Distress and Depression in Men Who Have Sex With Men: The Urban Men’s Health Study
Abstract
OBJECTIVE: This study estimates the prevalence of depression and describes the correlates and independent associations of distress and depression among U.S. men who have sex with men. METHOD: A household-based probability sample of men who have sex with men (N=2,881) was interviewed between 1996 and 1998 in four large American cities. With cutoff points of 15 and 22 for the Center for Epidemiological Studies Depression Scale, individual correlates and predictors of distress and depression were examined, and multinomial logistic regression was performed. RESULTS: The 7-day prevalence of depression in men who have sex with men was 17.2%, higher than in adult U.S. men in general. Both distress and depression were associated with lack of a domestic partner; not identifying as gay, queer, or homosexual; experiencing multiple episodes of antigay violence in the previous 5 years; and very high levels of community alienation. Distress was also associated with being of other than Asian/Pacific Islander ethnicity and experiencing early antigay harassment. Depression was also associated with histories of attempted suicide, child abuse, and recent sexual dysfunction. Being HIV positive was correlated with distress and depression but not significantly when demographic characteristics, developmental history, substance use, sexual behavior, and current social context were controlled by logistic regression. CONCLUSIONS: Rates of distress and depression are high in men who have sex with men. These high rates have important public health ramifications. The predictors of distress and depression suggest prevention efforts that might be effective when aimed at men who have sex with men.
Major depressive disorder and related mood disorders are important diagnoses, in terms of both their high prevalence and high cost. The National Health and Nutrition Examination Survey (1) estimates the lifetime prevalence of major depression in the United States at 7.0% and the current prevalence at 4.1%. The direct and indirect costs of major depression in the United States are estimated at between $26 and $43.7 billion per year (2), and major depression alone accounts for 11% of all years lived with disability worldwide (3). Groups in the United States with a high prevalence of depression include the chronically medically ill (4, 5), immigrants (6), and women, young adults, and people with less than a college education (7).
Accurate prevalence estimates require probability samples, a rarity in clinical research. Clinical research groups are usually convenience groups: people in treatment, either from a particular center or for a particular condition. Convenience groups are subject to selection bias, raising the question of whether similar people not in treatment, or in treatment elsewhere, would have similar characteristics. This is particularly problematic in trying to study a population defined by a nonclinical characteristic, such as men who have sex with men (Appendix 1). Hooker (8) showed that inferences based on psychoanalytic theory, derived from the treatment of men who have sex with men seeking to change their sexual behavior, were flawed by this bias; a convenience group of men who have sex with men not seeking treatment was no different from men in general. Similarly, men who have sex with men who were selected in gay bars have been shown to have a high rate of alcoholism compared to the general population (9). It is not surprising that examination of non-bar-based convenience groups of men who have sex with men eliminated this difference (10, 11).
While probability sampling eliminates many biases, probability samples of the general population in the United States have yielded small samples of men who have sex with men (12–14). These subsamples have been too small to power statistical analysis beyond prevalence estimates. The NEMESIS study (15), with 82 men who have sex with men within a total sample of 2,878 adult men, showed that Dutch men who have sex with men were nearly three times as likely to have a DSM-III-R-defined mood disorder than heterosexual men. Generating probability samples of men who have sex with men requires extensive (and expensive) screening, so earlier probability samples have been limited to “gay ghettos” (16) in single cities in the United States (17–19). The content of these studies focused on only AIDS, sexually transmitted diseases, and AIDS-related risk behaviors—not to mental health or health in general.
This article is based on data from the Urban Men’s Health Study, a large (N=2,881), geographically diverse (San Francisco, New York, Los Angeles, and Chicago, including areas outside gay ghettos), household-based probability sample of men who have sex with men in the United States. This article estimates the prevalence of major depression and distress in men who have sex with men and considers independent associations of depression and distress with a wide variety of health-related variables.
Method
Sample Design
A complete description of the construction of the sampling frame and overall sample demographics are described elsewhere (20). To summarize, a household-based probability sample of 2,881 men who have sex with men was obtained by identifying geographic areas for sampling (21) and then applying disproportionate and adaptive sampling methods (22, 23) to those areas. These strategies had been previously suggested for generating representative samples of hard-to-reach populations for AIDS studies (24). All data presented here have been weighted to reflect the probability of selection, adjustment for noncoverage and nonresponse, and maintenance of proportionality between cities based on each city’s estimated total population of men who have sex with men. Potential respondents could verify the nature of the study through local, national, and university contact names and telephone numbers. Telephone interviews started in late 1996 and continued until early 1998. In total, 63,783 households were screened; 3,700 households (5.8%) were found to contain at least one man who has sex with men; and 2,881 interviews (78% of eligible households) were completed. Interviews were conducted in Spanish (N=17) or in English at a time of the respondent’s choosing and lasted an average of 75 minutes. The Committee on Human Research of the University of California, San Francisco, provided human subject review and oversight, and consent procedures consistent with telephone interviewing techniques were applied.
Dependent Variables
Distress and depression were measured with the Center for Epidemiological Studies Depression Scale (CES-D Scale) (25). The CES-D Scale is a 20-item questionnaire asking the frequency of various depressive symptoms in the previous week and was originally developed in 1977 as a survey instrument measuring depression. The original cut point of 15 or greater has been shown to be inadequate as a screening examination for current major depressive disorder (26, 27). The National Institute for Occupational Safety and Health and the Centers for Disease Control and Prevention use the CES-D Scale with a cutoff of 22 to define “major depression” in their surveillance (28). Sensitivity and specificity for major depressive disorder are greater than 85% with cutoff points of 21 and 23, respectively (29, 30). Because the CES-D Scale does not request time course data, it is impossible to differentiate major depressive disorders from either dysthymic disorder or a depressive episode of bipolar disorder. Those two disorders are probably a large proportion of the false positives found by using this scale.
What characterized the respondents with CES-D Scale scores from 16 to 21? Many psychiatric disorders other than mood disorders (and some normal conditions, such as bereavement) have significant dysphoric elements, at least episodically. Anxiety disorders have been noted to confound CES-D Scale scores of 16 or greater (31). Other confounding conditions may include—but are not limited to—alcohol and drug withdrawal and adjustment disorders. Since a broad range of conditions are likely to have CES-D Scale scores in this range, this study categorizes respondents with CES-D Scale scores in the range of 16 to 21 as “distressed” rather than as having a particular diagnosis. Together with the depressed respondents, they represent much of the group at risk for needing voluntary mental health care.
A total of 2,678 (93%) of the 2,881 respondents completed the CES-D Scale. A three-category version of CES-D Scale scores was used as the dependent variable: euthymic (i.e., of normal mood), scores of 15 and below; distressed, scores from 16 to 21; and depressed, with scores of 22 and above.
Independent Variables
Six types of independent variables were chosen: demographics, developmental issues, substance use, sexual behavior, HIV experience, and current social context variables.
The demographic variables examined were age, race or ethnicity (white, African American, Hispanic, Asian/Pacific Islander, or Native American/other), educational level (not having a college degree, having an undergraduate degree, or postgraduate studies), area of residence (gay ghetto [32] or other), and city of residence (San Francisco, New York, Los Angeles, or Chicago).
Developmental issue variables included age at first sexual experience; history of parental substance abuse (including alcohol) or attempted suicide (both categorized “yes” or “no”); number of incidents of child abuse (defined as being “beaten up” by a parent or adult in charge), anti-gay harassment before the age of 16, and witnessing a number of incidents of domestic violence between parents (0, 1, or ≥2); lifetime number of incidents of forced sex (0, 1–5, or ≥6), and, if applicable, age at first forced sex and age at first suicide attempt.
Substance use was measured by frequent heavy alcohol use (weekly ingestion of at least five cocktail equivalents at one sitting or other), multiple drug use (use of at least three categories of drugs of abuse or other), three or more alcohol-related problems (“yes,” “no,” or “missing”), and frequent drug use (at least one drug of abuse at least once a week or other). Because of a technical problem, a high proportion (N=229) of the 2,881 respondents were missing data related to the number of alcohol-related problems. Therefore, a “marker” variable was created—“missing alcohol-related problems” (“yes” or “no”), and this variable was entered in the logistical model just before the substance use block to control for the missing data (33).
The variables for sexual behavior examined were any sexual dysfunction in the previous year (“yes” or “no”), number of sex partners in the previous year, and unsafe sex in the previous year, defined as anal or vaginal intercourse with a partner of different or unknown HIV serostatus (“yes” or “no”).
HIV exposure was assessed by self-reported—but internally validated (34)—HIV status (HIV positive or other); any care of a person with AIDS in the previous year (“yes” or “no”); responses to “Being [your serostatus] has made you feel like an outsider in the gay community,” and “You find it hard to tell other gay men [your serostatus]” (scored from 1 for “strongly disagree” to 4 for “strongly agree”); and numbers of HIV-related deaths of intimates (lovers, former lovers, close friends, or family members) and of current HIV-positive intimates. Of those who took care of any people with AIDS in the prior year, further variables studied were currently caring for a current or ex-domestic partner (“yes” or “no”), the number of people with AIDS cared for in the previous year, and the number of current care-giving relationships with persons with AIDS.
Current social context variables were being in a domestic partnership (living with a man in a committed relationship, regardless of its legal status) (“yes” or “no”), self-defined sexual identity (dichotomized as gay, queer, homosexual, or other), outness, community cohesion, and community alienation (all defined elsewhere [32]). Current variables were also numbers of incidents of anti-gay violence or threat of violence in the previous 5 years, of incidents of domestic violence in the prior 5 years, of gay-identified community organizations in which the respondent was involved, and of non-gay-identified community organizations in which the respondent was involved. Domestic partnership status and self-defined sexual identity were included in this block rather than as demographic characteristics because a respondent’s answer could easily be changed with no apparent change in behavior.
Data Analysis
Initially, t tests were used to test statistical comparisons of continuous independent variables for significance; statistical comparisons of categorical independent variables used chi-square analysis. Subsequent simultaneous comparisons of the three CES-D Scale categories by demographic, developmental, substance use, sexual behavior, HIV experience, and social context variables used multinomial logistic regression rather than ordinal logistic regression because the proportional odds assumption could not be made, given the diagnostic heterogeneity of the distressed subjects. For this regression, continuous variables were converted to categorical variables based on quartile values of the items in question, except age (categorized as 18–29, 30–39, 40–49, 50–59, 60–69, and ≥70 years), incidents of anti-gay violence or threat of violence in the previous year, incidents of domestic violence in the prior 5 years, and incidents of non-gay-identified community organization (all recoded as 0, 1, and ≥2). Histories of child abuse and early anti-gay harassment were dichotomized (as present or not). Two skewed 4-point Likert-scale variables were divided into two categories: responses to “Being [your serostatus] has made you feel like an outsider in the gay community,” was categorized as “agree” or “disagree,” and, “You find it hard to tell other gay men [your serostatus]” was recoded as “strongly disagree” or “less than strongly disagree”). Independent variables with p<0.05 in the preliminary comparisons were entered into the multivariate model in blocks in the following order: demographic characteristics, developmental issues, missing alcohol-related problems, substance use, sexual behavior, experience with the HIV epidemic, and current social context. Variables were eliminated stepwise within each block when p≥0.05. Conditional odds ratios were calculated for the final model by STATA, using the “svymlog” procedure (35, 36). The value of the goodness of fit test was calculated by first running separate binomial logistical models through LOGITSE, an SAS macro (37), with a weighted version of the preferred Hosmer-Lemeshow decile goodness of fit test on each pair of two values of the dependent variable (i.e., euthymic versus distressed, euthymic versus depressed, and distressed versus depressed). P values for goodness of fit obtained in these regressions were corrected by a reversed Bonferroni procedure to obtain an overall goodness of fit (38).
Results
While this analysis was not designed as a meta-analysis, and comparing studies using different instruments to measure a single phenomenon should not be undertaken lightly, a comparison of the prevalence of distress and/or depression in other probability samples of adult U.S. men provides a context that is necessary to understand these findings. Table 1 makes the comparisons.
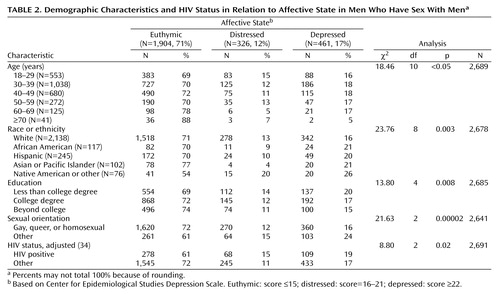
In the Urban Men’s Health Study sample, 17% of the men who have sex with men were depressed, 12% were distressed, and 71% were euthymic. Table 2 describes the demographic characteristics and HIV status of the sample by CES-D Scale category. Geographical variables of city and area of residence were not significant.
Table 3 describes the outcome of the multinomial logistic regression. Goodness of fit was excellent (p=0.42). Of note are some of the variables that are not in the model. Neither the number of sexual partners nor the history of unsafe sex in the prior year was associated with distress or depression. Not self-identifying as gay, queer, or homosexual was significant in predicting distress and depression, regardless of the level of “outness” (i.e., how publicly that identity is expressed). The only HIV experience variable (including HIV status) that remained in the model was being an outsider due to HIV status, whether positive or negative.
Discussion
Because this data was based on a survey of men who have sex with men, there is no direct control group for the purposes of proving a difference in the rates of depression and distress between men who have sex with men and men who do not have sex with men. Nonetheless, the Urban Men’s Health Study data on men who have sex with men and the data based on other probability samples of men in general are strikingly and consistently disparate. When we compared the entire at-risk group of distressed and depressed men with the same instrument as this study, men who have sex with men are 2.7 times as likely to be in the at-risk group than a general population of men (with a probability of less than one in a million). This is consistent with an odds ratio of 2.9 for all mood disorders in men who have sex with men over other men in the Dutch NEMESIS study (15). Different instruments and different authors define “current” as a time period of from 7 to 30 days (or decline to define it at all), further limiting the ability to make direct comparisons between studies. Even so, using each author’s definition of “current,” the “current” prevalence of depression in men who have sex with men appears to be 4.5 to 7.6 times more likely, and the differences appear significant at the level of less than one in a million. Presumably by using a scale with a short definition of “current,” such as the CES-D Scale, makes for a conservative estimate of the difference in prevalence. Even when comparing major depression in a sample that includes women (who are known to have higher rates of depression) (1), men who have sex with men have 2.6 times higher current rates of depression than the lifetime rates in the general population (χ2=239.2, df=1, p<0.000001, N=10,267). All these comparisons are all the more remarkable because the probability samples of the men in general included an unknown number of men who have sex with men. Although statistical proof is not possible here, the differences among these disparate studies makes it clear that further study of mental health in men should include measures of sexual orientation and behavior to more fully test these hypothetical differences.
Variables associated with both distress and depression are not having a domestic partner; a recent history of anti-gay threats or violence; not identifying as gay, queer, or homosexual; and feeling highly alienated from the gay community. Not being married was associated with multiple psychiatric conditions. The other three variables may reflect homophobia—internal or external. Multivariate analysis can establish association, not causality, but these variables imply hypotheses to test causality by measuring the effectiveness of community-based interventions in improving the mental health of men who have sex with men as a group. Does the enactment of statutes legalizing marriage or domestic partnership or punishing hate crimes based on sexual orientation lead to a lower prevalence of distress and depression in men who have sex with men? Natural experiments concerning both these hypotheses are occurring as local and state governments around the United States establish these laws. Would programs developed to encourage men who have sex with men to self-identify as gay, queer, or homosexual decrease levels of depression and distress? Might programs designed to promote the notion of a community of gay men decrease levels of alienation and thereby decrease rates of distress and depression? Both of these hypotheses are testable; in some places, research infrastructure that could be used to test them is already in place in AIDS-related, community-based organizations.
Parsing distress and depression by the variables to which each is uniquely associated is more complicated. Distress, compared to euthymia, is associated with other than Asian/Pacific Islander ethnicity and a history of early anti-gay harassment. Depression, relative to euthymia, is associated with a history of suicide attempt, child abuse, sexual dysfunction, and lower levels of community alienation. Within the overall at-risk group with CES-D Scale scores of 16 or greater, depression is associated with Asian/Pacific Islander ethnicity, a history of suicide attempt, child abuse, sexual dysfunction, and very high levels of community alienation, but it is negatively associated with a history of early anti-gay harassment.
This odd configuration of associations may be due, in part, to the heterogeneity of the “distressed” category. Some unknown portion of the distressed respondents likely has mood disorders that are not severe enough to attain high CES-D Scale scores. This could account for two variables that are associated with depression when compared to distress and that tend to be significant when we compared distress and euthymia: history of suicide attempt and high levels of community alienation. Sexual dysfunction may be associated with depression severe enough to attain high CES-D Scale scores but not with less severe variants. Cultural inhibitions in Asian/Pacific Islander respondents in which depressive symptoms are minimized until they are so problematic as to be undeniable (43, 44) could explain why, within the entire population of men who have sex with men, being of Asian/Pacific Islander extraction is protective for low-scoring mood disorders (and, hence, distress) as well as positively associated with depression in an at-risk population of men who have sex with men. The CES-D Scale may also have some cultural bias regarding U.S. Asians and Pacific Islanders. Cultural bias also may be evident in the finding that not being African American approaches significance as a predictor of distress over euthymia.
Interpretation of the pattern of associations of histories of child abuse and early anti-gay harassment is perplexing. History of child abuse is associated with depression when compared with both distress and euthymia. To the extent that child abuse is associated with dissociative defense mechanisms, men who have sex with men with this history may be less dysphoric (45), and hence it might not correlate with higher CES-D Scale scores unless particularly toxic stressors (e.g., intrusive recollection and unsupported breach of denial) are present. History of anti-gay harassment before the age of 16 is positively associated with distress (compared with euthymia), but it is protective against depression (compared with distress). Perhaps early anti-gay harassment is more likely to produce anxiety disorders or adjustment disorders. It may also produce external objects (e.g., homophobes or gay bashers) at which anger, which otherwise might be self-directed (leading to depression), might be outwardly directed, reducing the propensity toward depression. More study is needed to better explicate the relationship of these variables to distress and depression in men who have sex with men.
The power of the overall analysis may be reduced by using three categories of CES-D Scale scores and multinomial logistic regression analysis. Therefore, several additional variables with p values between 0.05 and 0.10 should be addressed. These include age of less than 50 for depression and outsider status due to HIV status and three or more alcohol-related problems for both depression and distress. Youth is a known risk factor for depression (7). Outsider status in HIV-negative men who have sex with men has been discussed elsewhere (46), as has alcohol use and abuse in the Urban Men’s Health Study survey (47).
Conspicuous by its absence is any further association between other HIV experiences and being distressed or depressed. The relationship of HIV infection and the risk for major depression has been difficult to demonstrate: finding that association required a meta-analysis of 10 studies (with a total N of 2,596), and a meta-analysis of five of those same studies (N=1,117) was unable to locate an association between depression and the presence of symptomatic HIV disease (48), presumably the most severe type of HIV-related stressor. The advent of protease inhibitors in 1996 and the perception of HIV disorders moving from inexorably fatal to chronic may mean that its mental health impact has diminished for both HIV-infected men who have sex with men as well as their caretakers.
This study has several limitations. As noted, because it is based on a survey of men who have sex with men, there is no direct heterosexual control group. Because the Urban Men’s Health Study was not focused on depression alone and required lengthy phone interviewing, it was not possible to cover the full gamut of issues that might be related to depression in men who have sex with men, including religiosity, early severe loss, divorce, or family history of depression or suicidality. Further research could explore these issues. Threat of violence and actual violence were not distinguished in this study; while either predicted distress or depression, actual violence may be a stronger predictor of distress and depression. Up to 15% of the depressed group may be false positives and false negatives (29, 30).
Although some of those false positives might be people with other mood disorders, such as a depressive episode of bipolar disorder or severe dysthymic disorder, their diagnosis is not of a major depressive disorder per se. Men who have sex with men who do not identify themselves as gay, queer, or homosexual may have been more likely to deny homosexual behavior and hence not to participate in the survey. Nonetheless, 16% of the men who have sex with men who were interviewed self-identified as bisexual, heterosexual, or other (20). Given that this study was cross-sectional in nature, any imputation of causality is ill-advised; proof of causality would require a cohort study. The sample frame excluded some men who have sex with men who live in urban areas with a low proportion of men who have sex with men, as well as those residing in small cities, in suburbs, or in rural areas. As probability sampling of these areas for men who have sex with men is prohibitively expensive, network sampling (49, 50) may be the sampling method of choice—albeit with significant limitations—to study these populations. Men who have sex with men of color are underrepresented in this study due to in-migration (20), and men who have sex with men of color may also be less likely to disclose sexual orientation or preferentially live in areas of the cities not sampled (32). The sample excluded a priori adolescent men who have sex with men and the 5% of the households in these cities that do not have telephones (51, 52). Convenience samples may be the only way to reach some subgroups of the very poor, such as those who are homeless; interviewing adolescents requires complicated (and probably biasing) parental consent.
The prevalence of depression in men who have sex with men is comparable to the prevalence of HIV seropositivity in men who have sex with men (20), and, like HIV disease, depression is chronic and enormously expensive in terms of lost wages, disability, cost of treatment, and decrease in life expectancy. In addition to treating individual men who have sex with men with depression or distress, public health efforts to prevent these conditions might also be attempted at the level of structural interventions designed to change the social environment in which men who have sex with men live. The relationships described in this article suggest that communities of men who have sex with men might experience lowered rates of distress and depression if efforts were made to encourage acknowledgment of sexual orientation or enhance community building to decrease the sense of alienation from the gay community for some men who have sex with men. Furthermore, the relationships described herein also suggest that encouragement of long-term intimate relationships between men who have sex with men (such as domestic partnership laws) and effective hate crime legislation might also reduce rates of distress and depression in men who have sex with men. There exist opportunities to measure how social policy changes might yield important health outcomes at the level of the individual. Efforts to take advantage of natural experiments that are created as changes in social policy about men who have sex with men and their central relationships may well yield important understandings in how to support health and social functioning in other marginalized populations.
 |
 |
 |
Received Aug. 29, 2002; revision received May 13, 2003; accepted Aug. 7, 2003. From the Department of Psychiatry, the Center for AIDS Prevention Studies, AIDS Research Institute, the Department of Medicine, and the Department of Epidemiology and Biostatistics, University of California at San Francisco. Address reprint requests to Dr. Mills, 203 Westminster Dr., N.E., Atlanta, GA 30309-3312; [email protected] (e-mail). Supported by NIMH grant MH-54320 and the Centers for Disease Control and Prevention’s Division of HIV/AIDS Prevention. The authors thank Johnny Blair and Dr. Graham Kalton for the design of the sampling frame, Dr. Richard Brand for statistical consultation, Dr. Kyung-hee Choi for help with the mental health needs of Americans of Asian or Pacific Island descent, and Dr. Trevor Hart for his criticism of the manuscript. This article is dedicated to the memory of Dr. Geoffrey K. Booth and his life partner, Gary Babcock.
 |
APPENDIX 1.
1. Druss BG, Hoff RA, Rosenheck RA: Underuse of antidepressants in major depression: prevalence and correlates in a national sample of young adults. J Clin Psychiatry 2000; 61:234–237Crossref, Medline, Google Scholar
2. Henry JA, Rivas CA: Constraints on antidepressant prescribing and principles of cost-effective antidepressant use. Pharmacoeconomics 1997; 11:419–443Crossref, Medline, Google Scholar
3. Greden JF: The burden of disease for treatment-resistant depression. J Clin Psychiatry 2001; 62(suppl 16):26–31Google Scholar
4. Rodin G, Voshart K: Depression in the medically ill: an overview. Am J Psychiatry 1986; 143:696–705Link, Google Scholar
5. Katon W, Schulberg H: Epidemiology of depression in primary care. Gen Hosp Psychiatry 1992; 14:237–247Crossref, Medline, Google Scholar
6. Olfson M, Shea S, Feder A, Fuentes M, Nomura Y, Gameroff M, Weissman MM: Prevalence of anxiety, depression, and substance use disorders in an urban general medicine practice. Arch Fam Med 2000; 9:876–883Crossref, Medline, Google Scholar
7. Blazer DG, Kessler RC, McGonagle KA, Swartz MS: The prevalence and distribution of major depression in a national community sample: the National Comorbidity Survey. Am J Psychiatry 1994; 151:979–986Link, Google Scholar
8. Hooker E: The adjustment of the male overt homosexual. J Projective Techniques 1957; 21:18–31Crossref, Medline, Google Scholar
9. Lohrenz L, Connelly J, Coyne L, Spare K: Alcohol problems in several Midwest homosexual populations. J Stud Alcohol 1978; 39:1959–1963Crossref, Medline, Google Scholar
10. McKirnan DJ, Peterson PL: Alcohol and drug use among homosexual men and women: epidemiology and population characteristics. Addict Behav 1989; 14:545–553Crossref, Medline, Google Scholar
11. Stall R, Wiley J: A comparison of alcohol and drug use patterns of homosexual and heterosexual men: the San Francisco Men’s Health Study. Drug Alcohol Depend 1988; 22:63–73Crossref, Medline, Google Scholar
12. Fay RE, Turner CF, Klassen AD, Gagnon JH: Prevalence and patterns of same-gender sexual contact among men. Science 1989; 243:338–348Crossref, Medline, Google Scholar
13. Laumann EO, Gagnon JH, Michael RT, Michaels S: The Social Organization of Sexuality: Sexual Practices in the United States. Chicago, University of Chicago Press, 1994Google Scholar
14. Binson D, Michaels S, Stall R, Coates TJ, Gagnon JH, Catania JA: Prevalence and social distribution of men who have sex with men: United States and its urban centers. J Sex Res 1995; 32:245–254Crossref, Google Scholar
15. Sandfort TG, de Graaf R, Bijl RV, Schnabel P: Same-sex sexual behavior and psychiatric disorders: findings from the Netherlands Mental Health Survey and Incidence Study (NEMESIS). Arch Gen Psychiatry 2001; 58:85–91Crossref, Medline, Google Scholar
16. Levine MP: Gay ghetto. J Homosex 1979; 4:363–367Crossref, Medline, Google Scholar
17. Winkelstein W, Lyman DM, Padian N, Grant R, Samuel M, Wiley JA, Anderson RE, Lang W, Riggs J, Levy JA: Sexual practices and risk of infection by the human immunodeficiency virus: the San Francisco Men’s Health Study. JAMA 1987; 257:321–325Crossref, Medline, Google Scholar
18. Kanouse DE, Berry S, Gorman E, Jano E, Carson S: Response to the AIDS Epidemic: A Survey of Homosexual and Bisexual Men in Los Angeles County. Santa Monica, Calif, Rand Corp, 1991Google Scholar
19. Osmond DH, Page K, Wiley J, Garrett K, Sheppard HW, Moss AR, Schrager L, Winkelstein W: HIV infection in homosexual and bisexual men 18 to 29 years of age: the San Francisco Young Men’s Health Study. Am J Public Health 1994; 84:1933–1937Crossref, Medline, Google Scholar
20. Catania JA, Osmond D, Stall RD, Pollack L, Paul JP, Blower S, Binson D, Canchola JA, Mills TC, Fisher L, Choi K-H, Porco T, Turner C, Blair J, Henne J, Bye LL, Coates TJ: The continuing HIV epidemic among men who have sex with men. Am J Public Health 2001; 91:907–914Crossref, Medline, Google Scholar
21. Binson D, Moskowitz J, Mills T, Anderson K, Paul J, Stall R, Catania J: Sampling men who have sex with men: strategies for a telephone survey in urban areas in the United States, in 1996 Proceedings of the American Statistical Association Section of Survey Research Methods. Alexandria, Va, American Statistical Association, 1996, pp 68–72Google Scholar
22. Blair J: A probability sample of gay urban males: the use of the two-phase adaptive sampling. J Sex Res 1999; 36:39–44Crossref, Google Scholar
23. Kalton G: Sampling considerations in research on HIV risk and illness, in Methodological Issues in AIDS Behavioral Research. Edited by Ostrow DG, Kessler RC. New York, Plenum Press, 1993, pp 53–74Google Scholar
24. Fowler FJ (ed): Health Survey Research Methods: National Center for Health Services Research Conference Proceedings Series: DHHS Publication PHS 889–3447. Washington, DC, US Government Printing Office, 1989Google Scholar
25. Radloff LS: The CES-D Scale: a self-report depression scale for research in the general population. J Applied Psychol Measurement 1977; 1:385–401Crossref, Google Scholar
26. Turk DC, Okifuji A: Detecting depression in chronic pain patients: adequacy of self-reports. Behav Res Ther 1994; 32:9–16Crossref, Medline, Google Scholar
27. Herman DB, Susser ES, Struening EL: Childhood out-of-home care and current depressive symptoms among homeless adults. Am J Public Health 1994; 84:1849–1851Crossref, Medline, Google Scholar
28. Impact of September 11 attacks on workers in the vicinity of the World Trade Center—New York City. MMWR Morb Mortal Wkly Rep 2002; 51(special Sept 11 issue):8–10Google Scholar
29. Fava GA, Pilowsky I, Pierfederici A, Bernardi M, Pathak D: Depression and illness behavior in a general hospital: a prevalence study. Psychother Psychosom 1982; 38:141–153Crossref, Medline, Google Scholar
30. Lyness JM, Noel TK, Cox C, King DA, Conwell Y, Caine ED: Screening for depression in elderly primary care patients: a comparison of the Center for Epidemiologic Studies-Depression scale and the Geriatric Depression scale. Arch Intern Med 1997; 157:449–454Crossref, Medline, Google Scholar
31. Breslau N: Depressive symptoms, major depression, and generalized anxiety: a comparison of self-reports on CES-D and results from diagnostic interviews. Psychiatry Res 1985; 15:219–229Crossref, Medline, Google Scholar
32. Mills TC, Stall R, Pollack L, Paul J, Binson D, Canchola J, Catania JA: Health-related characteristics of men who have sex with men: a comparison of those living in “gay ghettos” with those who live elsewhere. Am J Public Health, 2001; 91:980–983Crossref, Medline, Google Scholar
33. Cohen J, Cohen P: Applied Multiple Regression/Correlation Analysis for the Social Sciences, 2nd ed. New York, Wiley & Sons, 1984, pp 292–296Google Scholar
34. Osmond DH, Catania J, Pollack L, Canchola J, Jaffe D, MacKellar D, Valleroy L: Obtaining HIV test results with a home collection test kit in a community telephone sample. J Acquir Immune Defic Syndr 2000; 24:363–368Crossref, Medline, Google Scholar
35. STATA Reference Manual, Release 6, vol 2. College Station, Tex, Stata Corp, 1999Google Scholar
36. Gould W: Interpreting logistical regression in all its forms. Stata Technical Bull 2000; 53:19–29Google Scholar
37. Canchola JA, Marx BD, Catania JA: LOGITSE: a SAS macro for logistic regression modeling in complex surveys, in Proceedings of the 22nd Annual SAS Users International Conference. Cary, NC, SAS Institute, 1997, pp 1282–1287Google Scholar
38. Westfall PH, Young SS: Resampling-Based Multiple Testing. New York, John Wiley & Sons, 1993Google Scholar
39. World Health Organization: Composite International Diagnostic Interview (CIDI), version 1.0. Geneva, WHO, 1990Google Scholar
40. Wang PS, Berglund P, Kessler RC: Recent care of common mental disorders in the United States: prevalence and conformance with evidence-based recommendations. J Gen Intern Med 2000; 15:284–292Crossref, Medline, Google Scholar
41. Kessler RC, Andrews G, Mroczek D, Ustun B, Wittchen H-U: The World Health Organization Composite International Diagnostic Interview Short Form (CIDI-SF). Int J Methods in Psychiatr Res 1998; 7:171–185Crossref, Google Scholar
42. Robins LN, Helzer JE, Croughan J, Ratcliff KS: The National Institute of Mental Health Diagnostic Interview Schedule: its history, characteristics, and validity. Arch Gen Psychiatry 1981; 38:381–389Crossref, Medline, Google Scholar
43. Durvasula R, Sue S: Severity of disturbance among Asian American outpatients. Cult Divers Ment Health 1996; 2:43–51Crossref, Medline, Google Scholar
44. Sue S, Sue DW, Sue L, Takeuchi DT: Psychopathology among Asian Americans: a model minority? Cult Divers Ment Health 1995; 1:39–51Crossref, Medline, Google Scholar
45. Perry JC: A pilot study of defenses in adults with personality disorders entering psychotherapy. J Nerv Ment Dis 2001; 189:651–660Crossref, Medline, Google Scholar
46. Odets W: In the Shadow of the Epidemic: Being HIV-Negative in the Age of AIDS. Durham, NC, Duke University Press, 1995Google Scholar
47. Stall R, Paul JP, Greenwood G, Pollack LM, Bein E, Crosby GM, Mills TC, Binson D, Coates TJ, Catania JA: Alcohol use, drug use, and alcohol-related problems among men who have sex with men: the Urban Men’s Health Study. Addiction 2001; 96:1589–1601Crossref, Medline, Google Scholar
48. Ciesla JA, Roberts JE: Meta-analysis of the relationship between HIV infection and risk for depressive disorders. Am J Psychiatry 2001; 158:725–730Link, Google Scholar
49. Kalsbeek WD: Samples for studies related to AIDS, in Health Survey Research Methods: National Center for Health Services Research Conference Proceedings Series: DHHS Publication PHS 889–3447. Edited by Fowler FJ. Washington, DC, US Government Printing Office, 1989, pp 199–203Google Scholar
50. Sudman S, Sirken MG, Cowan DC: Sampling rare and elusive populations. Science 1988; 240:991–996Crossref, Medline, Google Scholar
51. Anderson J, Nelson D, Wilson R: Telephone coverage and measurement of health risk indicators: data from the National Health Interview Survey. Am J Public Health 1998; 88:1392–1395Crossref, Medline, Google Scholar
52. US Bureau of the Census: Census of Population and Housing, 1990: Public Use Microdata Samples US. Washington, DC, US Department of Commerce, 1997Google Scholar



