Does Memory of a Traumatic Event Increase the Risk for Posttraumatic Stress Disorder in Patients With Traumatic Brain Injury? A Prospective Study
Abstract
OBJECTIVE: The present study examined prospectively the relationship between memory of the traumatic event and subsequent development of posttraumatic stress disorder (PTSD). More specifically, the aims of this study were to 1) investigate the possibility that lack of memory of the traumatic event might be a protective factor; 2) assess whether memory of the traumatic event equally affects the three symptom clusters of PTSD: reexperiencing, avoidance, and hyperarousal; and 3) explore the predictive value of memory of the traumatic event for the development of subsequent PTSD in the immediate aftermath of the event. METHOD: One hundred twenty subjects with mild traumatic brain injury who were hospitalized for observation were assessed immediately after the trauma and followed up 1 week, 3 months, and 6 months later. All participants underwent psychiatric evaluation and self-assessment of their memory of the traumatic event. RESULTS: Overall, 17 (14%) of the participants met full criteria for PTSD at 6 months. Subjects with memory of the traumatic event were significantly more likely to develop PTSD than those without memory of the traumatic event; the difference between the groups resulted primarily from the reexperiencing cluster. Logistic regression analysis revealed that memory of the traumatic event within the first 24 hours is a strong predictor of PTSD 6 months after the event. CONCLUSIONS: Our study indicated that memory of a traumatic event is a strong predictor and a potential risk factor for subsequent development of PTSD. Future studies are needed to show whether these findings can be generalized to other traumatic conditions.
The intricate system of memory is commonly thought of as composed of two primary pathways. The first is referred to as explicit, or declarative, memory. This relates to conscious awareness of facts and requires focal attention for processing; it is probably mediated by the medial temporal lobe system that includes the hippocampal formation and related structures that enable verbal representation (1–3). The second pathway, referred to as implicit, or nondeclarative, memory, relates to memories acquired during skill learning, habit formation, and simple, classic conditioning. It also refers to other knowledge expressed through performance rather than recollection. These memories are believed to be less accessible to consciousness (4).
Traumatic memories share both explicit and implicit features and are processed differently than ordinary memories (5). This results in failure to organize the traumatic event into a coherent verbally represented narrative (5, 6). The abnormal nature of the traumatic memories is considered to be a central feature of posttraumatic stress disorder (PTSD). This is manifested by hyperamnestic symptoms, such as reexperiencing, intrusive thoughts, nightmares, and flashbacks on one hand and, at the same time, impaired memory of the traumatic event in the form of amnesia and delayed recall, which is also a well-known phenomenon in traumatized individuals (7). This raises the question as to the extent to which each constitutes a risk factor for PTSD.
In recent years, researchers have focused on traumatic memory and the mechanisms by which it operates to better understand the risk factors associated with it in the development of PTSD. However, empirically based studies are limited by practical and ethical constraints (8) and thus, naturalistic conditions, in which traumatic memories are compromised, may serve as models to study this question. Traumatic brain injury, which is commonly associated with impaired memory, has been used as a naturally occurring model for the investigation of the relationship between memory and PTSD (9–12).
Some of the studies that focused on traumatic brain injury have provided evidence that traumatic events involving traumatic brain injury are associated with reduced prevalence of PTSD, consistent with the view that amnesia of the traumatic event may play a protective role in this regard (13, 14). Other studies, however, have shown that PTSD is fairly prevalent among patients with traumatic brain injury, supporting the view that the traumatic brain injury and PTSD are not mutually exclusive (15, 16).
A significant limitation of these studies, however, is the fact that they did not directly evaluate or control for actual memory of the traumatic event. That is, the degree to which victims of traumatic brain injury, in fact, remember the traumatic event was not assessed. Although it is reasonable to assume that traumatic brain injury impairs memory of the traumatic event (9), there exists a significant variability within patients with traumatic brain injury with regard to the amount and quality of their memory of the traumatic event. It is quite possible that this variability provides an explanation for these conflicting results.
The main purpose of the present study was to overcome this limitation by direct assessment of the relationship between explicit memory of the traumatic event and subsequent development of PTSD in participants who had experienced a traumatic event associated with traumatic brain injury. More specifically, the goals of the present study were to further investigate the assumption that lack of memory of the traumatic event serves as a protective factor against the development of PTSD and to assess whether lack of memory of the traumatic event equally affects all three PTSD symptom clusters, namely, reexperiencing, avoidance, and hyperarousal. Finally, an attempt was made to assess the relative contribution of memory of the traumatic event to the development of PTSD in the context of other risk factors.
Method
Participants
The study population included 120 patients with traumatic brain injury who were recruited from two surgical wards at Rambam Medical Center to which they were admitted for medical care after traumatic brain injury. The participants had to be between the ages of 18 and 50 and be fluent in Hebrew. Excluded were those actively receiving psychiatric care at the time of injury or who had a prior history of head trauma, cognitive deficit, substance abuse, or a major untreated medical condition. After receiving a detailed description of the study, each subject provided written informed consent for participation in the study, which was approved by the institutional review board at Rambam Medical Center.
Of 198 eligible subjects, 44 (23%) refused to participate and 34 (17%) dropped out during follow-up. Thus, the final cohort consisted of 120 subjects who completed the entire follow-up. These were relatively young subjects (mean age=31.4 years, SD=2.7), with an average education of high school (mean=12.6 years, SD=2.5). The participants were predominantly men (58%), married (50%) or single (50%), Israeli-born (68%), without a prior history of physical (80%) or psychiatric (59%) disorders, who were injured primarily in traffic accidents (90%), with a mean injury severity score of 5.8 (SD=3.6), indicating mild physical injury. None of the participants was unconscious at the time of the admission, and their scores on the Glasgow Coma Scale (17) were in the upper range (score=13–15), which excludes loss of consciousness.
Procedure and Measures
The initial evaluation took place within the first 24 hours after the injury, during hospitalization. The participants were then invited for further evaluation after 7 to 10 days, 4 weeks, and 6 months from the traumatic event.
At the first interview, the participants were asked to provide information regarding their personal background and self-assessment of their memory of trauma. In addition, the severity of physical injury was assessed with the injury severity score, which is the sum of the Abbreviated Injury Scale (10), rated by a trained physician. Acute dissociative symptoms were measured with the Peritraumatic Dissociation Questionnaire (11).
Memory of the traumatic event was evaluated with a nine-item self-report questionnaire, which was specifically developed for the present study since no such tool was available during the time of the study. The questionnaire assesses the participants’ memory of the traumatic event regarding the following aspects of the trauma: 1) what was the event; 2) where did the event take place; 3) who (other than you) was involved in the event; 4) when did the event occur; 5) sights from the event; 6) sounds from the event; 7) odors from the event; 8) things you said during or after the event; and 9) things other people said during or after the event. Each of the nine items is rated on a 4-point Likert scale, ranging from 1 (no memory) to 4 (good memory), and a total score is derived by calculating a mean score for the memory of the nine traumatic event questions. The questionnaire, which was administered at all four time points, was found to be reliable, with a Cronbach’s alpha of 0.91. In follow-up assessments, the respondents were instructed to complete the Memory of Traumatic Event Questionnaire with an attempt to disregard their previous responses.
PTSD symptoms were assessed with two instruments: the Clinician-Administered PTSD Scale (12) and the Posttraumatic Stress Scale (18). The Clinician-Administered PTSD Scale is a 17-item questionnaire administered by a trained clinician to assess levels of posttraumatic symptoms during the previous 2 weeks. The severity of each item is rated on a 5-point Likert scale ranging from 0 (not at all) to 4 (very much). The total severity score, ranging from 0 to 68, is calculated as the mean of participants’ ratings on the 17 items.
The Posttraumatic Stress Scale is a 17-item self-report questionnaire assessing levels of posttraumatic symptoms levels during the previous 2 weeks. The severity of each item is rated on a 4-point Likert scale ranging from 0 (not at all) to 3 (very much). The total severity score, ranging from 0 to 51, is calculated as the mean of participants’ ratings on the 17 items.
In addition, three subscales were calculated corresponding to the definition of the diagnosis of PTSD: reexperiencing (items 1–5), avoidance (items 6–12), hyperarousal (items 13–17) (on both the Clinician-Administered PTSD Scale and the Posttraumatic Stress Scale). Pearson’s correlation analysis showed that the total score of each scale is highly correlated with its subscales (Clinician-Administered PTSD Scale: reexperiencing: r=0.89, avoidance: r=0.81, hyperarousal: r=0.88; Posttraumatic Stress Scale—reexperiencing: r=0.88, avoidance: r=0.82, hyperarousal: r=0.80).
Depression and anxiety symptoms were assessed with the Beck Depression Inventory (19) and the Beck Anxiety Inventory (20), respectively. All ratings were carried out at 7 to 10 days, 4 weeks, and 6 months.
In order to determine lifetime and current diagnoses of any DSM-IV axis I disorder (major psychiatric disorder), the Structured Clinical Interview for DSM-IV, Nonpatient Edition (21), was administered at 1 week and 6 months, respectively. The interview was carried out by an experienced and specially trained clinical social worker.
To detect general cognitive deficits that might have resulted from traumatic brain injury but were unrelated specifically to the memory of the traumatic event, the Automated Neuropsychological Assessment Metrics (22) was administered at the end of the study. The Automated Neuropsychological Assessment Metrics includes a battery of standardized tests designed for clinical use, from which a representative subset of the following six tests was chosen for the present study: 1) the Stanford Sleepiness Scale, 2) the Simple Reaction Time, 3) the Memory Search, 4) the Code Substitution, 5) the Matching to Sample, and 6) the Running Memory Continuous Performance Test.
Data Analysis
First, the distribution of PTSD and the memory of the traumatic event were each calculated separately at the different time points. The relationship between PTSD and the memory of the traumatic event was then assessed on both categorical and ordinal levels by using chi-square analysis (with Yates’s correction) and multivariate repeated-measures analysis of variance (MANOVA), respectively.
In order to explore the differential effect of memory of the traumatic event on the three PTSD symptom clusters, an additional MANOVA with repeated measures was performed by using memory of the traumatic event as an independent variable and the three PTSD symptom clusters (i.e., reexperiencing, avoidance, hyperarousal) as dependent variables.
Automated Neuropsychological Assessment Metrics results were analyzed with two-tailed Student’s t tests, comparing subjects with and without PTSD and those with and without memory of the traumatic event.
Finally, a logistic regression analysis was performed, with PTSD status at 6 months as the dependent variable. Only the variables that showed a significant association with PTSD in previous analyses were used as independent variables in the regression model.
Results
Prevalence and Longitudinal Course of PTSD
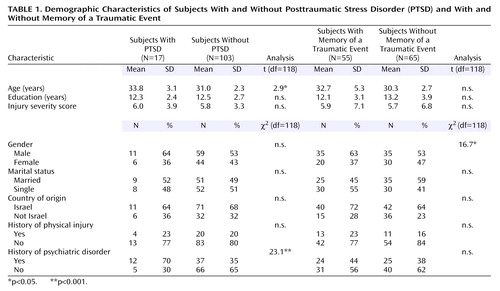
Six months after the traumatic event, 14% (17 of 120) of the participants met diagnostic criteria for PTSD and 10% (12 of 120) met diagnostic criteria for psychiatric disorder other than PTSD. Table 1 presents the demographic characteristics of the PTSD and the non-PTSD groups and shows that they were similar on all parameters except age (t=2.9, df=118, p<0.05), which was found to be higher in the PTSD group. Figure 1 presents the longitudinal course of posttraumatic symptoms in the two groups, as measured by the Clinician-Administered PTSD Scale and the Posttraumatic Stress Scale. Since the Clinician-Administered PTSD Scale and the Posttraumatic Stress Scale are correlated, it would have been possible to analyze them jointly. However, because most studies employ only one of these instruments, separate analyses enable comparisons across the different study groups. In addition, results from a joint MANOVA showed similar results to those reported. Visual inspection of Figure 1 reveals that an initial, relatively small difference between the groups appears to have increased progressively over the 6-month follow-up period. In line with this impression, MANOVAs with repeated measures showed a significant group-by-time interaction for the total score of the Clinician-Administered PTSD Scale (Wilks’s lambda: F=5.1, df=4, 69, p<0.001) and the Posttraumatic Stress Scale (Wilks’s lambda: F=4.7, df=4, 69, p<0.001). The main contribution to the overall interaction effect of PTSD on the Clinician-Administered PTSD Scale and on the Posttraumatic Stress Scale came from the second time interval, namely, the period from 1 week to 1 month (Clinician-Administered PTSD Scale: F(time)=5.1, df=1, 118, p<0.001, and the Posttraumatic Stress Scale: F(time)=4.1, df=1, 118, p<0.001). Duncan’s post hoc test revealed that the differences between the PTSD and the non-PTSD groups on both scales were significant at 1 month (Clinician-Administered PTSD Scale: F=3.1, df=1, 118, p<0.01, and the Posttraumatic Stress Scale: F=3.0, df=1, 118, p<0.01) and at 6 months (Clinician-Administered PTSD Scale: F=3.9, df=1, 118, p<0.001, and the Posttraumatic Stress Scale: F=3.4, df=1, 118, p<0.001) but not at 1 week.
Memory of the Traumatic Event
Figure 2 presents the distribution of respondents on the Memory of Traumatic Event Questionnaire at the initial interview, namely, 24 hours after the injury. As shown, a bimodal distribution is evident, with most participants reporting either good memory of the traumatic event or total lack of memory of the traumatic event. Consequently, a categorical approach was taken, with participants divided into two groups with the median (2.1) of the ordinal scale used as the cutoff point. Thus, the subjects were referred to as either “having memory of the traumatic event” or “having no memory of the traumatic event.” Accordingly, 55 participants (45%) had memory of the traumatic event and 65 (55%) had no memory of the traumatic event.
As shown in Table 1, the demographic characteristics of the participants with and without memory of the traumatic event were found to be comparable on all measures except gender (χ2=16.7, df=118, p<0.001).
Intraclass correlations showed stability of memory of the traumatic event over time, with a strong correlation between the scores on the questionnaire at the different time points (F=3.95, df=1, 118, p<0.001; alpha=0.76).
Relationship Between Memory of Traumatic Event and PTSD
Examination of the relationship between memory of the traumatic event and PTSD at 6 months revealed that PTSD was significantly more prevalent among participants with memory of the traumatic event than among those without memory of the traumatic event (χ2=20.1, df=118, p<0.001). Among the 55 participants with memory of the traumatic event, 13 (23%) had PTSD, whereas only four (6%) of the 65 participants without memory of the traumatic event developed PTSD. Thus, the crude relative risk for PTSD among the participants with memory of the traumatic event was almost five times higher than among those without memory of the traumatic event (odds ratio=4.6, confidence interval [CI]=1.1–9.9, p<0.001).
MANOVAs with repeated measures indicated that the association between memory of the traumatic event and PTSD remained stable over 6 months, as shown by significant effects on PTSD symptoms of both memory of the traumatic event (Clinician-Administered PTSD Scale: F=4.7, df=1, 118, p<0.001, and Posttraumatic Stress Scale: F=4.9, df=1, 118, p<0.001) and time (Clinician-Administered PTSD Scale: F=4.9, df=1, 118, p<0.001, and Posttraumatic Stress Scale: F=4.6, df=1, 118, p<0.001). No group-by-time interaction was found; namely, both the Clinician-Administered PTSD Scale and Posttraumatic Stress Scale scores were significantly higher among the participants with memory of the traumatic event than among those without memory of the traumatic event at all time points.
Next we assessed the differential effect of memory of the traumatic event on each of the three PTSD clusters (reexperiencing, avoidance, and hyperarousal) using MANOVAs with repeated measures. This analysis revealed that the difference between the groups was primarily due to the reexperiencing symptom cluster for both the Clinician-Administered PTSD Scale and the Posttraumatic Stress Scale (F≥3.4, df=1, 118, p<0.01). No significant differences were found on the avoidance and hyperarousal symptom clusters.
Analysis of the cognitive performance tests (Automated Neuropsychological Assessment Metrics) showed that no significant differences were evident between participants with and without memory of the traumatic event or between participants with and without PTSD on any of the measures.
Logistic Regression Analysis
In the final stage, a logistic regression analysis was performed, with PTSD status at 6 months as the dependent variable. The independent variables included in this model were only those that had shown significant associations with PTSD in previous analyses: memory of the traumatic event (within 24 hours after the event), dissociative reaction (within 24 hours after the event), acute PTSD symptoms (within 1 week after the event on both the Clinician-Administered PTSD Scale and the Posttraumatic Stress Scale), depressive symptoms (within 1 week after the event), anxiety symptoms (within 1 week after the event), age, history of psychiatric disorder, and gender.
The results indicated that accounting for all of these correlates and memory of the traumatic event was strongly associated with PTSD at 6 months. Thus, respondents with memory of the traumatic event were more than twice as likely to have PTSD compared with those without memory of the traumatic event (odds ratio=2.2, CI=1.0–10.1). In addition, acute posttraumatic symptoms (Clinician-Administered PTSD Scale: odds ratio=5.3, CI=1.1–9.3, and Posttraumatic Stress Scale: odds ratio=5.2, CI=1.0–9.4), depressive symptoms (odds ratio=5.1, CI=1.0–9.2), anxiety symptoms (odds ratio=4.9, CI=1.0–9.1) within 1 week of the traumatic event as well as a history of psychiatric disorder (odds ratio=3.7, CI=1.1–8.9) were all associated with an increased risk for PTSD at 6 months. The overall model explained 38% of the variance (Nagelkerke R2=38, p<0.001).
Discussion
The main goal of the present study was to assess the relationship between memory of the traumatic event and the subsequent development of PTSD in subjects with traumatic brain injury with a prospective design.
The central finding of our study is that memory of a traumatic event is positively associated with the risk for development of PTSD, while lack of memory of a traumatic event decreases the risk and might, in fact, play a protective role. Thus, along with other factors, such as history of previous trauma (23), previous psychiatric morbidity (23, 24), and physical injury (24, 25), memory of a traumatic event appears to be another risk factor for PTSD. Moreover, memory of a traumatic event assessed as early as 24 hours posttrauma appears to be a strong predictor of PTSD at 6 months.
A closer examination of the specific effect of memory of a traumatic event on the three PTSD symptom clusters reveals that it affects mainly the reexperiencing symptom cluster while the avoidance and hyperarousal clusters did not differ between those with and without memory of a traumatic event. This differential effect is not surprising given the role of memory in the reexperiencing symptom cluster. Nevertheless, this finding is different from our previous results in studies with injured survivors of motor vehicle accidents (24) and with combat survivors (25) in which bodily injury, another risk factor for PTSD, affects all three PTSD symptoms similarly. This difference might suggest that PTSD is not a homogeneous entity but rather a multidimensional and complex disorder.
Our findings further highlight the predictive value of memory of the traumatic event. Given the stability of memory of the traumatic event over the first 6 months after the trauma, memory of the traumatic event reported within 24 hours after the event appears to be a strong predictor of the presence of PTSD 6 months later. Thus, by merely asking traumatic brain injury survivors immediately within the first 24 hours after the event whether they remember its details may identify those who are at risk for the development of PTSD and thus in need of therapeutic intervention.
These findings seem to be in contrast with the theoretical assumptions underlying many of the therapeutic interventions with patients suffering from PTSD (e.g., exposure, abreaction, hypnosis) that highlight the importance of eliciting traumatic memories as part of the recovery process (26). Our findings indicate that at least for traumatic brain injury survivors without memory of the traumatic event, forgetting may be protective, in which case the process of deliberate recollection and remembering may be harmful rather than therapeutic.
It is noteworthy, however, that 6% of the participants in this study without memory of the traumatic event did meet full diagnostic criteria for PTSD at 6 months, indicating that PTSD can develop in the absence of memory of the traumatic event. One possible mechanism by which these results could be explained is that emotionally charged traumatic memories are initially processed with brain circuits that bypass cortical structures and are mediated primarily through the amygdala, resulting in the formation of implicit (unconscious) memories (27–29). In addition, the stress-induced secretion of glucocorticosteroids, which have been shown to impair hippocampal functioning, may disrupt the formation of explicit memory (30).
The generalizability of these findings beyond traumatic brain injury to other conditions, which are associated with impaired or reduced memory of the traumatic event, is at this point speculative and needs to be addressed cautiously. However, in a study of Holocaust survivors (31), it was shown that decrease in dream recall serves as a defensive adaptive function. Taking this even further, with all due caution, one might question whether “deliberate” disruption of memory of the traumatic event might prove therapeutically beneficial. This possibility was recently addressed in a double-blind study that examined the severity of acute PTSD symptoms among 18 subjects who were given 40 mg of propranolol 6 hours after trauma in comparison with the severity of symptoms among 23 participants who received placebo (32). Results showed that participants in the experimental group tended to exhibit lower levels of PTSD symptoms 10 days after the traumatic event. If further corroborated, these findings may support the notion that not only does lack of memory of the traumatic event protect against the development of PTSD but also the pharmacologically induced disruption of the consolidation of traumatic memories can be therapeutically beneficial for trauma survivors.
Several limitations of our study deserve attention. First, participants in this study were asked only to rate the degree to which they believe they did or did not remember certain aspects of the trauma. Thus, our instrument did not actually assess memory of the traumatic event but, rather, one’s confidence in the memory for details of the trauma. This distinction is important because our findings cannot rule out the possibility that false memory of the traumatic event can also increase the risk for PTSD or, alternatively, that just lack of confidence in one’s own memory can also serve as a protective factor against PTSD. Nevertheless, the finding that appraisal of memory of the traumatic event, regardless of its objective accuracy, appears to be a strong predictor of subsequent PTSD, is potentially important, and has both theoretical and clinical implications. A Traumatic Memory Inventory (8), which was not available at the time of our study, may prove helpful in further clarifying this in future studies. Second, we asked our participants only about their memory of the traumatic event but not of other nontraumatic events in their lives. Thus, it is impossible to determine whether memory of the traumatic event as a risk factor is specifically related to the trauma or, alternatively, is part of a more generalized pretraumatic vulnerability factor that relates to one’s autobiographical memory in general. Third, the instrument used for the evaluation of memory of the traumatic event does not cover the entire spectrum of the traumatic memory. Thus, participants may reexperience aspects of the trauma that are not captured by the instrument. Finally, it has often been suggested that PTSD patients are oversensitive to the adversity of the trauma and tend to overstate its etiological role in their psychopathology (7). Therefore, it could be argued that the retrospective appraisal of memory of the traumatic event might also be exaggerated. However, our findings indicate increased PTSD symptoms as early as 1 week after the trauma in respondents with memory of the traumatic event as well as the stability of memory of the traumatic event over time. Taken together, this makes it less likely that the findings of the current study are an artifact of retrospective exaggeration. Direct assessment with control for the degree to which it is important for the patient to remember the traumatic event may assist in clarifying this issue in future studies.
In conclusion, the results of our study indicate that in subjects with traumatic brain injury, memory of the traumatic event seems to be an important risk factor and predictor for subsequent PTSD. Future studies are needed to determine whether these findings are applicable to other traumatic conditions and whether interruption of the consolidation and the extinction of traumatic memories may be therapeutically beneficial.
 |
Received June 26, 2003; revision received April 28, 2004; accepted June 22, 2004. From the Department of Psychiatry, Rambam Medical Center, and Rappaport Faculty of Medicine, Technion Israel Institute of Technology, Haifa, Israel; the Faculty of Social Welfare and Health Studies, School of Social Work, and the Department of Psychology, University of Haifa, Israel. Address correspondence and reprint requests to Dr. Klein, Department of Psychiatry, Rambam Medical Center, P.O. Box 9602, Haifa 31096, Israel; [email protected] (e-mail).
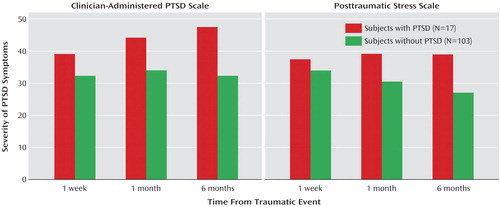
Figure 1. Severity of Posttraumatic Stress Disorder (PTSD) Symptoms Over 6 Months in Subjects With and Without Posttraumatic Stress Disorder
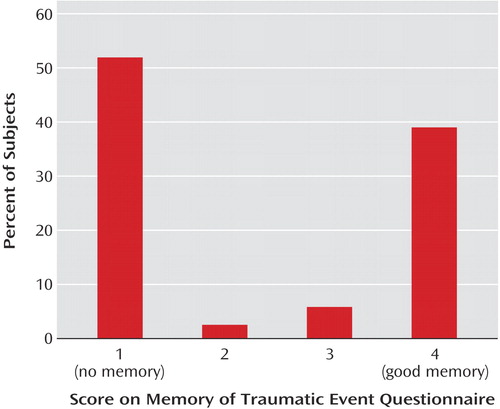
Figure 2. Distribution of 120 Subjects With and Without Posttraumatic Stress Disorder on the Memory of Traumatic Event Questionnairea
aThe questionnaire was developed for the study and assesses memory of a traumatic event regarding the following aspects of the trauma: 1) what was the event; 2) where did the event take place; 3) who (other than you) was involved in the event; 4) when did the event occur; 5) sights from the event; 6) sounds from the event; 7) odors from the event; 8) things you said during or after the event; and 9) things other people said during or after the event.
1. Squire L, Zola-Morgan S, Cave C: Memory: organization of brain systems and cognition. Cold Spring Harbor Symposia on Quantitative Biology 1990; 55:1007–1023Crossref, Medline, Google Scholar
2. Squire L: Declarative and non-declarative memory: multiple brain systems supporting learning and memory. J Cogn Neurosci 1992; 4:232–243Crossref, Medline, Google Scholar
3. Parkin A: Human memory. Curr Biol 1999; 9:582–585Crossref, Google Scholar
4. Siegel D: Memory, trauma, and psychotherapy. J Psychother Pract Res 1995; 4:93–120Google Scholar
5. Brewin CR: A cognitive neuroscience account of posttraumatic stress disorder and its treatment. Behav Res Ther 2001; 39:373–393Crossref, Medline, Google Scholar
6. Hopper JW, van der Kolk BA: Retrieving, assessing, and classifying traumatic memories: a preliminary report on three case studies of a new standardized method. J Aggression, Maltreatment & Trauma 2001; 4:33–71Crossref, Google Scholar
7. van der Kolk B: Trauma and memory in traumatic stress, in The Effects of Overwhelming Experience on Mind, Body, and Society. Edited by van der Kolk B, McFarlane A, Weisaeth L. New York, Guilford, 1996, pp 279–302Google Scholar
8. van der Kolk BA, Hopper JW, Osterman JE: Exploring the nature of traumatic memory: combining clinical knowledge with laboratory models, in Trauma and Cognitive Science: A Meeting of Minds, Science, and Human Experience. Edited by Freyd JJ, DePrince AP. Binghamton, NY, Haworth Press, 2001, pp 9–32Google Scholar
9. Bryant RA: Posttraumatic stress disorder and mild brain injury: controversies, causes and consequences. J Clin Exp Neuropsychol 2001; 23:718–728Crossref, Medline, Google Scholar
10. Association for the Advancement of Automotive Medicine: AIS: The Abbreviated Injury Scale, 1990 Revision. Des Plaines, Ill, AAAM, 1990Google Scholar
11. Marmar CR, Weiss DS, Schlenger WE, Fairbank JA, Jordan BK, Kulka RA, Hough RL: Peritraumatic dissociation and posttraumatic stress in male Vietnam theater veterans. Am J Psychiatry 1994; 151:902–907Link, Google Scholar
12. Blake D, Weathers F, Nagy L, Kaloupek D, Klauminzer G, Charney D, Keane T: Clinician-Administered PTSD Scale (CAPS), Form 1: Current and Lifetime Diagnosis Version. West Haven, Conn, National Center for Posttraumatic Stress Disorder, 1990Google Scholar
13. Mayou R, Bryant B, Duthie ER: Psychiatric consequences of road traffic accident. Br Med J 1993; 307:647–651Crossref, Medline, Google Scholar
14. Sbordone RJ, Liter JC: Mild traumatic brain injury does not produce post traumatic stress disorder. Brain Inj 1995; 9:405–412Crossref, Medline, Google Scholar
15. Bryant RA, Harvey AG: Relationship between acute stress disorder and posttraumatic stress disorder following mild traumatic brain injury. Am J Psychiatry 1998; 155:625–629Link, Google Scholar
16. Ohry A, Rattok J, Solomon Z: Post-traumatic stress disorder in brain injury patients. Brain Injury 1996; 10:687–695Crossref, Medline, Google Scholar
17. Teasdale G, Jennett B: Assessment of coma and impaired consciousness: a practical scale. Lancet 1974; 2:81–84Crossref, Medline, Google Scholar
18. Foa EB, Riggs DS, Dancu CV, Rothbaum BO: Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. J Trauma Stress 1993; 6:459–473Crossref, Google Scholar
19. Beck AT, Steer RA: Manual for the Revised Beck Depression Inventory. San Antonio, Tex, Psychological Corp, 1987Google Scholar
20. Beck AT, Steer RA: Manual for the Beck Anxiety Inventory. San Antonio, Tex, Psychological Corp, 1988Google Scholar
21. First MB, Spitzer RL, Gibbon M, Williams JBW: Structured Clinical Interview for DSM-IV Axis I Disorders—Non-Patient Edition (SCID-I/NP), version 2.0. New York, New York State Psychiatric Institute, Biometrics Research, 1997Google Scholar
22. Reeves D, Kane R, Winter K: Automated Neuropsychological Assessment Metrics (ANAM): Special Report NCRF-SR-96–01. San Diego, National Cognitive Recovery Foundation, 1996Google Scholar
23. Ballenger JC, Davidson JR, Jonathan RT: Consensus statement on posttraumatic stress disorder form international consensus group on depression and anxiety. J Clin Psychiatry 2000; 61:60–66Medline, Google Scholar
24. Koren D, Arnon I, Klein E: Acute stress response and posttraumatic stress disorder in traffic accident victims: a one-year prospective, follow-up study. Am J Psychiatry 1999; 156:367–373Abstract, Google Scholar
25. Koren K, Norman D, Cohen A, Berman J, Klein EM: Increased PTSD risk with combat-related injury: a matched comparison study of injured and uninjured soldiers experiencing the same combat events. Am J Psychiatry 2005; 162:276–282Link, Google Scholar
26. Foa ED, Davidson JRT, Frances A, Culpepper L, Ross R, Ross D: The expert consensus guidelines series: treatment of posttraumatic stress disorder. J Clin Psychiatry 1999; 60(suppl 16): 5–76Google Scholar
27. Ledoux JE, Cicchetti P, Xagoraris A, Romanski L: The lateral amygdaloid nucleus: sensory interface of the amygdala in fear conditioning. J Neurosci 1990; 10:1062–1069Crossref, Medline, Google Scholar
28. LeDoux JE: Emotion, memory and the brain. Sci Am 1994; 270:50–57Crossref, Medline, Google Scholar
29. LeDoux JE: Fear and the brain: where have we been, and where are we going? Biol Psychiatry 1998; 44:1229–1238Crossref, Medline, Google Scholar
30. Sapolsky RM, Uno H, Rebert CS, Finch CE: Hippocampal damage associated with prolonged glucocorticoid exposure in primates. J Neurosci 1990; 10:2897–2902Crossref, Medline, Google Scholar
31. Lavie P, Kaminer H: Sleep, dreaming, and coping style in Holocaust survivors, in Trauma and Dreams. Edited by Barrett D. Cambridge, Mass, Harvard University Press, 2001, pp 114–124Google Scholar
32. Pitman RK, Sanders KM, Zusman RM: Pilot study of secondary prevention of posttraumatic stress disorder with propranolol. Biol Psychiatry 2002; 51:189–192Crossref, Medline, Google Scholar



