Mortality Risk Among Offspring of Psychiatric Inpatients: A Population-Based Follow-Up to Early Adulthood
Abstract
Objective: The purpose of this article was to estimate relative risks of all-cause mortality associated with parental psychiatric disorder based on offspring age (up to 25 years of age), parental diagnosis, maternal versus paternal disorder, and number of affected parents. Method: The study group consisted of all Danish singleton live and stillbirths (N=1.46 million) during 1973-1998, identified using the Central Population Register and Medical Birth Register. Dates of death were recorded with follow-up to Jan. 1, 1999. Parental admission histories since 1969 were obtained from the Psychiatric Central Register. Results: Mortality risks were elevated from birth through early adulthood among offspring of people admitted with any type of psychopathology, although relative risks were attenuated during school attendance years. Effect sizes varied according to offspring ages, the highest being during infancy. The following high-risk subgroups were identified: postneonates with two mentally ill parents, neonates and postneonates whose mothers had alcohol and drug-related disorders, and neonates whose mothers had affective disorders. In general, from the postneonatal period onward, there was no indication that maternal psychopathology is associated with higher offspring mortality risk than paternal disorder. Conclusions: The greatest number of excess deaths were attributable to alcohol-related disorders, this being the most prevalent paternal diagnostic category and the second most prevalent in mothers. Some findings were unexpected. For example, there was no evidence that mortality risk among offspring of parents with schizophrenia and related disorders was significantly greater than that associated with all other parental psychiatric conditions, whereas the relative risk for neonatal death associated with maternal affective disorders was markedly raised.
Investigation of mortality risk among offspring of mentally ill people has been conducted since the 1930s (1) . Earlier studies generally reported no evidence for higher risk in offspring of affected parents (2 – 4) , whereas most studies since the 1960s have indicated greater risk of fetal, perinatal, and infant mortality associated with parental schizophrenia (5 , 6) , specifically maternal schizophrenia (7 – 9) and the broader range of maternal psychoses (10) . The best available evidence to date has come from large register-based studies conducted in Denmark (8) , Sweden (9) , and Australia (11) , although the latter recently found no evidence of higher offspring mortality risk. The two Scandinavian studies reported elevated relative risks associated with maternal schizophrenia of approximately twofold for stillbirth and between two- and threefold for infant death. The Danish study (8) additionally found a fivefold relative risk for sudden infant death syndrome. An elevated risk of sudden infant death syndrome associated with postnatal depression (12 , 13) and maternal substance misuse (14 , 15) has also been indicated. Evidence is, however, currently lacking for mortality risk among these offspring beyond infancy and for effects of paternal versus maternal disorder (1) .
Higher mortality risks may be linked to inadequate antenatal care (16) , restricted fetal growth (17) , obstetric complications (18 , 19) , medication toxicity (20) , adverse social environment (21 , 22) , and genetic inheritance (23) . The relative importance of these putative mechanisms is likely to vary with the age of the child, parental diagnosis, and which parent is affected. It seems intuitive to expect that effects of maternal disorders are stronger, especially during the perinatal period and infancy. Maternal schizophrenia may be associated with particularly high risk because of the enduring and debilitating nature of the disorder and because parenting outcomes have been shown to be poor in these mothers compared with those admitted with affective disorders (24) .
The objectives of our investigation were 1) to conduct a population-based follow-up study of all-cause mortality risk in offspring of mentally ill people from birth through early adulthood; 2) to investigate different parental diagnostic groups (i.e., schizophrenia and related disorders, affective disorders, alcohol and drug-related disorders), and 3) to compare relative risks for maternal versus paternal disorder and by number of affected parents.
We hypothesized that 1) offspring of mothers and fathers admitted with some type of psychiatric diagnosis would be at greater risk of mortality at all ages compared with the general population; 2) relative risks would be greater for perinatal and infant mortality versus death at age 1 year and over, for maternal versus paternal disorders, and for two versus one affected parent; and 3) relative risks would be especially high among offspring of parents with schizophrenia and related disorders compared with those whose parents had other types of psychiatric disorder.
Method
The Study Cohort
All births that occurred in Denmark between Jan. 1, 1973, and Dec. 31, 1998, were enumerated using the Central Population Register and Medical Birth Register (25) to identify live and stillbirths, respectively. Dates of death from all causes were also recorded in these registers. For simplicity of analysis and presentation, the dataset was restricted to singletons (97.5% of all births). Multiple pregnancies that resulted in a fetal death and a live birth were identified and excluded if the fetal loss occurred at 28 weeks gestation or beyond. Offspring of mothers born outside Denmark were excluded because of the unavailability of their psychiatric histories prior to immigration, a potential source of information bias. The birth cohort was linked to the Psychiatric Central Register (26 , 27) , which records all admissions to psychiatric hospitals and wards that have occurred nationally since 1969. A unique identification number enabled virtually complete linkage between registers and of offspring to their birth mothers and registered fathers (28) . It was impossible to check that the registered father was the biological father for any births in the cohort.
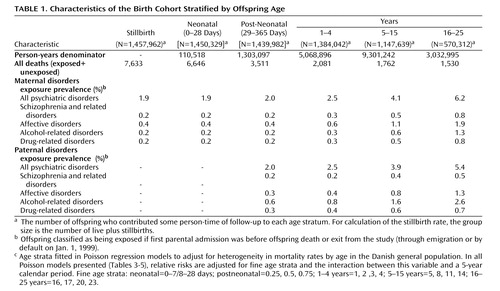
Standard World Health Organization definitions were used to categorize offspring age during the first year of life, i.e., neonatal period (0–28 days) and postneonatal period (from 28 days to the end of the first year). There is currently no internationally agreed definition for stillbirth. In Denmark, fetal deaths at 28 weeks are classified as stillbirths (29) . The age groups 1–4, 5–15, and 16–25 years were chosen to reflect preschool, schooling, and early adulthood periods, respectively. The oldest age stratum was truncated at 25 years of age, the maximum length of follow-up in the cohort. The 1.45 million live births were followed up for over 18.8 million person-years in total. Stratification of this denominator by offspring age is shown in Table 1 . Age-specific relative risks for mortality among live-born offspring were estimated as incidence-rate ratios, the incidence rate (λ) being the number of deaths ( n ) divided by the aggregate number of person-years ( pyrs ) per age stratum. The incidence rate ratio is (n e /pyrs e )/(n u /pyrs u ), where ne is the number of deaths in the exposed group; pyrse is the number of person-years at risk in the exposed group; nu is the number of deaths in the unexposed group; and pyrsu is the number of person-years at risk in the unexposed group.
Relative risks for stillbirth were estimated as risk ratios using all births as the denominator. The risk ratio is the proportion of all births that are stillbirths in the exposed group divided by this proportion in the unexposed group. For these analyses, only those maternal first admissions prior to birth classified offspring to the exposed group.
The age-specific study-group size, which is the number of offspring contributing at least some person-time to the denominator in each age stratum, declined as the children became older ( Table 1 ). This was partly because of attrition by death and emigration, but mostly because only subsets of all the births were eligible for follow-up beyond the neonatal period. Thus, since the last day of observation was Jan. 1, 1999, only subjects born before the end of Dec. 1982 could be followed up into the oldest age stratum (16–25 years).
Parental Diagnostic Categories
Parental diagnostic categories were selected to maximize clinical relevance while yielding sufficient numbers of events for precise estimation of offspring age-specific relative risks. All parental first admissions at age 16 years and over were identified using the psychiatric register, with episodes coded by ICD-8 for years 1973–1993 and ICD-10 for 1994–1998. The following categories were investigated: 1) all psychiatric diagnoses (ICD-8: 290–315; ICD-10: F00-F99); 2) schizophrenia and related disorders, i.e., schizophrenia, schizophrenia-like, or schizoaffective disorder (ICD-8: 295, 296.8, 297, 298.39, 301.83; ICD-10: F20-F29); 3) affective disorders (ICD-8: 296.09, 296.19, 296.29, 296.39, 296.99, 298.09, 298.19, 300.49, 301.19; ICD-10: F30-F39) 4) alcohol-related disorders (ICD-8: 291, 303; ICD-10: F10) 5) drug-related disorders (ICD-8: 294.30, 294.38, 304, 980.09; ICD-10: F11-F16, F-18, F-19).
The codes used to delineate affective disorders (including bipolar disorder) versus schizoaffective disorder were based on those used in previous Danish register-based studies (30 , 31) , except we included ICD-8 296.8/296.89 in the schizoaffective list.
Statistical Analyses
Statistical analyses were performed using Stata software (32) . For each subject, the person-years at risk were calculated and then stratified according to time-dependent exposure variables (33 , 34) . To eliminate potential reverse causality bias, offspring were only classified as being exposed if parental first admission occurred prior to the date of death (if applicable), since a recent Danish study found an elevated risk of parental hospitalization following the death of a child (35) . If parental first admission occurred after the offspring was born, the person-years years were stratified according to unexposed then exposed categories in a stepwise time-dependent fashion. For each parental diagnostic group, a categorical exposure variable was thereby created, for example, 1=mother not admitted (reference category; relative risk=1.00), 2=mother admitted for any psychiatric diagnosis, and 3=mother admitted for specific diagnostic category (e.g., affective disorder).
Relative risks were modeled using log-linear Poisson regression without significant evidence of overdispersion (36) . Finely stratified offspring age and 5-year calendar period (and an interaction term between the two) were fitted as time-dependent covariates to comprehensively adjust for cohort effects by age (33) . These fine age strata are shown in Table 1 and were selected empirically according to homogeneity of mortality risk in the general population. In this way, for example, adjustment was made for differences over time in parental admission rates. Hospitalization rates declined through the study period, but interaction terms indicated that none of the observed associations were restricted to either the earlier or later periods of observation. The effects of maternal age at birth, offspring sex, and birth order were also assessed, but these variables were excluded from the final models since they had little confounding effect. Wald z tests of linear combinations of coefficients in the Poisson models were also calculated to assess evidence for excess risk specific to diagnostic categories relative to all other parental disorders. These evident excess risks are highlighted with asterisks in the tables according to their significance level (*: p<0.05, **: p<0.01, and ***: p<0.001).
In a study of maternal schizophrenia and perinatal and infant mortality, conducted using the same Danish registers, Bennedsen et al. (8) additionally fitted General Estimation Equation models to correct for statistical nonindependence within sibships. These made no material difference to the relative risks and variances compared to the estimates from models fitted without such correction. On this basis and because our analyses were conducted on a larger study group with aggregated person-years data and with no evidence of overdispersion, models correcting for sibship clustering were not implemented.
Results
Descriptive Analyses
A total of 1,457,962 live and stillbirths occurred between Jan. 1, 1973 and Dec. 31, 1998 ( Table 1 ). Of these, 1,450,329 were born alive, and the study group size declined with increasing offspring age to 570,312 at 16–25 years. A total of 23,163 deaths occurred across the study age range. Stratified by age, the most prevalent conditions were affective then alcohol-related disorders for maternal disorders and alcohol-related then affective disorders for paternal disorders. For all types of parental disorders and each specific diagnostic category, exposure prevalence increased as the children aged, which reflects the time-dependent nature of these variables. The identity of the registered father was unknown for a small proportion of all births (1%), but registration practices rendered this information missing for more than one-quarter of stillbirths and neonatal deaths compared with only 2% of deaths at ages 1–25 years. Further investigation suggested that relative risks for stillbirth and neonatal death associated with paternal disorders were strongly biased because of these missing data, so these effect estimates are not reported. Comparison of relative risks for maternal versus parental disorder are thus restricted to the postneonatal period onward.
Relative Risks Among Offspring of Mentally Ill Mothers
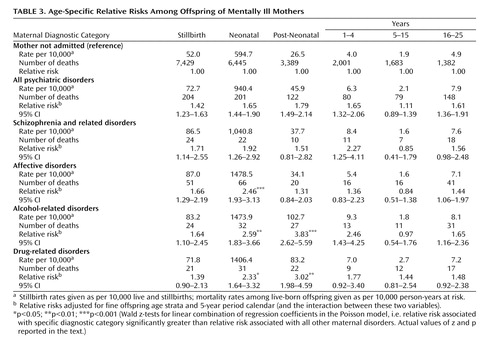
To assess the degree of variability in age-specific relative risks associated with maternal psychiatric disorders, χ 2 tests for interaction by age were performed. These indicated significant variability in age-specific effects associated with all maternal disorders and with specific diagnostic categories (affective disorders, alcohol-related disorders) but not with schizophrenia and related disorders or drug-related disorders ( Table 2 ).
Relative risks of mortality associated with all maternal disorders were significantly raised within each offspring age group from birth through early adulthood, apart from ages 5–15 years ( Table 3 ). The other age-specific relative risks associated with all maternal disorders were significantly elevated, with the largest being for postneonatal death. The highest relative risks associated with the specific maternal diagnostic categories tended to occur during the neonatal and postneonatal periods. There was no evidence of elevated risk during school attendance years associated with any specific maternal diagnostic category compared to the risk in the general population.
Wald z tests gave strong evidence for the existence of high-risk offspring subgroups according to maternal diagnosis (i.e., relative risks of 2.5 or greater that were significantly higher than those associated with other maternal conditions). These were neonates and postneonates whose mothers had alcohol-related disorders (z=2.67, p=0.001; z=4.14, p<0.001, respectively), neonates and postneonates whose mothers had drug-related disorders (z=2.03, p=0.03; z=2.59, p=0.01, respectively), and neonates whose mothers had affective disorders (z=3.64, p<0.001). However, there was no indication that schizophrenia and related disorders were associated with an excess mortality risk relative to all other maternal disorders.
The neonatal period is conventionally divided into early and late periods, with the former reflecting markedly higher risks in the first postpartum week. In relation to all maternal disorders, the relative risk in the early neonatal period (0–7 days: N=166 deaths; relative risk=1.65, 95% confidence interval [CI]=1.41–1.92) was equivalent to that in the late neonatal period (8–28 days: N=35; relative risk=1.68, 95% CI=1.20–2.35). Mortality events were too sparse to estimate effects during the late neonatal period specific to each maternal diagnostic category. Only two broad maternal categories yielded adequate numbers: affective disorders and substance-related disorders (defined as an alcohol or a drug-related disorder). For these categories, significantly elevated relative risks of between two and three for both early and late neonatal death were found.
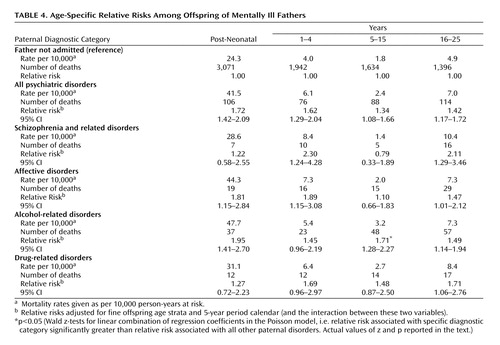
Relative Risks Among Offspring of Mentally Ill Fathers
Age-specific relative risks from the postneonatal period onward associated with paternal disorders are presented in Table 4 . As with all maternal disorders, the highest relative risk associated with all paternal conditions occurred during the postneonatal period. The lowest was again at ages 5–15 years, although this effect was significant in relation to paternal illness. For each age stratum, there was no evidence of excess mortality risk specific to schizophrenia and related disorders relative to other paternal disorders. One high-risk subgroup was indicated. The relative risk among 5–15 years olds whose fathers were admitted for alcohol-related disorders was significantly higher than that associated with all other paternal disorders (z=2.21, p=0.03). During school attendance years, relative risks specific to all other types of paternal disorder were not elevated.
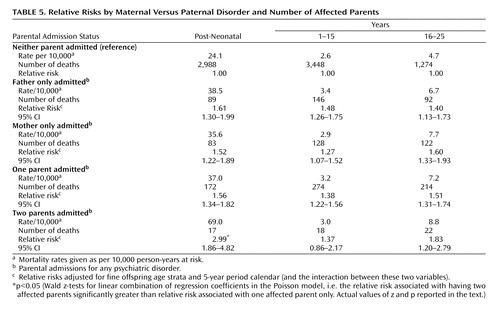
Relative Risks by Maternal Versus Paternal Disorder and Number of Affected Parents
For these results (presented in Table 5 ) “neither parent admitted” was used as a common reference category and, because of sparse data, analyses were restricted to associations with all parental disorders. Within each offspring age stratum (postneonatal period onward), the relative risks of mortality specific to maternal disorder were of similar magnitude to those specific to paternal disorder. The relative risks associated with having two affected parents were higher than those for one affected parent, although the excess was statistically significant only during the postneonatal period (z=2.55, p=0.01). A threefold elevated risk was indicated for postneonatal death among offspring with two mentally ill parents compared to those with unaffected parents.
Discussion
Some of these findings confirmed our prior hypotheses. First, significantly raised mortality risks in offspring of mothers admitted for any type of psychiatric diagnosis were observed from birth through early adulthood, although relative risks were attenuated at ages 5–15 years. Second, relative risks associated with maternal illness varied significantly by age and were generally greatest in the first year of life, during the neonatal (early and late) and postneonatal periods. Relative risks for stillbirth were, however, somewhat lower. Third, the relative risk of postneonatal death among offspring with two mentally ill parents was significantly higher than that associated with having only one affected parent.
However, some findings were contrary to expectation. First, from the postneonatal period onward, similar effect sizes were observed for maternal verus paternal disorder in general. Second, we identified several high-risk subgroups that had relative risks higher than those associated with other psychiatric disorders, but these did not include offspring of parents with schizophrenia and related disorders. Compared with all other maternal disorders, relative risks were significantly raised among neonates and postneonates whose mothers had alcohol and drug-related disorders and among neonates whose mothers had affective disorders. The latter was a particularly surprising result.
This is the first large population-based investigation of mortality risk among offspring of mentally ill parents with follow-up through early adulthood. The effects of a broader range of parental disorders were assessed in previous studies, and derivation of time-dependent exposure variables enabled comparison of associations with specific diagnostic groups versus parental psychopathology in general. Comparisons of effects associated with maternal versus paternal disorders, and of having two versus one affected parent, were performed with a much larger study group than previously available (5 , 6) .
Since Denmark has no privately funded psychiatric inpatient services, the national register provides a near complete population-based record of admissions since 1969. Selection biases, however, do exist because the majority of mentally ill people are never admitted. The degree of bias is likely to vary by diagnostic category. Bennedsen et al. (8) argue that most people with schizophrenia are probably admitted at least once. Thus, even though the register may not capture all cases of schizophrenia and related disorders that occur in the population, the group identified would have good external validity (37) . Selection bias is likely to be higher for investigation of parental affective and substance-related disorders because most of these people are not admitted. For these categories, the observed results are applicable only to the severe end of the diagnostic spectrum. Currently, there are no registers available in Denmark or elsewhere to undertake population-based studies of illnesses that are usually treated in the community. In terms of diagnostic validity, Munk-Jørgensen (38) reported a high positive predictive value of 90% for ICD-8 diagnosis of schizophrenia. Kessing reported good validity for ICD-10 diagnoses of affective disorders (39) and continuity between 8th and 10th ICD revisions for these disorders (40) . There have been no diagnostic validation studies of alcohol or drug-related disorders in the Danish psychiatric register.
Our study has several limitations. First, although a large birth cohort was investigated, the rarity of death among exposed offspring led to sparse data in certain subgroups. This, for example, precluded estimation of relative risks among offspring of two parents affected with specific diagnoses. Second, relative risks of stillbirth and neonatal death associated with paternal disorders were not estimable without substantial bias because of missing data for paternal identity. Third, as in many open cohort studies, bias due to left censoring is likely. Parental psychiatric admission histories were unavailable prior to April 1, 1969, when the psychiatric register was computerized. Thus, misclassification of exposure status because of previous unregistered parental admissions could especially bias effect estimates for births occurring in the earlier years of the cohort. However, this is likely to have attenuated the observed relative risks so that the associations we report are not spurious, and the effect size estimates are conservative.
Finally, we were unable to adjust for potentially important confounders, such as antenatal care attendance, smoking, substance misuse without inpatient admission, and socioeconomic status. Other investigators were also unable to adjust for these factors in recent register-based studies (8 , 11) . Nilsson et al. (9) did account for maternal smoking and educational status, but their adjusted relative risks for stillbirth and infant death associated with maternal schizophrenia remained significantly elevated. It seems intuitive to assume that the confounding effects of these factors are greater in relation to maternal (versus paternal) disorder and for stillbirths and infant deaths compared with mortality beyond the first year. Controlling for factors such as low antenatal attendance, substance misuse, and smoking during pregnancy could also lead to overadjustment, since these measured exposures are likely to occur as a consequence of maternal psychiatric illness.
Our data overlap considerably with those used in a previous study (8) investigating rates of stillbirth and infant death among all women diagnosed with schizophrenia who gave birth during 1973–1993. We extended the birth cohort up to 1998, investigated other maternal conditions as well as paternal disorders, and assessed mortality outcomes beyond infancy through early adulthood. To avoid potential reverse causality bias, we also used a more stringent definition of exposure to include only maternal first admissions that occurred prior to an offspring death. Where comparison is possible, i.e., risk of stillbirth and infant mortality associated with maternal schizophrenia, our findings are consistent with those reported from Sweden (9) , but not with those from a recent Australian study (11) . These investigators found no evidence of higher risk of stillbirth, infant mortality, or early childhood mortality in offspring of mothers with schizophrenia, bipolar disorder, or unipolar disorder. Type II error seems an unlikely explanation for their negative finding, since the odds ratios reported were generally close to unity. Substantive differences between study populations, or between health and social care systems, may explain the incongruous findings. Our results are, however, consistent with those of most studies published since the 1960s, which have generally shown raised mortality risks among the offspring of mentally ill parents (1) .
Relative risks vary according to age. Offspring of mentally ill parents are at higher risk of death during infancy and the years prior to attending school, and relative risks rise again in early adulthood. It may be that during schooling years these children are partially protected from the environmental hazards that are apparently associated with parental mental illness. Relative risks also vary by diagnostic category. Clinicians should be mindful of the high-risk subgroups identified as well as our finding that schizophrenia and related disorders are not associated with excess mortality risks relative to other parental disorders. The greatest number of excess deaths were attributable to alcohol-related disorders, this being the most prevalent paternal diagnostic group and the second most prevalent in mothers.
Identification and interpretation of etiological mechanisms must await investigation of cause-specific mortality, which was the objective of our current investigations. Future studies should investigate the impact of parental conditions that are generally treated in community settings and estimate unbiased relative risks of perinatal mortality associated with paternal disorder.
1. Webb R, Abel K, Pickles A, Appleby L: Mortality in the offspring of people with psychotic disorders: a critical review and meta-analysis. Am J Psychiatry 2005; 162:1045–1056Google Scholar
2. Kallmann FJ: The Genetics of Schizophrenia. New York, JJ Augustin, 1938Google Scholar
3. Erlenmeyer-Kimling L: Mortality rates in the offspring of schizophrenic parents and a physiological advantage hypothesis. Nature 1968; 220:798–800Google Scholar
4. Lindelius R: A study of schizophrenia: a clinical, prognostic and family investigation. Acta Psychiatr Scand 1970; 216(suppl):1–125Google Scholar
5. Rieder RO, Rosenthal D, Wender P, Blumenthal H: The offspring of schizophrenics. Arch Gen Psychiatry 1975; 32:200–211Google Scholar
6. Modrzewska K: The offspring of schizophrenic parents in a North Swedish isolate. Clin Genet 1980; 17:191–201Google Scholar
7. Sobel DE: Infant mortality and malformations in children of schizophrenic women: preliminary data and suggested research. Psychiatr Q 1961; 35:60–64Google Scholar
8. Bennedsen BE, Mortensen PB, Olesen AV, Henriksen TB: Congenital malformations, stillbirths, and infant deaths among children of women with schizophrenia. Arch Gen Psychiatry 2001; 58:674–679Google Scholar
9. Nilsson E, Lichtenstein P, Cnattingius S, Murray RM, Hultman CM: Women with schizophrenia: pregnancy outcome and infant death among their offspring. Schizophr Res 2002; 58:221–229Google Scholar
10. Howard LM, Goss C, Leese M, Thornicroft G: Medical outcome of pregnancy in women with psychotic disorders and their infants in the first year after birth. Br J Psychiatry 2003; 182:63–67Google Scholar
11. Jablensky AV, Morgan V, Zubrick SR, Bower C, Yellachich LA: Pregnancy, delivery, and neonatal complications in a population cohort of women with schizophrenia and major affective disorders. Am J Psychiatry 2005; 162:79–91Google Scholar
12. Mitchell EA, Thompson JMD, Stewart AW, Webster ML, Taylor BJ, Hassall IB, Ford RPK, Allen EM, Scragg R, Becroft DMO: Postnatal depression and SIDS: a prospective study. J Paediatr Child Health 1992; 28(suppl 1):S13–S16Google Scholar
13. Sanderson CA, Cowden B, Hall DMB, Taylor EM, Carpenter RG, Cox JL: Is postnatal depression a risk factor for sudden infant death? Br J Gen Pract 2002; 52:636–640Google Scholar
14. Ward SL, Bautista D, Chan L, Derry M, Lisbin A, Durfee MJ, Mills KSC, Keens TG: Sudden infant death syndrome in infants of substance-abusing mothers. J Pediatr 1990; 117:876–881Google Scholar
15. Kandall SR, Gaines J, Habel L, Davidson G, Jessop D: Relationship of maternal substance abuse to subsequent sudden infant death syndrome in offspring. J Pediatr 1993; 123:120–126Google Scholar
16. Kelly RH, Danielson BH, Golding JM, Anders TF, Gilbert WM, Zatzick DF: Adequacy of prenatal care among women with psychiatric diagnoses giving birth in Calfornia in 1994 and 1995. Psychiatr Serv 1999; 50:1584–1590Google Scholar
17. Bennedsen BE, Mortensen PB, Olesen AV, Henriksen TB: Preterm birth and intra-uterine growth retardation among children of women with schizophrenia. Br J Psychiatry 1999; 175:239–245Google Scholar
18. Sacker A, Done DJ, Crow TJ: Obstetric complications in children born to parents with schizophrenia: a meta-analysis of case-control studies. Psychol Med 1996; 26:279–287Google Scholar
19. Cannon M, Jones PB, Murray RB: Obstetric complications and schizophrenia: historical and meta-analytic review. Am J Psychiatry 2002; 159:1080–1092Google Scholar
20. Webb R, Howard L, Abel K: Antipsychotic drugs for non-affective psychosis during pregnancy and postpartum [Cochrane Review], in The Cochrane Library, Issue 2, Chichester, UK, John Wiley and Sons, Ltd, 2004Google Scholar
21. Brown GW, Davidson S: Social class, psychiatric disorder of mother, and accidents to children. Lancet 1978; 1:378–381Google Scholar
22. Bågedahl-Strindlund M, Tunell R, Nilsson B: Children of mentally ill mothers: mortality and utilization of paediatric health services. Acta Paediatr Scand 1988; 77:242–250Google Scholar
23. Brent DA, Oquendo M, Birmaher B, Greenhill L, Kolko D, Stanley B, Zelazny J, Brodsky B, Bridge J, Ellis S, Salazar JO, Mann JJ: Familial pathways to early-onset suicide attempt. Arch Gen Psychiatry 2002; 59:801–807Google Scholar
24. Abel KM, Webb RT, Salmon MP, Wan MW, Appleby L: The prevalence and predictors of parenting outcomes in a cohort of mothers with schizophrenia admitted to joint mother and by psychiatric units in England. J Clin Psychiatry 2005; 66:781–789Google Scholar
25. Knudsen LB, Olsen J: The Danish Medical Birth Registry. Dan Med Bull 1998; 45:320–323Google Scholar
26. Munk-Jørgensen P, Mortensen PB: The Danish Psychiatric Central Register. Dan Med Bull 1997; 44:82–84Google Scholar
27. Munk-Jørgensen P, Kastrup M, Mortensen PB: The Danish Psychiatric Register as a tool in epidemiology. Acta Psychiatr Scand 1993; 370(suppl):27–32Google Scholar
28. Malig C: The Civil Registration System in Denmark. Technical papers number 66. Bethesda, Md, International Institute for Vital Registration and Statistics, 1996Google Scholar
29. Kesmodel U, Wisborg K, Olsen SF, Henriksen TB, Secher NJ: Moderate alcohol intake during pregnancy and risk of stillbirth and death in the first year of life. Am J Epidemiol 2002; 155:305–312Google Scholar
30. Mortensen PB, Pedersen CB, Melbye M, Mors O, Ewald H: Individual and familial risk factors for bipolar affective disorders in Denmark. Arch Gen Psychiatry 2003; 60:1209–1215Google Scholar
31. Laursen TM, Labouriau R, Licht RW, Bertelsen A, Munk-Olsen T, Mortensen PB: Family history of psychiatric illness as a risk factor for schizoaffective disorder. Arch Gen Psychiatry 2005; 62:841–848Google Scholar
32. StataCorp: Stata Statistical Software: Release 8.0. College Station (Texas), STATA Corporation, 2003Google Scholar
33. Clayton D, Hills M: Statistical Methods in Epidemiology. Oxford, Oxford University Press, 1993Google Scholar
34. Macaluso M: Exact stratification of person-years. Epidemiology 1992; 3:441–448Google Scholar
35. Li J, Laursen TM, Precht DH, Olsen J, Mortensen PB: Hospitalization for mental illness among parents after the death of a child. N Eng J Med 2005; 352:1190–1196Google Scholar
36. Gardner W, Mulvey EP, Shaw EC: Regression analyses of counts and rates: Poisson, overdispersed pPisson, and negative binomial models. Psychol Bull 1995; 118:392–404Google Scholar
37. Mortensen PB: The untapped potential of case registers and record-linkage studies in psychiatric epidemiology. Epidemiol Rev 1995; 17:205–209Google Scholar
38. Munk-Jørgensen P. Faldende førstegangsindlæggelsesrater for skizofreni i Danmark, 1970–1991 [Decreasing first admission rates for schizophrenia in Denmark, 1970–1991] [thesis]. Copenhagen, Denmark, University of Copenhagen, Dept. of Psychiatric Demography, 1995Google Scholar
39. Kessing LV: Validity of diagnosis and other clinical register data in patients with affective disorder. Eur Psychiatry 1998; 13:392–398Google Scholar
40. Kessing LV: A comparison of ICD-8 and ICD-10 diagnoses of affective disorder—a case register study from Denmark. Eur Psychiatry 1998; 13:342–345Google Scholar