:587–600Crossref, Medline, Google Scholar
19. Bifulco A, Brown GW, Adler Z: Early sexual abuse and clinical depression in adult life. Br J Psychiatry 1991; 159:115–122Crossref, Medline, Google Scholar
20. Brown GR, Anderson B: Psychiatric morbidity in adult inpatients with childhood histories of sexual and physical abuse. Am J Psychiatry 1991; 148:55–61Link, Google Scholar
21. Pribor EF, Dinwiddie SH: Psychiatric correlates of incest in childhood. Am J Psychiatry 1992; 149:52–56Link, Google Scholar
22. Glod CA: Long-term consequences of childhood physical and sexual abuse: Arch Psychiatr Nurs 1993; 7:163–173Google Scholar
23. Hall LA, Sachs B, Rayens MK, Lutenbacher M: Childhood physical and sexual abuse: their relationship with depressive symptoms in adulthood. Image 1993; 25:317–323Google Scholar
24. Boudewyn AC, Liem JH: Childhood sexual abuse as a precursor to depression and self-destructive behavior in adulthood. J Trauma Stress 1995; 8:445–459Crossref, Medline, Google Scholar
25. Winokur G, Coryell W, Endicott J, Akiskal H: Further distinctions between manic-depressive illness (bipolar disorder) and primary depressive disorder (unipolar depression). Am J Psychiatry 1993; 150:1176–1181Link, Google Scholar
26. Quitkin FM, Stewart JW, McGrath PJ, Liebowitz MR, Harrison WM, Tricamo E, Klein DF, Rabkin JG, Markowitz JS, Wager SG: Phenelzine versus imipramine in the treatment of probable atypical depression: defining symptom boundaries of selective MAOI responders. Am J Psychiatry 1988; 145:306–311Link, Google Scholar
27. Kendler KS, Eaves LJ, Walters EE, Neale MC, Heath AC, Kessler RC: The identification and validation of distinct depressive syndromes in a population-based sample of female twins. Arch Gen Psychiatry 1996; 53:391–399Crossref, Medline, Google Scholar
28. Weissman MM, Klerman GL: Sex differences and the epidemiology of depression. Arch Gen Psychiatry 1977; 34:98–111Crossref, Medline, Google Scholar
29. MacMillan HL, Fleming JE, Trocme N, Boyle MH, Wong M, Racine YA, Beardslee WR, Offord DR: Prevalence of child physical and sexual abuse in the community. JAMA 1997; 275:131–135Crossref, Google Scholar
30. Boyle MH, Offord DR, Campbell D, Catlin G, Goering P, Lin E, Racine YA: Mental Health Supplement to the Ontario Health Survey: methodology. Can J Psychiatry 1996; 41:549–558Crossref, Medline, Google Scholar
31. Wittchen H-U: Reliability and validity studies of the WHO Composite International Diagnostic Interview (CIDI): a critical review. J Psychiatr Res 1994; 28:57–84Crossref, Medline, Google Scholar
32. Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen H-U, Kendler KS: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry 1994; 51:8–19Crossref, Medline, Google Scholar
33. Bagley C: Prevalence and correlates of unwanted sexual acts in childhood in a national Canadian sample. Can J Public Health 1989; 80:295–296Medline, Google Scholar
34. Levitan RD, Lesage A, Parikh SV, Goering P, Kennedy SH: Reversed neurovegetative symptoms of depression: a community study of Ontario. Am J Psychiatry 1997; 154:934–940Link, Google Scholar
35. Thase ME, Himmelhoch JM, Mallinger AG, Jarrett DB, Kupfer DJ: Sleep EEG and DST findings in anergic bipolar depression. Am J Psychiatry 1989; 146:329–333Link, Google Scholar
36. Asnis GM, McGinn LK, Sanderson WC: Atypical depression: clinical aspects and noradrenergic function. Am J Psychiatry 1995; 152:31–36Link, Google Scholar
37. Davidson J, Zisook S, Giller E, Helms M: Symptoms of interpersonal sensitivity in depression. Compr Psychiatry 1989; 30:357–368Crossref, Medline, Google Scholar
38. Stewart JW, McGrath PJ, Rabkin JG, Quitkin FM: Atypical depression: a valid clinical entity? Psychiatr Clin North Am 1993; 16:479–495Google Scholar
39. Klein DF, Gittelman R, Quitkin FM, Rifkin A: Diagnosis and Drug Treatment of Psychiatric Disorders: Adults and Children. Baltimore, Williams & Wilkins, 1980, pp 243–246Google Scholar
40. Davidson JRT, Miller RD, Turnbull CD, Sullivan JL: Atypical depression. Arch Gen Psychiatry 1982; 39:527–534Crossref, Medline, Google Scholar
41. Horwath E, Johnson J, Weissman MM, Hornig CD: The validity of major depression with atypical features based on a community sample. J Affect Disord 1992; 26:117–126Crossref, Medline, Google Scholar
42. Pollitt J, Young J: Anxiety or masked depression? a study based on the action of monoamine oxidase inhibitors. Br J Psychiatry 1971; 119:143–149Crossref, Medline, Google Scholar
43. McKinney WT Jr, Suomi SJ, Harlow HF: Depression in primates. Am J Psychiatry 1971; 127:1313–1320Link, Google Scholar
44. Post RM, Weiss SR: Emergent properties of neural systems: how focal molecular neurobiological alterations can affect behavior. Development and Psychopathology 1997; 9:907–929Crossref, Medline, Google Scholar
45. Liu D, Diorio J, Tannenbaum B, Caldji C, Francis D, Freedman A, Sharma S, Pearson D, Plotsky PM, Meaney MJ: Maternal care, hippocampal glucocorticoid receptors, and hypothalamic-pituitary-adrenal responses to stress. Science 1997; 277:1659–1662Crossref, Medline, Google Scholar
46. Zaharia MD, Kulczycki J, Shanks N, Meaney MJ, Anisman H: The effects of early post-natal stimulation on Morris water-maze acquisition in adult mice: genetic and maternal factors. Psychopharmacology (Berl) 1996; 128:227–239Crossref, Medline, Google Scholar
47. Stein MB, Yehuda R, Koverola C, Hanna C: Enhanced dexamethasone suppression of plasma cortisol in adult women traumatized by childhood sexual abuse. Biol Psychiatry 1997; 42:680–686Crossref, Medline, Google Scholar
48. Strober M, Morrell W, Burroughs J, Lampert C, Danforth H, Freeman R: A family study of bipolar I disorder in adolescence: early onset of symptoms linked to increased familial loading and lithium resistance. J Affect Disord 1988; 15:255–268Crossref, Medline, Google Scholar
49. West SA, McElroy SL, Strakowski SM, Keck PE Jr, McConville BJ: Attention deficit hyperactivity disorder in adolescent mania. Am J Psychiatry 1995; 152:271–273Link, Google Scholar
50. Wozniack J, Biederman J, Kiely K, Ablon JS, Faraone SV, Mundy E, Mennin D: Mania-like symptoms suggestive of childhood-onset bipolar disorder in clinically referred children. J Am Acad Child Adolesc Psychiatry 1995; 34:867–876Crossref, Medline, Google Scholar
51. Wozniack J, Biederman J, Mundy E, Mennin D, Faraone SV: A pilot family study of childhood-onset mania. J Am Acad Child Adolesc Psychiatry 1995; 34:1577–1583Crossref, Medline, Google Scholar
52. Friedrich WN, Boriskin JA: The role of the child in abuse: a review of the literature. Am J Orthopsychiatry 1976; 46:580–590Crossref, Medline, Google Scholar
53. Engfer A, Schneewind KA: Causes and consequences of harsh parental punishment: an empirical investigation in a representative sample of 570 German families. Child Abuse Negl 1982; 6:129–139Crossref, Medline, Google Scholar
54. Field T: Attachment as psychobiological attunement: being on the same wavelength, in Psychobiology of Attachment and Separation. Edited by Reite M, Field T. Orlando, Fla, Academic Press, 1985, pp 431–432Google Scholar
55. van der Kolk BA: The trauma spectrum: the interaction of biological and social events in the genesis of the trauma response. J Trauma Stress 1988; 1:272–290Crossref, Google Scholar
56. Green AH: Child abuse, neglect and depression, in Depression in Children and Adolescents: Monographs in Clinical Pediatrics, vol 6. Edited by Koplewicz HS, Klass E. Philadelphia, Harwood Academic/Gordon and Breach, 1993, pp 55–62Google Scholar
57. Rutter M, Maughan B: Retrospective reporting of childhood adversity: issues in assessing long-term recall. J Personality Disorders 1997; 11:19–33Crossref, Medline, Google Scholar
58. Perugi G, Akiskal HS, Lattenzi L, Cecconi C, Mastrocinque A, Patronelli S, Vignoli S, Bemi E: The high prevalence of “soft” bipolar (II) features in atypical depression. Compr Psychiatry 1998; 39:63–71Crossref, Medline, Google Scholar



