Is the 5-HT1Dβ Receptor Gene Implicated in the Pathogenesis of Obsessive-Compulsive Disorder?
Abstract
OBJECTIVE: Obsessive-compulsive disorder (OCD) is a psychiatric condition for which strong evidence of a genetic component and serotonergic system involvement exists. Recent studies have shown that sumatriptan, a selective ligand of the serotonin (5-HT)1Dβ autoreceptor, modifies OCD symptoms. The aim of this study was to investigate the presence of linkage disequilibrium between the 5-HT1Dβ receptor gene, which has a variant caused by a silent G to C substitution at nucleotide 861 of the coding region, and OCD.METHOD: DNA was collected from 67 probands who met DSM-IV criteria for OCD and from their living parents or siblings. Transmission Disequilibrium Test/sib-Transmission Disequilibrium Test analyses were then conducted with the DNA data.RESULTS: Thirty-two families were informative for the analysis, which showed a preferential transmission of the G allele to the affected subjects.CONCLUSIONS: If the results are confirmed, there may be important implications for the 5-HT1Dβ receptor gene in the pathogenesis and treatment of OCD.
Obsessive-compulsive disorder (OCD) is a psychiatric condition with a lifetime prevalence of up to 3% (1). The etiology of OCD is unknown, but data from challenge studies (2) and from pharmacological trials (3) have supported the involvement of the serotonergic system. Genetic studies have investigated possible variants of serotonergic system genes: the serotonin (5-HT) receptor gene variants 5-HT2A and 5-HT2C were found not to be associated to OCD (4, 5), while mixed results were found for the serotonin transporter gene (6, 7). The 5-HT1Dβ receptor appears to be particularly interesting. It is a terminal autoreceptor, and challenge studies with nonselective ligands (e.g., m-CPP) (2) showed an acute worsening of obsessive-compulsive symptoms. In addition, a worsening of OCD symptoms has been reported following acute administration of sumatriptan, a selective agonist of the 5-HT1Dβ receptor (2). On the other hand, in OCD patients resistant to conventional pharmacotherapy, improvements have been reported with chronic administration of sumatriptan (8).
The aim of the current study was to investigate the presence of linkage disequilibrium between the 5-HT1Dβ receptor gene (9) and OCD.
Method
Sixty-seven OCD probands were selected. All patients were administered the Structured Clinical Interview for DSM-IV (SCID) and the Yale-Brown Obsessive Compulsive Scale (10). To be eligible for the study, patients had to have either both biological parents or at least one sibling living and willing to participate. The supposedly unaffected siblings were also administered the SCID, and those with any psychiatric disorders were excluded. Patients with a history of neurological or metabolic diseases, bipolar disorder, schizophrenia, or schizoaffective disorder, or with a positive history of substance dependence, were excluded. Written informed consent to participate in the study was obtained from all subjects. Genomic DNA was extracted from whole blood (11), and genotyping of the G861 variant of the gene was performed by means of standard procedures (9).
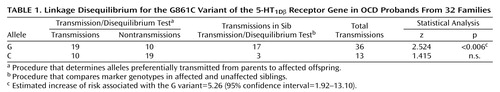
We tested for the presence of linkage disequilibrium between the 5-HT1Dβ; receptor gene G861C polymorphism and OCD with the Transmission Disequilibrium Test/sib-Transmission Disequilibrium Test analyses (12). This procedure combines the Transmission Disequilibrium Test, which examines alleles preferentially transmitted from the parents to the affected offspring, with the sib-Transmission Disequilibrium Test, which compares the marker genotypes in affected and unaffected siblings. We specifically tested for excess of transmissions to the affected siblings by using the z test statistic, one-tailed (12).
Results
The proband group included 27 men and 40 women (mean age=33.3 years, SD=8.2; mean age at OCD onset=15.2 years, SD=8.0); there were no significant differences between sexes. The frequency of comorbid tic disorder was 37.3% (N=25). The mean severity of obsessive-compulsive symptoms as measured by score on the Yale-Brown scale was 19.9 (SD=8.7). After genotyping the total study group, 32 families were found suitable for the Transmission Disequilibrium Test/sib-Transmission Disequilibrium Test procedure. Twenty-two were triads that showed heterozygosity at the marker, and 10 were sibships with one affected and one unaffected sibling. The other 35 were families with homozygous parents. The genotype frequencies in the proband group were GG=59.4% (N=19), GC=37.5% (N=12), and CC=3.1% (N=1), while allele frequencies were 78.1% (N=50) and 21.9% (N=14) for the G and the C allele, respectively. The results of the Transmission Disequilibrium Test/sib-Transmission Disequilibrium Test are shown in Table 1.
Discussion
Our results indicate a significant linkage disequilibrium between the G861C variant of the 5-HT1Dβ receptor gene and OCD, with preferential transmission of the G allele to the affected subjects. Despite the fact that the silent G861C variant has been claimed to not directly affect the function of the receptor, there are several other possibilities to explain the role of this polymorphism in the pathogenesis of OCD. First, as it has been hypothesized for other serotonin receptor genes (e.g., 5-HT2A) (13), one of the variants of the G861C polymorphism could induce different mRNA secondary structure, thereby affecting the efficiency of translation. Second, other polymorphisms may exist in the gene that could be in linkage disequilibrium with the G861C variant and be functionally relevant. Further investigations should focus on additional markers in the area and other possible variants of the gene. As seen with other complex disorders, more than one gene is expected to be involved in the etiology of OCD in a model in which each gene per se has a relatively small effect in increasing the risk for the disease. In our case, the estimated increase of risk to develop OCD, as an effect of the presence of the G variant, was equal to 5.26 (Table 1). The possibility that the C variant may play a protective role in the development of OCD is also possible.
The OCD phenotype is heterogeneous, as suggested by the variability in the response to medications in both acute and chronic administrations (2, 14). The investigation of the distribution of this and other 5-HT1Dβ receptor gene polymorphisms in OCD patients designated as responsive versus nonresponsive to medication will be useful.
Finally, even though it is impossible at this time to define more precisely the role of the 5-HT1Dβ receptor gene in OCD, the magnitude of the effect that we observed deserves further investigations. Only a combined strategy, which implies an exhaustive exploration of the OCD phenotype and a more extended knowledge of the genetic complexity of the 5-HT1Dβ gene, will be able to shed light on this potential component of the etiology of OCD.
 |
Received June 23, 1999; revision received Nov. 24, 1999; accepted Jan. 27, 2000. From the Neurogenetics Section and the Anxiety Disorders Clinic of the Centre for Addiction and Mental Health, University of Toronto. Address reprint requests to Dr. Kennedy, Neurogenetics Section, Centre for Addiction and Mental Health, 250 College St., Toronto, Ont., Canada, M5T 1R8. Supported in part by a grant from the Ontario Mental Health Foundation.
1. Sasson Y, Zohar J, Chopra M, Lustig M, Iancu I, Hendler T: Epidemiology of obsessive-compulsive disorder: a world view. J Clin Psychiatry 1997; 58(suppl 12):7–10Google Scholar
2. Gross R, Sasson Y, Chopra M, Zohar J: Biological models of obsessive-compulsive disorder: the serotonin hypothesis, in Obsessive-Compulsive Disorder: Theory, Research, and Treatment. Edited by Swinson RP, Antony MM, Rachman S, Richter MA. New York, Guilford, 1998, pp 147–148Google Scholar
3. Greist JH, Jefferson JW, Kobak KA, Katzelnick DJ, Serlin RC: Efficacy and tolerability of serotonin transport inhibitors in obsessive-compulsive disorder: a meta-analysis. Arch Gen Psychiatry 1995; 52:53–60Crossref, Medline, Google Scholar
4. Nicolini H, Cruz C, Camarena B, Orozco B, Kennedy JL, King N, Weissbecker K, de la Fuente JR, Sidenberg D: DRD2, DRD3 and 5HT2A receptor genes polymorphisms in obsessive-compulsive disorder. Mol Psychiatry 1996; 1:461–465Medline, Google Scholar
5. Cavallini MC, Di Bella D, Pasquale L, Henin M, Bellodi L:5HT2C CYS23/SER23 polymorphism is not associated with obsessive-compulsive disorder. Psychiatry Res 1998; 77:97–104Google Scholar
6. Billett EA, Richter MA, King N, Heils A, Lesch KP, Kennedy JL: Obsessive-compulsive disorder, response to serotonin reuptake inhibitors and the serotonin transporter gene. Mol Psychiatry 1997; 2:403–406Crossref, Medline, Google Scholar
7. McDougle CJ, Epperson CN, Price LH, Gelernter J: Evidence for linkage disequilibrium between serotonin transporter protein gene (SLC6A4) and obsessive-compulsive disorder. Mol Psychiatry 1998; 3:270–273Crossref, Medline, Google Scholar
8. Stern L, Zohar J, Cohen R, Sasson Y: Treatment of severe, drug resistant obsessive-compulsive disorder with the 5HT1D agonist sumatriptan. Eur Neuropsychopharmacol 1998; 8:325–328Crossref, Medline, Google Scholar
9. Lappalainen J, Dean M, Charbonneau L, Virkkunen M, Linnoila M, Goldman D: Mapping of the serotonin 5HT1Dβ autoreceptor gene on chromosome 6 and direct analysis for sequence variants. Am J Med Gen Neuropsychiatr Genet 1995; 60:157–161Crossref, Medline, Google Scholar
10. Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, Heninger GR, Charney DS: The Yale-Brown Obsessive Compulsive Scale, I: development, use, and reliability. Arch Gen Psychiatry 1989; 46:1006–1011Google Scholar
11. Lahiri DK, Nurnberger JI Jr: A rapid non-enzymatic method for the preparation of HMW DNA from blood for RFLP studies. Nucleic Acids Res 1991; 19:5444Crossref, Medline, Google Scholar
12. Spielman RS, Ewens WJ: A sibship test for linkage in the presence of association: the Sib Transmission/Disequilibrium Test. Am J Hum Gen 1998; 62:450–458Crossref, Medline, Google Scholar
13. Arranz M, Collier D, Sodhi M, Ball D, Roberts G, Price J, Sham P, Kerwin R: Association between clozapine response and allelic variation in 5HT2A receptor gene. Lancet 1995; 346:281–282Crossref, Medline, Google Scholar
14. Mundo E, Bareggi SR, Pirola R, Bellodi L: Effects of acute intravenous clomipramine and antiobsessional response to proserotonergic drugs: is gender a predictive variable? Biol Psychiatry 1999; 45:290–294Google Scholar



