The Changing Prevalence and Severity of Obsessive-Compulsive Disorder Criteria From DSM-III to DSM-IV
Abstract
OBJECTIVE: Relative to other mental disorders, the prevalence of obsessive-compulsive disorder (OCD) in the general population is not well established. Some epidemiological surveys have determined the prevalence of DSM-III OCD, but this is one of the first reports, to the authors’ knowledge, of DSM-IV OCD’s prevalence. METHOD: Data from the Australian National Survey of Mental Health and Well-Being, a nationally representative epidemiological survey of mental disorders, were analyzed. The prevalence and associated characteristics of DSM-IV OCD were identified, and then the data were rescored for DSM-III OCD. Cases defined by each system were compared. RESULTS: The 12-month prevalence of DSM-IV OCD was 0.6%, considerably less than found in surveys employing DSM-III diagnostic criteria. DSM-IV OCD showed significantly higher levels of comorbidity, disability, health service use, and treatment received. CONCLUSIONS: Changes in the reported prevalence and severity of OCD between DSM-III and DSM-IV cases are most likely a function of the differences in diagnostic criteria between DSM-III and DSM-IV.
Obsessive-compulsive disorder (OCD) is a chronic and debilitating condition of which the prevalence in the general population remains somewhat controversial. Early investigations suggested that OCD was a relatively rare condition, with Black (1) reporting that only 3% of all neurotic patients from a series of studies were diagnosed as obsessional and Woodruff and Pitts (2) estimating that OCD affects a mere 0.05% of the population. Karno et al. (3) reported the lifetime prevalence rate of DSM-III OCD in the Epidemiologic Catchment Area (ECA) studies as 2.5%, averaged across five U.S. catchment areas. The point prevalence (2 weeks) was 1.2%, and the annual prevalence was 1.6%. The Cross National Collaborative Group (4) summarized the findings from the various DSM-III studies and reported lifetime prevalence rates in seven countries as ranging from a low of 0.7% (in Taiwan) to a high of 2.5% (in Puerto Rico). Taiwan excluded, the 12-month prevalence rates across the other sites were consistent; the U.S. study reported 1.3%; Edmonton, Canada 1.4%; Puerto Rico 1.8%; Munich 1.6%; and Korea and New Zealand 1.1%.
The findings of higher-than-expected rates of OCD in epidemiological studies resulted in OCD being labeled a “hidden epidemic” (5) and being ranked 20th in the Global Burden of Disease studies among all diseases as a cause of disability-adjusted life years lost in developed countries (6). Subsequent investigations cast some doubt on the reliability of the results obtained in these epidemiological studies. Nelson and Rice (7) examined the temporal stability of the lifetime National Institute of Mental Health Diagnostic Interview Schedule (DIS) diagnosis of DSM-III OCD by reinterviewing ECA subjects (wave 1) with a positive diagnosis of OCD 12 months later (wave 2). The authors reported a kappa statistic of 0.2, with only 19% of the original 291 subjects reporting lifetime OCD at wave 1 receiving a similar diagnosis at wave 2. Because of these findings, the authors concluded that the wave 1 lifetime prevalence may have been largely made up of false positives and that the validity of DIS-diagnosed OCD is questionable. Stein et al. (8) also cast doubt on the validity of the DSM-III epidemiological data. The authors examined the prevalence of DSM-IV OCD in 2,261 Canadian subjects who were interviewed by lay interviewers over the telephone. The study used a modified version of the Composite International Diagnostic Interview and noted a 1-month prevalence rate of 3.1%. However, when a subgroup of positively diagnosed OCD subjects was reinterviewed by clinicians using a structured clinical interview (the Structured Clinical Interview for DSM-IV), the 1-month prevalence rate fell to 0.6%, with a further 0.6% fulfilling the authors’ criteria for subclinical OCD. The main source of discrepancy was the tendency for respondents to label everyday sources of “worry, concern, preoccupation or interests as obsessions” (8, p. 1123), which lay interviewers were unable to differentiate from true obsessions, as well as a tendency for respondents to overestimate the degree of disability or distress associated with the symptoms.
Up to 80% of the general population may experience intrusive, unpleasant, unwanted thoughts similar to those seen in OCD (9, 10), albeit to a less distressing and frequent degree than in OCD. More than half the population may engage in ritualized behavior (11), also to a less distressing degree than clinical subjects. The possibility that OCD diagnosed with the DIS/Composite International Diagnostic Interview is overinclusive because of its inability to determine the frequency, distress, and disability of obsessive-compulsive symptoms is not surprising. Similarly, the finding that everyday worries were often confounded with obsessions is not surprising, particularly because one item that makes up the diagnosis of OCD in the DIS and the Composite International Diagnostic Interview (version 1.1) includes “persistent or unpleasant thoughts that relatives who are away have been hurt or killed,” a symptom more in keeping with generalized anxiety disorder than with OCD.
Possible inaccuracies in the reported DSM-III prevalence rates were also noted by Karno and Golding (12), who suggested that more refined definitions of obsessions and compulsions associated with DSM-III-R would “reduce the number of ‘borderline’ cases in future epidemiological studies employing the revised criteria and will produce a slight lowering of prevalence rates” (12, p. 207). Changes in the DSM-III-R and DSM-IV diagnostic criteria have indeed focused on better defining obsessions and compulsions while also emphasizing the degree of distress and impairment required for the diagnosis to be positive. For example, DSM-III suggests that “obsessions or compulsions are a significant source of distress to the individual or interfere with social or role functioning” (p. 235). DSM-IV notes that the obsessions or compulsions should be recognized at some point as “excessive or unreasonable” and that they “cause marked distress, are time consuming, or significantly interfere with the person’s normal routine, occupational (or academic) functioning or usual social activities or relationships” (p. 423). Of equal importance, DSM-IV specifically excludes other axis I disorders that may confound the diagnosis. Thus, the prevalence of OCD may also be affected by the changes in the diagnostic criteria from DSM-III to DSM-IV.
The purpose of the current study was twofold: first, to report on the prevalence of DSM-IV OCD in Australia, as determined in the Australian National Survey of Mental Health and Well-Being, and second, to examine the prevalence rates when the data are rescored according to the DSM-III diagnostic criteria. This was the first such analysis in a nationally representative survey.
Method
Survey Design and Sample
The Australian National Survey of Mental Health and Well-Being was a nationwide household survey of adults conducted in 1997. It aimed to determine the prevalence of both ICD-10 and DSM-IV mental disorders in the community and to describe their associated disability and service use. The overall method and design of the survey have been described in detail elsewhere (13). The interview was computerized and conducted by trained interviewers from the Australian Bureau of Statistics, a statutory body responsible for conducting such surveys using ethical protocols that include written informed consent. The Australian Bureau of Statistics employed a stratified multistage sampling process resulting in a sample of 10,641 persons over the age of 18, a response rate of 78.1%. The sample was weighted to conform to the age and sex distribution of the Australian population and to account for the probability of selection.
Assessment of Diagnosis
DSM-IV diagnoses of OCD and other anxiety, affective, and substance use disorders were made by using the Composite International Diagnostic Interview (version 2.1). The presence of DSM-IV obsessions was assessed with 10 separate questions. The first two asked about unpleasant, intrusive, inappropriate, and persistent thoughts, such as “the idea that your hands are dirty or have germs on them” or “the idea that you might harm someone, even though you really didn’t want to.” If either of these questions was answered positively, eight remaining questions asked about attempts to suppress the thoughts; the excessiveness, unreasonableness, distress, and interference in normal functioning caused by the thoughts; whether the thoughts were time-consuming; and whether they were exclusively related to the symptoms of a comorbid axis I disorder. The presence of DSM-IV compulsions was then assessed with 10 questions. The first four questions asked about four different types of repetitive behaviors: “doing something over and over again…things like washing their hands…or going back several times to make sure they’ve locked the door or turned off the stove”; “doing something in a certain order, like getting dressed”; “counting something like the squares in a tile floor”; and “saying certain words over and over, either aloud or to yourself.” The remaining six questions asked about the excessiveness, unreasonableness, distress, and interference in normal functioning caused by the compulsions; whether they were time-consuming; and whether they were exclusively related to the symptoms of a comorbid axis I disorder. All symptoms were assessed for their presence within the 12 months before the interview. One-month diagnoses were derived from 12-month diagnoses by restricting the sample to those who experienced the symptoms in the 4 weeks before the interview. Personality disorder diagnoses were made with the use of a screening questionnaire for personality disorders (14). This screening questionnaire was not a fully standardized diagnostic interview for personality disorders but was included in the interview to provide a tentative estimate of the prevalence of personality disturbance.
Assessment of Disability
Three measures of disability are reported. The Medical Outcomes Study 12-Item Short-Form Health Survey (15) is a measure of disablement. It has two regression-weighted scales: a mental health summary scale and a physical health summary scale. The continuous scales are scored such that the mean is 50 and the standard deviation is 10. Higher scores indicate less disability. The role functioning scale of the Brief Disability Questionnaire (16) assesses the extent to which physical and social role activities have been limited in the 4 weeks before the interview. The Disability Days Scale (17) is a summary measure of the number of days in the past 4 weeks that an individual has been unable to perform or has had to cut down on his or her normal activities because of ill health. For ease of interpretation, scores on the three continuous measures of disability were transformed into z scores (calculated as the individual score minus the mean of all scores divided by the standard deviation of all scores). Thus, when these measures are used as independent variables in logistic regression analyses, the resultant odds ratios represent a one standard deviation—as opposed to a 1-point—shift in the disability measure.
Assessment of Service Use and Treatment Received
The respondents were asked about both inpatient and outpatient service use in the 12 months before the interview. If the respondents had consulted any health professional, they were asked how many times they had visited the office for mental health problems, including “stress, anxiety, depression, or dependence on drugs or alcohol.” Those consulting for mental health problems were asked about the type of help received.
Analysis
Odds ratios were derived from logistic regression models and are presented as either unadjusted odds ratios derived from bivariate regression models where only one predictor was entered into the model or adjusted odds ratios where some or all predictors were entered into the model at the same time to obtain estimates that account for the effects of other variables. Standard errors around proportions and confidence intervals around odds ratios were calculated with delete-one jackknife repeated replications (18) to account for the complex sampling design. The SUDAAN software package, designed specifically for use with complex survey samples, was used for all analyses (19).
Rescoring to Obtain DSM-III Diagnoses of OCD
Data were rescored to generate DSM-III OCD diagnoses. This was made possible by the similarity between the items in the Composite International Diagnostic Interview and the DIS that assess OCD symptoms as well as the method that both instruments employed to probe for clinical significance. To meet criteria for DSM-III OCD, the respondents were required to meet two criteria. First, a positive response on either of the two questions about unpleasant, intrusive, inappropriate, and persistent thoughts was needed, and then a positive response on one of the three questions about engaging in repetitive behaviors was required (DSM-III criterion A). The question about cognitive compulsions was not included because it was not considered part of the DSM-III diagnosis of OCD. Second, a positive response to the questions assessing distress and/or interference was required (DSM-III criterion B). The exclusion rules in DSM-III criterion C were not operationalized. The modifications to the scoring algorithm used in the current study are available from Dr. Slade.
Results
Prevalence and Demographic Correlates of DSM-IV OCD
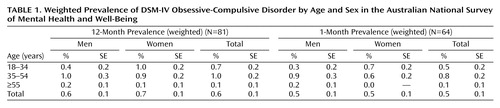
The weighted prevalence of 12- and 1-month DSM-IV OCD by age and sex is shown in Table 1. A total of 81 subjects (0.6%) were assigned a 12-month diagnosis of OCD. The weighted 1-month prevalence was 0.5%. The average age at onset was 27 years (SE=4.5) for men and 25 years (SE=3.1) for women.
Unadjusted and adjusted demographic correlates of 12-month DSM-IV OCD were calculated. No differences between people with OCD and the remainder of the sample were noted for sex, marital status, education, language spoken at home, migration status, urbanicity, or household composition. There was a significantly higher prevalence of OCD among those who were unemployed and those who were not in the labor force than among those who were employed (adjusted odds ratio=8.7 and 4.3, respectively), and older individuals (>55 years) were significantly less likely than those in younger age groups to have OCD (adjusted odds ratio=0.1).
Comorbidity
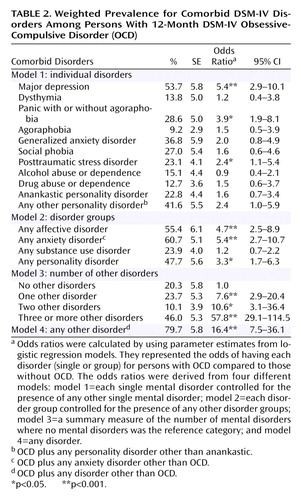
Comorbidity was common. The percents of DSM-IV OCD subjects who also met criteria for other DSM-IV disorders are shown in Table 2. Overall, individuals with OCD were significantly more likely than people without OCD to have met criteria for at least one affective, anxiety, substance use, or personality disorder (odds ratio=16.4), with 79.7% of those with OCD having another disorder. OCD subjects were also significantly more likely to have two (odds ratio=10.6) and three or more other disorders (odds ratio=57.8) than those without a diagnosis of OCD, with 46% of individuals with OCD meeting the criteria for three or more disorders in the 12 months before the interview.
Among the individual disorders, comorbidity with major depression was highest at 54% (odds ratio=5.4). Although a general association between OCD and any other anxiety disorder was found (odds ratio=5.4), the presence of OCD was significantly associated only with the presence of panic disorder (odds ratio=3.9) and posttraumatic stress disorder (odds ratio=2.4). No relationship was noted between OCD and substance use disorders. Although there was a more general association between OCD and any personality disorder (odds ratio=3.3), there was no specific association between OCD and anankastic personality disorder, the ICD-10 personality disorder that is most similar to DSM-IV obsessive-compulsive personality disorder.
Disability, Health Service Use, and Treatment Received
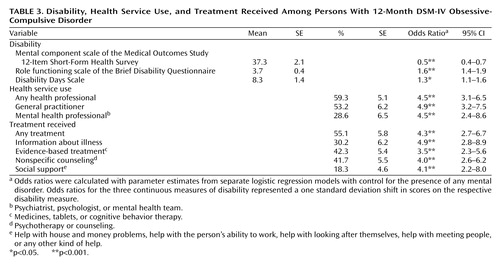
Disability, health service use, and treatment received for DSM-IV OCD are shown in Table 3. Compared to the rest of the population, OCD was associated with significant disability, as measured by the mental component scale of the 12-Item Short-Form Health Survey (odds ratio=0.5; low scores indicate high levels of disability), the role functioning scale of the Brief Disability Questionnaire (odds ratio=1.6), and the Disability Days Scale (odds ratio=1.3).
The proportion of OCD subjects who consulted health professionals in the 12 months before the interview was consistent with the levels of disability. Fifty-nine percent of those with OCD consulted at least one health professional for a mental health problem, although many consulted more than one professional. A general practitioner was consulted by 53.2% of those with OCD and a psychologist or psychiatrist by 28.6% of those with OCD. A summary of the treatments received indicates that approximately half of the OCD subjects who consulted any health professional for a mental health problem received treatment of any kind, and 42% received an evidence-based intervention.
Comparison of DSM-III and DSM-IV OCD
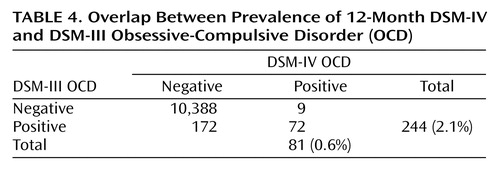
The overlap between the prevalence of DSM-IV and DSM-III OCD is shown in Table 4. The weighted prevalence of 12-month DSM-III OCD was 2.1%, a prevalence rate somewhat higher than the rates reported in the cross-national sites but not markedly higher than Puerto Rico at 1.8% and Munich at 1.6%. It is possible for individuals to meet both DSM-IV and DSM-III diagnostic criteria for OCD. For statistical comparison purposes, two mutually exclusive groups were constructed, one containing all DSM-IV cases of OCD (N=81) and the other containing DSM-III but not DSM-IV cases of OCD (N=172). These two groups represent all DSM-III or DSM-IV OCD cases in the sample. It should be noted that 89% of those with DSM-IV OCD also met the criteria for DSM-III OCD.
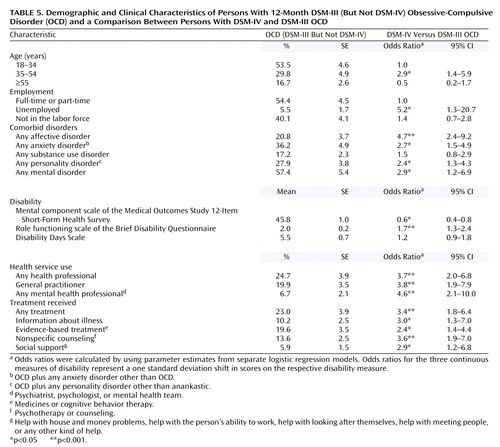
Comparisons between the DSM-IV and DSM-III cases of OCD are displayed in Table 5. DSM-IV subjects of OCD were more severe on a number of levels. They were significantly more likely among the 35–54-year-old age group compared to the younger age group as well as among the unemployed compared to the employed. DSM-IV OCD subjects were more likely to have comorbid psychiatric disorders except for substance use disorders (statistically significant odds ratios ranged from 2.4 to 4.7). With control for the presence of any comorbid disorder, DSM-IV OCD subjects were also more likely than DSM-III cases to be disabled on two out of the three disability measures, and they were more likely to use health services and to receive treatment.
Discussion
The 12-month prevalence of DSM-IV OCD in Australia was found to be 0.6% of the adult population, less than that reported in epidemiological studies employing DSM-III criteria. There are a number of general similarities between the current study and previous epidemiological investigations. First, the average age at onset of OCD was 26.1 years, similar to the age at onset reported in the U.S. ECA survey (26.2 years) and in Edmonton and New Zealand (27.2 years) (4). Second, the sex ratio of close to one is similar to the majority of other epidemiological studies. Third, there was a noteworthy decrease in prevalence of OCD in older age groups (>55 years). Fourth, the high rate of OCD comorbidity with anxiety disorders and affective disorders is noted in a number of epidemiological and clinical studies. Overall, lower rates of alcohol and substance abuse were found in the current 12-month Australian cohort than in lifetime cohorts from other countries. The DSM-IV criteria for drug abuse or dependence were fulfilled by 12.7% of those with 12-month DSM-IV OCD in the current investigation, compared to a DSM-III lifetime rate of 17.6% of the U.S. ECA survey OCD cohort and 26.5% in Edmonton (12, 20).
There are a number of differences. In general, comorbidity rates of OCD with affective and anxiety disorders are higher in the current study than in previous investigations. For example, in the U.S. ECA survey, Karno et al. (3) reported that 31.7% of the OCD cohort met criteria for lifetime major depression, while 13.8% met the criteria for panic disorder. Similar rates of lifetime depression (29.6%) and panic (9.8%) were reported in Edmonton (20). In contrast, 12-month major depression was reported in 53.7% of the OCD subjects in the current study, and panic (with and without agoraphobia) was found in 28.6% of the OCD cohort. The fact that the current investigation focuses on 12-month diagnoses while the U.S. ECA survey focused on lifetime diagnoses would suggest the opposite, i.e., that there would be a higher rate of comorbidity in the lifetime studies. This result tends to reinforce the notion that those fulfilling DSM-IV OCD criteria in the current study were more severely ill than those identified as suffering from OCD in other epidemiological studies based on DSM-III criteria.
Further support for DSM-IV severity comes from rescoring of the data according to DSM-III criteria. This resulted in an additional 172 cases being assigned a positive diagnosis of OCD, translating to a weighted 12-month population prevalence rate of 2.1%, a figure not unlike previous epidemiological studies employing DSM-III criteria. However, noteworthy differences are evident when comparing the features of the individuals assigned a DSM-III diagnosis of OCD (but not a DSM-IV diagnosis) to those assigned a DSM-IV diagnosis. DSM-IV subjects were more comorbidly ill, more disabled, and more likely to seek treatment and to receive a specific treatment. They were also significantly more likely to be unemployed. Although an argument can be made that the increased disability of DSM-IV subjects could be a function of greater levels of comorbidity, control for the presence of any comorbid condition resulted in the DSM-IV subjects remaining significantly more disabled on the mental component scale of the 12-Item Short-Form Health Survey and the role functioning scale of the Brief Disability Questionnaire.
The DSM-IV 12-month prevalence rate of 0.6% and the 1-month prevalence of 0.5% are almost identical to the 1-month prevalence rate of 0.6% reported by Stein et al. (8) when a proportion of the OCD subjects identified with the Composite International Diagnostic Interview were reassessed clinically. The instrument used in the current study (the Composite International Diagnostic Interview [version 2.1]), also administered by lay interviewers, was designed to specifically reflect the changes in the OCD diagnostic criteria from DSM-III to DSM-IV. The current Composite International Diagnostic Interview/DSM-IV diagnosis of OCD is made on the basis of more clearly defined obsessions and compulsions that include cognitive rituals and specific exclusion of thoughts not directly associated with OCD. More important, a positive diagnosis also requires ratings of unreasonableness, intrusiveness, distress, excessiveness, interference, discomfort, and resistance. Thus, the difference between the prevalence rates reported in the current study and previous epidemiological studies may be a function of changes to the diagnostic criteria and subsequent changes in the instruments used to assess the disorder.
Traditionally, OCD has been regarded as a chronic, disabling condition that was difficult to treat. The defining criteria of the condition were intrusive thoughts and compulsive rituals, and the early diagnostic systems reflected such criteria. To a large extent, disability was assumed because only the severe and disabled came in for treatment and were described in the literature. As the knowledge base of OCD increased, refinements to the DSM criteria of OCD as well as acknowledgment of the disability associated with the clinical presentation of the disorder resulted in the application of more stringent diagnostic criteria. Although this has led to a lower overall prevalence rate, the higher degree of disability and comorbidity in the identified cases is more in keeping with the clinical presentation of the disorder, and this in itself may be problematic in determining the community prevalence of OCD.
Clearly, clinical presentation has informed changes in the diagnostic criteria. While benefits have included better definition and demarcation of obsessions and compulsions, it is more than likely that the more severely disabled are seen for treatment, resulting in an artificially raised severity threshold for a positive diagnosis. As noted in previous sections, obsessions and compulsions are common in the community, although reported disability and interference are less common. Ratings of disability and interference are often subjective and do not take into account such influencing factors as accommodation of symptoms, embarrassment, or denial of interference. Although the evidence is merely anecdotal, it is not uncommon for patients to be seen for treatment because of family or a significant other’s insistence and to deny any interference or disability. Similarly, it is not uncommon for loved ones and health professionals to seek assistance for OCD sufferers who refuse to acknowledge any difficulty as they accommodate their symptoms (e.g., getting up an hour early to perform checking rituals before leaving home). Such community cases, the prevalence of which is unknown, would not have been included in the current survey.
Other issues in the identification of positive cases also need to be considered in interpreting the data from the current study. Any structured instrument administered by lay interviewers will be less reliable in properly assessing the sometimes complex presentation of OCD, and clinical assessment is sometimes necessary to differentiate it from other disorders where there may be overlap. Clinical reassessment of a proportion of identified DSM-III and DSM-IV OCD cases would have considerably strengthened the findings of the current study; however, privacy agreements precluded repeated access to any participants in the survey. Alternatively, the addition of self-report obsessive-compulsive inventories (e.g., the Padua Inventory, the Yale-Brown Obsessive Compulsive Scale self-report) may have further assisted in identifying positive cases, particularly among those fulfilling DSM-III but not DSM-IV criteria. Of greater importance is the possibility that a significant proportion of those fulfilling DSM-III but not DSM-IV criteria may have fallen below the cutoff for DSM-IV disability and interference criteria on the basis of receiving effective treatment. One-fifth (19.6%) of those fulfilling DSM-III criteria reported receiving evidence-based treatment (pharmacotherapy or cognitive behavior therapy), and 23% reported receiving treatment of any kind. It could be argued that some or all of these individuals may have fulfilled DSM-IV criteria in the absence of such treatment, i.e., that they were treatment responders, particularly those reporting evidence-based treatment. Although 42.3% of the DSM-IV sample had received evidence-based treatment, their overall greater disability and comorbidity would suggest that many of these individuals may have been at the more severe end of the OCD spectrum and their symptoms may have been less likely to fall below the DSM-IV disability threshold, even though there may have been some treatment response. Finally, the literature suggests that a significant proportion of OCD subjects report a waxing and waning course, and a small proportion are classified as episodic (21, 22). It is possible that a proportion of those whose symptoms were classified as meeting DSM-III but not DSM-IV OCD criteria also did not meet disability and interference thresholds as a result of the natural severity fluctuations of OCD. Again, those fulfilling DSM-IV criteria, being more severely ill, may have had symptoms remaining above the thresholds, despite similar fluctuations.
Conclusions
The 12-month prevalence of DSM-IV OCD in Australia is 0.6%, a figure considerably less than expected from estimates of previous DSM-III epidemiological studies conducted in other countries. The findings from the current study indicate that the differing prevalence is a function of the changes in diagnostic criteria from DSM-III to DSM-IV, which are reflected in the instruments used to assess population prevalence. Comparison of identified DSM-IV cases with DSM-III cases that did not meet DSM-IV criteria indicated considerably greater severity among the DSM-IV cases in terms of comorbidity, disability, service use, and unemployment. Previous epidemiological estimates may have been confounded by identification of milder (nonclinical) cases and other disorders where symptoms may overlap with OCD. The cases identified in the current study are similar to those seen in clinical practice in terms of disability and comorbidity. Although identified cases are reflective of the OCD population presenting for clinical treatment, they may not be an accurate reflection of the full dimension of OCD-type symptoms in the community.
 |
 |
 |
 |
 |
Received Dec. 28, 2003; revision received May 25, 2004; accepted Aug. 30, 2004. From the Clinical Research Unit for Anxiety and Depression, St. Vincent’s Hospital; the School of Psychiatry, University of New South Wales, Sydney. Address correspondence and research requests to Dr. Slade, Clinical Research Unit for Anxiety and Depression, St. Vincent’s Hospital, 299 Forbes St., Darlinghurst, N.S.W., 2010, Australia; [email protected] (e-mail).
1. Black A: The natural history of obsessional neurosis, in Obsessional States. Edited by Beech HR. London, Methuen, 1974, pp 19–54Google Scholar
2. Woodruff R, Pitts FN Jr: Monozygotic twins with obsessional illness. Am J Psychiatry 1964; 120:1075–1080Link, Google Scholar
3. Karno M, Golding JM, Sorenson SB, Burnam MA: The epidemiology of obsessive compulsive disorder in five US communities. Arch Gen Psychiatry 1986; 45:1094–1099Crossref, Google Scholar
4. Weissman MM, Bland RG, Canino GJ, Greenwald S, Hwu H-G, Lee CK, Newman SC, Oakley-Browne MA, Rubio-Stipec M, Wickramaratne PJ, Wittchen H-U, Yeh E-Y (Cross National Collaborative Group): The cross-national epidemiology of obsessive-compulsive disorder. J Clin Psychiatry 1994; 55(suppl 3):5–10Google Scholar
5. Hollander E: Obsessive-compulsive disorder: the hidden epidemic. J Clin Psychiatry 1997; 58(suppl 12):3–6Google Scholar
6. Murray CJL, Lopez AD: The Global Burden of Disease. Geneva, World Health Organization, 1996Google Scholar
7. Nelson E, Rice J: Stability of diagnosis of obsessive-compulsive disorder in the Epidemiologic Catchment Area study. Am J Psychiatry 1997; 154:826–831Link, Google Scholar
8. Stein MB, Forde DR, Anderson G, Walker JR: Obsessive-compulsive disorder in the community: an epidemiologic survey with clinical reappraisal. Am J Psychiatry 1997; 154:1120–1126Link, Google Scholar
9. Salkovskis PM, Harrison J: Abnormal and normal obsessions: a replication. Behav Res Ther 1984; 22:308–312Crossref, Google Scholar
10. Rachman SJ, de Silva P: Abnormal and normal obsessions. Behav Res Ther 1978; 16:233–238Crossref, Medline, Google Scholar
11. Muris P, Merchelback H, Clavan M: Abnormal and normal compulsions. Behav Res Ther 1997; 35:249–252Crossref, Medline, Google Scholar
12. Karno M, Golding JM: Obsessive compulsive disorder, in Psychiatric Disorders in America: The Epidemiological Catchment Area Study. Edited by Robins L, Reiger DA. New York, Free Press, 1991, pp 204–219Google Scholar
13. Andrews GA, Henderson S, Hall W: Prevalence, comorbidity, disability and service utilisation: overview of the Australian National Mental Health Survey. Br J Psychiatry 2001; 178:145–153Crossref, Medline, Google Scholar
14. Loranger AW, Janca A, Sartorius N (eds): Assessment and Diagnosis of Personality Disorders. Cambridge, UK, Cambridge University Press, 1997Google Scholar
15. Ware J Jr, Kosinski M, Keller SD: A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996; 34:220–233Crossref, Medline, Google Scholar
16. Von Korff M, Ustun TB, Ormel J, Kaplan I, Simon GE: Self report disability in an international primary care study of psychological illness. J Clin Epidemiol 1996; 49:297–303Crossref, Medline, Google Scholar
17. Kessler R, Frank G: The impact of psychiatric disorders on work loss days. Psychol Med 1997; 27:861–873Crossref, Medline, Google Scholar
18. Kish L, Frankel MR: Inference from complex samples. J R Stat Soc B 1974; 36:1–37Google Scholar
19. Shah BV, Barnwell BG, Bieler GS: SUDAAN User’s Manual, Release 7.5. Research Triangle Park, NC, Research Triangle Institute, 1997Google Scholar
20. Kolada JL, Bland RC, Newman SC: Obsessive-compulsive disorder. Acta Psychiatr Scand Suppl 1994; 376:24–35Crossref, Medline, Google Scholar
21. Kringlen E: Obsessional neurotics: a long term follow-up. Br J Psychiatry 1965; 111:709–722Crossref, Medline, Google Scholar
22. Rasmussen SA, Eisen JL: The epidemiology and differential diagnosis of obsessive compulsive disorder. J Clin Psychiatry 1992; 53(suppl 4):4–10Google Scholar



