Impacts of Structural Racism, Socioeconomic Deprivation, and Stigmatization on Mental Health
As a field, we need to prioritize critical social and environmental factors that impact individuals’ well-being and mental health. The degree of trauma and stress associated with structural racism, socioeconomic deprivation, and the stigmatization of mental illness is immense, and because of its pervasiveness its toll on human suffering is inestimable. While each are important in their own right, these societal factors are inextricably linked in complex ways that promote the development of psychiatric disorders and impede access to, and the delivery of, mental health care. It is important to recognize, and admit, that in the past, American Psychiatry espoused racist views that were directly damaging to BIPOC individuals and contributed to structural racism (1). Additionally, Psychiatry has a history of pathologizing issues related to sexual identity and gender orientation resulting in further distress to already marginalized individuals and to the stigmatization of the LGBTQ community.
In the September 2020 issue of AJP, the Deputy Editors and myself published a statement that reflected our commitment to use the Journal to combat racism, social injustice, and health care inequities (2). We stated that our goal was to prioritize the publication of scientific data and clinical information aimed at fighting racism and its devastating effects on psychiatric care and well-being. The current issue of AJP represents a step in this direction as we present papers that focus on the role of structural racism in psychiatry and psychiatric illnesses. In an Overview that serves as a centerpiece for this issue, Dr. Ruth Shim from the University of California at Davis presents a strategy to dismantle structural racism in psychiatry with the aim of achieving mental health equity (1). It is my hope that this paper will serve as a foundational “blueprint” for the field as we move forward in our goal to achieve equitable mental health care for all individuals. Other papers in this issue focus on racism as a societal factor that increases the risk of developing psychotic disorders, the impact of socioeconomic deprivation on the heritability of educational attainment, and methods to reduce the stigmatization of individuals with illnesses such as schizophrenia. In addition to these papers, we also include a review on suicide prevention authored by Christina Michel and colleagues from Columbia University, and three papers relevant to opioid use and the treatment of opioid use disorder.
Racism as a Social Determinant of Psychosis in the United States
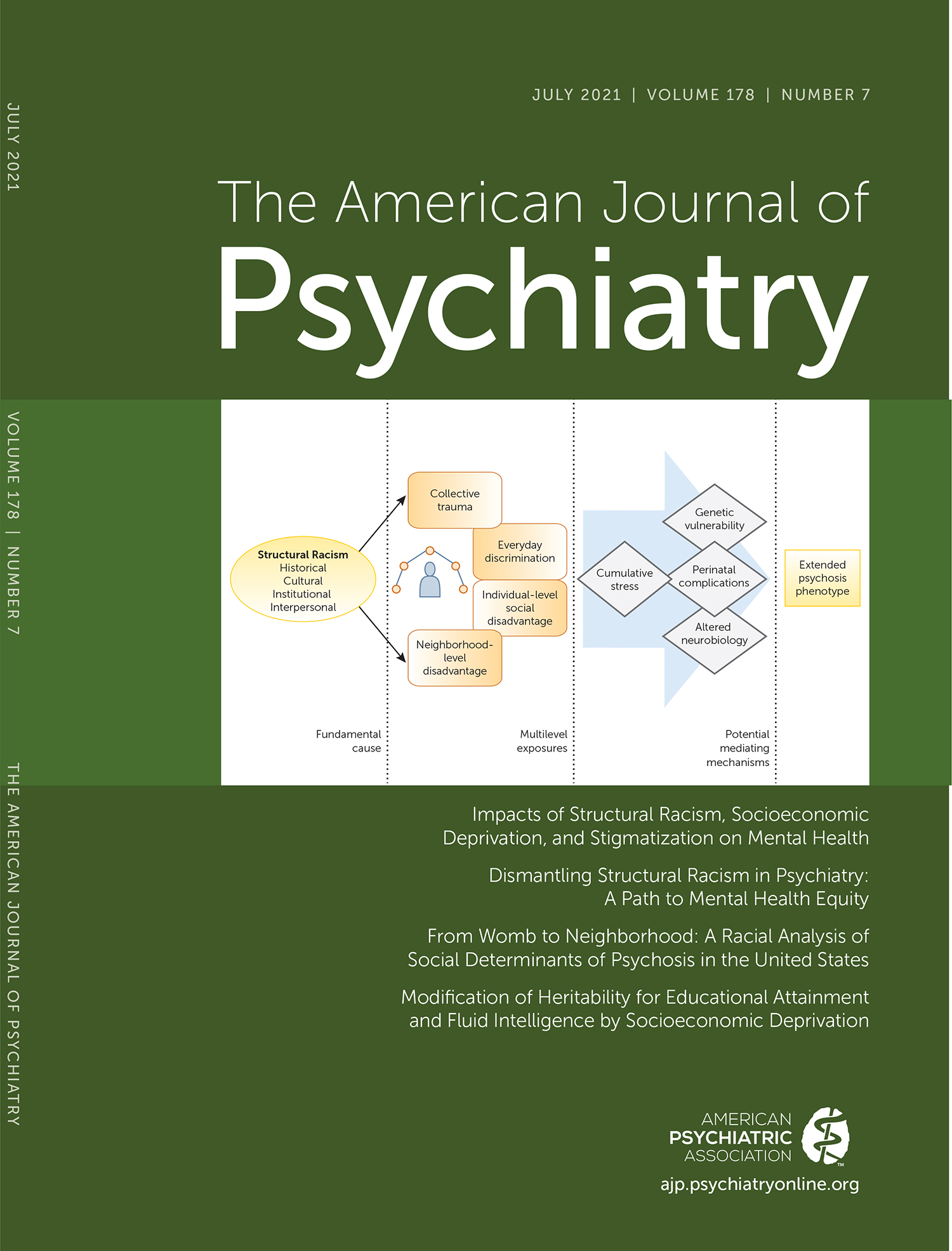
Anglin and coauthors (3) discuss the potential impacts of structural racism in relation to the inequities in social and environmental factors that are associated with the increased risk to develop psychotic symptoms. While considerable work has been done in other countries, the authors point out the need for large scale studies in the United States to effectively understand the role that social inequities, specific to the U.S. population, play in psychiatric illnesses. These studies should be designed to take into account factors such as race-related misdiagnoses (i.e., a diagnosis bias in which schizophrenia is overdiagnosed and affective disorders underdiagnosed in Black individuals), and socioeconomic disparities. The main focus of the current paper is the presentation of a model that links racism to the risk to develop psychosis. Specifically, the model highlights the impacts of structural racism on critical intermediary factors involved in promoting the emergence of psychotic symptoms, such as impoverished neighborhoods, increased levels of ongoing trauma and stress, and increased pre- and postnatal complications affecting early infant development. It should be noted that while the focus of the Anglin et al. paper is on the development of psychosis, in reality their model is relevant to all psychiatric illnesses. The authors conclude their paper with the following call to action: “We recommend that the field of psychiatry devote considerably more effort to addressing the structural racism and social determinants of psychosis in funding priorities, training, and intervention development.” Drs. Nathaniel Harnett and Kerry Ressler from McLean Hospital and Harvard Medical School contribute an editorial on this paper that further expands on the importance of recognizing the trauma caused by systemic racism (4). As an exemplar of ongoing research in this area, they discuss findings from the Grady Trauma Project, which to date has studied over 12,000 participants, 90% of whom are Black. Their editorial also emphasizes the importance of focusing future scientific efforts on identifying the biological pathways (e.g., neural circuits and epigenetic mechanisms) by which racism-related stress, trauma, and discrimination increase the risk to develop psychopathology.
Socioeconomic Deprivation in the UK Interacts With the Heritability of Educational Attainment
Rask-Andersen et al. (5) use genetic and socioeconomic data from the UK Biobank to understand potentially important gene x environment interactions in relation to measures of intelligence and educational success. The study is remarkable because of its large sample size (362,498 participants) and is highly relevant to understanding how environments may differentially impact the heritability of such important outcomes as educational attainment. Participants in this study were classified into five socioeconomic groups based on their current score on the Townsend deprivation index, a measure that incorporates various metrics associated with socioeconomic status. Using measures of heritability based on genomewide single nuclear polymorphism (SNP) assessments, as well as polygenic risk scores, the researchers found that genetics appeared to have a greater impact on fluid intelligence, educational attainment, and years of education in individuals with higher levels of socioeconomic deprivation. Stated another way, the findings suggest that socioeconomic deprivation appears to favor genetic, compared with environmental, influences in relation to educational attainment. For example, in relation to determinants associated with years of education, SNP heritability for the most deprived socioeconomic group was estimated to be 24.3% as compared with 13.8% in the most privileged group. The findings from this study provide insights into how interactions between heritability and environment may be related to the substantial challenges that individuals living in impoverished environments must overcome to reach success. It is important to point out that the sample in this study consisted of only Caucasian individuals and the generalizability of these findings to other populations outside the UK remains to be determined. Future work needs to incorporate racially and culturally diverse samples to understand the interactions between heritability and environment in individuals that also suffer from the consequences of racism and social injustice. Dr. David Hill from the University of Edinburgh provides an editorial (6) that discusses these findings and offers alternative explanations for the GWAS findings, including the possibility of so called “genetic nurturing effects.”
Developing Methods to Decrease Stigma Toward Individuals With Psychosis
In addition to racial discrimination, societal stigmatization is another form of prejudice that is commonly aimed at individuals suffering from mental illness. Stigmatization is especially prominent for individuals with the most severe illnesses such as psychosis. In addition to the impacts of stigmatization on self-esteem, stigmatization can decrease the motivation of affected individuals to seek care. Amsalem and coauthors (7) present data from a randomized study in which they attempted to reduce stigma-related attitudes toward individuals with psychosis in a cohort of 18–30-year-olds. This late adolescent/young adult age range was selected for various reasons, including the reality that this age period is a common time for the emergence of first psychotic episodes. In this study, 1,055 individuals were recruited using an internet-based crowdsourcing platform. They were then randomly assigned into one of three groups: brief video intervention, written vignette intervention with the same material as the video, or no intervention. Seventy-three percent of the sample identified themselves as White, while only 11% identified as Hispanic and 1% as African American. The brief video intervention consisted of viewing a 90-second video of a woman with schizophrenia discussing her symptoms along with her ability to work and engage in satisfying relationships. Assessments related to stigmatization were made prior to the intervention, postintervention, and 30 days after the intervention. The data demonstrated superior effects of the video intervention: individuals in this group compared with the other groups had significantly greater immediate and sustained reductions in their stigma-related attitudes. Taken together, these data are encouraging as they support the use of a simple and brief method with the potential to change negative attitudes toward individuals suffering from psychiatric disorders. In an accompanying editorial, Dr. Stephen Marder from UCLA discusses stigma specifically in relation to schizophrenia and emphasizes the importance of humanizing the illness as a means to reduce stigma (8). He further discusses how stigmatization can delay the length of time for individuals to seek treatment for their first psychotic episode and how this can result in poorer long-term outcomes.
Overdose and Drug-Related Poisonings in Relation to the Concomitant Use of Benzodiazepine and Z-Drugs With Opioids and Buprenorphine
Two papers in this issue address potentially harmful outcomes in patients concomitantly taking benzodiazepines or Z-drugs with opioids. Szmulewicz et al. (9) report that patients prescribed Z-drugs (i.e., zolpidem, zopiclone, or zaleplon) for sleep-related problems in conjunction with prescribed opioids had a significantly increased risk of unintentional overdose as compared with patients that were taking opioids and not Z-drugs. Although this finding is well known in relation to the combination of benzodiazepines with opioids, less data exists for Z-drugs. It is important to point out that while Z-drugs are not benzodiazepines, they have similar effects via their actions on modulating GABA-A receptor function. Data from the current study compared data derived from the claim records of 510,529 patients that were prescribed opiates with Z-drugs and with data from a sample of the same number of individuals that were prescribed opiates and not Z-drugs. There were 217 overdoses reported in the group that took opiates with Z-drugs compared with 57 overdoses in the group that only took opiates. When controlling for various other factors, the authors report an overdose hazard ratio of 2.29 that was associated with the combination of opiates and Z-drugs. It is important to point out that while the combination of Z-drugs with opiates appeared to increase risk, the overall incidence of unintentional overdoses across both groups was of a low frequency.
Buprenorphine, a mixed opiate agonist/antagonist, and benzodiazepine/Z-drugs are commonly used to treat symptoms and maintain abstinence in opiate use disorder patients. Xu et al. (10) examine the use of these medications in relation to “poisoning” events in patients with opiate use disorder. The data used in this study were based on a large pharmaceutical claim database that allowed the investigators to identify 23,036 individuals that had been treated with buprenorphine and had nonlethal drug-related poisoning events, including overdoses. The analytic design tracked data within subjects over time, characterizing the relation between the timing of their medication use (buprenorphine, benzodiazepine/Z-drugs, and their combination) in relation to episodes of drug poisoning. Overall, the results demonstrated that buprenorphine treatment days were associated with a 40% decrease in poisoning events compared with an 88% increase in poisonings associated with taking benzodiazepine or Z-drugs. The increased risk associated with benzodiazepines and Z-drugs appeared to be dose dependent. Interestingly, the effects of high-dose benzodiazepine/Z-drugs on increasing poisonings appeared to be lessened during periods in which individuals also took buprenorphine.
Sublingual Buprenorphine/Naloxone versus Injectable Naltrexone in Treating Opioid Use Disorder
Nunes and coauthors (11) present data from secondary analyses of a randomized clinical trial comparing the efficacy of buprenorphine-naloxone (N=287) to injectable extended-release naltrexone (N=283) in inpatients planning to begin treatment for opioid use disorder (12). Consistent with real-world treatment, a number of the participants failed to initiate treatment, and overall both treatments were found to be equally effective. The results of the current analyses were interesting and varied as to whether patients were homeless. For example, patients that were homeless had lower relapse rates (41.4%) when taking extended-release naltrexone as compared with a relapse rate of 68.6% when taking buprenorphine-naloxone. This difference in relapse rate was not observed in individuals that were not homeless. The better outcomes observed in homeless individuals taking extended-release naltrexone compared with daily buprenorphine-naloxone are not surprising and were likely due to the greater difficulty this population has in adhering to treatment regimens that require daily dosing. In her editorial, Dr. Kathleen Brady from the Medical University of South Carolina discusses the generalizability of the findings in relation to the study design, provides an overview of available treatments for opioid use disorder, and emphasizes the hurdles associated with initiating treatments in this population (13).
Conclusions
This issue of the Journal highlights papers focused on the severe negative impacts of structural racism, socioeconomic disparities, and stigmatization on mental health and well-being. I am very grateful to the authors that provided these papers. As the Editor-in-Chief of AJP, I view papers in this area as a priority and invite others to submit manuscripts relevant to systemic racism and other societal inequities as they impact mental health. In addition, I want to emphasize action steps that I believe we must take as a profession in our efforts to combat the influences of structural racism and to effectively care for the mental health of marginalized individuals. To help promote change, individual psychiatrists need to commit to antiracist and destigmatizing strategies aimed at developing equitable mental health care for BIPOC and other underprivileged or excluded individuals. Academic Departments of Psychiatry need to create welcoming and supportive environments for these individuals with the intention of prioritizing their clinical and research training. Academic Departments, along with NIMH, must also prioritize research efforts that will ultimately result in the improvement of mental health for BIPOC and marginalized individuals. Leaders in the field, academic institutions, and our professional societies must vigorously advocate for new laws that will institutionalize equity and social justice at the societal level. This issue of AJP is intentionally comprised of papers addressing the consequences of structural racism on mental health. It is my hope that the contents of this issue will serve as a clear signal to the field that AJP is prioritizing papers in this area and is fully committed to antiracist efforts.
1. : Dismantling structural racism in psychiatry: a path to mental health equity . Am J Psychiatry 2021 ; 178 : 592 – 598 Link, Google Scholar
2. : The American Journal of Psychiatry’s commitment to combat racism, social injustice, and health care inequities . Am J Psychiatry 2020 ; 177 : 791 Link, Google Scholar
3. : From womb to neighborhood: a racial analysis of social determinants of psychosis in the United States. Am J Psychiatry 2021 ; 178:599–610 Google Scholar
4. : Structural racism as a proximal cause for race-related differences in psychiatric disorders (editorial) . Am J Psychiatry 2021 ; 178 : 579 – 581 Link, Google Scholar
5. : Modification of heritability for educational attainment and fluid intelligence by socioeconomic deprivation in the UK Biobank . Am J Psychiatry 2021 ; 178 : 625 – 634 Link, Google Scholar
6. : Environmental influences on genetic contributions to intelligence and education (editorial) . Am J Psychiatry 2021 ; 178 : 582 – 583 Link, Google Scholar
7. : Sustained effect of a brief video in reducing public stigma toward individuals with psychosis: a randomized controlled trial of young adults . Am J Psychiatry 2021 ; 178 : 635 – 642 Link, Google Scholar
8. : Changing the face of schizophrenia (editorial) . Am J Psychiatry 2021 ; 178 : 584 – 585 Link, Google Scholar
9. : The risk of overdose with concomitant use of Z-drugs and prescription opioids: a population-based cohort study . Am J Psychiatry 2021 ; 178 : 643 – 650 Link, Google Scholar
10. : Association between benzodiazepine or Z-drug prescriptions and drug-related poisonings among patients receiving buprenorphine maintenance: a case-crossover analysis . Am J Psychiatry 2021 ; 178 : 651 – 659 Link, Google Scholar
11. : Sublingual buprenorphine-naloxone compared with injection naltrexone for opioid use disorder: potential utility of patient characteristics in guiding choice of treatment . Am J Psychiatry 2021 ; 178 : 660 – 671 Link, Google Scholar
12. : Comparative effectiveness of extended-release naltrexone versus buprenorphine-naloxone for opioid relapse prevention (X:BOT): a multicentre, open-label, randomised controlled trial . Lancet 2018 ; 391 : 309 – 318 Crossref, Medline, Google Scholar
13. : Optimizing treatment for opioid use disorder (editorial) . Am J Psychiatry 2021 ; 178 : 586 – 587 Link, Google Scholar