Treatment Issues Related to the Use of Psychedelics, Trichotillomania, Social Anxiety Disorder, Schizophrenia, and Opioid Use Disorder
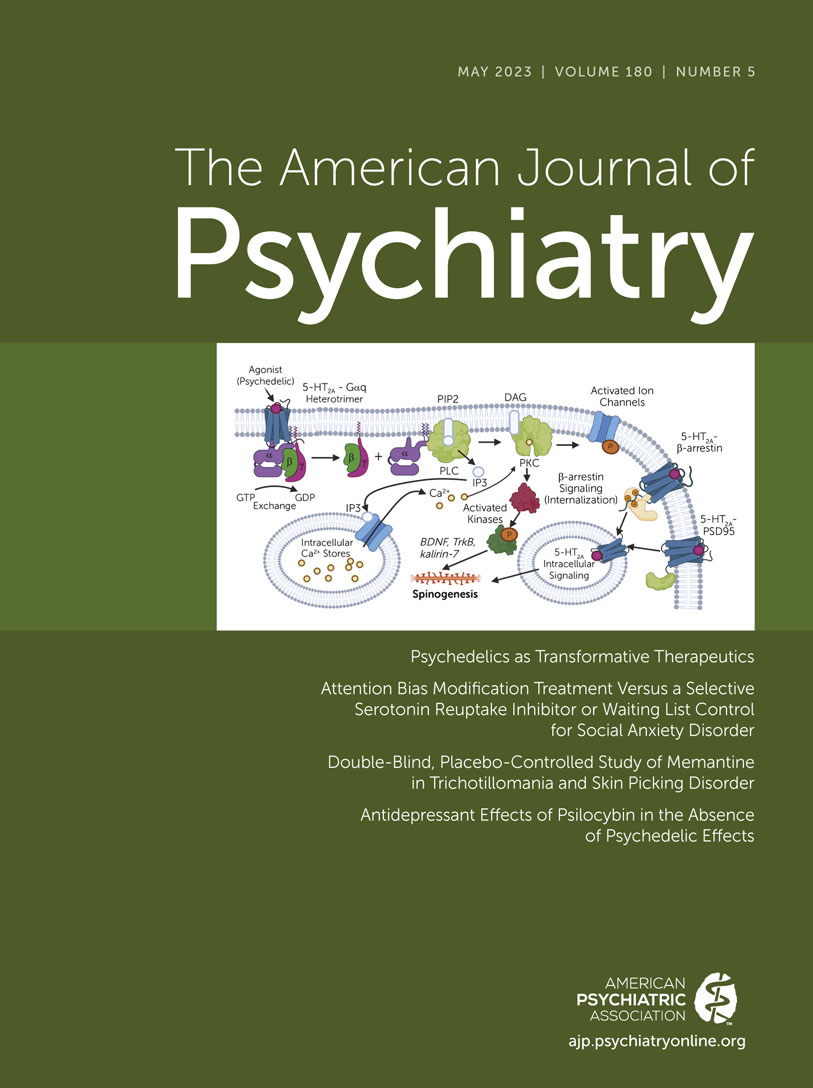
This issue of the Journal brings together clinically relevant papers, several of which are focused on new treatment development. The issue begins with an overview from Drs. Bryan Roth and Ryan Gumpper (1) that is very timely, given the high level of interest in psychedelics and the related emerging clinical trial data. In addition to discussing potential clinical applications, this paper delves into 5-HT2A receptor mechanisms and other serotonin-related, neurochemical, and molecular mechanisms. Of particular interest is the discussion regarding how understanding the mechanisms of action of psychedelics can form the basis for the development of similar potentially therapeutic compounds that are devoid of psychedelic effects. Related to this, a letter to the Editor in this issue briefly presents a case study that raises the possibility that psilocybin’s antidepressant effect is not dependent on having a psychedelic experience (2). Since trichotillomania and skin picking disorder are illnesses for which there is little evidence to support psychopharmacologic treatment approaches, we include a study that presents data from a double-blind, placebo-controlled trial assessing the efficacy of the NMDA antagonist memantine in treating individuals with these disorders. Another study compares the efficacy of a new behavioral treatment, eye-tracking-based attention bias modification training, to an SSRI for the treatment of social anxiety disorder. The issue includes two studies directly relevant to the treatment of schizophrenia. The first assesses the effectiveness of combining motivational therapy with cognitive behavioral therapy for treating motivation-related negative symptoms. The other uses a very large database to compare antipsychotic monotherapy and concomitant use of multiple antipsychotic medications in relation to serious negative medical outcomes. We also include a study that is focused on opiate misuse, attempting to understand factors that are related to overdoses in individuals who are undergoing medication treatment for opiate use disorder and opioid dependence.
Assessing the Efficacy of Memantine for Treating Trichotillomania and Skin Picking Disorder
While trichotillomania and skin picking can be debilitating, little research has focused on establishing effective pharmacotherapies for these disorders. Grant et al. (3) present data from a double-blind, placebo-controlled study assessing the effects of the NMDA antagonist memantine on reducing the symptoms associated with these disorders. Patients with the diagnoses of trichotillomania and skin picking disorder are included together in this clinical trial with the rationale that the disorders have similar symptoms and that both disorders are hypothesized to be associated with alterations in habit-related brain systems. The interest in memantine stems from preclinical work suggesting that alterations in glutamatergic function may drive habitual self-directed behaviors such as excessive grooming. In this study, 100 individuals were randomly assigned to receive either memantine (10 mg/day for 1 week and then increased to 20 mg/day) or placebo over an 8-week period. Participants could be taking other psychotropic medications if doses were stable over the preceding 3 months, and they also could be receiving psychotherapy. The primary outcome measure was the change in the NIMH symptom scale, which was initially developed for trichotillomania and later modified by the researchers for skin picking disorder. A majority of the participants (62%) had other comorbidities, with major depression (40%) and anxiety disorders (38.2%) being the most common. In the 80 individuals that completed the study, the results demonstrated memantine-related significant improvements in the primary outcome measure as well as the Sheehan disability scale and the Clinical Global Impression (CGI) severity scale. At the end of the study, assessments with the CGI improvement scale demonstrated that 60.5% of the individuals in the memantine group were deemed to be much or very much improved as compared to 8.3% of individuals in the placebo group. The effect size in this study was large and memantine was well tolerated, with adverse effects not significantly differing from the placebo group. In their editorial, Drs. Erica Greenberg and Daniel Geller from the Massachusetts General Hospital and Harvard University (4) put the findings into context and further discuss their implications.
Treating Social Anxiety Disorder: Eye-Tracking-Based Attention Modification Bias Training Versus an SSRI
With additional treatments needed for social anxiety disorder, this paper by Arad and colleagues (5) explores the relative efficacy of attention bias modification training compared with SSRIs and a waiting list comparison group in decreasing social anxiety symptoms. Attention bias modification training has shown promise in treating social anxiety disorder, based on the idea that attentional training will decrease the bias of anxious individuals’ to preferentially orient toward what they perceive as threatening faces and thereby mediate the reduction of social avoidance symptoms. In this study, 105 individuals with social anxiety disorder were randomly assigned to one of the three 12-week treatment conditions. The eye-tracking-based attention bias modification group received 10 training sessions over this period, the SSRI group received escitalopram up to 20 mg/day (with an average maximum dose of 11.6 mg/day), and the waiting list group received no treatment with the expectation that they later would receive attention bias modification training. The primary outcome measure was the clinician-rated severity score on the Leibowitz Social Anxiety Scale that was collected by raters who were unaware of the participants’ treatment condition. Results demonstrated that both active treatments significantly reduced social anxiety symptoms when compared to the waiting list group, and there was no significant difference between attention bias modification and SSRI treatment. SSRI treatment significantly decreased depression symptoms, whereas this was not the case for attention bias modification treatment. In contrast, attention bias modification treatment, and not SSRIs, decreased the amount of time participants spent looking at threatening compared with neutral faces. However, individual differences in this effect were not associated with treatment responses. Taken together, these findings support the use of attention bias modification training in the treatment of social anxiety disorder and point to the importance of SSRI treatment in patients that also have comorbid depression symptoms. There are some issues in the design of this study that should be considered in the interpretation of the data, which include the use of a waiting list control as a comparator group and the relative low dose of escitalopram that was used. In his editorial, Dr. Colin MacLeod from the University of Western Australia (6) provides the background for the rationale underlying the use of attention bias modification, highlights the findings from this paper, and suggests future potential applications of attention bias modification training.
Testing the Efficacy of a Novel Treatment for Motivation-Related Negative Symptoms in Schizophrenia
Reddy et al. (7) report data from a randomized clinical trial in schizophrenia patients that assesses the efficacy of a novel psychotherapeutic intervention that is aimed at reducing the negative symptoms of schizophrenia associated with decreased motivation. The authors point out that negative symptoms, such as decreased drive and volition, are particularly important in contributing to the real world marked functional disabilities experienced by many schizophrenia patients. The 12-week intervention used in this study combined motivational interviewing with cognitive behavioral therapy (CBT), with the idea that the combination of these strategies would optimize outcomes, in part by facilitating adherence to treatment while targeting deficits in motivational processes. Previous studies have shown CBT and motivational interviewing to be helpful in treating schizophrenia. In this study, 79 patients were randomly assigned to receive 12 weeks of motivational interviewing/CBT or as a comparator, mindfulness training. Assessments were also performed at 24 weeks, which was 12 weeks after the conclusion of treatment. One of the primary outcome measures was the Motivation and Pleasure subscale of the Clinical Assessment Interview for Negative Symptoms (CAINS-MAP); another was a measure of community functioning as assessed with the Specific Level of Function scale. Results demonstrated that the motivational interviewing/CBT intervention group had a significant reduction in the CAINS-MAP scores at the end of the intervention period, which did not occur in the mindfulness intervention group. The effects of motivational interviewing/CBT compared with mindfulness training were less prominent when assessed 12 weeks after the intervention. However, when assessing the effects of the interventions on community functioning, only a nonsignificant trend toward an increase in functioning after acute treatment was observed in the mindfulness/CBT intervention group. In their editorial, Drs. Meyer-Kalos and Vinogradov from the University of Minnesota (8) provide a historical perspective on the negative symptoms of schizophrenia, discuss the interpretation of the findings in relation to study design issues, and emphasize the need to systematically target neurocognitive and reward-related symptoms with behavioral interventions in schizophrenia patients.
A Within-Participant, Longitudinal Assessment of Antipsychotic Monotherapy Versus Polypharmacy in Relation to Nonpsychiatric Hospitalizations
The use of polypharmacy is common in psychiatry, as is the case throughout medicine. Understanding and developing an evidence base to inform the drawbacks and virtues of polypharmacy is critical, especially for treating illnesses that require long-term therapies. Taipale et al. (9) address the question of antipsychotic monotherapy versus polypharmacy in the treatment of schizophrenia. More specifically, using a database from Finland consisting of all hospitalized individuals diagnosed with schizophrenia between 1972–2014 (N=61,889), this study focuses on the propensity of antipsychotic monotherapy and antipsychotic polypharmacy treatment to be associated with the development of significant medical problems as indexed by nonpsychiatric and cardiovascular-related hospitalizations. This large database with follow-up for a mean of 8.8 years provides a unique opportunity to address, at a within-subject level, the co-occurrence of monotherapy, polypharmacy, or no medications at seven dose levels with medical hospitalizations. Over the follow-up across all individuals, 45.9% of the time was spent being treated with antipsychotic monotherapy, 33.8% of the time with multiple antipsychotics, and 20.3% of the time with no antipsychotic use. Regardless of the specific medication used, the most common dosing was in the high dosage range as characterized by the defined daily dose, a metric used to relate doses across different drugs within a class in relation to a stated average daily maintenance dose. Monotherapy and polypharmacy treatment were both common within individuals, as 79% of individuals had treatment periods of monotherapy, 68% had treatment periods with multiple antipsychotics, and 75% had periods when they took no antipsychotics. Results demonstrated a significantly reduced risk of nonpsychiatric hospitalizations in individuals when using polypharmacy at doses greater than the 1.1 defined dose per day as compared to monotherapy in the same dosage range. The highest polypharmacy dose range (≥1.6 defined dose per day), compared to monotherapy, was also associated with an 18% reduction in the risk for a cardiovascular-related hospitalization. In their editorial (10), Drs. Robert Buchanan and Julie Kreyenbuhl from the University of Maryland discuss other work supporting the use of multiple antipsychotic agents in treating schizophrenia and consider potential factors that may underlie the observed decrease in significant medical morbidity when individuals were treated with multiple antipsychotic drugs.
Identifying Factors Associated With Overdose During Medication Treatment for Opioid Use Disorder
The human cost of drug abuse and in particular opiate abuse is incalculable and on the rise. From April 2020 to April 2021, the CDC estimated that there were 100,306 drug-related overdose deaths, with 75,637 of these attributed to opioids (11). While effective medication treatment for opiate use disorder mitigates the risk of overdosing, during treatment for opiate use disorder there continues to be considerable overdose risk. Brandt and colleagues (12) focused on identifying factors associated with this risk in individuals undergoing treatment with the hope that this will enable better identification of individuals that are at the greatest risk. To acquire a large data set, the researchers used data from three randomized clinical trials that were performed within the National Institute on Drug Abuse Clinical Trials Network. This resulted in data from 2,199 individuals undergoing medication treatment for opioid use disorder or opioid dependence that were treated with either methadone (N=283), extended-release injected naltrexone (N=529), or buprenorphine/naloxone (4:1) (N=1,387). The risk of overdose was assessed 24 weeks after beginning treatment. Over this time period, 39 participants had at least one overdose with a total occurrence of 57 overdoses. Opioids were involved in 28 of the overdoses, and seven were believed to involve benzodiazepines, the other most frequent class of drugs used to overdose. Across all the studies, individuals assigned to naltrexone treatment had the highest level of overdoses at 5.3% compared with methadone at 1.51% and buprenorphine at 1.15%. The higher percentage of overdoses in the naltrexone group could in part be attributed to the fact that more individuals in this group did not initiate treatment. Patients that reported taking benzodiazepines during the 28-day period prior to the study were at greater risk for overdose (hazard ratio=3.36) as were individuals that either did not initiate treatment (hazard ratio=6.64) or dropped out of treatment (hazard ratio=4.04). Drs. Roger Weiss and Hillary Connery from McLean Hospital and Harvard Medical School contribute an editorial (13) in which they review approved medication treatments for opioid use disorder, discuss the findings from this study in greater detail, and emphasize the critical factor of treatment retention in facilitating positive outcomes and reducing overdoses.
Conclusion
This issue of the Journal presents papers that are very clinically relevant, with an update on psychedelics and their putative mechanisms of action along with studies addressing the efficacy of novel treatments for trichotillomania, social anxiety disorder, and the negative symptoms of schizophrenia. Major findings include 1) the efficacy of the NMDA antagonist memantine in treating trichotillomania and skin picking disorder; 2) how eye-tracking-based attention bias modification training performs as well as escitalopram in treating social anxiety disorder; 3) that treatment approaches combining motivational interviewing with CBT show promise in reducing negative symptoms related to decreased motivation in schizophrenia patients; 4) how in schizophrenia patients followed longitudinally, periods of multiple antipsychotic drug use were not associated with more nonpsychiatric hospitalizations (and that at the higher dose ranges the risk was actually reduced); and 5) the increased risk of overdose in individuals undergoing medication treatment for opiate use disorder was more likely to occur in individuals who were treated with naltrexone, had a recent history of benzodiazepine use, or who were not adherent to the treatments.
Taken together, the findings reported in this issue highlight new promising clinical approaches and provide clinically useful insights into current treatments while presenting the science underlying the potential efficacy of psychedelics, the possible negative consequences associated with these drugs, and, importantly, a pathway for developing treatments that target similar mechanisms without producing psychedelic effects.
1. : Psychedelics as transformative therapeutics. Am J Psychiatry 2023; 180:340–347Abstract, Google Scholar
2. : Antidepressant effects of psilocybin in the absence of psychedelic effects. Am J Psychiatry 2023; 180:395–396Abstract, Google Scholar
3. : Double-blind placebo-controlled study of memantine in trichotillomania and skin-picking disorder. Am J Psychiatry 2023; 180:348–356Abstract, Google Scholar
4. : Cautious optimism for a new treatment option for body-focused repetitive behavior disorders. Am J Psychiatry 2023; 180:325–327Abstract, Google Scholar
5. : Attention bias modification treatment versus a selective serotonin reuptake inhibitor or waiting list control for social anxiety disorder: a randomized clinical trial. Am J Psychiatry 2023; 180:357–366Abstract, Google Scholar
6. : The attention bias modification approach to anxiety: origins, limitations, and opportunities. Am J Psychiatry 2023; 180:328–330Abstract, Google Scholar
7. : A novel psychosocial intervention for motivational negative symptoms in schizophrenia: combined motivational interviewing and CBT. Am J Psychiatry 2023; 180:367–376Abstract, Google Scholar
8. : Treating pathologies of the will. Am J Psychiatry 2023; 180:331–333Abstract, Google Scholar
9. : Safety of antipsychotic polypharmacy versus monotherapy in a nationwide cohort of 61,889 patients with schizophrenia. Am J Psychiatry 2023; 180:377–385Abstract, Google Scholar
10. : An argument for antipsychotic polypharmacy. Am J Psychiatry 2023; 180:334–336Abstract, Google Scholar
11. : Provisional Drug Overdose Death Counts. Atlanta, Centers for Disease Control and Prevention, 2023. https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htmGoogle Scholar
12. : Risk of experiencing an overdose event for patients undergoing treatment with medication for opioid use disorder. Am J Psychiatry 2023; 180:386–394Abstract, Google Scholar
13. : Drug overdose prevention: an exercise in optimism. Am J Psychiatry 2023; 180:337–339Abstract, Google Scholar