Increased PTSD Risk With Combat-Related Injury: A Matched Comparison Study of Injured and Uninjured Soldiers Experiencing the Same Combat Events
Abstract
OBJECTIVE: The aim of the present study was to isolate the unique contribution of physical injury to the subsequent development of posttraumatic stress disorder (PTSD). METHOD: Participants were 60 injured soldiers and a comparison group of 40 soldiers (matched by rank, military role, and length of service) who took part in the same combat situations but were not injured. Current and lifetime diagnoses were determined by using the Structured Clinical Interview for DSM-IV. In addition, an extensive battery of self-report questionnaires was given to assess severity of PTSD, anxiety, depression, and dissociative symptoms. The average time that elapsed between the injury and the interview was 15.5 months (SD=7.3). RESULTS: Ten (16.7%) of the 60 injured survivors but only one (2.5%) of the 40 comparison soldiers met diagnostic criteria for PTSD at the time of the interview (odds ratio=8.6, 95% confidence interval=1.1–394.3). Moreover, wounded participants had significantly higher scores than their noninjured counterparts on all clinical measures. Finally, presence of PTSD was not related to severity of injury or severity of the trauma. CONCLUSIONS: The findings clearly indicate that bodily injury is a major risk factor—rather than a protective one—for PTSD. While supporting the notion that bodily injury contributes to the appraisal of the traumatic event as more dangerous, the data also suggest that this heightened level of perceived threat is not a simple, straightforward function of the severity of injury or of the traumatic event.
The past two decades have witnessed growing attention to the interplay between physical and psychological injuries, i.e., to the psychological consequences of physical injury caused by a traumatic event (1). Traditional views, particularly psychoanalytic ones, tended to regard bodily injury as a protective factor against the development of posttraumatic stress disorder (PTSD) (2). At the basis of this belief was the assumption that physical injury absorbs much of one’s “free-floating psychic energy,” thus reducing the chance of developing anxious or conflicting feelings about the traumatic event. In addition, unlike psychological wounds, bodily injuries typically engender more sympathy from the environment. And finally, a physical wound often removes the source of anxiety by providing an escape from the stressful situation, especially in combat conditions. In support of this view, Merbaum and Hefez (3) found that wounded soldiers (representing the full range of injury severity) showed minimal, if any, psychological disturbances.
However, over the past two decades numerous studies of injured trauma survivors have challenged these traditional understandings of the relationship between PTSD and injury. First, studies in wounded Vietnam veterans have found two- to threefold higher rates of PTSD among this population than among those who returned unharmed (4, 5). Second, multiple studies have found moderate to high rates of PTSD among injured survivors of other types of traumatic events, such as traffic accidents (6–9), terrorism (10), criminal assault (11), and burn injuries (12). The prevalence rates of PTSD in these samples varied from 11% to 40% (8, 9, 12). Similar rates of PTSD have also been observed in mildly injured brain trauma survivors (13). Finally, while a few studies have shown that risk for PTSD is associated with severity of injury (14), other studies have failed to replicate these results (5, 15).
Thus, despite the marked variability in the reported rates of PTSD among injured populations, the rapidly growing literature on this topic suggests that traumatic injury not only does not reduce the risk for PTSD, as believed by traditional psychoanalytic views, but may even increase it. Yet, while considerably contributing to our understanding of the risk-elevating nature of injury with regard to PTSD, the increasing body of literature reveals relatively little about the unique contribution of bodily injury, over and above that of the trauma itself, to the subsequent development of PTSD. The reason is that no study directly compared, in a matched, case-control design, injured and noninjured survivors of the same trauma.
The aim of the present study was to estimate the unique contribution of physical injury, over and above that of the trauma itself, to the subsequent development of PTSD. More specifically, our goals were to 1) replicate previous findings regarding higher than average rates of PTSD in injured survivors of combative actions and 2) evaluate the relationship of PTSD symptoms with both the nature and severity aspects of the injury. To accomplish these goals, we employed an event-based, matched design in a group of injured and noninjured soldiers who experienced the same traumatic combat event.
Method
Participants
Participants in this study were 60 injured soldiers and a matched comparison group of 40 noninjured soldiers. The sampling frame for injured cases in this study was a list of 176 soldiers admitted to the emergency trauma units of three major hospitals in the northern part of Israel between 1998 and 2000 for medical care of combat-induced injuries. Inclusion criteria were a minimum hospitalization length of 2 days and the ability to communicate fluently in Hebrew. Exclusion criteria were severe head injury or evidence of brain damage or active treatment for a psychiatric disorder at the time of the injury. On the basis of these criteria, 172 soldiers were listed as suitable candidates for the study. An attempt to contact these 172 candidates was made first with a letter informing them about the study and then with a telephone call from one of the four interviewers to invite them to participate and schedule an interview. Using this method, we were able to reach and establish contact with 117 (68.0%) injured soldiers (the main reasons for failure to establish contact were change in address and telephone numbers). Of these, 76 (65.0%) agreed to participate in the study. However, 16 (21.1%) of these 76 potential participants could not keep their scheduled appointment, leaving 60 injured soldiers, which represents a total response rate of 51.3%. The average time that elapsed between the injury and the interview was 15.5 months (SD=7.3). All participants gave written informed consent to the study, which had been approved by the Helsinki committees of both the Rambam Medical Center and the Medicine Corps of the Israel Defense Forces. Participants were paid $25 for their time, and their travel expenses were reimbursed.
The sampling frame for the comparison group were soldiers who took part in the same combat situation but were not injured. Selection of participants for this group was done on a one-by-one basis, guided by the following matching criteria: 1) ethnic origin (Ashkenazi/non-Ashkenazi Jews), 2) socioeconomic status, 3) rank, 4) length of service, 5) role in the unit, and 6) preinjury medical profile. The medical profile is a global score used by the Israel Defense Forces to characterize one’s overall health status (both physically and mentally). Medical profile scores are assigned by a medical panel appointed by the Surgeon General of the Israel Defense Forces and range from a low of 21 to a high of 97. Assignment to frontline (profile >64) versus rearline (31 <profile <65) units is determined by this medical profile score, whereas a score of 24 or below means unfit for service. A previous study by Benbenishty (16) provides further explanation of this scale.
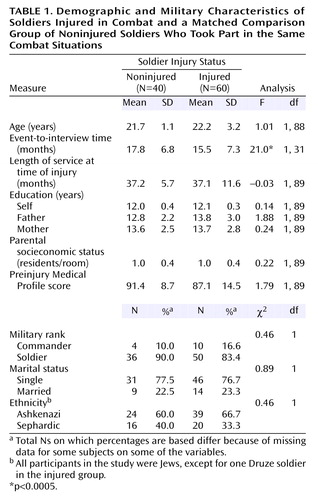
The matching procedure yielded 32 event-based injured-noninjured groupings (27 injured cases were each matched with one noninjured comparison subject, four were matched with two comparison subjects, and one injured soldier was matched with four noninjured comparison subjects). Altogether, 40 noninjured comparison subjects were recruited for the matching process. Table 1 presents other basic sociodemographic and military characteristics of the two groups. As can be seen, the two groups were well matched on these criteria. The only exception was event-to-interview time, which because of our sampling procedure (i.e., injured cases first, then selection of matched comparison subjects) was slightly longer in the noninjured group (mean=17.8, SD=6.8).
Procedure and Measures
Suitable candidates who agreed to participate were invited for a one-time interview meeting with a master’s-level student in clinical psychology at the Rambam Medical Center (Haifa, Israel), or, in cases where the participant could not get to the hospital, at the participant’s home. Following a complete description of the study at the start of the interview, written informed consent was obtained. The participants were then asked to answer questions regarding their personal background (e.g., family status, country of origin, level of education). After background information was acquired, details of the incident, including feelings, thoughts, duration, time of day, casualty, evacuation time, etc., were elicited from the participants. In addition, an extensive battery of self-report questionnaires was given covering areas such as PTSD, general psychopathology, level of dissociative experiences, and trauma history.
The psychiatric evaluation included lifetime and current DSM-IV axis I diagnoses determined with the Hebrew translation of the Structured Clinical Interview for Axis I DSM-IV Disorders (SCID) (17). Symptoms of PTSD were evaluated with the Clinician-Administered PTSD Scale (18), a 17-item structured interview that assesses symptom frequency and symptom intensity on a 5-point Likert scale and produces an overall PTSD score that ranges from 0 to 136 and is the sum of the two scores. Symptoms of depression and anxiety were evaluated by the Beck Depression Inventory (19) and the Beck Anxiety Inventory (20), respectively.
Dissociative reactions during the incident were assessed by using the Peritraumatic Dissociative Experiences Questionnaire (21), which is a self-report measure designed to evaluate retrospectively the level of depersonalization, derealization, and amnesia of each participant.
Severity of physical injury was assessed by the Injury Severity Score, a physician-rated score based on the Abbreviated Injury Scale (22), a tool for the assessment of physical injury according to body regions (head/neck, face, chest, abdomen, extremities, external). As defined in the manual, the Injury Severity Score is calculated as the sum of squares of the highest Abbreviated Injury Scale score on an ordinal severity scale ranging from 1 (minor) to 6 (currently untreatable).
Data Analysis
Because of the matching procedure, a set of one-factor tests (SAS: Proc Mixed [23]) for correlated continuous variables and logistic regressions for correlated binary data (SAS: Proc GENMOD [23]) were used to compare the demographic and trauma-related characteristics of the two groups. The association between injury and formal diagnosis of PTSD was tested using an exact logistic regression for stratified data (SAS: Proc Logistic [23]). This procedure was selected for two reasons; first, it controls for within-strata (the matched event-based units, in our case) correlation; and, second, it is more suitable for circumstances of rare events. The effect of injury on the severity of posttraumatic, anxiety, depression, and dissociation symptoms was tested with a set of one-factor tests (SAS: Proc Mixed [23]) that take into account the intraclass correlation caused by the matching. Finally, the effect of injury on the severity of these symptoms at each level of PTSD status (i.e., within those with and without PTSD) was tested using preplanned contrasts (LSMEANS option) in a set of two-factor (injury-by-PTSD status) tests (SAS: Proc Mixed [23]), that once again take into account the intraclass correlation caused by the matching. All tests were two-tailed, with p<0.05 indicating statistical significance.
Results
Prevalence of PTSD
According to the SCID, 10 (16.7%) of the 60 injured survivors, but only one (2.5%) of the 40 comparison participants, met diagnostic criteria for PTSD at the time of the interview (since trauma is typically not single in combat, it is worth noting that the event that caused the injury was the major traumatic event in all cases with PTSD). Another three (5.0%) of the 60 injured soldiers, but none of the comparison noninjured soldiers, reached a subthreshold level of PTSD (i.e., diagnostic criteria were met for two of the three DSM core posttraumatic clusters). The difference in the prevalence of PTSD between the two groups was statistically significant (odds ratio=8.6, 95% CI=1.1–394.3; p<0.04). Comparison of respondents with and without PTSD on background variables indicated that the two groups were highly homogeneous, with no statistically significant differences on any of the variables examined.
In addition to PTSD, participants were also assessed for other current and lifetime major axis I diagnoses. Of the 60 injured soldiers, two met DSM-IV criteria for current major depression, one for bipolar depression, two for adjustment disorder with depressive mood, and another two for substance use disorder. Of the 40 noninjured soldiers, one met diagnostic criteria for major depression and another one for adjustment disorder with depressive mood. In all cases, the onset of these comorbid diagnoses was after the traumatic event. While presence of any of these diagnoses was not significantly related to injury, there was a significantly greater likelihood that soldiers with PTSD would also suffer from a mood-related disorder (36.4%) than those without PTSD (3.4%) (p=0.008, Fisher’s exact test).
Psychiatric Symptom Severity
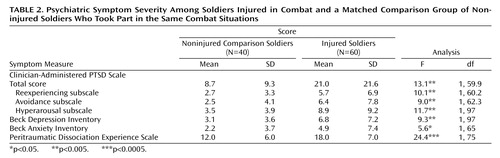
In this step, rather than focusing on PTSD as a formal diagnosis, we compared the frequency and intensity of PTSD symptoms—as well as dissociation, anxiety, and depression symptoms—in the injured and noninjured groups (Table 2). As can be seen, wounded participants, as a group, had significantly higher scores on all clinical scales than their noninjured comparison counterparts. With respect to the Clinician-Administered PTSD Scale subscales, the direction and size of intergroup differences were generally consistent across all three PTSD cluster scores (i.e., reexperiencing, avoidance, and hyperarousal), with a slightly larger effect on the hyperarousal subscale.
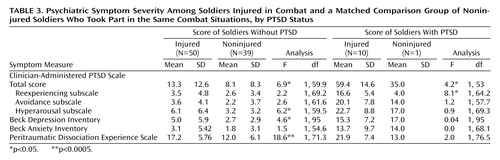
Next, in order to examine whether these intergroup differences could be explained solely on the basis of the larger number of participants with PTSD in the injured group, we retested the effect of injury on all clinical symptoms while controlling for PTSD status. That is, we tested the effect of injury twice: first only in those without PTSD and then only in those with PTSD (Table 3). As can be seen, the effect of injury on the Clinician-Administered PTSD Scale total score remained significant regardless of PTSD status. Of interest though is that while score on the hyperarousal subscale appeared to contribute most to the effect of injury on the overall Clinician-Administered PTSD Scale score among those without PTSD, among those with PTSD it was score on the reexperiencing subscale. This suggests that injury elevates hyperarousal symptoms in all subjects, but has a special effect on reexperiencing symptoms among those who go on to develop PTSD. Finally, Table 3 also reveals that injury has a significant effect on symptoms of both depression and peritraumatic dissociation in those without PTSD.
Severity of Trauma and Injury
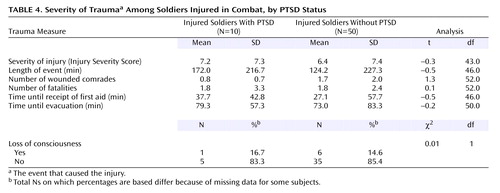
Next, we examined the potential mediating role of trauma severity as it affects the relationship between traumatic injury and further development of PTSD. Table 4 presents potential indicators of the severity of the trauma (i.e., the event that caused the injury) among the injured soldiers with and without PTSD. As can be seen, a set of t tests for independent groups revealed no significant differences between participants with and without PTSD on any of these characteristics. It is particularly noteworthy that there was no difference between the two groups on severity of injury, as assessed by the Injury Severity Score. This finding was corroborated by the correlations of the Injury Severity Score with the Clinician-Administered PTSD Scale subscale scores and its total score being all practically zero.
Last, we looked at the effect of physical injury on the co-occurrence of PTSD, depression, and anxiety symptoms. It is interesting that in the injured group, the correlations between PTSD symptoms and symptoms of anxiety (r=0.65, df=58, p<0.0001) and depression (r=0.75, df=58, p<0.0001) were remarkably higher than in the noninjured comparison group (r=–0.28 and r=–0.06, respectively). Moreover, a set of t tests revealed that the between-group differences for all pairs of corresponding correlations were also statistically significant (t=2.15–4.02, p<0.05).
Discussion
The current study attempted to isolate the unique contribution of bodily injury to the development of PTSD. To accomplish this goal we used an event-based, matched design. To the best of our knowledge, this is the first study that addresses this question utilizing such a powerful design. Consistent with most of the recent literature (4, 14), our findings clearly indicate that bodily injury is a risk factor—rather than a protective one—for PTSD. Moreover, in addition to just advancing the robustness of this notion, the data also suggest that the odds of developing PTSD following traumatic injury are approximately eight times higher than following injury-free trauma. In fact, they suggest that even this rather high figure might be an underestimate. This is so because about 35% of the originally approached injured soldiers, but none of the noninjured comparison subjects, refused participation. From the explanations that these nonparticipants gave for their refusal, it was quite obvious that many of them did so for reasons that can be interpreted as avoidance.
It is interesting that while associated with higher levels of anxiety and depression symptoms, bodily injury in this study was not related to increased prevalence of comorbid psychiatric diagnoses. In contrast, psychiatric comorbidity was significantly related to presence or absence of PTSD. This finding is consistent with previous studies, including our own (7), suggesting a strong association between PTSD and psychiatric comorbidity among injured trauma survivors. Taken together, our findings indicate that PTSD moderates psychiatric comorbidity following traumatic injury.
Our findings further suggest that bodily injury does not have a differential effect on any of the PTSD symptom domains. This finding was evident by the direction and size of differences, which were generally consistent across all three PTSD cluster scores. Such a finding is consistent with our previous results in a study with injured survivors of motor vehicle accidents (7).
What other factors might explain the increased risk for PTSD associated with bodily injury? The most simple and straightforward hypothesis is that bodily injury increases the perceived threat to one’s life or physical integrity during the trauma. Indeed, according to the literature, the perceived level of danger by trauma survivors is a better predictor of PTSD than the actual severity of the traumatic event (10). However, this explanation may be too simplistic because while strongly supporting the possibility that bodily injury contributes to the appraisal of the traumatic event as more dangerous, our data also suggest that this heightened level of perceived threat is not a simple, straightforward function of the severity of injury. This finding, which is consistent with previous studies (5, 14), suggests that bodily injury exerts its effect on perceived threat via interaction with other factors, such as the effect that it has on one’s (perceived and real) ability to function and cope during the traumatic event.
Another potential mediating factor between physical injury and PTSD might be peritraumatic dissociation, which has been implicated as a risk factor for PTSD in previous studies (24). This possibility was supported in our study by injured participants, with or without PTSD, reporting significantly higher levels of peritraumatic dissociation than their noninjured fellows. Furthermore, controlling for peritraumatic dissociation remarkably decreased the differences between the injured and noninjured groups on all the PTSD as well as the other clinical measures. While dissociation is commonly conceived of as a vulnerability factor in its impairing integration and reprocessing of the trauma, an interesting alternative possibility is that the relationship between bodily injury and dissociation might be reversed. That is, people who tend to dissociate under stress might be at higher risk for getting injured. Because of the post facto, retrospective nature of this study, such a possibility cannot be ruled out.
While not directly assessed in this study, there are also noteworthy biological mechanisms that may mediate between injury and PTSD. These hypothesized mechanisms relate to the complex interactions between the immune and stress-regulating systems, in particular the interaction between the hypothalamic-pituitary-adrenal (HPA) axis and proinflammatory mediators such as cytokines. In addition to its key role in the regulation of the stress response, the HPA axis is also involved in modulation of the immune response to inflammation and injury through proinflammatory mediators such as cytokines (25). Since alterations in the HPA axis have been suggested as a vulnerability factor for PTSD (26), situations that involve both emotional and injury-related stress may create an extra burden on an already compromised HPA axis. While this hypothesis has yet to be explored, numerous preclinical studies found that cytokines have adverse effects on memory, sleep, and mood (27). Similarly, they promote sickness behavior (27). Indeed, a previous study (28) found elevated CSF concentrations of interleukin-6 in patients with PTSD versus normal comparison subjects.
Finally, the extent to which the current findings can be generalized to other populations is worth consideration. Overall, the rate of PTSD in our sample (10%) was generally in line with, although at the lower end of, previous estimates among soldiers involved in combat activity. However, prevalence of PTSD in the noninjured group was very low (2.5%). This may be explained by the nature of the participants in our study, who were soldiers in elite units who underwent extensive preinduction screening and a long and demanding course of basic training, which enables further selection and facilitates acquisition of habitual coping styles. In addition, these units are characterized by high levels of motivation and unit cohesion, which have been shown to be resilience factors against the development of PTSD (29) as well as general mental health problems (30). These factors suggest that generalizing from this study should be made with caution and call for further replication with a more heterogeneous and unscreened sample.
A few methodological issues that limit interpretation of the current findings are worth mentioning. First, PTSD symptoms were assessed relatively long after the traumatic injury. Thus, our data provide a reliable estimate of stable posttraumatic symptoms (which also minimizes concerns regarding potential effects of the slightly longer event-to-interview time difference in the injured group). However, they do not answer questions related to acute stress reactions or the temporal course of posttraumatic adjustment as it is related to recovery from the physical injury. Second, severity of injury was assessed only at the time of hospitalization but not again at the time of assessment. Thus, our data cannot clarify the degree to which current injury or physical disability status may affect reported PTSD symptoms, nor can it clarify the degree to which pace of physical recovery may be influenced by early PTSD symptoms. Third, the raters completing the SCID and the Clinician-Administered PTSD Scale were not blind to the injury status of the participants. While this could result in a potential bias in PTSD diagnosis, this possibility is less likely given that ratings on the self-report measures (i.e., Peritraumatic Dissociation Experience Scale, Beck Depression Inventory, Beck Anxiety Inventory) were remarkably consistent with the raters’ evaluations. Finally, as can be recalled, a sizable proportion (35%) of injured patients refused to participate in the study. This raises the possibility that our sampling procedure was at risk for selection bias. Because of ethical constraints (i.e., lack of consent), we could not collect the necessary data to rule this possibility out. Yet, from the little we do know about these subjects (i.e., the reasons they gave for nonparticipation), it is obvious that such bias, had it existed, could only further strengthen our findings rather than weaken them. Last, and perhaps most important, trauma in this study was defined and assessed only in terms of its objective characteristics (i.e., combat participation). Since it is possible that not all combatants perceive this experience as subjectively traumatic, the current data cannot answer questions related to the unique contribution of physical injury to PTSD only among those whose combat experience was self-identified as traumatic.
In conclusion, our study provides clear evidence that bodily injury during trauma is a major risk factor for subsequent PTSD. Considering that emotional distress is often overlooked among injured patients hospitalized in surgical and trauma units, these findings highlight the importance of paying more attention to psychological aspects of their condition in general and to the early symptoms of PTSD in particular, both during hospitalization and after discharge.
 |
 |
 |
 |
Received May 5, 2003; revision received Dec. 10, 2003, and March 31, 2004; accepted April 23, 2004. From the University of Haifa Psychology Department, Haifa, Israel; the Departments of Psychiatry and Orthopedics, Rambam Medical Center; and the Faculty of Industrial Engineering and Management, Technion, Haifa, Israel. Address correspondence and reprint requests to Dr. Koren, Psychiatry Department, Rambam Medical Center, Haifa, Israel; [email protected] (e-mail). Supported by a grant from the Chief Scientist of the Medicine Corps of the Israel Defense Forces. The authors thank O. Shelli-Vacnin, A. Tzarfati, D. Mor, Y. Goshen-Kita, and L. Ziv for their assistance in participant recruitment and interviewing. The authors also thank Y. Baruch, M.D., and E. Budner, Ph.D., from the Medicine Corps of the Israel Defense Forces for assistance in patient recruitment.
1. O’Donnell ML, Creamer M, Bryant RA, Schnyder U, Shalev A: Posttraumatic disorders following injury: an empirical and methodological review. Clin Psychol Rev 2003; 23:587–603Crossref, Medline, Google Scholar
2. Ulman RB, Brothers D: A self-psychological reevaluation of posttraumatic stress disorder (PTSD) and its treatment: shattered fantasies. J Am Acad Psychoanal 1987; 15:175–203Crossref, Medline, Google Scholar
3. Merbaum M, Hefez A: Some personality characteristics of soldiers exposed to extreme war stress. J Consult Clin Psychol 1976; 44:1–6Crossref, Medline, Google Scholar
4. Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, Weiss DS: Trauma and the Vietnam War Generation: Report of Findings From the National Vietnam Veterans Readjustment Study. New York, Brunner/Mazel, 1990Google Scholar
5. Pitman RK, Altman B, Macklin ML: Prevalence of posttraumatic stress disorder in wounded Vietnam veterans. Am J Psychiatry 1989; 146:667–669Link, Google Scholar
6. Ursano RJ, Fullerton CS, Epstein RS, Crowley B, Kao T-C, Vance K, Craig KJ, Dougall AL, Baum A: Acute and chronic posttraumatic stress disorder in motor vehicle accident victims. Am J Psychiatry 1999; 156:589–595Abstract, Google Scholar
7. Koren D, Arnon I, Klein E: Acute stress response and posttraumatic stress disorder in traffic accident victims: a one-year prospective, follow-up study. Am J Psychiatry 1999; 156:367–373Abstract, Google Scholar
8. Blanchard EB, Hickling EJ, Barton KA, Taylor AE, Loos WR, Jones-Alexander J: One-year prospective follow-up of motor vehicle accident victims. Behav Res Ther 1996; 34:775–786Crossref, Medline, Google Scholar
9. Mayou R, Bryant B, Duthie R: Psychiatric consequences of road traffic accidents. BMJ 1993; 307:647–651Crossref, Medline, Google Scholar
10. Shalev AY: Posttraumatic stress disorder among injured survivors of a terrorist attack: predictive value of early intrusion and avoidance symptoms. J Nerv Ment Dis 1992; 180:505–509Crossref, Medline, Google Scholar
11. Kilpatrick DG, Saunders BE, Amick-McMullan A, Best CL, Veronen LJ, Resnick HS: Victim and crime factors associated with the development of crime-related post-traumatic stress disorder. Behav Ther 1989; 20:199–214Crossref, Google Scholar
12. Perry S, Difede J, Musngi G, Frances AJ, Jacobsberg L: Predictors of posttraumatic stress disorder after burn injury. Am J Psychiatry 1992; 149:931–935Link, Google Scholar
13. Bryant RA, Harvey AG: Relationship between acute stress disorder and posttraumatic stress disorder following mild traumatic brain injury. Am J Psychiatry 1998; 155:625–629Link, Google Scholar
14. Michaels AJ, Michaels CE, Moon CH, Smith JS, Zimmerman MA, Taheri PA, Peterson C: Posttraumatic stress disorder after injury: impact on general health outcome and early risk assessment. J Trauma 1999; 47:460–467Crossref, Medline, Google Scholar
15. Mellman TA, David D, Bustamante V, Fins AI, Esposito K: Predictors of post-traumatic stress disorder following severe injury. Depress Anxiety 2001; 14:226–231Crossref, Medline, Google Scholar
16. Benbenishty R: Combat stress reaction and changes in military medical profile. Mil Med 1991; 156:68–70Crossref, Medline, Google Scholar
17. First MB, Spitzer RL, Gibbon M, Williams JBW: Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition (SCID-P), version 2. New York, New York State Psychiatric Institute, Biometrics Research, 1994Google Scholar
18. Blake DD, Weathers FW, Nagy LN, Kaloupek DG, Klauminzer G, Charney DS, Keane TM: A clinician rating scale for assessing current and lifetime PTSD: the CAPS-1. Behavior Therapist 1990; 18:187–188Google Scholar
19. Beck AT, Steer RA: Manual for the Revised Beck Depression Inventory. San Antonio, Tex, Psychological Corp, 1987Google Scholar
20. Beck AT, Steer RA: Beck Anxiety Inventory Manual. San Antonio, Tex, Psychological Corp, 1990Google Scholar
21. Marmar CR, Weiss DS, Metzler TJ: The Peritraumatic Dissociative Experiences Questionnaire, in Assessing Psychological Trauma and PTSD. Edited by Wilson JP, Keane TM. New York, Guilford, 1997, pp 412–428Google Scholar
22. Association for the Advancement of Automotive Medicine: The Abbreviated Injury Scale, 1990 Revision. Des Plaines, Ill, AAAM, 1990Google Scholar
23. SAS/STAT User’s Guide, version 8. Cary, NC, SAS Institute, 1999Google Scholar
24. Shalev AY, Peri T, Canetti L, Schreiber S: Predictors of PTSD in injured trauma survivors: a prospective study. Am J Psychiatry 1996; 153:219–225Link, Google Scholar
25. Schobitz B, Reul JM, Holsboer F: The role of the hypothalamic-pituitary-adrenocortical system during inflammatory conditions. Crit Rev Neurobiol 1994; 8:263–291Medline, Google Scholar
26. Yehuda R: Biology of posttraumatic stress disorder. J Clin Psychiatry 2001; 62(suppl 17):41–46Google Scholar
27. Larson SJ, Dunn AJ: Behavioral effects of cytokines. Brain Behav Immun 2001; 15:371–387Crossref, Medline, Google Scholar
28. Baker DG, Ekhator NN, Kasckow JW, Hill KK, Zoumakis E, Dashevsky BA, Chrousos GP, Geracioti TD Jr: Plasma and cerebrospinal fluid interleukin-6 concentrations in posttraumatic stress disorder. Neuroimmunomodulation 2001; 9:209–217Crossref, Medline, Google Scholar
29. Eid J, Johnsen BH: Acute stress reactions after submarine accidents. Mil Med 2002; 167:427–431Crossref, Medline, Google Scholar
30. Martin L, Rosen LN, Durand DB, Knudson KH, Stretch RH: Psychological and physical health effects of sexual assaults and nonsexual traumas among male and female United States Army soldiers. Behav Med 2000; 26:23–33Crossref, Medline, Google Scholar



