Acute Stress Response and Posttraumatic Stress Disorder in Traffic Accident Victims: A One-Year Prospective, Follow-Up Study
Abstract
OBJECTIVE: This study was designed to assess the natural course of posttraumatic symptoms formation, as well as the degree to which acute stress reactions predict later posttraumatic stress disorder (PTSD) in injured traffic accident victims. METHOD: A prospective, 1-year follow-up study was carried out on 74 injured traffic accident victims and a comparison group of 19 patients who were hospitalized for elective orthopedic surgery. Participants were interviewed within the first week following the accident, and follow-up interviews were performed 1, 3, 6, and 12 months after the accident. At 12 months, a structured clinical interview was administered to determine a formal DSM-III-R diagnosis of PTSD. RESULTS: Twenty-four (32%) of the 74 traffic accident victims, but none of the 19 comparison subjects, met DSM-III-R criteria for PTSD at 1 year. Traffic accident victims who developed PTSD had higher levels of premorbid and comorbid psychopathology. Levels of posttraumatic symptoms were significantly higher from the outset in the subjects who developed PTSD and worsened progressively over the first 3 months, in contrast to subjects without PTSD, who manifested gradual amelioration of symptoms during this time. Existence of posttraumatic symptoms immediately after the accident was a better predictor of later PTSD than was accident or injury severity. CONCLUSIONS: In this study, a significant portion of injured traffic accident victims manifested PTSD 1 year after the event. The development of PTSD at 1 year can be predicted as early as 1 week after the accident on the basis of the existence and severity of early PTSD-related symptoms. However, the first 3 months following the accident appear to be the critical period for the development of PTSD. (Am J Psychiatry 1999; 156:367–373)
Posttraumatic stress disorder (PTSD) is a pervasive and devastating anxiety disorder, the lifetime prevalence of which, as assessed in several community-based studies, is estimated at 3%–8% (1, 2). These high prevalence rates, along with findings from recent studies, clearly indicate that PTSD can follow the experiencing of any major, life-threatening trauma, such as rape, physical assault, natural and industrial disasters, or traffic accidents. On the other hand, it is also well known today that exposure to trauma in itself is not sufficient for subsequent development of PTSD. Only low to moderate proportions of subjects exposed to trauma develop PTSD (e.g., 15.2% of Vietnam veterans [3], 23.6% of young urban adults [4], and 39% of traffic accident victims [5]). Moreover, the traumatic symptoms may at times improve or disappear altogether within a few months after the traumatic event, suggesting a self-limited process similar to spontaneous recovery from a depressive episode (6). The relative lack of knowledge about the nature of the relationship between PTSD and the traumatic stressor, and about the course of PTSD development, has refocused the attention of clinicians and researchers on the early course of PTSD, around and immediately after the exposure to trauma.
This renewed interest has led to numerous hypotheses about the possible interplay among pretraumatic vulnerabilities, objective and perceived trauma characteristics, and initial stress reactions in their contribution to the development of PTSD (7, 8). From a diagnostic point of view, this is reflected also by the introduction of acute stress disorder in DSM-IV. The essential diagnostic criterion of acute stress disorder, differentiating it from PTSD, is its temporal limitation to the first 4 weeks following exposure to trauma (criterion G). Otherwise, except for the addition of dissociative symptoms (criterion B), it shares with PTSD symptoms of reexperiencing, avoidance, and hyperarousal. A key question arising from the inclusion of acute stress disorder in DSM-IV concerns the degree to which it predicts later PTSD. To date, however, little prospective research has been conducted in order to assess the relationship between acute stress disorder and PTSD, as well as the validity of 1 month as the critical time in the transition from the former to the latter.
Longitudinal studies, starting immediately after exposure to the trauma and using repeated assessments at multiple points in time, are critically important for the illumination of the developmental course of PTSD. Moreover, this approach may be helpful in choosing between the two major alternative hypotheses regarding the relationship between acute stress reaction and PTSD: The first views PTSD as a failure to extinguish acute stress reaction, which is a normal, straightforward response to abnormal circumstances (9). The second claims that PTSD is, in fact, an abnormal response to traumatic events, not necessarily extreme in nature, occurring in predisposed individuals (10).
While not directly addressing the natural course of posttraumatic symptom formation, previously published prospective studies on trauma survivors significantly contributed to identification of risk factors and predictors of PTSD. Low socioeconomic and educational status, prior traumatization, previous axis I morbidity, and personality traits such as neuroticism (7, 11, 12) were identified as pretraumatic risk factors for PTSD. Perception of a direct threat to life (5), peritraumatic dissociation (8), and severity of physical injury (5, 13, 14), on the other hand, were each found to be significant peritraumatic predictors of PTSD.
Traffic accidents have emerged in recent years as a major cause of psychiatric morbidity in general (15, 16)and of PTSD in particular (5, 16, 17). In fact, motor vehicle accidents have been found to be the single leading cause of PTSD in the general population (18). Studies have shown that while acute stress symptoms exhibited by most traffic accident victims resolve within a few weeks, a significant portion of these subjects (10%–30%) still display PTSD symptoms 6 to 18 months after the accident(5, 17). Consistent with findings from prospective research on other traumatized populations, perceived threat to life and severity of physical injury were found to be the strongest and most reliable predictors of PTSD in traffic accident victims (5).
The present study was designed to assess, prospectively, the relationship between acute stress symptoms following exposure to trauma and the later development of PTSD. More specifically, our aims were to replicate previous estimates of PTSD prevalence in injured victims of traffic accidents and, more important, to delineate the developmental course of posttraumatic stress symptoms, as well as to identify the critical point in time in the transition from acute stress reaction to PTSD. In order to achieve these goals, posttraumatic symptoms were repeatedly assessed at five points in time during the first year following trauma. The formal diagnosis of acute stress disorder was not used in this study because it was designed and carried out before the introduction of DSM-IV. However, acute stress disorder key symptoms were assessed. The population of injured traffic accident victims was chosen because of its availability for immediate assessment soon after exposure to trauma.
METHOD
Participants
Participants included 99 traffic accident victims and 21 comparison subjects, who were followed up for 1 year between 1993 and 1996. All participants were recruited from three orthopedic wards (Rambam and Afula Medical Centers) to which they were admitted for medical care of their injuries, or elective surgery in the case of the comparison group. The elective surgery group was selected in order to control for possible hospitalization effects. All participants gave written informed consent after receiving a detailed explanation of the purpose and design of the study. Participants were considered eligible for the study group (traffic accident victims) if they were between the ages of 18 and 65 and had sustained mild to moderate physical injury because of traffic accidents, requiring hospitalization of at least 2 days. Participants were excluded if they had sustained head injury or showed evidence of brain damage, were in a coma or unconscious for more than 10 minutes before or during their emergency room admission, were actively treated for psychiatric disorder at the time of the accident, or were unable to communicate fluently in Hebrew. Screening for gross cognitive deficits was performed by using the Mini-Mental State examination (19).
The resultant group of traffic accident victims consisted of relatively young (mean age=27.5 years, SD=10.0), predominantly male (66.7%), Jewish (88.8%) individuals, fairly well educated (mean=12.3 years, SD=2.1) and from middle socioeconomic class backgrounds, as measured by their housing conditions (i.e., number of rooms per person) (mean=1.1 rooms, SD=0.7). The elective surgery subjects were slightly, but not significantly, older and more educated than the traffic accident victims. They averaged 32.0 years of age (SD=13.7) and had an average of 13.3 years of formal education (SD=2.3).
Procedure and Measures
Initial evaluation took place within the first week of hospitalization after the accident. Participants were asked to answer questions regarding their personal background (e.g., family status, country of origin, level of education) and to rate their experience of the traumatic event on several key dimensions, such as helplessness, loss of control, and perceived threat to life. In addition, an extensive battery of self-report questionnaires was administered, covering areas such as PTSD and general psychiatric symptoms, pain severity, quality of sleep, work and social adjustment, and life events. This battery was repeated with the traffic accident victims 1, 3, 6, and 12 months after the accident and 3 and 12 months after surgery in the case of the comparison group. Because this article’s focus is on the relationship between early stress symptoms and later development of PTSD, findings related to some of these measures will be reported elsewhere.
Severity of physical injury was assessed through use of the Abbreviated Injury Scale (20). Abbreviated Injury Scale ratings were determined by a surgeon experienced with traumatic injuries on the basis of examination of the patient and the medical records. Ratings between 0 and 6 were given for injuries to seven bodily areas and were then summed.
In order to assess PTSD symptoms, the Impact of Event Scale (21) and the DSM-III-R Scale for Severity of PTSD Symptomatology (22) were used. Because these scales have been used in previous studies of PTSD, they will not be described here. A broader spectrum of psychiatric symptoms was evaluated through use of the SCL-90 (23). Levels of general psychosocial and environmental stress in the year before and year after the accident were assessed with the Abbreviated Life Event Questionnaire (24). Both weighted (by severity of event) and simple life change unit scores were calculated.
At 12 months, the Structured Clinical Interview for DSM-III-R—Non-Patient Edition (SCID-NP) (25) was administered in order to reach a formal DSM-III-R diagnosis for PTSD. All participants were interviewed by an experienced clinical psychologist (I.A.) trained in the use of the SCID-NP. In addition to PTSD diagnosis, current and lifetime diagnoses (before and after the traffic accident) of the various DSM-III-R axis I disorders covered by the SCID-NP were determined as well. In order to ensure independence of PTSD diagnosis at 1 year from PTSD symptom measures collected earlier, the SCID-NP interviewer did not have access to the data collected at earlier time points.
Data Analysis
In order to examine relationships between continuous demographic and accident-related characteristics and the presence or absence of PTSD, a set of one-way univariate analyses of variance (ANOVAs) was performed (PROC GLM) (26). Chi-square tests were used for categorical variables (PROC FREQ) (26).
In order to compare the overall longitudinal pattern of clinical scale scores among the PTSD, non-PTSD, and comparison groups, a set of multivariate repeated measures ANOVAs (MANOVAs) (PROC GLM) (26) was used. Comparisons between successive points in time were performed by using the profile transformation. One-way univariate ANOVAs with Tukey post hoc tests were performed separately for individual points in time, only in the presence of a significant multivariate effect (alpha=0.05). This conservative approach to data analysis reduced the likelihood of a type I error.
Approximately 12% of the data on the clinical psychometric scales were missing because of logistical constraints. In order to apply multivariate techniques while retaining a reasonable group size, we input missing data points on the individual scale scores by setting them equal to the overall group means for that point in time. A set of t tests was used to ascertain that the data were missing in a random fashion in regard to criterion variables such as age, education, socioeconomic status, and clinical scale scores.
In order to assess the stability of posttraumatic symptoms over the various points in time, a set of within-measure correlations, between successive points in time and between each point in time and 1 year, was computed. Finally, in order to assess which variables best predict PTSD diagnosis at 1 year, a set of logistic regression analyses (PROC LOGISTIC) (26), with PTSD status as the dependent variable, was used.
RESULTS
PTSD 1 Year After the Accident
Seventy-four (75%) of the 99 traffic accident victims (who were mildly to moderately injured) and 19 (91%) of the 21 comparison subjects who initially volunteered to participate in the study completed the full 1-year follow-up. Twenty-four (32%) of the 74 traffic accident victims met DSM-III-R criteria for PTSD at the 12-month SCID-NP assessment, and 50 did not. None of the 19 comparison subjects was diagnosed with PTSD at the 1-year evaluation.
The three groups (i.e., traffic accident victims with and without PTSD and comparison subjects) did not differ significantly on any of the sociodemographic measures, such as age, gender, marital status, ethnicity, reported level of education, and socioeconomic status, as well as on amount or severity of life events in the year before the accident (table 1). The only significant difference was in the percentage of Israeli-born subjects, which was lower in the comparison group than in both traffic accident groups. Similarly, PTSD diagnosis among traffic accident victims was not significantly associated with any of the accident-related characteristics assessed in this study, including severity of injury, objective responsibility as judged by the police, subjective sense of guilt, and initiation of litigation (table 2).
The PTSD and non-PTSD groups exhibited different rates of psychiatric comorbidity. Sixteen (67%) of the 24 traffic accident victims who met diagnostic criteria for PTSD qualified also for other concurrent psychiatric diagnoses (11 for affective disorder and five for anxiety disorder), whereas only nine (18%) of the 50 non-PTSD traffic accident victims received another psychiatric diagnosis (six for affective disorder and three for anxiety disorder). This difference was statistically significant (Yates’s corrected χ2=15.1, df=1, p<0.001; odds ratio=9.1; 95% confidence interval=3.0–27.8). Diagnosis of PTSD at 1 year showed a trend toward a significant relationship with premorbid psychiatric history (Yates’s corrected χ2=2.7, df=1, p<0.10; odds ratio=3.1, 95% confidence interval=1.0–9.9). It was found, retrospectively, that eight (33%) of the traffic accident victims with PTSD had histories of premorbid psychiatric disorders (seven had affective disorder and one, anxiety disorder). Seven of these eight patients had a comorbid diagnosis at 1 year. Seven (14%) of the non-PTSD traffic accident victims were found to have a history of premorbid psychiatric disorders (four had affective disorder and three, anxiety disorder). Only one of these seven individuals received a psychiatric diagnosis at 1 year.
All 25 traffic accident victims and two comparison subjects who dropped out of the study did so after the initial evaluation during hospitalization. Dropping out was not significantly related to any of the sociodemographic measures, except for ethnicity; dropout traffic accident victims were significantly more likely to be Sephardic (60%) or Arab (28%) (χ2=22.8, df=6, p<0.001). Similarly, dropping out was not related to any of the accident variables, except for responsibility for the accident as determined by the police; dropout traffic accident victims were more likely to be either fully or partially responsible for the accident (81%) (χ2=29.2, df=4, p<0.001).
Longitudinal Course of PTSD Development
Figure 1 presents the development of posttraumatic as well as general psychiatric symptoms as measured by the DSM-III-R questionnaire, the Impact of Event Scale, and the SCL-90 in the three study groups over the multiple points of assessment. Visual inspection of figure 1 reveals opposite trends in the PTSD and non-PTSD groups on all three measures. The nature of these opposite trends is such that an initial, relatively small difference between the scores of the PTSD and non-PTSD groups on these scales appears to increase progressively over the first 3 months following the accident. No apparent difference is evident between the non-PTSD and comparison groups.
Quantitatively, a MANOVA for repeated measures revealed a significant group-by-time interaction for the total scores of both the DSM-III-R Questionnaire (Wilks’s lambda F=4.40, df=4, 69, p<0.005) and the Impact of Event Scale (Wilks’s lambda F=12.03, df=4, 69, p<0.0001). The main time contribution to the overall interaction effect of PTSD on DSM-III-R came from the second time interval, that is, the period from 1 month to 3 months (F=4.75, df=1, 72, p<0.05). Similarly, the main source for the interaction effect on the Impact of Event Scale score was also the second time interval (F=15.22, df=1, 72, p<0.0002). The difference between the two groups at time of initial assessment, 1 week after the accident, was significant for the DSM-III-R total score (F=12.54, df=1, 72, p<0.0007; 95% confidence interval=5.0–17.7) but not for the Impact of Event Scale total score (F=2.49, df=1, 72; 95% confidence interval=–1.3–11.2). However, there was a significant effect of later PTSD on Impact of Event Scale total scores at the 1-month assessment (F=7.17, df=1, 72, p<0.009; 95% confidence interval=1.8–12.1). Replication of these analyses through use of the three DSM-III-R subscales (i.e., reexperiencing, avoidance, and hyperarousal) and the two Impact of Event Scale subscales (i.e., intrusion and avoidance) yielded a similar pattern of results, with no major differences between the subscales.
Last, a MANOVA for repeated measures revealed a significant group-by-time interaction for the total score on the SCL-90 questionnaire (Wilks’s lambda, F=5.40, df=2, 71, p<0.006). The contribution to the overall interaction effect came from both the first time interval (the period between the first week and 3 months) (F=9.97, df=1, 72, p<0.002) and the second time interval (the period from 3 to 12 months) (F=6.53, df=1, 72, p<0.05).
Relationship Between Acute Stress Reaction and PTSD at 1 Year
Next, in order to examine the stability of stress symptoms along the course of the first year after the accident, we correlated DSM-III-R and Impact of Event Scale scores at each point in time, with scores for the next and last points in time, within the entire group. As seen in table 3, the between-time correlations increased progressively during the first 3 months after the accident and remained stable thereafter. Moreover, DSM-III-R and Impact of Event Scale scores at 3 months appear to be the best predictors of posttraumatic symptoms at 1 year.
In order to further examine the relationship between the different points in time and PTSD at 1 year, we performed a set of logistic regression analyses in which DSM-III-R and Impact of Event Scale scores from 1 week to 6 months were included as predictors of the presence or absence of PTSD at 1 year. The overall models, for both DSM-III-R and Impact of Event Scale scores, were highly significant (χ2=27.59, df=4, p<0.0001, and χ2=20.73, df=4, p<0.0005, respectively). When we tested each predictor, after adjusting for its scores at the other points in time, only month 6 DSM-III-R score was significant (χ2=4.26, df=1, p<0.05). Month 3 DSM-III-R and Impact of Event Scale scores showed a trend toward significance (χ2=2.74, df=1, p<0.09, and χ2=3.11, df=1, p<0.07, respectively). When DSM-III-R scores from all points in time were entered into a stepwise logistic regression, only month 3 and month 12 were selected for the model (χ2=5.17, df=1, p<0.02, and χ2=4.36, df=1, p<0.04, respectively). For Impact of Event Scale scores, only month 12 was included in the model (χ2=12.56, df=1, p<0.0004).
Last, we tested the diagnostic efficacy of the DSM-III-R questionnaire when treated as a dichotomous variable. Subjects were determined to have or not to have PTSD if the pattern of their answers to the DSM-III-R questionnaire did or did not meet the DSM-III-R criteria for PTSD. At 1 week, the DSM-III-R questionnaire correctly classified 70.3% of all subjects, including 70.8% of the PTSD patients (sensitivity) and 71.4% of the non-PTSD patients (specificity) (χ2=11.78, df=1, p<0.001). At 1 month, the overall accuracy was 70.6%, with 95.0% sensitivity and 60.4% specificity (χ2=17.59, df=1, p<0.001). At 3 months, the overall accuracy was 74.6%, with 89.5% sensitivity and 68.8% specificity (χ2=18.49, df=1, p<0.001).
DISCUSSION
In this study of 74 mildly to moderately injured traffic accident victims, 24 (32%) satisfied diagnostic criteria for PTSD 1 year after the accident. This figure is consistent with findings from previous prospective studies on other traumatized populations (8, 27), as well as with studies of traffic accident victims (5, 16, 17). Furthermore, the presence of additional axis I morbidity, primarily affective and anxiety disorders, in the PTSD (71%) and non-PTSD (14%) groups supports previous findings (15, 16) that suggest that psychiatric sequelae of traffic accidents are not limited to posttraumatic symptoms. In light of reports on high rates of comorbidity in PTSD patients (22, 28, 29), and spontaneous remission of PTSD symptoms in a significant portion of patients (6) these results highlight the need to further investigate, over longer periods of time, the relationship between PTSD and other psychiatric morbidity in traumatized subjects.
The only premorbid factor that, in the current study, was related to PTSD at 1 year was previous psychiatric morbidity, especially affective and anxiety disorders. These findings are in accordance with data from previous studies(5, 7) that found prior major depression to be an important risk factor for PTSD in traffic accident victims. Given that current views of anxiety and affective disorders link their onset to increased sensitivity to stressful life events, the development of PTSD in these subjects might reflect a diathesis to abnormal reactions to stress in general. In addition, this might account for the significantly different rates of comorbid disorders in the PTSD and non-PTSD groups.
The current data do not support a link between PTSD and major characteristics of the traumatic stressor itself. In contrast to previous studies (5, 7), but as in the study by Shalev et al. (8), trauma- and injury-related characteristics assessed in the present study, such as accident and injury severity and subjective perception of a threat to life, were not found to be associated with PTSD at 1 year. Considering the important implications of these results for the diagnosis of PTSD (the “criterion A” issue) and the equivocal findings in the literature, further investigation of the relationship between stressor characteristics and PTSD is warranted.
A major goal of this study was to examine prospectively the developmental course of PTSD formation in traffic accident victims throughout the first year after the accident. Our findings indicate a clear divergence of symptom profiles between traffic accident victims who did and did not meet diagnostic criteria for PTSD at 1 year. Three key features characterize these diverging trends. First, even though most subjects manifest acute stress symptoms immediately after the accident, their severity is significantly higher in the PTSD group. Second, this initial difference appears to intensify over the first 3 months, in that PTSD subjects show a marked and progressive worsening of symptoms, whereas non-PTSD subjects manifest gradual amelioration of symptoms to a level very similar to that of the comparison group. And last, during the period from 3 months to 1 year after the accident, distinct symptom levels in both groups seem to stabilize. The similarity between the symptom profiles of the non-PTSD and comparison groups suggests that hospitalization, in and of itself, was not responsible for PTSD.
Additional support for the importance of 3 months as a critical period for symptom crystallization was obtained from the peak of between-time correlations at this point in time. If true, these findings suggest that 3 months, rather than 1 month as reflected in the DSM-IV criterion for PTSD, might be a more appropriate cutoff for the transition from acute stress disorder to PTSD. In addition, the initial significant difference between the two groups supports the hypothesis that PTSD is an abnormal response to traumatic events in predisposed individuals (8). On the other hand, considering the gradual amelioration of symptoms in the non-PTSD group, the alternative hypothesis viewing PTSD as a failure to extinguish an initially normal response to a traumatic event (8) cannot be dismissed.
Our final goal in this study was to explore the diagnostic efficiency of early predictors for PTSD at 1 year. Using both the continuous and dichotomous approaches, we obtained relatively high sensitivity and specificity figures for the DSM-III-R questionnaire and, to a lesser degree, for the Impact of Event Scale. While firm conclusions regarding absolute levels of diagnostic accuracy cannot be drawn without cross-validation in an independent sample, these results clearly indicate that it is possible, as early as 1 week after the traumatic event, to detect subjects who will later develop PTSD.
The fact that formal diagnosis of PTSD was assessed only at 1 year limits our ability to address the issue of acute- versus delayed-onset PTSD in our group, namely, to identify subjects who were initially diagnosable but who later recovered or others who were initially free of symptoms but who were diagnosable at 1 year. However, the diagnostic efficiency results, as well as the high between-time correlations, suggest that the vast majority of PTSD subjects in our group (about 90%) had an acute rather than a delayed onset.
Another limitation of our findings relates to the fact that litigation status was only partially controlled for. This might be a potential confound. However, we believe that this could not account for the current results for several reasons. First, in Israel, all victims of traffic accidents, regardless of their legal responsibility, are entitled to free medical care and disability compensation. Thus, in actuality, all traffic accident victims, independent of their long-term morbidity, file litigation. This was true for our subjects as well (table 2). Second, our results show significant intergroup differences on some of the measures as early as 1 week after the accident, when none of the subjects was in a medical condition to obtain legal advice. Finally, while traditional views, dating back to Miller’s concept of “accident neurosis” (30), suggest a perpetuating role for litigation in the formation of PTSD, more recent studies (16, 31, 32) question this relationship, showing that litigation settlement does not result in improvement of posttraumatic stress symptoms in those who develop them.
In summary, the results of this study provide further support for the fact that injured victims of traumatic events, traffic accidents in our case, are at considerable risk for development of PTSD even when they are only mildly injured. Furthermore, those who develop PTSD can be identified shortly after the traumatic event, even though the optimal point for making a diagnosis of PTSD appears to be 3 months. Finally, given the high percentage of subjects who develop PTSD and the apparent feasibility of early diagnosis, the preventive efficacy of early pharmacological and psychotherapeutic intervention needs to be studied. This is particularly important given the chronic course that PTSD tends to follow.
Based on a thesis (Mr. Arnon, 1997) submitted in partial fulfillment of the requirements for the degree of doctor of sciences at the Technion-Israel Institute of Technology. Received Jan. 27, 1998; revision received June 25, 1998; accepted Aug. 25, 1998. From the Department of Psychiatry of the Rambam Medical Center and the B. Rappaport Faculty of Medicine, Technion, I.I.T., Haifa, Israel; and the Psychology Department, University of Haifa, Haifa, Israel. Address reprint requests to Dr. Klein, Department of Psychiatry, Rambam Medical Center, Haifa 31906, Israel. Supported by grants from the Chief Scientist of the Israel Ministry of Health and the Rehabilitation Department of the Israel Ministry of Defense. The authors thank H. Stein, M.D., D. Herer, M.D., C. Zinman, M.D., D. Reiss, M.D., and M. Rinot, M.D., for assistance in patient recruitment; N. Snow, M.A., for assistance in data collection; A. Cohen, Ph.D., for statistical consultation; and P. Lavie and Z. Solomon for comments on the manuscript.
 |
 |
 |
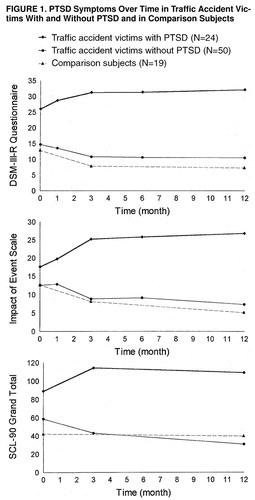
FIGURE 1. PTSD Symptoms Over Time in Traffic Accident Victims With and Without PTSD and in Comparison Subjects
1. Helzer JE, Robins LN, McEvoy L: Posttraumatic stress disorder in the general population: findings of the Epidemiologic Catchment Area survey. N Engl J Med 1987; 317:1630–1634Crossref, Medline, Google Scholar
2. Kessler R, Sonnega A, Bromet E, Nelson CB: Posttraumatic stress disorder in national comorbidity survey. Arch Gen Psychiatry 1995; 52:1048–1060Crossref, Medline, Google Scholar
3. Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, Weiss DS: Trauma and the Vietnam War Generation: Report of Findings From the National Vietnam Veterans Readjustment Study. New York, Brunner/Mazel, 1990Google Scholar
4. Breslau N, Davis GC, Anderski P, Peterson E: Traumatic events and posttraumatic stress disorder in urban population of young adults. Arch Gen Psychiatry 1991; 48:216–222Crossref, Medline, Google Scholar
5. Blanchard EB, Hickling EJ, Taylor AE, Loos WR, Forneris CA, Jaccard J: Who develops PTSD from motor vehicle accidents? Behav Res Ther 1996; 34:1–10Google Scholar
6. Rothbaum BO, Foa EB: Subtypes of posttraumatic stress disorder, in Posttraumatic Stress Disorder: DSM-IV and Beyond. Edited by Davidson JRT, Foa EB. Washington, DC, American Psychiatric Press, 1993, pp 23–35Google Scholar
7. McFarlane AC: The aetiology of post traumatic morbidity: predisposing, precipitating, and perpetuating factors. Br J Psychiatry 1989; 154:221–228Crossref, Medline, Google Scholar
8. Shalev AY, Peri T, Canetti MA, Schreiber S: Predictors of PTSD in injured trauma survivors: a prospective study. Am J Psychiatry 1996; 153:219–225Link, Google Scholar
9. Horowitz MJ: Stress response syndromes: character style and dynamic psychotherapy. Arch Gen Psychiatry 1974; 31:768–781Crossref, Medline, Google Scholar
10. Shalev AY: Stress versus traumatic stress: from acute homeostatic reactions to chronic psychopathology, in Traumatic Stress. Edited by van der Kolk BA, McFarlane AC, Weisaeth L. New York, Guilford Press, 1996, pp 77–101Google Scholar
11. Solomon Z: A three year prospective study of posttraumatic stress disorder in Israeli combat veterans. J Trauma Stress 1989; 2:59–73Crossref, Google Scholar
12. Green BL: Psychosocial research in traumatic stress: an update. J Trauma Stress 1994; 7:341–362Crossref, Medline, Google Scholar
13. Buydens-Branchy L, Noumair D, Branchy M: Duration and intensity of combat exposure and posttraumatic stress disorders among Vietnam veterans. J Nerv Ment Dis 1990; 178:582–587Crossref, Medline, Google Scholar
14. Pitman RK, Altman B, Macklin ML: Prevalence of posttraumatic stress disorder in wounded Vietnam veterans. Am J Psychiatry 1989; 146:667–669Link, Google Scholar
15. Malt UF: The long term consequences of accidental injury. Br J Psychiatry 1988; 153:810–818Crossref, Medline, Google Scholar
16. Mayou R, Bryant B, Duthie R: Psychiatric consequences of road traffic accidents. BMJ 1993; 307:647–651Crossref, Medline, Google Scholar
17. Green MM, McFarlane AC, Hunter CE, Griggs WM: Undiagnosed posttraumatic stress disorder following motor vehicles accidents. Med J Aust 1993; 159:529–534Crossref, Medline, Google Scholar
18. Blanchard EB, Hickling EJ: After the Crash: Assessment and Treatment of Motor Vehicle Accident Survivors. Washington, DC, American Psychological Association, 1993, pp 13–34Google Scholar
19. Folstein MF, Folstein SE, McHugh PR: “Mini-Mental State”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975; 12:189–198Crossref, Medline, Google Scholar
20. Association for the Advancement of Automotive Medicine: AIS: The Abbreviated Injury Scale, 1990 Revision. Des Plaines, Ill, AAAM, 1990Google Scholar
21. Horowitz MJ, Wilner N, Alvarez W: Impact of Event Scale: a measure of subjective stress. Psychosom Med 1979; 41:209–218Crossref, Medline, Google Scholar
22. Lerer B, Bleich A, Kotler M, Garb R, Hertzberg M, Levin B: Posttraumatic stress disorder in Israeli combat veterans: effect of phenelzine treatment. Arch Gen Psychiatry 1987; 44:976–981Crossref, Medline, Google Scholar
23. Derogatis L: The SCL-90 Manual: Scoring, Administration, and Procedure for the SCL-90. Baltimore, Md, John Hopkins School of Medicine, 1979Google Scholar
24. Holmes TH: The Social Readjustment Rating Scale (SRRS), in Abnormal Psychology and Modern Life. Edited by Coleman JC, Butcher JN, Carson RC. Chicago, Scott, Foresman, 1980, p 110Google Scholar
25. Spitzer RL, Williams JBW, Gibbon M, First MB: Structured Clinical Interview for DSM-III-R—Non-Patient Edition (SCID-NP, Version 1.0). Washington, DC, American Psychiatric Press, 1990Google Scholar
26. SAS/Stat User’s Guide: Changes and Enhancements Through Release 6.11. Cary, NC, SAS Institute, 1992Google Scholar
27. McFarlane AC: The phenomenology of posttraumatic stress disorder following a natural disaster. J Nerv Ment Dis 1988; 176:22–29Crossref, Medline, Google Scholar
28. Roszell DK, McFall ME, Malas KL: Frequency of symptoms and concurrent psychiatric disorder in Vietnam veterans with chronic PTSD. Hosp Community Psychiatry 1991; 42:293–296Abstract, Google Scholar
29. McFarlane AC: Multiple diagnoses in posttraumatic stress disorder in the victims of a natural disaster. J Nerv Ment Dis 1992; 180:498–504Crossref, Medline, Google Scholar
30. Miller H: Accident neurosis. BMJ 1961; 1:919–925, 992–998Crossref, Medline, Google Scholar
31. Grunert BK, Matloub HS, Sanger JR, Yousif NJ, Hetterman S: Effects of litigation on maintenance of psychological symptoms after severe hand injury. J Hand Surg 1991; 16:1031–1034Crossref, Medline, Google Scholar
32. Blanchard EB, Hickling EJ, Taylor AE, Buckly TC, Loos WR, Walsh J: Effects of litigation settlements on posttraumatic stress symptoms in motor vehicle accident victims. J Trauma Stress 1998; 11:337–354Crossref, Medline, Google Scholar



