Generalized Anxiety Disorder in Patients With Major Depression: Is DSM-IV’s Hierarchy Correct?
Abstract
OBJECTIVE: DSM-III imposed a hierarchical relationship in the diagnosis of anxiety disorders in depressed patients, stipulating that anxiety disorders could not be diagnosed if their occurrence was limited to the course of a mood disorder. In the subsequent versions of the DSM this hierarchy was eliminated for all anxiety disorders except generalized anxiety disorder. The authors examined the validity of this remaining hierarchical relationship between mood and anxiety disorders. METHOD: Psychiatric outpatients with major depressive disorder (N=332) were evaluated with a semistructured diagnostic interview and completed paper-and-pencil questionnaires on presentation for treatment. To study the validity of the DSM-IV hierarchical relationship between generalized anxiety disorder and mood disorders, the authors made a diagnosis of modified generalized anxiety disorder for patients with major depressive disorder who met all the criteria for generalized anxiety disorder except for the exclusion criterion. The analyses compared the characteristics of three nonoverlapping groups of patients with DSM-IV major depressive disorder: 1) those with coexisting DSM-IV generalized anxiety disorder, 2) those with coexisting modified generalized anxiety disorder, and 3) those with neither DSM-IV nor modified generalized anxiety disorder. RESULTS: Compared to the depressed patients without generalized anxiety disorder, the depressed patients with DSM-IV and modified generalized anxiety disorder had higher levels of suicidal ideation; poorer social functioning; a greater frequency of other anxiety disorders, eating disorders, and somatoform disorders; higher scores on most subscales of a multidimensional self-report measure of DSM-IV axis I disorders; a greater level of pathological worry; and a higher morbid risk for generalized anxiety disorder in first-degree family members. The two generalized anxiety disorder groups did not differ from each other. CONCLUSIONS: The findings question the validity of the DSM-IV hierarchical relationship between major depressive disorder and generalized anxiety disorder and suggest that the exclusion criterion should be eliminated.
The frequent occurrence of anxiety syndromes in depressed patients has stimulated a debate over the past 20 years regarding the hierarchical relationship between anxiety and depressive disorders (1–5). In DSM-III, anxiety disorders were excluded if they occurred during a depressive episode. However, subsequent research indicated that patients with comorbid anxiety and depression exhibited more severe symptoms, impairment, and subjective distress and a more chronic course than those with “pure” disorders (6–9). These findings suggested that it was more appropriate to make a separate diagnosis of an anxiety disorder for patients with a diagnosis of depression, and the hierarchy was eliminated in DSM-III-R. That is, the hierarchical relationship was eliminated for all anxiety disorders except for generalized anxiety disorder. The validity of the continued hierarchical relationship between generalized anxiety disorder and mood disorders is the subject of the present report.
Generalized anxiety disorder, which was first defined in DSM-III, is characterized by fluctuating levels of uncontrollable worry associated with fatigue, insomnia, muscle tension, poor concentration, and irritability. The DSM-IV symptom inclusion criteria for major depressive disorder and generalized anxiety disorder overlap, with four of six generalized anxiety disorder symptoms (sleep disturbance, difficulty concentrating, restlessness, and fatigue) also constituting criteria for a diagnosis of major depressive disorder. It is, therefore, understandable why both diagnoses would not be made when the symptoms of generalized anxiety disorder occur only during the course of the mood disorder. According to DSM-IV, depressed patients who experience the generalized anxiety disorder syndrome when they are not depressed receive both diagnoses. However, DSM-IV precludes the diagnosis of generalized anxiety disorder for patients who experience generalized anxiety disorder symptoms exclusively during the course of a mood disorder. The question remains whether depressed patients who would otherwise meet the criteria for generalized anxiety disorder, except for the exclusion criterion, resemble or differ from depressed patients who do not experience symptoms suggesting generalized anxiety disorder.
In the present report from the Rhode Island Methods to Improve Diagnostic Assessment and Services (MIDAS) project, we compared demographic, clinical, family history, and psychosocial characteristics among three nonoverlapping groups of patients with a principal diagnosis of major depressive disorder: 1) those with a coexisting DSM-IV generalized anxiety disorder diagnosis, 2) those with a coexisting “modified generalized anxiety disorder” diagnosis (meeting all DSM-IV criteria except the exclusion criterion), and 3) those without generalized anxiety disorder.
Method
Subjects
From the larger sample of psychiatric outpatients evaluated in the MIDAS project, 332 patients with a principal diagnosis of nonbipolar, nonpsychotic DSM-IV major depressive disorder are the subjects of this report. All patients came to the Rhode Island Hospital Department of Psychiatry outpatient practice for treatment. They were evaluated with a semistructured diagnostic interview and completed some paper-and-pencil questionnaires on presentation for treatment. The Rhode Island Hospital institutional review committee approved the research protocol, and all patients provided informed, written consent. Not all patients who came for treatment participated in the study. As described elsewhere, patients who did and did not participate in the study were similar in gender, education, marital status, and scores on self-administered symptom questionnaires (10).
Assessments
We used the January 1995 DSM-IV patient version of the Structured Clinical Interview for DSM-IV (SCID) (11), supplemented with questions from the Schedule for Affective Disorders and Schizophrenia (SADS) (12) assessing the severity of symptoms during the week before the evaluation. An extracted Hamilton Depression Rating Scale score was derived from the SADS ratings by using the algorithm developed by Endicott and colleagues (13). The interview also included items from the SADS on best level of social functioning during the past 5 years, social functioning during adolescence, and the amount of time employed during the past 5 years. The Clinical Global Impression of depression severity (14) was rated for all patients. Trained raters administered the interviews. During the course of the study, joint-interview diagnostic reliability information was collected for 47 patients. For disorders diagnosed in at least two patients by at least one of the raters, the kappa coefficients were 0.91 for major depressive disorder, 0.88 for dysthymic disorder, 0.85 for bipolar disorder, 1.00 for panic disorder, 0.84 for social phobia, 1.00 for obsessive-compulsive disorder (OCD), 0.91 for specific phobia, 0.93 for generalized anxiety disorder, 1.00 for modified generalized anxiety disorder, 0.91 for posttraumatic stress disorder, 0.64 for alcohol abuse/dependence, 0.73 for drug abuse/dependence, 1.00 for any impulse control disorder, and 1.00 for any somatoform disorder.
At the end of each SCID module we included the following question about the reason for seeking treatment: “Was (symptoms of disorder) one of the main reasons you decided to seek treatment now?” If the patient’s answer was no, we asked the following question: “Now that we’ve talked about (symptoms of disorder), would you like your treatment here to address these symptoms?” When asking these questions, the interviewer reviewed the features of the disorder that had just been described so the patient understood to which symptoms the question referred.
During the first year of the MIDAS project, we had observed that many depressed patients had high levels of chronic anxiety characterized by excessive worrying and other features of generalized anxiety disorder, but that they did not receive a diagnosis of generalized anxiety disorder, per DSM-IV, because the symptoms occurred only during the course of a mood disorder. To study the validity of the DSM-IV hierarchical relationship between generalized anxiety disorder and mood disorders, we changed our diagnostic procedure and made a diagnosis of modified generalized anxiety disorder for patients who met all generalized anxiety disorder criteria except the exclusion criterion. The 332 patients included in the present report had all been evaluated with the modified interview.
When scheduling their appointments, patients were told to arrive early to complete two questionnaires—the Psychiatric Diagnostic Screening Questionnaire (15, 16) and the Diagnostic Inventory for Depression (17). Because we were planning to test the instruments’ validity by examining their relationship with psychiatric diagnoses, SCID interviewers were blind to the subjects’ responses on the measures. The Psychiatric Diagnostic Screening Questionnaire is a reliable self-report instrument with concurrent, convergent, and discriminant validity for the assessment of multiple DSM-IV disorders (15, 16). We compared the three groups on the total Psychiatric Diagnostic Screening Questionnaire score, which is an index of the breadth and severity of axis I pathology, as well as on the subscale scores. The Diagnostic Inventory for Depression (unpublished 2002 paper of M. Zimmerman et al.) is a new self-report scale designed to generate a diagnosis of major depressive disorder according to DSM-IV, assess psychosocial impairment related to depression, and evaluate subjective quality of life.
After the SCID interview, patients completed a booklet of questionnaires that included measures of generic health concepts (the Medical Outcomes Study 36-item Short-Form Health Survey [17]) and cognitions common in generalized anxiety (Penn State Worry Questionnaire [18]).
Family history diagnoses were based on information provided by the patient. The interview followed the guide provided in the Family History Research Diagnostic Criteria (19) and assessed the presence or absence of problems with anxiety, mood, substance use, etc., for all first-degree family members. Information about functional impairment, types of treatment, and hospitalizations was also recorded. Morbid risks were calculated by using age-corrected denominators on the basis of Weinberg’s shorter method (20). Thus, relatives older than the age of risk for the particular illness were given a value of 1, those within the age for risk were given a value of 0.5, and those younger than the age of risk were given a value of 0. Limits for the ages of risk were for 11–35 years for generalized anxiety disorder, 25–44 years for major depressive disorder, 25–40 years for panic disorder, 8–18 years for social phobia, 16–35 years for posttraumatic stress disorder, 16–35 years for OCD, 11–30 years for specific phobia, 20–34 years for alcoholism, and 20–34 years for drug use disorder. These ages of risk were based on the distribution of ages at illness onset in the probands. Morbid risks were compared by using the chi-square statistic.
Statistical Analysis
We compared the demographic, family history, and clinical characteristics of three nonoverlapping groups of patients: 1) major depressive disorder patients with DSM-IV generalized anxiety disorder; 2) major depressive disorder patients with modified generalized anxiety disorder; and 3) major depressive disorder patients without DSM-IV generalized anxiety disorder or modified generalized anxiety disorder. One-way analyses of variance were used to compare the three groups on continuously distributed variables. Follow-up pairwise comparisons were conducted only when the three-group analysis was significant. Categorical variables were compared by using the chi-square statistic or by using Fisher’s exact test if the expected value in any cell of a two-by-two table was less than 5.
Results
General Characteristics of Patients
Three hundred thirty-two patients presented with a chief complaint of depression and were given a principal diagnosis of nonbipolar major depressive disorder. The group included 109 (32.8%) men and 223 (67.2%) women who ranged in age from 18 to 76 years (mean=38.7, SD=11.7). More than two-fifths of the subjects were married (N=137, 41.3%); the remainder were single (N=93, 28.0%), divorced (N=58, 17.5%), separated (N=22, 6.6%), widowed (N=5, 1.5%), or living with someone as if in a marital relationship (N=17, 5.1%). About two-thirds (N=223) had a high school degree or equivalency certificate, 8.7% (N=29) had not graduated from high school, and 24.1% (N=80) had graduated from a 4-year college. The group was predominantly white (N=293, 88.3%). The mean Global Assessment of Functioning Scale score of the depressed patients was 50.8 (SD=9.1). More than half the patients had experienced at least one other prior episode of major depressive disorder (N=193, 58.1%), and the median duration of the current episode was 50 weeks.
One-fifth of the patients received a diagnosis of comorbid DSM-IV generalized anxiety disorder (N=68), and 14% (N=48) were designated as having modified generalized anxiety disorder. There were no differences between groups on age, gender, education, or marital status.
Clinical Correlates
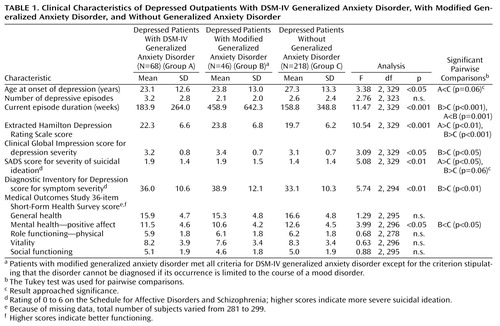
The data in Table 1 show that the depressed patients with modified generalized anxiety disorder were more severely depressed than the group without generalized anxiety disorder on both the interview and the self-report measures of depression severity. Both anxiety disorder groups had higher levels of suicidal ideation, although the difference between the group with modified generalized anxiety disorder and the group without generalized anxiety disorder only approached significance (p=0.06). There was no difference between groups in lifetime history of suicide attempts or psychiatric hospitalization (data available upon request). The only difference between the group with DSM-IV generalized anxiety disorder and the group with modified generalized anxiety disorder was a longer episode duration in the modified generalized anxiety disorder group. This difference was an artifact of the method for diagnosing modified generalized anxiety disorder. The criteria for modified generalized anxiety disorder stipulated that the anxiety symptoms, of at least 6 months’ duration, must occur during the course of the mood disorder; consequently, the depressive episodes must be of at least 6 months’ duration.
A comparison of the three groups on the total number of major depressive disorder criteria met and the frequency of each of the nine individual major depressive disorder criteria found only one significant difference: compared to the patients without generalized anxiety disorder, both generalized anxiety disorder groups were significantly less likely to have experienced appetite disturbance (30.9% of the DSM-IV generalized anxiety disorder group, 34.8% of the modified generalized anxiety disorder group, and 50.9% of the group without generalized anxiety disorder) (χ2=10.5, df=2, p<0.01). Likewise, a comparison of the DSM-IV and modified generalized anxiety disorder groups on the total number of generalized anxiety disorder criteria met and the frequency of the six individual generalized anxiety disorder criteria found only one significant difference: the patients with modified generalized anxiety disorder were more likely to experience concentration problems (97.8% versus 79.4% of the DSM-IV generalized anxiety disorder group) (χ2=8.1, df=1, p<0.01).
More than 90% of the depressed patients with either DSM-IV or modified generalized anxiety disorder indicated that they wanted treatment to address their symptoms of chronic anxiety (91.2% and 97.8%, respectively) (χ2=2.0, df=1, n.s.)
Psychosocial Correlates
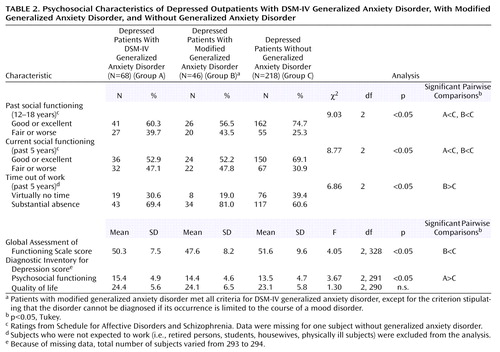
Depressed patients with DSM-IV and modified generalized anxiety disorder had poorer current and adolescent social functioning than the patients without generalized anxiety disorder (Table 2). Compared to the patients without generalized anxiety disorder, the group with modified generalized anxiety disorder was more likely to have missed some time from work during the last 5 years, and their Global Assessment of Functioning Scale scores were significantly lower. There was no difference in subjectively perceived quality of life. In the first stepwise regression analysis, which compared the groups with generalized anxiety disorder and the group without generalized anxiety disorder, current social functioning as measured with the Diagnostic Inventory for Depression was the only significant correlate (F=7.85, df=1, 289, p=0.005). In the second regression analysis, symptom severity as measured by the Hamilton depression scale and episode duration independently were associated with the distinction between modified generalized anxiety disorder and no generalized anxiety disorder (F=11.39, df=2, 218, p<0.001). Because episode duration might be confounded with the modified generalized anxiety disorder diagnosis, we repeated the regression analysis without including episode duration as one of the predictors. In this analysis, symptom severity as measured by the Hamilton depression scale and childhood social functioning were independent predictors (F=7.38, df=2, 218, p=0.001).
Penn State Worry Questionnaire scores, an index of pathological worry, were significantly different across the groups (F=18.7, df=2, 218, p<0.001). Follow-up tests indicated that the total Penn State Worry Questionnaire score was significantly higher in the depressed patients with either DSM-IV or modified generalized anxiety disorder than in those without any generalized anxiety disorder (68.1 and 65.7 versus 55.9). There was no significant difference between the two generalized anxiety disorder groups (p=0.73, Tukey).
Comorbidity as Measured by Interview and Self-Report Measures
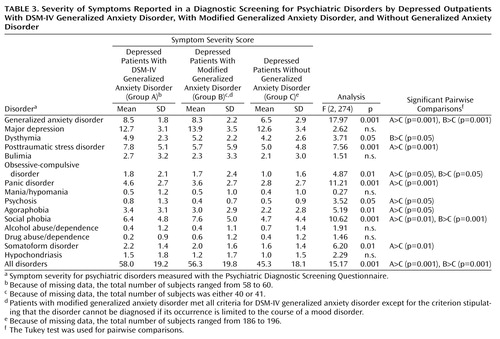
On the total Psychiatric Diagnostic Screening Questionnaire score, an index of the severity and breadth of axis I pathology, both generalized anxiety disorder groups scored significantly higher than the group without generalized anxiety disorder and did not score significantly different from each other (Table 3).
On the SCID, both groups with generalized anxiety disorder received significantly more current axis I disorder diagnoses than the patients without generalized anxiety disorder, and both generalized anxiety disorder groups were twice as likely to have two or more comorbid disorders (Table 4). The patients with DSM-IV generalized anxiety disorder had higher rates of current panic disorder, specific phobia, social phobia, eating disorders, and somatoform disorders than the depressed patients without generalized anxiety disorder, although only the rates for social phobia and any eating disorder were significant in the logistic regression analysis. The patients with modified generalized anxiety disorder were more likely to receive a diagnosis of social phobia and a somatoform disorder, although only the rate of social phobia remained significant in the regression analysis. There were no differences between the DSM-IV and modified generalized anxiety disorder groups.
Family History
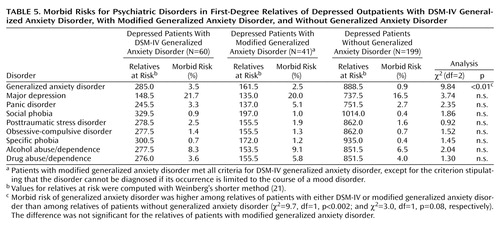
We compared the morbid risk for mood, anxiety, and substance use disorders in the first-degree relatives of the three groups. Family members were considered to have a diagnosis of any of these disorders if they had received treatment for the disorder. Table 5 shows that the only significant difference between groups was in family history of generalized anxiety disorder: the morbid risk of generalized anxiety disorder was higher in both groups of generalized anxiety disorder patients than in the group with no generalized anxiety disorder, although the difference was not significant for the group with modified generalized anxiety disorder (χ2=3.0, df=1, p=0.08). The two generalized anxiety disorder groups did not differ from each other.
Discussion
Depressed outpatients with comorbid DSM-IV generalized anxiety disorder, compared to depressed outpatients without generalized anxiety disorder, had a younger age at illness onset; a greater level of suicidal ideation; poorer social functioning; a greater frequency of other anxiety disorders, eating disorders, and somatoform disorders; higher scores on most subscales of a multidimensional self-report measure of DSM-IV axis I disorders; a greater level of pathological worry; and a higher morbid risk for generalized anxiety disorder in first-degree family members. These findings are consistent with those of other studies (8, 9, 21, 22). The pattern of differences found in our study between the depressed patients with and without DSM-IV generalized anxiety disorder was largely maintained when the group with modified generalized anxiety disorder was compared to the group without generalized anxiety disorder. Moreover, there were few differences between the patients with DSM-IV and with modified generalized anxiety disorder (except for episode duration, which was confounded with the definition of modified generalized anxiety disorder, and the frequency of impaired concentration). These findings question the validity of the DSM-IV hierarchical relationship between major depressive disorder and generalized anxiety disorder and suggest that the modified generalized anxiety disorder group should, in fact, receive a diagnosis of generalized anxiety disorder.
There were more depressed patients with DSM-IV generalized anxiety disorder than with modified generalized anxiety disorder (N=68 versus N=46). Although the majority of the patients who met the DSM-IV inclusion criteria for generalized anxiety disorder met the full set of DSM-IV generalized anxiety disorder criteria, elimination of the exclusion criterion would have markedly increased the frequency of generalized anxiety disorder in the depressed outpatients from 20.5% to 34.3%. With this change in the definition of generalized anxiety disorder, this disorder would become the most frequent comorbid anxiety disorder in depressed patients.
Depressed patients with the symptoms of generalized anxiety disorder almost always wanted treatment to address these symptoms, irrespective of whether the symptoms were or were not limited to the period of depression. We reported elsewhere that there is great variability among the DSM-IV disorders in patients’ desire for treatment and that generalized anxiety disorder is one of four disorders for which most patients want treatment even when it is not the principal reason for seeking treatment (23). One can infer patients’ relatively high level of distress and discomfort caused by their symptoms from their desire to have these symptoms addressed in treatment. From this consumer-oriented perspective, the symptoms of generalized anxiety disorder are among the most bothersome of the axis I disorders.
Because our findings suggest that generalized anxiety disorder should be diagnosed whether or not the anxiety symptoms are limited to the depressive episode, we conducted a post hoc analysis to determine how the classification of the patients with modified generalized anxiety disorder affected the comparisons of depressed patients with and without generalized anxiety disorder. When the DSM-IV hierarchy was followed, and the patients with modified generalized anxiety disorder were included in the group without generalized anxiety disorder, fewer significant differences were found between the groups with and without generalized anxiety disorder than when the patients with modified generalized anxiety disorder were included with the DSM-IV generalized anxiety disorder patients. Specifically, there were no longer differences between the groups with and without generalized anxiety disorder in the Global Assessment of Functioning Scale score, measures of past and current social functioning, the amount of unemployment due to psychiatric symptoms, depression symptom severity as measured by the Diagnostic Inventory for Depression, the level of pathological worry, and the mental health index of the Medical Outcomes Study 36-item Short-Form Health Survey (17). These findings indicate that studies in which the hierarchy between depression and generalized anxiety disorder is suspended are more likely to find differences between depressed patients with and without generalized anxiety disorder than are studies that adhere to the DSM-IV hierarchy.
In the 1960s and 1970s, depressed patients were subtyped according to the presence or absence of anxiety symptoms rather than being given separate diagnoses (24, 25). In the post-DSM-III era, the emphasis has been on making multiple diagnoses; thus, both a mood and anxiety disorder are diagnosed. Disagreement about how best to conceptualize and classify conditions with high levels of both depression and anxiety is reflected by the changes in the hierarchical exclusion rules. In DSM-III, anxiety disorders were excluded if the symptoms occurred only during the course of the mood disorder. Thus, the depression diagnosis was considered valid, whereas the anxiety symptoms were considered an epiphenomenon, or associated feature, of the depressive disorder, and an additional diagnosis was not made when the anxiety symptoms were limited to the same time period as the depressive symptoms. When the anxiety symptoms predated the onset of depression, then multiple disorders could be diagnosed. This hierarchical relationship changed in DSM-III-R, and multiple diagnoses generally were not excluded regardless of the time course of the depressive and anxious symptoms. However, evidence in support of making a separate anxiety disorder diagnosis in the depressed patients included the findings of increased rates of anxiety disorders in family members (22).
What are the treatment and prognostic implications of the presence of a comorbid anxiety disorder in depressed patients? In general, the literature has suggested that comorbid anxiety disorder is associated with poorer outcome (2, 26–31), although negative findings have also been reported (32). This DSM-III-era literature is consistent with studies from the 1960s by Overall, Hollister and colleagues (25, 33) and from the 1970s by Paykel et al. (24, 34), which found that depressed patients with high levels of anxiety had poorer response to tricyclic antidepressants. To our knowledge, no studies have examined the question of whether the treatment of depressed patients with and without comorbid anxiety should differ, although clinical experience and inference from the extant literature suggest that the presence of a comorbid anxiety disorder affects case formulation and treatment planning. For example, pharmacologic treatment planning for depressed patients with a comorbid anxiety disorder could include referral for cognitive behavior therapy for the anxiety disorder. Choice and dosing of pharmacologic agents might also vary. If a selective serotonin reuptake inhibitor is prescribed, dosage titration might be more gradual (35). A recent study found that venlafaxine, but not fluoxetine, was superior to placebo in the treatment of depressed patients with comorbid generalized anxiety disorder (36).
In summary, we found that depressed patients with a full generalized anxiety disorder syndrome that occurs only during the course of a depressive episode, and thus is not diagnosed according to DSM-IV, are indistinguishable in their clinical, psychosocial, family history, and demographic characteristics from depressed patients with the DSM-IV diagnosis of generalized anxiety disorder. Moreover, both groups differ from depressed patients without generalized anxiety disorder. Our findings thus question the validity of the DSM-IV hierarchical relationship between major depressive disorder and generalized anxiety disorder and suggest that the exclusion criterion should be eliminated.
 |
 |
 |
 |
 |
Received Jan. 23, 2002; revision received Sept. 13, 2002; accepted Sept. 27, 2002. From the Department of Psychiatry and Human Behavior, Brown University School of Medicine, Rhode Island Hospital, Providence, R.I. Address reprint requests to Dr. Zimmerman, Department of Psychiatry, Rhode Island Hospital, 235 Plain St., Suite 501, Providence, RI 02905; [email protected] (e-mail). Supported in part by NIMH grant MH-56404.
1. Breslau N, Davis G: Refining DSM-III criteria in major depression: an assessment of the descriptive validity of criterion symptoms. J Affect Disord 1985; 9:199-206Crossref, Medline, Google Scholar
2. Coryell W, Endicott J, Andreasen NC, Keller MB, Clayton PJ, Hirschfeld RM, Scheftner WA, Winokur G: Depression and panic attacks: the significance of overlap as reflected in follow-up and family study data. Am J Psychiatry 1988; 145:293-300Link, Google Scholar
3. Lesser IM, Rubin RT, Pecknold JC, Rifkin A, Swinson RP, Lydiard RB, Burrows GD, Noyes R, DuPont RL: Secondary depression in panic disorder and agoraphobia. Arch Gen Psychiatry 1988; 45:437-443Crossref, Medline, Google Scholar
4. Brown TA, Barlow DH, Liebowitz MR: The empirical basis of generalized anxiety disorder. Am J Psychiatry 1994; 151:1272-1280Link, Google Scholar
5. Kendler K: Major depression and generalised anxiety disorder: same genes, (partly) different environments—revisited. Br J Psychiatry 1996; 30:68-75Google Scholar
6. Breslau N, Davis G: Further evidence on the doubtful validity of generalized anxiety disorder (letter). Psychiatry Res 1985; 16:177-179Crossref, Medline, Google Scholar
7. Grove WM, Andreasen NC, Clayton PJ, Winokur G, Coryell WH: Primary and secondary affective disorders: baseline characteristics of unipolar patients. J Affect Disord 1987; 13:249-257Crossref, Medline, Google Scholar
8. Kessler RC, DuPont RL, Berglund P, Wittchen H-U: Impairment in pure and comorbid generalized anxiety disorder and major depression at 12 months in two national surveys. Am J Psychiatry 1999; 156:1915-1923Link, Google Scholar
9. Wittchen H, Carter R, Pfister H, Montgomery S, Kessler R: Disabilities and quality of life in pure and comorbid generalized anxiety disorder and major depression in a national survey. Int Clin Psychopharmacol 2000; 15:319-328Crossref, Medline, Google Scholar
10. Zimmerman M, Mattia JI: Psychiatric diagnosis in clinical practice: is comorbidity being missed? Compr Psychiatry 1999; 40:182-191Crossref, Medline, Google Scholar
11. First MB, Spitzer RL, Gibbon M, Williams JBW: Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition (SCID-P), version 2. New York, New York State Psychiatric Institute, Biometrics Research, 1995Google Scholar
12. Endicott J, Spitzer RL: A diagnostic interview: the Schedule for Affective Disorders and Schizophrenia. Arch Gen Psychiatry 1978; 35:837-844Crossref, Medline, Google Scholar
13. Endicott J, Cohen J, Nee J, Fleiss JL, Serantakos S: Hamilton Depression Rating Scale: extracted from regular and change versions of the Schedule for Affective Disorders and Schizophrenia. Arch Gen Psychiatry 1981; 38:98-103Crossref, Medline, Google Scholar
14. Guy W (ed): ECDEU Assessment Manual for Psychopharmacology: Publication ADM 76-338. Washington, DC, US Department of Health, Education, and Welfare, 1976, pp 218-222Google Scholar
15. Zimmerman M, Mattia JI: A self-report scale to help make psychiatric diagnoses: the Psychiatric Diagnostic Screening Questionnaire (PDSQ). Arch Gen Psychiatry 2001; 58:787-794Crossref, Medline, Google Scholar
16. Zimmerman M, Mattia JI: The Psychiatric Diagnostic Screening Questionnaire: development, reliability, and validity. Compr Psychiatry 2001; 42:175-189Crossref, Medline, Google Scholar
17. Ware JE Jr, Sherbourne CD: The MOS 36-Item Short-Form Health Survey (SF-36), I: conceptual framework and item selection. Med Care 1992; 30:473-483Crossref, Medline, Google Scholar
18. Meyer TJ, Miller ML, Metzger RL, Borkovec TD: Development and validation of the Penn State Worry Questionnaire. Behav Res Ther 1990; 28:487-495Crossref, Medline, Google Scholar
19. Endicott J, Andreasen N, Spitzer RL: Family History Research Diagnostic Criteria, 3rd ed. New York, New York State Psychiatric Institute, Biometrics Research, 1978Google Scholar
20. Stromgren E: Statistical and genetic population studies within psychiatry: methods and principal results. Actualities Scientifiques et Industrelles, 1101 Congres International de Psychiatrie 1950; 6:155-157Google Scholar
21. Brown C, Schulberg H, Shear M: Phenomenology and severity of major depression and comorbid lifetime anxiety disorders in primary medical care practice. Anxiety 1996; 2:210-218Crossref, Medline, Google Scholar
22. Sherbourne CD, Wells KB: Course of depression in patients with comorbid anxiety disorders. J Affect Disord 1997; 43:245-250Crossref, Medline, Google Scholar
23. Zimmerman M, Mattia JI: Principal and additional DSM-IV disorders for which outpatients seek treatment. Psychiatr Serv 2000; 51:1299-1304Link, Google Scholar
24. Paykel ES: Depressive typologies and response to amitriptyline. Br J Psychiatry 1972; 120:147-156Crossref, Medline, Google Scholar
25. Overall JE, Hollister LE, Johnson M, Pennington V: Nosology of depression and differential response to drugs. JAMA 1965; 195:946-948Crossref, Google Scholar
26. VanValkenburg C, Akiskal HS, Puzantian V, Rosenthal T: Anxious depressions: clinical, family history, and naturalistic outcome—comparisons with panic and major depressive disorders. J Affect Disord 1984; 6:67-82Crossref, Medline, Google Scholar
27. Grunhaus L: Clinical and psychobiological characteristics of simultaneous panic disorder and major depression. Am J Psychiatry 1988; 145:1214-1221Link, Google Scholar
28. Grunhaus L, Harel Y, Krugler T, Pande A, Haskett R: Major depressive disorder and panic disorder. Clin Neuropharmacol 1988; 11:454-461Crossref, Medline, Google Scholar
29. Brown TA, Barlow DH: Comorbidity among anxiety disorders: implications for treatment and DSM-IV. J Consult Clin Psychol 1992; 6:835-844Crossref, Google Scholar
30. Gaynes BN, Magruder KM, Burns BJ, Wagner HR, Yarnall KSH, Broadhead WE: Does a coexisting anxiety disorder predict persistence of depressive illness in primary care patients with major depression? Gen Hosp Psychiatry 1999; 21:158-167Crossref, Medline, Google Scholar
31. Brown C, Schulberg HC, Prigerson HG: Factors associated with symptomatic improvement and recovery from major depression in primary care patients. Gen Hosp Psychiatry 2000; 22:242-250Crossref, Medline, Google Scholar
32. Petersen T, Gordon J, Kant A, Fava M, Rosenbaum J, Nierenberg A: Treatment resistant depression and axis I co-morbidity. Psychol Med 2001; 31:1223-1229Crossref, Medline, Google Scholar
33. Hollister LE, Overall JE, Shelton J, Pennington V, Kimbell I, Johnson M: Drug therapy of depression: amitriptyline, perphenazine, and their combination in different syndromes. Arch Gen Psychiatry 1967; 17:486-493Crossref, Medline, Google Scholar
34. Paykel ES, Prusoff BA, Klerman GL, Haskell D, DiMascio A: Clinical response to amitriptyline among depressed women. J Nerv Ment Dis 1973; 156:149-165Crossref, Medline, Google Scholar
35. Gorman JM, Liebowitz MR, Fyer AJ, Goetz D, Campeas D, Fyer MR, Davies SO, Klein DF: An open trial of fluoxetine in the treatment of panic attacks. J Clin Psychopharmacol 1987; 7:329-332Crossref, Medline, Google Scholar
36. Silverstone P, Salina E: Efficacy of venlafaxine extended release in patients with major depressive disorder and comorbid generalized anxiety disorder. J Clin Psychiatry 2001; 62:523-529Crossref, Medline, Google Scholar



