The Psychological Impact of Terrorism: An Epidemiologic Study of Posttraumatic Stress Disorder and Associated Factors in Victims of the 1995–1996 Bombings in France
Abstract
OBJECTIVE: A wave of bombings struck France in 1995 and 1996, killing 12 people and injuring more than 200. The authors conducted follow-up evaluations with the victims in 1998 to determine the prevalence of and factors associated with posttraumatic stress disorder (PTSD). METHOD: Victims directly exposed to the bombings (N=228) were recruited into a retrospective, cross-sectional study. Computer-assisted telephone interviews were conducted to evaluate PTSD, per DSM-IV criteria, and to assess health status before the attack, initial injury severity and perceived threat at the time of attack, and psychological symptoms, cosmetic impairment, hearing problems, and health service use at the time of the follow-up evaluation. Factors associated with PTSD were investigated with univariate logistic regression followed by multiple logistic regression analyses. RESULTS: A total of 196 respondents (86%) participated in the study. Of these, 19% had severe initial physical injuries (hospitalization exceeding 1 week). Problems reported at the follow-up evaluation included attack-related hearing problems (51%), cosmetic impairment (33%), and PTSD (31%) (95% confidence interval=24.5%–37.5%). Results of logistic regression analyses indicated that the risk of PTSD was significantly higher among women (odds ratio=2.54), participants age 35–54 (odds ratio=2.83), and those who had severe initial injuries (odds ratio=2.79) or cosmetic impairment (odds ratio=2.74) or who perceived substantial threat during the attack (odds ratio=3.99). CONCLUSIONS: The high prevalence of PTSD 2.6 years on average after a terrorist attack emphasizes the need for improved health services to address the intermediate and long-term consequences of terrorism.
Initially described in wartime combatants, posttraumatic stress disorder (PTSD) is recognized as a common health problem associated with exposure to traumatic events such as natural catastrophes, motor vehicle accidents, assault, rape, and robbery (1, 2). Research over the past 15 years has also examined the psychological impact of terrorist acts such as hostage-taking, bombings, and shootings, but mainly in the short term (3–14). Estimates of the prevalence of PTSD after terrorist attacks range from 7.5% to 50% in the year after the event depending on the degree of victimization. Despite the increase in terrorist attacks worldwide, there is less evidence about the intermediate and long-term psychological consequences of terrorism, in particular PTSD, or about risk factors (5, 15–18). Studies of individuals incurring physical injuries should also be considered in addressing the long-term consequences of traumatic events. Research on victims of motor vehicle accidents shows a higher risk of PTSD, at rates that vary between 11% and 46%, 1–5 years postaccident (19, 20). While few studies have evaluated the long-term prevalence of PTSD among burn victims, it appears to fall between 22% and 45% after 1 year and has been reported to be higher after discharge than during hospitalization (21, 22).
Between July 25, 1995, and December 3, 1996, a wave of bombings attributed to Islamist fundamentalist networks hit France. Six struck Paris, and one struck the Lyon region; most occurred in metro stations. Twelve people were killed. Approximately 450 people applied for compensation from the French Terrorism Victim Guarantee Fund, a public guarantee fund to provide immediate financial aid and indemnification for health consequences and long-term sequelae. In 1998, we carried out a retrospective, cross-sectional epidemiologic study of terrorist bombing victims to evaluate the prevalence of and factors associated with PTSD.
Method
Subjects
The target population was made up of victims who had been directly exposed to the bombings. The French Terrorism Victim Guarantee Fund required every person applying for compensation to undergo an evaluation, carried out by independent experts, to confirm exposure to the bombing and to assess its health consequences. Participants were civilian, 18 years or older at the time of the event, spoke French, and could be reached by telephone. SOS Attentats, a nongovernmental organization created in 1986 to represent French victims of terrorism, identified the sampling frame and contacted the subjects. Of 450 subjects who applied for compensation, 222 (49.3%) chose not to undergo the French Terrorism Victim Guarantee Fund evaluation. Thus, 228 subjects remained for whom direct exposure was confirmed and who were contacted by SOS Attentats. In compliance with French law, details about the target population, data collection protocol, and procedures guaranteeing anonymity were reported to the Commission for Computer Privacy.
Data Collection
SOS Attentats sent an information letter to eligible participants 10 days before the study began. This was followed by a telephone invitation to participate in the study from a survey research institute. After describing the study to subjects, oral consent was obtained. Data were collected from September 16 to October 5, 1998, by computer-assisted telephone interviews conducted by 20 professional interviewers. The validity of using the telephone to assess anxiety-related stress disorders has been demonstrated in several studies (23, 24).
Measures
We defined PTSD at follow-up with a 22-item standardized instrument based on DSM-IV criteria (25–27). The structure and details of the instrument were very similar to the DSM-IV criteria—we simply broke some criteria down into several items to make them more understandable, as a back-translation confirmed. In a different, unpublished study, the reliability (Cronbach’s alpha=0.91), specificity (0.88), and sensitivity (0.73) of the instrument were confirmed in a group of 15 subjects with PTSD and 33 subjects with anxiety or depressive disorders; concurrent validity was compared with the judgment of an external clinical expert with substantial experience in the use of semistructured instruments (G. Sydor, Faculty of Psychology, Catholic University of Louvain, Belgium). Questions asked about symptoms associated with the event (e.g., “Do you currently have, without wanting them, upsetting memories about the attack?”), the duration of symptoms (more or less than 1 month), and repercussions on social and work life. Symptoms were rated on a 5-point intensity scale (0=not at all; 4=very much). A score of at least 3 defined the presence of a symptom.
Risk factors and health outcomes were also assessed by questionnaire. An initial gravity score was used to classify injury severity as mild (no hospitalization or surgery), moderate (initial hospitalization of less than 1 week or delayed/deferred surgery), or severe (initial hospitalization of more than 1 week). Perceived threat was coded as present for subjects who answered “yes” to at least one of two questions: Did you see people injured or killed during the attack? Did you feel you were dying during the attack? Hearing problems were assessed with four questions: Do you have hearing problems related to the attack? Have you seen a specialist in the past 4 weeks for a hearing problem related to the attack? Have you had buzzing or ringing in one or both ears in the past 4 weeks? Do you wear a hearing aid because of the attack? Hearing problems were coded as severe for subjects who answered yes to at least two questions and moderate for those who answered yes to one question. Four questions from the Burn-Specific Health Scale (28) were used to assess cosmetic impairment: Did the attack change your appearance to the point of interfering with your relationships? Would you like to forget that your appearance has changed? Do you feel that members of your family and friends are uncomfortable around you because of your appearance? Do you have the impression that people would not want to touch you? Questions were rated on a 5-point intensity scale (1=very much or all the time; 5=not at all or never). Cosmetic impairment was defined as a rating of 1, 2, or 3 in response to at least one of the questions. Psychiatric history was assessed with three questions. Two addressed the use of tranquilizers or sleep-inducing drugs for at least 6 months at any time before the attacks, and one addressed psychological problems: “Before the attack, had you been followed by a general practitioner, psychiatrist, psychologist or other psychotherapist for more than 6 months for a psychological problem?” A psychiatric history was defined as present if at least one of the three questions was answered positively.
Data Analysis
Factors associated with PTSD were investigated with univariate logistic regression followed by multiple logistic regression analyses. A forward/backward stepwise procedure was used to retain explanatory variables in the models. At each step, a new variable was entered in the model, which was then recomputed to test whether this variable should remain in the model (and another be withdrawn). This process continued until no variable in the equation could be removed and no variables not already in the equation could be added. The entry and exit thresholds for other variables were p=0.15 and p=0.05, respectively; we used the Hosmer and Lemeshow goodness-of-fit test and the c-index to evaluate the fit of the resulting model. We used SAS (version 6.12) software (SAS Institute, Cary, N.C.) for all statistical analyses.
Results
Of the 228 bombing victims who underwent medical evaluation for the French Terrorism Victim Guarantee Fund, 196 (86%) agreed to participate.
Respondent Characteristics
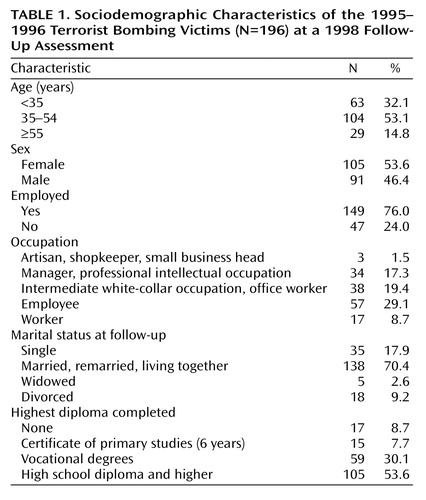
At the follow-up assessment, approximately three-quarters of the respondents (74%) were younger than 50 years old, were employed (76%), and were living with a partner (70%) (Table 1). More than half were women and had completed high school. The majority of respondents (83.7%) were injured in one of the two Paris subway bombings. The mean interval between the event and follow-up was 2.6 years (SD=0.6, range=1.8–3.2).
Prevalence of PTSD
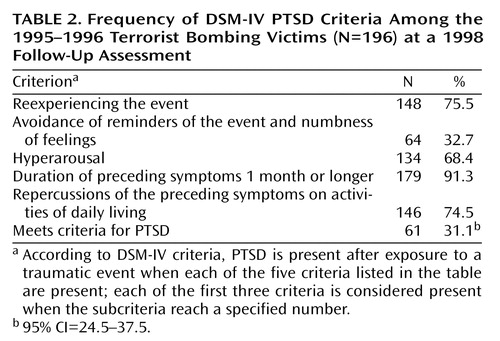
PTSD at the follow-up assessment was identified in 61 respondents (31.1%) (Table 2). The prevalence of PTSD in those with severe injuries was 50% (95% CI=34.1%–65.9%) and was lower in participants with moderate or mild injuries (27% [95% CI=17.5%–36.8%] and 26% [95% CI=16.2%–35.8%], respectively). The most and least frequent symptoms were reexperiencing the event (76%) and avoidance of reminders of the event and numbness of feelings (33%), respectively.
Risk Factors Associated With PTSD
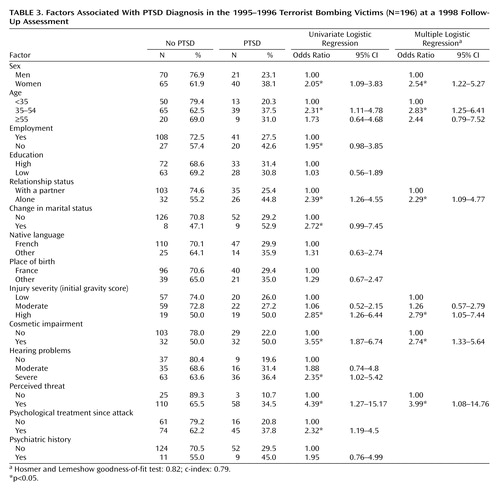
Results of univariate analyses indicated that the risk of PTSD was significantly higher for women; participants 35–54 years of age; those who were not working; those who lived alone; those whose marital situation had changed after the attack (divorce, widowed); those who had severe injuries, cosmetic impairment, or hearing problems; and those who reported a high perceived threat at the time of the attack or who had received treatment by a psychologist since the attack (Table 3). A history of psychiatric disorders was associated with a nonsignificant increase in the prevalence of PTSD. The prevalence of PTSD was not associated with the site of the attack or the number of years since the attack. Multiple logistic regression analyses showed a significant association between PTSD and age (35–54 years), sex, marital status, injury severity, cosmetic impairment, and perceived threat (Table 3). The odds ratios associated with these variables in the multiple logistic regression analysis did not substantially change from those in the univariate analysis. The Hosmer and Lemeshow goodness-of-fit test and the c-index show that the model fit the data well.
Discussion
This study surveyed 196 terrorist bombing victims (86% of eligible respondents), a relatively high number compared with most other studies focusing on the intermediate- and long-term psychological consequences of terrorist attacks (15, 16, 18, 29). According to the French Terrorism Victim Guarantee Fund, this group included almost all people injured during the 1995–1996 bombings.
The overall prevalence of PTSD was high (31.1%) at a mean of 2.6 years (SD=0.6) after the event. Comparisons with other studies focusing on intermediate- and long-term psychological consequences of terrorist attacks are difficult because of differences between populations, study methods, and measures (15, 16, 18, 29). However, the prevalence of PTSD was higher than the 18.1% prevalence rate in a study of victims of bombings between 1982 and 1987 in France (17). Most studies report that the prevalence of PTSD after a traumatic event decreases over time. Moreover, in a study of PTSD subjects 15 to 54 years of age in the U.S. general population, the median time to remission was 64 months in people who were not treated and 36 months in those who received treatment (1). One-third of respondents did not have a single remission in the 10 years following the onset of PTSD.
Our findings show a significant relation between injury severity and PTSD prevalence at a follow-up evaluation 2.6 years after the attacks. A relation between the nature and severity of injuries (including burns) and PTSD is reported only inconsistently. Some studies observe no such relation (3, 22, 30–33)—these authors stress instead the prominent role of subjective perception of stressors in mediating the development of PTSD. Others state that the severity of physical injury is one of the most reliable predictors of PTSD (10, 17, 34–36). Two hypotheses have been proposed. Solomon (34) hypothesized that more severe injuries may be associated with a more traumatic initial reaction that is also predictive of a PTSD that progresses more rapidly and lasts longer. Others have suggested that results may depend on the length of time elapsed since the accident, with extent of injury becoming a more important predictor over time (35); long-term disability due to severe injury serves as a constant reminder of the trauma and thereby tends to extend the duration of PTSD.
Our finding of an association between cosmetic impairment and PTSD is similar to the findings in a study of Japanese burn patients, which found that facial disfigurement was associated with PTSD only among women (29). This difference may be due to cultural differences or to the methods used to assess physical sequelae (clinical examination in the study by Fukunishi [29], self-report in ours). Cosmetic impairment may constantly remind the victims of the traumatic event, which may explain the poorer long-term adjustment and greater distress than for other respondents. Nonetheless, negative appraisal of cosmetic impairment may also be associated with the presence of depressive or PTSD symptoms that may increase patients’ focus on threats to their self-image (21). Our study design did not allow us to confirm a causal relation between PTSD and cosmetic impairment, but it raises a novel and potentially quite important hypothesis regarding this risk factor, which deserves further research.
We also found a higher prevalence of PTSD among respondents with moderate and mild injuries (27.2% and 26.0%, respectively) compared with the general population (1). This suggests that factors other than those associated with physical trauma, such as perceived threat, may play a role in the development of PTSD. The highest odds ratio (3.99) was found between perceived threat and PTSD; this result is supported by studies showing that factors such as the threat of death or the viewing of mutilated bodies are associated with the onset of PTSD (2, 37).
Our finding of a higher prevalence of PTSD in women is supported by results from several studies (1, 38–41). There is mixed support in the literature for our finding of an association between age and PTSD (40, 42, 43), although several studies have observed an increased risk of PTSD in 35–54-year-olds during natural catastrophes (43–45). These findings may be explained by the substantial economic consequences experienced by respondents with PTSD in this age group.
Failure of prior psychiatric history to be a strong predictor of PTSD may be related to the proxy variables used, which did not allow a thorough reconstruction of the nature and severity of past psychiatric disorders. It might also result from insufficient statistical power: relatively few subjects reported a past history of psychiatric disorders (11 subjects without and nine with PTSD).
The main limitation of this study is its retrospective design. The psychological consequences of the terrorist bombings were assessed through retrospective self-reports. Respondents’ recollections of the attack and its sequelae may have been influenced by their psychological state at follow-up (37, 46). However, it is unlikely that respondents overreported PTSD symptoms to seek financial gain. Participants were aware that all information they provided was confidential and would not be passed on to the French Terrorism Victim Guarantee Fund. They had already been recognized as victims and entered into the indemnification process by the French Terrorism Victim Guarantee Fund at the time of the study.
We have restricted our study to those who were directly exposed to the bombings; because of the high response rate, reconstruction of this group was substantially complete. Victims who were not directly exposed were excluded. It is very difficult to predict the consequence of this exclusion on the estimate of PTSD prevalence, since PTSD, perhaps less severe, may also occur in these subjects. Because our comparisons involved subjects with relatively similar experiences, the odds ratios associated with injury severity, cosmetic impairment, and perceived threat may be underestimated.
In conclusion, few studies have evaluated the long-term prevalence of PTSD several years after terrorist attacks. We surveyed a large sample of victims (N=196), evaluated psychological outcomes a mean of 2.6 years after the 1995–1996 attacks with rigorous measures, and found a high prevalence of PTSD in injured victims. Our findings suggest that psychological care for some victims may have been inadequate in the 2–3-year period after the event and thus highlights the need for improved health services to address the intermediate and long-term physical, psychological, and social consequences of terrorism. Risk factors associated with PTSD that may help to identify those at highest psychological risk include female gender, severe initial injuries, and high perceived threat. Finally, results suggest the role of cosmetic impairment in the persistence of PTSD.
 |
 |
 |
Received Oct. 28, 2002; revision received Sept. 9, 2003; accepted Nov. 20, 2003. From the Regional Health Observatory-INSERM U379, Marseille, France; the Conservatoire National des Arts et Métiers, Paris; the Health Services Research Unit, London School of Hygiene and Tropical Medicine, London, U.K.; McGill University, Jewish General Hospital, Montreal; Cemka-Eval, Bourg-la-Reine, France; and the Albert Chenevier and Henri Mondor University Hospital Center, Créteil—Paris XII Faculty of Medicine, Paris, France. Address reprint requests to Dr. Verger, Observatoire Régional de la Santé Paca, 23 rue Stanislas Torrents, 13006 Marseille, France. This study received financial support from the Directorate General of Health (a section of the Ministry of Health) and the Association “Les Gueules Cassées.” The authors thank the members of the scientific committee of the study; SOFRES Medical for undertaking the interviews; Anne Duburcq from EVAL for data analysis; Stéphane Hautecouverture, France Lert, and Anne Lowell for comments on draft versions of the manuscript; and Jo Ann Cahn for the translation.
1. Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB: Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 1995; 52:1048–1060Crossref, Medline, Google Scholar
2. Yehuda R: Post-traumatic stress disorder. N Engl J Med 2002; 346:108–114Crossref, Medline, Google Scholar
3. Curran PS, Bell P, Murray A, Loughrey G, Roddy R, Rocke LG: Psychological consequences of the Enniskillen bombing. Br J Psychiatry 1990; 156:479–482Crossref, Medline, Google Scholar
4. Loughrey GC, Bell P, Kee M, Roddy RJ, Curran PS: Post-traumatic stress disorder and civil violence in Northern Ireland. Br J Psychiatry 1988; 153:554–560Crossref, Medline, Google Scholar
5. Shalev AY: Posttraumatic stress disorder among injured survivors of a terrorist attack: predictive value of early intrusion and avoidance symptoms. J Nerv Ment Dis 1992; 180:505–509Crossref, Medline, Google Scholar
6. North CS, Smith EM, Spitznagel EL: Posttraumatic stress disorder in survivors of a mass shooting. Am J Psychiatry 1994; 151:82–88Link, Google Scholar
7. Somasundaram DJ: Post-traumatic responses to aerial bombing. Soc Sci Med 1996; 42:1465–1471Crossref, Medline, Google Scholar
8. Trappler B, Friedman S: Posttraumatic stress disorder in survivors of the Brooklyn Bridge shooting. Am J Psychiatry 1996; 153:705–707Link, Google Scholar
9. Amir M, Weil G, Kaplan Z, Tocker T, Witztum E: Debriefing with brief group psychotherapy in a homogenous group of non-injured victims of a terrorist attack: a prospective study. Acta Psychiatr Scand 1998; 98:237–242Crossref, Medline, Google Scholar
10. North CS, Nixon SJ, Shariat S, Mallonee S, McMillen JC, Spitznagel EL, Smith EM: Psychiatric disorders among survivors of the Oklahoma City bombing. JAMA 1999; 282:755–762Crossref, Medline, Google Scholar
11. Galea S, Ahern J, Resnick H, Kilpatrick D, Bucuvalas M, Gold J, Vlahov D: Psychological sequelae of the September 11 terrorist attacks in New York City. N Engl J Med 2002; 346:982–987Crossref, Medline, Google Scholar
12. Smith DW, Christiansen EH, Vincent R, Hann NE: Population effects of the bombing of Oklahoma City. J Okla State Med Assoc 1999; 92:193–198Medline, Google Scholar
13. Schuster MA, Stein BD, Jaycox LH, Collins RL, Marshall GN, Elliott MN, Zhou AJ, Kanouse DE, Morrison JL, Berry SH: A national survey of stress reactions after the September 11, 2001, terrorist attacks. N Engl J Med 2001; 345:1507–1512Crossref, Medline, Google Scholar
14. Schlenger WE, Caddell JM, Ebert L, Jordan BK, Rourke KM, Wilson D, Thalji L, Dennis JM, Fairbank JA, Kulka RA: Psychological reactions to terrorist attacks: findings from the national study of Americans’ reactions to September 11. JAMA 2002; 288:581–588Crossref, Medline, Google Scholar
15. Jehel L, Duchet C, Paterniti S, Consoli S, Guelfi J: Etude prospective de l’état de stress post-traumatique parmi les victimes d’un attentat terroriste. Encephale 2001; 27:393–400Medline, Google Scholar
16. Bouthillon-Heitzmann P, Crocq L, Julien H: Stress immédiat et séquelles psychiques chez les victimes d’attentats terroristes. Psychol Med (Paris) 1992; 24:465–470Google Scholar
17. Abenhaim L, Dab W, Salmi LR: Study of civilian victims of terrorist attacks (France 1982–1987). J Clin Epidemiol 1992; 45:103–109Crossref, Medline, Google Scholar
18. Desivilya HS, Gal R, Ayalon O: Extent of victimization, traumatic stress symptoms, and adjustment of terrorist assault survivors: a long-term follow-up. J Trauma Stress 1996; 9:881–889Crossref, Medline, Google Scholar
19. Blaszczynski A, Gordon K, Silove D, Sloane D, Hillman K, Panasetis P: Psychiatric morbidity following motor vehicle accidents: a review of methodological issues. Compr Psychiatry 1998; 39:111–121Crossref, Medline, Google Scholar
20. Mayou R, Tyndel S, Bryant B: Long-term outcome of motor vehicle accident injury. Psychosom Med 1997; 59:578–584Crossref, Medline, Google Scholar
21. Bryant RA: Predictors of post-traumatic stress disorder following burns injury. Burns 1996; 22:89–92Crossref, Medline, Google Scholar
22. Baur KM, Hardy PE, Van Dorsten B: Posttraumatic stress disorder in burn populations: a critical review of the literature. J Burn Care Rehabil 1998; 19:230–240Crossref, Medline, Google Scholar
23. Baruffol E, Verger P, Rotily M: L’utilisation du téléphone dans une enquête de santé mentale: analyse de l’impact du rang d’appel, des données manquantes et de l’effet “enquêteur.” Population 2001; 6:987–1010Crossref, Google Scholar
24. Rohde P, Lewinsohn PM, Seeley JR: Comparability of telephone and face-to-face interviews in assessing axis I and II disorders. Am J Psychiatry 1997; 154:1593–1598Link, Google Scholar
25. Sydor G, Philippot P: [Psychological consequences of the 1994 massacres in Rwanda]. Sante Ment Que 1996; 21:229–245 (French)Crossref, Medline, Google Scholar
26. Sydor G, Philippot P: Prévalence des symptômes de stress post-traumatique et intervention de prévention secondaire suite à une catastrophe humanitaire. Eur Rev Appl Psychol 1996; 46:269–275Google Scholar
27. Verger P, Hunault C, Rotily M, Baruffol E: [Risk factors for post-traumatic stress symptoms five years after the 1992 flood in the Vaucluse (France)]. Rev Epidemiol Sante Publique 2000; 48(suppl 2):2S44–2S53 (French)Google Scholar
28. Munster AM, Horowitz GL, Tudahl LA: The abbreviated Burn-Specific Health Scale. J Trauma 1987; 27:425–428Crossref, Medline, Google Scholar
29. Fukunishi I: Relationship of cosmetic disfigurement to the severity of posttraumatic stress disorder in burn injury or digital amputation. Psychother Psychosom 1999; 68:82–86Crossref, Medline, Google Scholar
30. Lyons HA: Terrorists’ bombing and the psychological sequelae. J Ir Med Assoc 1974; 67:15–19Medline, Google Scholar
31. Green B: Psychological research in traumatic stress: an update. J Trauma Stress 1994; 7:341–362Crossref, Medline, Google Scholar
32. Koren D, Arnon I, Klein E: Acute stress response and posttraumatic stress disorder in traffic accident victims: a one-year prospective, follow-up study. Am J Psychiatry 1999; 156:367–373Abstract, Google Scholar
33. Mayou R, Bryant B: Consequences of road traffic accidents for different types of road user. Injury 2003; 34:197–202Crossref, Medline, Google Scholar
34. Solomon Z: The impact of posttraumatic stress disorder in military situations. J Clin Psychiatry 2001; 62:11–15Medline, Google Scholar
35. Jeavons S: Predicting who suffers psychological trauma in the first year after a road accident. Behav Res Ther 2000; 38:499–508Crossref, Medline, Google Scholar
36. Blanchard EB, Hickling EJ, Taylor AE, Loos WR, Forneris CA, Jaccard J: Who develops PTSD from motor vehicle accidents? Behav Res Ther 1996; 34:1–10Crossref, Medline, Google Scholar
37. Baum A, Solomon SD, Ursano RJ, Bickman L, Blanchard E, Green BL, Keane TM, Laufer R, Norris F, Reid J, Smith EM, Steinglass P: Emergency/disaster studies: practical, conceptual, and methodological issues, in International Handbook of Traumatic Stress Syndromes. Edited by Wilson J, Raphael B. New York, Plenum, 1993, pp 125–134Google Scholar
38. Breslow N, Davis GC, Andreski P, Peterson EL, Schultz LR: Sex differences in posttraumatic stress disorder. Arch Gen Psychiatry 1997; 54:1044–1048Crossref, Medline, Google Scholar
39. Carr VJ, Lewin TJ, Webster RA, Hazell PL, Kenardy JA, Carter GL: Psychosocial sequelae of the 1989 Newcastle earthquake, I: community disaster experiences and psychological morbidity 6 months post-disaster. Psychol Med 1995; 25:539–555Crossref, Medline, Google Scholar
40. Gibbs MS: Factors in the victim that mediate between disaster and psychopathology: a review. J Trauma Stress 1989; 2:489–514Crossref, Google Scholar
41. Smith EM, North CS: Post-traumatic stress disorder in natural disasters and technological accidents, in International Handbook of Traumatic Stress Syndromes. Edited by Wilson JP, Raphael B. New York, Plenum, 1993, pp 405–419Google Scholar
42. Goenjian AK, Najarian LM, Pynoos RS, Steinberg AM, Manoukian G, Tavosian A, Fairbanks LA: Posttraumatic stress disorder in elderly and younger adults after the 1988 earthquake in Armenia. Am J Psychiatry 1994; 151:895–901Link, Google Scholar
43. Thompson MP, Norris FH, Hanacek B: Age differences in the psychological consequences of Hurricane Hugo. Psychol Aging 1993; 8:606–616Crossref, Medline, Google Scholar
44. Gleser GC, Green BL, Winget CN: Prolonged Psychosocial Effects of Disaster: A Study of Buffalo Creek. New York, Academic Press, 1981Google Scholar
45. Price J: Some age-related effects of the Brisbane floods. Aust NZ J Psychiatry 1978; 12:55–58Crossref, Medline, Google Scholar
46. Bromet E, Dew MA: Review of psychiatric epidemiologic research on disasters. Epidemiol Rev 1995; 17:113–119Crossref, Medline, Google Scholar



