Computer-Assisted Delivery of Cognitive-Behavioral Therapy for Addiction: A Randomized Trial of CBT4CBT
Abstract
Objectives: This study evaluated the efficacy of a computer-based version of cognitive-behavioral therapy (CBT) for substance dependence. Method: This was a randomized clinical trial in which 77 individuals seeking treatment for substance dependence at an outpatient community setting were randomly assigned to standard treatment or standard treatment with biweekly access to computer-based training in CBT (CBT4CBT) skills. Results: Treatment retention and data availability were comparable across the treatment conditions. Participants assigned to the CBT4CBT condition submitted significantly more urine specimens that were negative for any type of drugs and tended to have longer continuous periods of abstinence during treatment. The CBT4CBT program was positively evaluated by participants. In the CBT4CBT condition, outcome was more strongly associated with treatment engagement than in treatment as usual; furthermore, completion of homework assignments in CBT4CBT was significantly correlated with outcome and a significant predictor of treatment involvement. Conclusions: These data suggest that CBT4CBT is an effective adjunct to standard outpatient treatment for substance dependence and may provide an important means of making CBT, an empirically validated treatment, more broadly available.
Cognitive-behavioral therapy (CBT) has a comparatively strong level of empirical support across a range of psychiatric disorders (1 – 3) , including substance use disorders (1 , 4 , 5) . Despite evidence of positive and durable outcome (6 , 7) , CBT remains rarely implemented in the range of settings where individuals with substance use disorders are treated (8) . There are a number of obstacles to delivering CBT and other empirically validated therapies in clinical practice, including the limited availability of professional and specialty training programs that provide high-quality training, supervision, and certification in CBT (9) ; high rates of clinician turnover and lack of a CBT-trained workforce in many treatment settings (10 – 12) ; the relative complexity and cost of training clinicians in CBT (13 , 14) ; and high caseloads and limited resources. Available evidence suggests that although many clinicians report using CBT, they tend to overestimate their use of this and other empirically supported therapies (15) .
Hence, computer-assisted delivery of CBT, if demonstrated to be feasible and effective, could play an important role in broadening its availability and improving the quality of addiction treatment. Computer-assisted therapy could provide a comparatively low-cost means of teaching CBT skills to more substance users and allow clinicians to focus on acute concerns and problems of the individuals with whom they work. Moreover, by standardizing treatment delivery, computer-assisted training could also provide more consistent, and perhaps more effective, teaching and demonstration of CBT than is available in some settings through its capacity to convey information by means of a range of media (text, video, audio instruction, and interactive exercises). The ability to select or tailor content to address the needs of particular individuals allows for a choice of different topics, control over the speed of presentation of information, and repetition of modules when necessary. These flexible parameters may be especially important for substance abusers, many of whom experience significant cognitive impairment, including memory and concentration problems, particularly in the early stages of treatment (16 , 17) .
In the treatment of depression and anxiety disorders, computer-assisted delivery of CBT has been demonstrated in randomized trials to be both effective (18 – 25) and cost-effective (26) . However, there have been few evaluations of computer-assisted treatment of any type of addiction. Much of this work has been done in the area of smoking, in which several randomized trials of predominantly cognitive-behavioral interventions or self-help guidelines delivered by means of computers/the Internet have indicated positive effects on quit rates or attempts (27 – 29) . Computer-assisted brief motivational approaches and self-control training programs have shown promise in randomized, controlled trials with problem drinkers (30 , 31) and college students (32) . A computer-based HIV/AIDS education program was more effective than counselor-provided education in helping injection drug users learn and retain information about HIV, although both approaches were comparable in reducing HIV risk behaviors (33) .
In this report, we describe main outcome findings from a randomized clinical trial of a six-module computer-based training in CBT (CBT4CBT) skills, in which individuals entering a community-based clinic were randomly assigned to standard treatment (treatment as usual) or treatment as usual plus CBT4CBT over a period of 8 weeks. Given the established efficacy of CBT across a range of addictions and the unavailability of empirically validated therapies in many community based settings, CBT4CBT was evaluated in terms of one model of how it might be used in clinical practice, that is, as a stand-alone addition to regular clinical practice delivered to a heterogeneous group of individuals seeking treatment for addiction. The primary hypothesis was that individuals assigned to CBT4CBT would reduce their frequency of substance use and submit fewer positive urine toxicology screens than those randomly assigned to treatment as usual. Given data from previous CBT trials linking compliance, homework completion, and outcome (34 – 36) , a secondary hypothesis was that treatment engagement, including homework completion, in the CBT4CBT program would be more strongly linked to positive substance use outcomes than treatment as usual.
Method
Participants
The participants were recruited from individuals seeking treatment at Liberation Program’s Mill Hill Clinic, a community-based outpatient substance abuse treatment provider in Bridgeport, Conn. The participants were English-speaking adults who met DSM-IV criteria for any current substance dependence disorder, including alcohol, cocaine, opioids, or marijuana. Exclusion criteria were minimal to facilitate recruitment of a clinically representative group of individuals seeking treatment in a community setting. Thus, individuals were excluded only if they 1) had not used alcohol or illegal drugs within the past 28 days or failed to meet DSM-IV criteria for a current substance dependence disorder, 2) had an untreated psychotic disorder that precluded outpatient treatment, or 3) were unlikely to be able to complete 8 weeks of outpatient treatment due to a planned move or pending court case from which incarceration was likely to be imminent.
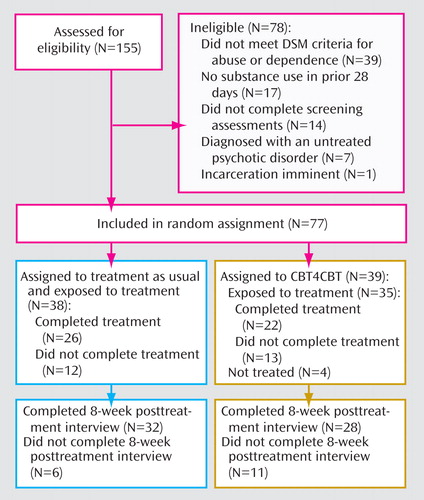
As shown in the participant flow diagram ( Figure 1 ), 77 of the 155 individuals screened were determined to be eligible for the study, provided written informed consent, and were randomly assigned to groups. Following a complete description of the study and provision of written informed consent approved by the Yale University School of Medicine Human Investigations Committee, the participants were randomly assigned to either treatment as usual or CBT4CBT with a computerized urn randomization program (37) to balance treatment groups with respect to primary substance used, gender, and ethnicity.
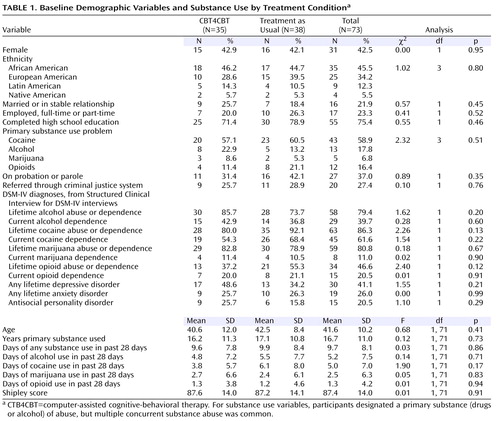
a CBT4CBT=computer-assisted cognitive-behavioral therapy.
Treatments
All participants were offered standard treatment at the clinic, which consisted of weekly individual and group sessions of general drug counseling. All participants also met twice weekly with an independent clinical evaluator who collected urine and breath specimens, assessed recent substance use, and monitored other clinical symptoms. Those randomly assigned to the CBT4CBT condition were provided access to the computer program in a small private room within the clinic. A research associate guided participants through their initial use of the CBT4CBT program and was available to answer questions and assist participants each time they used the program. The participants accessed the program through an identification/password system to protect confidentiality.
The CBT4CBT program was intended to be user-friendly, requiring no previous experience with computers and minimal use of text-based material. The multimedia style of the program was based on elementary-level computer learning games, and the presentation of material was done in a range of formats, including graphic illustrations, videotaped examples, verbal instructions, audio voiceovers, interactive assessments, and practice exercises.
The program consisted of six lessons, or modules, the content of which was based closely on a CBT manual published by the National Institute on Drug Abuse (38) used in several previous randomized, controlled trials in a range of substance-using populations (6 , 39 , 40) . The modules covered the following core concepts: 1) understanding and changing patterns of substance use, 2) coping with craving, 3) refusing offers of drugs and alcohol, 4) problem-solving skills, 5) identifying and changing thoughts about drugs and alcohol, and 6) improving decision-making skills. The first module provided a brief explanation of how to use and navigate the program; following completion of the first module, the participants could choose to access the modules in any order they preferred and repeat any section or module as many times as they wished.
Each module in the CBT4CBT program was structured as follows. First, the key concept for each module was introduced through a brief “movie” using actors and realistic settings depicting situations in which an individual was offered drugs or had to cope with a challenging situation in which substance use was likely. Next, after the narrator explained the key skill covered in that module with graphics and voiceovers, the “movie” was repeated, this time with a different ending, as the same characters applied the skills to change the outcome of the situation so as to avoid substance use (e.g., emphasis was on how individuals could use the CBT skills to “change their story”). Additional videotaped vignettes were used to reinforce the skills taught (e.g., in the “refusal skills” module, the user could click buttons to see additional examples of the characters demonstrating assertive versus aggressive versus passive responding). Next, each module included an interactive assessment followed by a short vignette with an actor explaining how use of each skill had helped him/her avoid substance use and how each CBT principle could be applied to other problems; the intention of this section was to address common areas of resistance in CBT (“Why should I do homework?”) and to emphasize how CBT skills could be generalized beyond substance use issues. Finally, each module concluded with the narrator providing a review of the key points covered, followed by the characters demonstrating how they would complete the “homework” or practice assignment for that module based on the situation depicted in the movie. The participants were then given an identical practice assignment and a reminder sheet to take with them.
This general sequence of activities was intended to be similar to the CBT manual’s (38) therapist guidelines for structuring sessions (introduction of the skill topic, didactic instruction, practice through modeling and role playing, assessment of the patient’s understanding of the material, and assignment of homework). However, this sequence also capitalized on the unique advantages of multimedia computer-assisted instruction, including presentation of information in a range of media formats. Each module was intended to require about 45 minutes to complete, depending on the speed with which the user navigated the program and the amount of material he or she selected to access or repeat.
Assessments
The participants were assessed before treatment, twice weekly during treatment, and at the 8-week treatment termination point by an independent clinical evaluator. The participants were administered the Structured Clinical Interview for DSM-IV (SCID) (41) before random assignment to establish substance use and psychiatric diagnoses. The Substance Abuse Calendar, similar to the Timeline Follow Back (42 , 43) , was administered weekly during treatment to collect detailed day-by-day self-reports of drug and alcohol use throughout the 56-day treatment period as well as for the 28-day period before random assignment.
Participant self-reports of illegal drug use were verified through urine toxicology screens that were obtained at every assessment visit. Of 578 urine specimens collected during the treatment phase of the study (between days 4 and 56), the majority were consistent with participant self-report in that only 58 (10%) were positive for drugs in cases in which the participant had denied recent use during the period the drug’s metabolites are typically detectable in urine (3 days for cocaine and opioids, seven for marijuana). Using these cutoffs, 23 urine samples were submitted that were positive for cocaine when the participant had reported no cocaine use in the past 3 days, 31 were positive for marijuana when the participant had reported no marijuana use in the past 7 days, and nine were positive for opioids when the participant had reported no opioid use in the past 3 days. This rate is consistent with previous studies of substance-dependent samples (43 – 45) . Breathalyzer samples were also collected at each assessment visit; none indicated recent alcohol use.
Data Analyses
The a priori primary outcome measures were the results of urine toxicology screens (operationalized as the number of drug-positive urine samples collected during treatment) and the frequency of substance use (operationalized as the percentage of days in the 56-day treatment period the participant reported using alcohol or any illegal drug). Secondary outcomes included the longest period of abstinence attained during treatment and retention in treatment. The principal data analytic strategy was analysis of variance for the two primary outcome variables for the 77 participants who were randomly assigned to treatment (intention to treat) and the 73 participants who initiated treatment (treatment-exposed). Four participants who were randomly assigned but did not initiate treatment had been assigned to CBT4CBT; of these, three were arrested after random assignment but before the onset of treatment. Results were highly consistent across analysis samples, and therefore, results from the treatment-exposed group are presented below (the four individuals who dropped out immediately after random assignment were not exposed to any protocol treatment, could not be located for any further assessments, and therefore contributed minimally to the data set since no urine or self-report data were available).
Results
Group Description
Table 1 presents baseline demographic characteristics and substance use and psychiatric diagnoses of the 73 participants who initiated treatment. Of these, 43% were women, and 46% identified themselves as African American, 34% as European American, 12% as Hispanic, and 6% as Native American. Most were single or divorced, 77% were unemployed, and 75% had completed high school. Over one-third (37%) of the group reported that they were on probation or parole, and 27% indicated that their application for treatment had been prompted by the criminal justice system.
Most participants (59%) reported cocaine use as their primary substance use problem, followed by alcohol (18%), opioids (16%), and marijuana (7%), with multiple types of concurrent substance use common (79.5% were users of more than one type of drug or users of both alcohol and drugs). The participants reported that they had been using their primary substance for a mean of 17 years and reported using their primary substance for an average of 10 of the past 28 days. Analysis of variance and chi-square analyses indicated no significant differences by treatment condition on any of the variables presented in Table 1 .
Treatment Implementation, Retention, and Data Availability by Condition
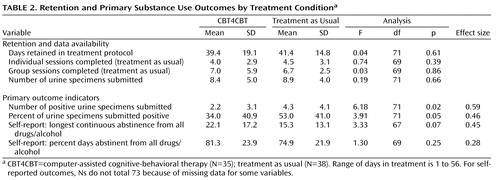
Of the 73 individuals who initiated treatment, 48 (66%) completed the study (22 in CBT4CBT, 26 in treatment as usual: n.s.). As shown in Table 2 , levels of exposure to the standard counseling services offered in the program were also comparable in both groups, with those assigned to CBT4CBT completing a mean of 39 days and those assigned to treatment as usual completing 41 days of the 56-day protocol. Hence, analyses of the primary substance use outcomes were not constrained by differential rates of attrition nor by data availability.
Of those who initiated the CBT4CBT program, the mean number of computer sessions completed was 4.3 (SD=2.4) of the six modules offered. The participants spent an average of 38.3 (SD=8.2) minutes per session working with each module and tended to complete the modules in the order presented (e.g., 34 of 35 participants completed module 1: patterns of use and functional analysis; 25 completed module 2: coping with craving; 20 completed module 3: refusing offers; 19 completed module 4: problem solving; 18 completed module 5: addressing cognitions; and 15 completed module 6: decision making). As noted earlier, homework was assigned at the end of each module; the participants completed an average of 2.9 homework assignments (SD=2.0). Twenty-six participants completed evaluation of the program, in which they were asked to rate their level of agreement with a range of statements about the CBT4CBT program using a Likert-type scale with ratings of 1 indicating low satisfaction and 5 indicating high satisfaction. For the 17 items evaluating various aspects of the program (e.g., “The directions were easy to understand”; “The program helped me think about my problems in a new way”), the mean satisfaction rating was 4.3 (SD=0.6).
Effects of Treatment on Primary Substance Use Outcomes
The participants assigned to CBT4CBT submitted significantly fewer urine specimens that were positive for any type of drug use (2.2 versus 4.3; F=6.18, df=71, p=0.02), with a moderate effect size (d=0.59) and a lower proportion of urines that were positive for any drug (34% versus 53%; F=3.9, df=71, p=0.05; d=0.46). This was most marked for cocaine (28% versus 44% positive specimens). Duration of longest continuous (urine-confirmed) period of abstinence during treatment was longer for those assigned to CBT4CBT than treatment as usual (22 versus 15 days). Although this fell just short of statistical significance, the effect size was moderate (d=0.45). The difference between groups for self-reported percent days of abstinence for all illicit drugs and alcohol was not statistically significant.
CBT4CBT Program Use and Outcome
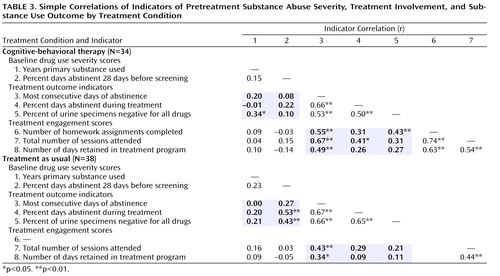
Consistent with previous support for links between pretreatment substance use severity (46) , treatment retention (47) , and outcome, we expected strong relationships between these variables and outcome among participants in this group, but with treatment involvement more closely tied to outcome in the CBT4CBT condition than in treatment as usual. Table 3 presents simple correlations between baseline severity of substance use (frequency of substance use at baseline, years of substance use), treatment involvement (indicated by the number of days retained in the treatment program, the number of individual and group sessions attended, and homework completion), and treatment outcome (percent of drug-negative urine specimens, self-reported days abstinent, and duration of longest consecutive period of abstinence during treatment). In treatment as usual, the indicators of baseline substance use severity tended to have higher correlations with outcome than the treatment-retention indicators, whereas the reverse held for the CBT4CBT condition, in which treatment involvement and completion of homework assignments had higher correlations. The results of structural equation modeling (48) were consistent with this interpretation, with a good-fitting model indicating that treatment involvement (r=0.77, critical ratio=3.5, p<0.001) and completion of homework (r=0.85, critical ratio=4.2, p<0.001) were strongly related to outcome in CBT4CBT.
Discussion
In this randomized clinical trial of the efficacy of a computer-assisted CBT program for reducing drug use, participants using the CBT4CBT program submitted significantly fewer drug-positive urines specimens and tended to have longer periods of abstinence during treatment compared with standard treatment as usual at a community-based clinic. This is, to our knowledge, the first randomized clinical trial evaluating computer-assisted treatment for substance use disorders that reports on biologically verified drug use outcomes. Thus, the study both adds to the existing positive literature on computer-assisted delivery of CBT for depression and anxiety disorders by extending it to a new and highly challenging population and also provides strong evidence for the efficacy of computer-assisted training through use of data from urine toxicology screens rather than self- or therapist reports, both of which may be subject to bias. The CBT4CBT program was viewed by participants as highly engaging, was associated with promising outcomes, and potentially addresses a critical issue related to the availability of CBT in clinical practice.
Similarly, this trial is consistent with multiple trials suggesting that the practice of CBT skills outside of sessions through completion of homework assignments may be an important active ingredient of outcome CBT (34 , 36) in that there was a significant positive relationship between the number of CBT4CBT homework assignments completed and substance use outcomes. That is, indicators of treatment involvement were strongly related to outcome in the CBT4CBT condition, whereas in the treatment as usual condition, outcome was more strongly related to baseline severity of substance use than level of treatment engagement. Given the link between use of the program and outcome, more frequent access to and use of the CBT4CBT program (e.g., through the Internet) should be evaluated as a strategy to enhance the potential benefits of this approach.
Strengths of this trial included random assignment of a comparatively large and diverse group of participants in a community clinic, comparable levels of retention and data availability in both conditions, and reliance on independent, biological indicators of outcome. While not addressed in this study, the high level of control over the delivery of specific modules or treatment components (such as homework) in computer-assisted training may permit more refined study of the specific mediators of CBT through future clinical trials in which these elements are systematically manipulated with greater precision than is typically possible in clinician-delivered therapies.
This study had several limitations as well. First, it should be noted that the study did not address whether computer-assisted delivery of training was comparable or superior to clinician-delivered CBT, nor did it control for the additional time the participants spent working with the computer program in addition to the treatment as usual received. Moreover, use of a treatment-as-usual comparison condition that was not constrained or controlled had the typical disadvantages of this type of comparison (49) , including variability in content and duration. On the other hand, it did constitute an active treatment comparison (50 , 51) and therefore provided a rigorous control for evaluating any added benefit conferred by CBT4CBT. Second, in common with most trials involving substance users, attrition was an issue, as approximately 65% of those who initiated their protocol treatment completed it. On the other hand, data availability was comparable for both conditions, and the retention rates are comparatively high given the unselected nature of the study population. Moreover, our extensive efforts to reach and collect data from those who dropped out of treatment (52) provided complete data for over 80% of the treatment-exposed group for the full 56-day study period. Third, it should be noted that the analyses evaluating the relationships between baseline substance use severity, treatment involvement, and outcome are correlational, and causality cannot be inferred.
Finally, because CBT has been demonstrated to be effective across several substance use disorders, we decided to evaluate CBT4CBT with a heterogeneous group of outpatients who used multiple substances concurrently. Although this provided stronger evidence for the generalizability of the CBT4CBT program, it produced insufficient group sizes for analyzing different subgroups of patients. In this regard, it should also be noted that our significant urine outcomes are complicated by the fact that some substances are detectable in urine for longer periods (marijuana) than others (cocaine). On the other hand, detecting a significant difference under these circumstances and in a heterogeneous community-based group provided comparatively strong support for this promising new model. These results should be replicated before CBT4CBT is advocated for broader use in the substance abuse treatment system, and we are currently conducting a larger trial with a more homogeneous cocaine-dependent methadone-maintained group.
1. DeRubeis RJ, Crits-Christoph P: Empirically supported individual and group psychological treatments for adult mental disorders. J Consult Clin Psychol 1998; 66:37–52Google Scholar
2. Roth A, Fonagy P: What Works for Whom? A Critical Review of the Psychotherapy Literature, 2nd ed. New York, Guilford, 2005Google Scholar
3. Watkins E, Williams R: The efficacy of cognitive-behavioral therapy. Cogn Behav Ther 1998; 8:165–187Google Scholar
4. Irvin JE, Bowers CA, Dunn ME, Wong MC: Efficacy of relapse prevention: a meta-analytic review. J Consult Clin Psychol 1999; 67:563–570Google Scholar
5. Carroll KM, Onken LS: Behavioral therapies for drug abuse. Am J Psychiatry 2005; 162:1452–1460Google Scholar
6. Carroll KM, Rounsaville BJ, Nich C, Gordon LT, Wirtz PW, Gawin FH: One year follow-up of psychotherapy and pharmacotherapy for cocaine dependence: delayed emergence of psychotherapy effects. Arch Gen Psychiatry 1994; 51:989–997Google Scholar
7. Anton RF, O’Malley SS, Ciraulo DA, Cisler RA, Couper D, Donovan DM, Gastfriend DR, Hosking JD, Johnson BA, LoCastro JS, Longabaugh R, Mason BJ, Mattson ME, Miller WR, Pettinati HM, Randall CL, Swift RM, Weiss RD, Williams LD, Zweben A, COMBINE Study Research Group: Combined pharmacotherapies and behavioral interventions for alcohol dependence: the COMBINE study: a randomized controlled trial. JAMA 2006; 295:2003–2017Google Scholar
8. Institute of Medicine: Bridging the Gap Between Practice and Research: Forging Partnerships With Community-Based Drug and Alcohol Treatment. Washington, DC, National Academy Press, 1998Google Scholar
9. Weissman MM, Verdeli H, Gameroff MJ, Bledsoe SE, Betts K, Mufson L, Fitterling H, Wickramaratne P: National survey of psychotherapy training in psychiatry, psychology, and social work. Arch Gen Psychiatry 2006; 63:925–934Google Scholar
10. McLellan AT, Carise D, Kleber HD: Can the national addiction treatment infrastructure support the public’s demand for quality care? J Subst Abuse Treat 2003; 25:117–121Google Scholar
11. McLellan AT, Lewis DC, O’Brien CP, Kleber HD: Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA 2000; 284:1689–1695Google Scholar
12. McLellan AT, Meyers K: Contemporary addiction treatment: a review of systems problems for adults and adolescents. Biol Psychiatry 2004; 56:764–770Google Scholar
13. Sholomskas D, Syracuse G, Ball SA, Nuro KF, Rounsaville BJ, Carroll KM: We don’t train in vain: a dissemination trial of three strategies for training clinicians in cognitive behavioral therapy. J Consult Clin Psychol 2005; 73:106–115Google Scholar
14. Morgenstern J, Morgan TJ, McCrady BS, Keller DS, Carroll KM: Manual-guided cognitive-behavioral therapy training: a promising method for disseminating empirically supported substance abuse treatments to the practice community. Psychol Addict Behav 2001; 15:83–88Google Scholar
15. Martino S, Ball SA, Nich C, Frankforter TL, Carroll KM: Internal validity of MET and MI when delivered by community therapists in multisite effectiveness studies. Drug and Alcohol Dependence (in press)Google Scholar
16. Aharonovich E, Hasin DS, Brooks AC, Liu X, Bisaga A, Nunes EV: Cognitive deficits predict low treatment retention in cocaine dependent patients. Drug Alcohol Depend 2006; 81:313–322Google Scholar
17. Fals-Stewart W, Bates ME: The neuropsychological test performance of drug-abusing patients: an examination of latent cognitive abilities and risk factors. Exp Clin Psychopharmacol 2003; 11:34–45Google Scholar
18. Spek V, Cuijpers P, Nyklicek I, Riper H, Keyzer J, Pop V: Internet-based cognitive-behaviour therapy for symptoms of depression and anxiety: a meta-analysis. Psychol Med 2007; 37:319–328Google Scholar
19. Kenardy JA, Dow MGT, Johnston DW, Newman MG, Thomson A, Taylor CB: A comparison of delivery methods of cognitive-behavioral therapy for panic-disorder: an international multicenter trial. J Consult Clin Psychol 2003; 71:1068–1075Google Scholar
20. Newman MG, Kenardy J, Herman S, Taylor CB: Comparison of palmtop-computer assisted brief cognitive-behavioral treatment to cognitive-behavioral treatment for panic disorder. J Consult Clin Psychol 1997; 65:178–183Google Scholar
21. Proudfoot J, Goldberg D, Mann A, Everitt B, Marks I, Gray JA: Computerized, interactive, multimedia cognitive-behavioral program for anxiety and depression in general practice. Psychol Med 2003; 33:217–227Google Scholar
22. Selmi PM, Klein MH, Greist JH, Sorrell SP, Erdman HP: Computer-administered cognitive-behavioral therapy for depression. Am J Psychiatry 1990; 147:51–56Google Scholar
23. Klein B, Richards JC, Austin DW: Efficacy of Internet therapy for panic disorder. J Behav Ther Exp Psychiatry 2006; 37:213–238Google Scholar
24. Tumur I, Kaltenthaler E, Ferriter M, Beverley C, Parry G: Computerised cognitive behaviour therapy for obsessive-compulsive disorder: a systematic review. Psychother Psychosom 2007; 76:196–202Google Scholar
25. Wright JH, Wright AS, Albano AM, Basco MR, Goldsmith LJ, Raffield T, Otto MW: Computer-assisted cognitive therapy for depression: maintaining efficacy while reducing therapist time. Am J Psychiatry 2005; 162:1158–1164Google Scholar
26. McCrone P, Knapp M, Proudfoot J, Ryden C, Cavanagh K, Shapiro DA, Ilson S, Gray JA, Goldberg D, Mann A, Marks I, Everitt B, Tylee A: Cost-effectiveness of computerized cognitive-behavioral therapy for anxiety and depression in primary care: randomized controlled trial. Br J Psychiatry 2004; 185:55–62Google Scholar
27. Strecher VJ, Shiffman S, West R: Randomized controlled trial of a Web-based computer-tailored smoking cessation program as a supplement to nicotine patch therapy. Addiction 2005; 100:682–688Google Scholar
28. Japuntich SJ, Zehner ME, Smith SS, Jorenby DE, Valdez JA, Fiore MC, Baker TB, Gustafson DH: Smoking cessation via the internet: a randomized clinical trial of an internet Intervention as adjuvant treatment in a smoking cessation intervention. Nicotine Tob Res 2006; 8(suppl 1):S59–S67Google Scholar
29. Glenn IM, Dallery J: Effects of Internet-based voucher reinforcement and a transdermal nicotine patch on cigarette smoking. J Appl Behav Anal 2007; 40:1–13Google Scholar
30. Hester RK, Squires DD, Delaney HD: The Drinker’s Check-up: 12-month outcomes of a controlled clinical trial of a stand-alone software program for problem drinkers. J Subst Abuse Treat 2005; 28:159–169Google Scholar
31. Hester RK, Delaney HD: Behavioral self-control program for Windows: results of a controlled clinical trial. J Consult Clin Psychol 1997; 65:686–693Google Scholar
32. Saitz R, Palfai TP, Freedner N, Winter MR, MacDonald A, Lu J, Ozonoff A, Rosenbloom DL, DeJong W: Screening and brief intervention online for college students: the ihealth study. Alcohol Alcohol 2007; 42:28–36Google Scholar
33. Marsch LA, Bickel WK: Efficacy of computer-based HIV/AIDS education for injection drug users. Am J Health Behav 2004; 28:316–327Google Scholar
34. Carroll KM, Nich C, Ball SA: Practice makes progress: homework assignments and outcome in the treatment of cocaine dependence. J Consult Clin Psychol 2005; 73:749–755Google Scholar
35. Gonzalez VM, Schmitz JM, DeLaume KA: The role of homework in cognitive behavioral therapy for cocaine dependence. J Consult Clin Psychol 2006; 74:633–637Google Scholar
36. Kazantzis N, Deane FP, Ronan KR: Homework assignments in cognitive and behavioral therapy: a meta-analysis. Clin Psychol: Sci Pract 2000; 7:189–202Google Scholar
37. Stout RL, Wirtz PW, Carbonari JP, Del Boca FK: Ensuring balanced distribution of prognostic factors in treatment outcome research. J Stud Alcohol Suppl 1994; 12:70–75Google Scholar
38. Carroll KM: A Cognitive-Behavioral Approach: Treating Cocaine Addiction. Rockville, Md, National Institute on Drug Abuse, 1998Google Scholar
39. Carroll KM, Easton CJ, Nich C, Hunkele KA, Neavins TM, Sinha R, Ford HL, Vitolo SA, Doebrick CA, Rounsaville BJ: The use of contingency management and motivational/skills-building therapy to treat young adults with marijuana dependence. J Consult Clin Psychol 2006; 74:955–966Google Scholar
40. Carroll KM, Fenton LR, Ball SA, Nich C, Frankforter TL, Shi J, Rounsaville BJ: Efficacy of disulfiram and cognitive-behavioral therapy in cocaine-dependent outpatients: a randomized placebo controlled trial. Arch Gen Psychiatry 2004; 64:264–272Google Scholar
41. First MB, Spitzer RL, Gibbon M, Williams JBW: Structured Clinical Interview for DSM-IV, Patient Edition. Washington, DC, American Psychiatric Press, 1995Google Scholar
42. Fals-Stewart W, O’Farrell TJ, Freitas TT, McFarlin SK, Rutigliano P: The Timeline Follow Back reports of psychoactive substance use by drug-abusing patients: psychometric properties. J Consult Clin Psychol 2000; 68:134–144Google Scholar
43. Hersh D, Mulgrew CL, Van Kirk J, Kranzler HR: The validity of self-reported cocaine use in two groups of cocaine abusers. J Consult Clin Psychol 1999; 67:37–42Google Scholar
44. Zanis DA, McLellan AT, Randall M: Can you trust patient self-reports of drug use during treatment? Drug Alcohol Depend 1994; 35:127–132Google Scholar
45. Ehrman RN, Robbins SJ: Reliability and validity of 6-month timeline reports of cocaine and heroin use in a methadone population. J Consult Clin Psychol 1994; 62:843–850Google Scholar
46. McLellan AT, Alterman AI, Metzger DS, Grissom GR, Woody GE, Luborsky L, O’Brien CP: Similarity of outcome predictors across opiate, cocaine, and alcohol treatments: role of treatment services. J Consult Clin Psychol 1994; 62:1141–1158Google Scholar
47. Simpson DD, Joe GW, Broome KM: A national 5-year follow-up of treatment outcomes for cocaine dependence. Arch Gen Psychiatry 2002; 59:538–544Google Scholar
48. Bentler PM, Stein JA: Structural equation models in medical research. Stat Methods Med Res 1992; 1:159–181Google Scholar
49. Bickman L: The death of treatment as usual: an excellent first step on a long road. Clin Psychol: Sci Pract 2002; 9:195–199Google Scholar
50. Kazdin AE: Comparative outcome studies of psychotherapy: methodological issues and strategies. J Consult Clin Psychol 1986; 54:95–105Google Scholar
51. Carroll KM, Rounsaville BJ: Bridging the gap between research and practice in substance abuse treatment: a hybrid model linking efficacy and effectiveness research. Psychiatr Serv 2003; 54:333–339Google Scholar
52. Nich C, Carroll KM: Intention to treat meets missing data: implications of alternate strategies for analyzing clinical trials data. Drug Alcohol Depend 2002; 68:121–130Google Scholar