George Engel, M.D. (1913–1999)
George Engel’s basic convictions are best known from his “biopsychosocial model,” a general theory of illness and healing (1–3). When these ideas were forming in the early 1950s, he had already made a name for himself in neurology and medicine through his studies of fainting, delirium, and ulcerative colitis and was beginning the studies that would document the correlation of loss with the onset of a variety of diseases.
George Engel’s own story, his biopsychosocial profile, highlights the influence of his family—especially his uncle and distinguished biomedical stalwart, Emanuel Libman, and his identical twin, Frank, also a physician, whose death in 1963 imposed a deeply personal sense of loss and self-awareness (4). Dr. Engel’s profile would reflect the physiological orientation of his basic training and early research with Soma Weiss, Ralph Gerard, and, in Leningrad, Alexander Gurwitsch.
Dr. Weiss was his postgraduate mentor at Peter Bent Brigham in 1941. He introduced him to John Romano, M.D., a young psychiatrist; they worked jointly on studies of delirium. He joined with Romano, first tentatively and then wholeheartedly, at Harvard, then in Cincinnati, and finally in Rochester.
An early effect of the Romano-Engel combination was a revolution in medical education at Rochester, bringing together the usual medical-psychiatric distinctions, to the mutual advantage of all (5).
Psychoanalysis and Dr. Engel’s studies with Theresa Benedek played a part in his broadened syncretic view, providing a concept of symbolic use of the body for the expression of fantasy, conflict, or affect. Unlike Franz Alexander, he appreciated that autonomic functioning could serve as an avenue of symbolic expression, an awareness that led to his own and his colleagues’ studies of disease onset and exacerbation.
The Monica case study is probably best remembered by the generations of physicians influenced by George Engel (6, 7). Who can forget the movies of Monica, an infant with esophageal atresia who was fed by gastrostomy, Franz Reichsman (the “friendly doctor”), and George Engel (the “somber stranger”)? We recall her wriggling excitement, beaming smile, and the gastric juice gushing from her gastrostomy tube when Franz approached and her sudden, dramatic quietude, bodily withdrawal, and dry gastric mucosa when George appeared. It was and is a classic case study, followed from 1953 when Monica was 1 year old until Dr. Engel’s death 46 years later. By then Monica was a grandmother, and the family epic—or portions of it—was forever captured on film. From this study came the familiar phrases “conservation-withdrawal,” “giving up–given up,” and “helplessness/hopelessness affect” (8).
In the 1980s and early 1990s, biopsychosocial medicine became the watchword of progressive unification of the medical and behavioral sciences, including psychiatry, in a search for etiological and preventive factors in human health and disease (9). Today that goal has been replaced by neuroscience and a return to descriptive psychiatry.
In his later years, George Engel never lost his good humor, his bite, or his generosity (10). He loved and was deeply loved by the students and physicians who worked and learned with him. He would appreciate the fact that some of us have taken on a bit of his flintiness, attempt his wry humor, and retain his determination to see our patients as “united, biopsychosocial persons” rather than as “biomedical persons” divorced from their psychological and social dimensions.
Address correspondence and reprint requests to Dr. Dowling, 22300 S. Woodland Rd., Beachwood, OH 44122-3067; [email protected] (e-mail). The photograph was provided courtesy of the University of Rochester.
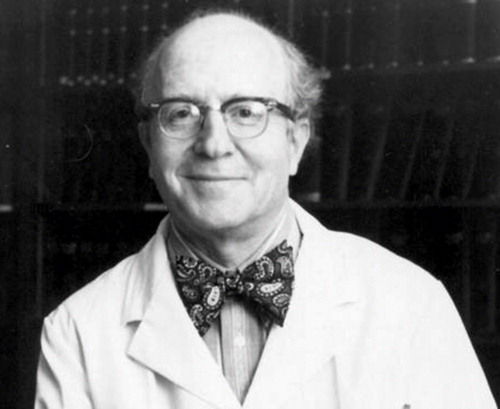
George Engel
1. Engel GL: The need for a new medical model: a challenge for biomedicine. Science 1977; 196:129–136Crossref, Medline, Google Scholar
2. Engel GL: The clinical application of the biopsychosocial model. Am J Psychiatry 1980; 137:535–544Link, Google Scholar
3. Engel GL: From biomedical to biopsychosocial: being scientific in the human domain. Psychosomatics 1997; 38:521–528Crossref, Medline, Google Scholar
4. Engel GL: The death of a twin: mourning and anniversary reactions—fragments of 10 years of self-analysis. Int J Psychoanal 1975; 56:23–40Medline, Google Scholar
5. Brown T: George Engel and Rochester’s biopsychosocial tradition: historical and developmental perspectives (2000), in The Biopsychosocial Approach: Past, Present, Future. Edited by Frankel RM, Quill TE, McDaniel SH. Rochester, NY, University of Rochester Press, 2003, pp 199–218Google Scholar
6. Engel GL, Reichsman F, Segal HL: A study of an infant with a gastric fistula, I: behavior and the rate of total hydrochloric acid secretion. Psychosom Med 1956; 18:374–398Crossref, Medline, Google Scholar
7. Engel GL, Reichsman F: Spontaneous and experimentally induced depressions in an infant with a gastric fistula. J Am Psychoanal Assoc 1956; 4:428–452Crossref, Medline, Google Scholar
8. Engel GL: A life setting conducive to illness. Ann Intern Med 1968; 69:293–300Crossref, Medline, Google Scholar
9. Frankel RM, Quill TE, McDaniel SH (eds): The Biopsychosocial Approach: Past, Present, Future. Rochester, NY, University of Rochester Press, 2003Google Scholar
10. Engel PA: George L Engel, MD, 1913–1999: remembering his life and work; rediscovering his soul. Psychosomatics 2001; 42:94–99Crossref, Medline, Google Scholar



