Family Functioning and Peer Affiliation in Children of Fathers With Antisocial Personality Disorder and Substance Dependence: Associations With Problem Behaviors
Abstract
OBJECTIVE: Family functioning and peer influences are theoretically linked to child psychopathology. This study quantified the functional status of families with fathers with substance dependence with or without comorbid antisocial personality disorder and evaluated the peer environments of preadolescent offspring. The authors examined associations between the child’s psychopathology, paternal substance dependence/antisocial personality disorder status, and measures of family and peer environments. METHOD: Families with the presence or absence of paternal substance dependence were subdivided into those with and without paternal antisocial personality disorder. Grouped families were contrasted on measures of family functioning, the child’s peer affiliation, and the child’s problem behaviors. Regression analysis determined the influence of these factors on the child’s psychopathology. RESULTS: Families with paternal substance dependence functioned worse than normal comparison families. However, families with paternal substance dependence and antisocial personality disorder (N=34) did not differ markedly from those with substance dependence without antisocial personality disorder (N=84). The children of fathers with both substance dependence and antisocial personality disorder had greater affiliation with deviant peers than those with substance dependence without antisocial personality disorder and comparison families (N=104). CONCLUSIONS: Children of fathers with substance dependence and antisocial personality disorder demonstrated higher externalizing and internalizing psychopathology than those with substance dependence but not antisocial personality disorder and those without either condition. Paternal substance dependence/antisocial personality disorder status and the child’s affiliation with deviant peers were most robustly associated with the child’s psychopathology. Research is needed to develop interventions that effectively address parental risk and healthy peer relations.
Various studies have examined the specific psychosocial roles of intrafamilial factors in the etiology of drug use and associated problems in offspring. For example, Kandel and colleagues (1) demonstrated the importance of parental substance use behavior and parent-child relations in predicting drug use in offspring. The salience of these factors was also confirmed in several later studies (e.g., Labouvie et al. [2]). Brook and colleagues (3–5) evaluated theoretically relevant deficiencies in parent-child relations, such as low parental affection, low “child-centeredness,” low involvement with children, and conflictual relationships and demonstrated their impact on substance use behavior among offspring. Of importance, parental antisociality was found to predict drug use behavior, while prosocial parental behavior (i.e., conventionality) was associated with resilience. In adopted children, familial environmental factors such as divorce and the presence of psychiatric disturbance in the adoptive family have been found to be associated with a greater risk for drug abuse (6). This research is consistent with the substantial literature supporting the observation that children with behavior problems tend to live in homes that are problematic, deviant, or dysfunctional (see review by Rutter [7]). Several studies have shown that problematic parenting behavior is characteristic of families with substance abuse (e.g., Hawkins and colleagues [8]).
The process model of family functioning (9) proposes that the overriding goal of the family is the successful achievement of basic developmental and crisis tasks that provide for the continued development of individual family members in a secure, cohesive, and effective environment. Successful accomplishment of these tasks requires the assumption of appropriate roles, engagement in effective communication, and appropriate expression of affect among family members. Family members must be emotionally involved with each other and be able to influence each other’s behavior in a consistent and productive fashion. All of this occurs against a background of cultural norms and values that the family shares. Theoretically, children of substance-dependent parents are at a high risk for subsequent substance abuse, not only because of the transmission of some as-yet-unidentified heritable influence, but also because they grow up in dysfunctional families that negatively affect their capacity for normal development.
Patterson and colleagues (10, 11) are proponents of a developmental paradigm of antisociality that posits that adolescent and adult dyssocial behavior is a consequence of poor parental family management practices interacting with the child’s aggressive and oppositional behavior. Deficits in family functioning, such as harsh and inconsistent parent-child interactions, high levels of parent-child coercion, and poor parental monitoring result in a child’s greater affiliation with deviant peers, ultimately placing the child on a developmental trajectory of deviancy (12). Thus, the child’s dispositional characteristics interact with the functional status of the family and the availability of deviant peers to increase the developmental risk for delinquency, antisociality, and problem behaviors, including the abuse of drugs.
In this report, we characterize the functional status of families and the magnitude of delinquency and prosocial behavior (i.e., conventionality) in the peer environment among three groups of preadolescent children hypothesized to be at increasing levels of familial risk for later antisociality and substance abuse. Specifically, these are children of fathers with antisocial personality disorder and substance dependence and children of fathers with substance dependence but without antisocial personality disorder; we also included a comparison group of children of fathers without either condition. We have previously reported greater levels of externalizing (i.e., conduct problems) and internalizing (i.e., anxiety and depression) behavior problems found among children of fathers with antisocial personality disorder and substance dependence than among children in the other two groups (13). We now examine the associations between these problem behaviors and indicators of family functioning and the peer environment. The purpose is to determine the relative influence of paternal substance dependence/antisocial personality disorder status, family functioning, and peers on problem behaviors for children at this age. The results may be informative in directing prevention interventions targeting this preadolescent group.
Method
Subjects
These analyses were conducted on an initial group of preadolescent boys (N=181; mean age=10.92 years, SD=0.91) and girls (N=41; mean age=10.98 years, SD=0.96) ascertained by the Center for Education and Drug Abuse Research at the University of Pittsburgh on the basis of the presence or absence of a lifetime substance dependence diagnosis (excluding nicotine dependence) in the biological father of the child and having complete data in the areas under investigation. The core protocol for this center has resulted in numerous research reports. Recruitment sources and procedures, inclusionary and exclusionary criteria, and assessment procedures are described in detail elsewhere (14). The purpose and nature of the research procedures and risks as well as benefits were explained in detail to all participants in this study before we obtained written documentation of informed consent from the adult participants. All minor children in this project provided written documentation of their assent to participate. The informed consent procedures and consent and assent forms were approved by the institutional review board of the University of Pittsburgh and are reviewed annually.
Among the boys, 28 had fathers who met lifetime diagnostic criteria for substance dependence and antisocial personality disorder. There were 98 boys whose fathers met lifetime diagnostic criteria for substance dependence in the absence of antisocial personality disorder. In addition, 96 boys had fathers who did not meet lifetime diagnostic criteria for either substance dependence or antisocial personality disorder.
Among the girls, six had fathers who met diagnostic criteria for both substance dependence and antisocial personality disorder. There were 15 girls whose fathers met lifetime diagnostic criteria for substance dependence without antisocial personality disorder. There were 20 girls whose fathers did not meet diagnostic criteria for substance dependence or antisocial personality disorder.
Age, ethnic background, grade in school, and household socioeconomic status of the subjects are displayed according to study group in Table 1. It is noteworthy that the children of fathers with both substance dependence and antisocial personality disorder and those with substance dependence but without antisocial personality disorder came from families with significantly lower socioeconomic status than did the children of fathers without either condition. This observation is consistent with the research of others documenting higher rates of substance abuse and antisocial personality disorders among individuals of lower social status (15).
Measures
Lifetime psychiatric diagnoses were made according to DSM-III-R criteria. (This research was initiated before the availability of DSM-IV.) As described in detail elsewhere (14), the index sons and daughters and their mothers and fathers were all evaluated by structured clinical psychiatric interviews to determine substance dependence and psychiatric status. Parents were administered the Structured Clinical Interview for DSM-III-R Personality Disorders (SCID-II) (16). For the sons and daughters, one parent—typically the mother—was administered an expanded version of the Schedule for Affective Disorders and Schizophrenia for School-Age Children—Epidemiologic Version (17) concerning the index child. The modification of the interview provided additional alcohol and drug use, abuse, and dependence items. The prevalence of psychiatric disorders among these children was previously reported (13).
Antisocial personality disorder diagnoses were assessed through administration of the SCID-II Personality Disorders Questionnaire (16); positive endorsements were confirmed by interview. This questionnaire includes retrospective symptoms for conduct disorder, since onset before age 15 is a prerequisite for antisocial personality disorder under DSM-IIII-R criteria. As with other diagnoses, antisocial personality disorder was determined through the consensus diagnostic process.
Interviews were administered by graduate-level clinicians and discussed in a diagnostic consensus conference with two psychologists or psychiatrists, the interviewers, and the evaluation coordinator. The consensus team reviewed all available information gathered in the assessment protocol, as well as psychiatric treatment records and teacher reports, when available. Psychiatric diagnoses were then determined by the “best-estimate” diagnostic procedure (18).
The mothers and teachers of the study subjects each independently completed appropriate versions of the Child Behavior Checklist (19), reporting on the index child. This validated instrument provides information regarding internalizing and externalizing behavior, total problem behaviors, social competence, and psychopathology. Although the parent and teacher versions of the Child Behavior Checklist are not analogous in their primary scale structure, they both provide comparable summary scales for internalizing and externalizing problem behaviors. Internalizing problems represent behavioral syndromes described by scale scores for withdrawal, somatic complaints, and anxiety or depression. Externalizing problems are derived from scale scores for delinquent and aggressive behavior.
There is controversy as to the use of different informants on child problem behaviors on the basis of the low correlations observed between informants (e.g., teachers and parents) (20). One potential approach to this problem involves combining mother and teacher scores as two important sources of reporting on the child’s behavior (21). This method is also the least disruptive to the distributional properties of the individual scores. Therefore, the combined mother-teacher problem-behavior scores were used as measures of the child’s internalizing and externalizing psychopathology. We had previously reported significant between-group differences in both externalizing and internalizing problem behaviors, such that scores for children of fathers with substance dependence and antisocial personality disorder were significantly greater than the scores for children of fathers without either condition for both internalizing and externalizing problem behaviors. Contrasts between the children of fathers with substance dependence with or without antisocial personality disorder were also significantly different for internalizing and externalizing problem behaviors. However, scores for children of fathers with substance dependence without antisocial personality disorder were not found to be significantly different from scores for children of fathers without either condition (13). The data presented here are from a representative subset of that original study group. Essentially, all of the trends in Child Behavior Checklist scores that were originally reported are evident here.
The Family Assessment Measure, version III (22), is a self-report instrument that provides quantitative indices of family functioning based on a process model (22). The Family Assessment Measure provides a general scale that focuses on the family as a system. Scale scores are obtained for an individual’s perception of the family’s 1) task accomplishment, 2) role performance, 3) communication, 4) affective expression, 5) affective involvement, 6) control, 7) values and norms, and also 8) an overall rating that provides an aggregate assessment of family functioning. Raw scores are converted into T scores, such that each subscale has a mean of 50 and a standard deviation of 10 with data generated by its administration by the test authors to a group of normal families. Higher scores indicate greater problems in a given domain. This instrument has been demonstrated to have good internal consistency and validity (23). Since families were ascertained in this study on the basis of the father’s substance use disorder and antisociality, we employed the mother’s assessment of the functional state of the family for our analyses in order to minimize any potential confounds due to rater bias as a consequence of psychopathology.
The peer delinquency scale of the Pittsburgh Youth Study Interview (24) comprises 15 questions on a 5-point scale concerning the number of friends of the subject that have engaged in a variety of antisocial and delinquent behaviors over the past 6 months. These behaviors range from skipping school without an excuse, to using weapons, to using force to commit robbery. Higher scores indicate that more friends were engaged in these behaviors, while the lowest score indicates the complete absence of any friends involved in these delinquent acts. For the purpose of these analyses, scale scores were summed for each subject, thereby reflecting the overall degree of exposure to peers engaged in delinquent and antisocial behaviors.
The scale on the Pittsburgh Youth Study Interview regarding conventional activities of friends (24) comprises eight questions concerning the number of friends that engaged in prosocial (i.e., conventional) activities during the past 6 months. These behaviors range from obeying school rules to participating in religious activities. Higher scores indicate that more friends engage in these conventional behaviors, and the lowest score reflects the complete absence of any friends involved in these prosocial and traditional activities. Scale scores were summed for each subject, thereby reflecting the overall degree of exposure to peers engaged in these conventional behaviors.
Statistical Analysis
Because of the small number of girls in the group of children whose fathers had both substance dependence and antisocial personality disorder and the lack of significant sex differences, data for boys and girls were combined in these analyses. Significant skewness was observed for scores on both the Child Behavior Checklist internalizing and externalizing problem-behavior scales. Consequently, these continuous data were transformed into more normally distributed variables by using a natural logarithm transformation. Scores regarding peer delinquency and conventional activities of friends were standardized by using z scores. Multivariate analysis of variance (MANOVA) was employed to examine differences in ratings for the Family Assessment Measure subscales, peer delinquency, the Child Behavior Checklist, and conventional activities of friends among family groups in which the father had substance dependence with or without antisocial personality disorder or neither condition. (Listwise deletion of patients with any missing data yielded the final group sizes.) Multivariate analyses were followed by post hoc multiple comparison testing with Tukey’s honestly significant difference test. Mean scores by group, univariate F statistics, significance levels, and significant post hoc comparisons are displayed in Table 2.
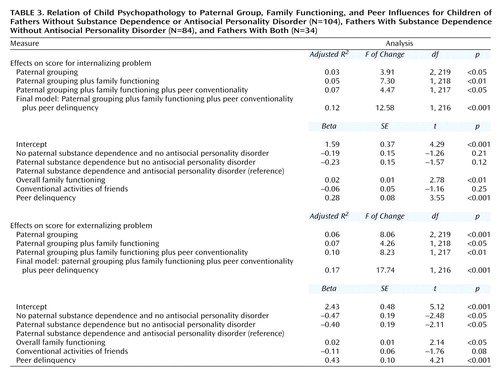
Linear regression models were used to assess the extent to which the presence or absence of paternal antisocial personality disorder and drug dependence, the overall family environment, and measures of peer environment explained the variance in scores for problem behaviors (internalizing and externalizing). Because our interest was primarily on the effects of parental substance abuse phenotypes, this variable was entered first into all regressions, followed by entry of the overall score on the Family Assessment Measure as a summary indicator of family functioning, and, finally, by the scores for conventional activities of friends and peer delinquency as indicators of peer environments. The contributions of each block in explaining responses were measured by F change values if the significance level of 0.05 was attained. The interpretation of the individual variables was on the basis of the alpha coefficients from the final model. The results of these analyses are displayed in Table 3.
Results
The effects of paternal substance dependence and antisocial personality disorder on the child’s internalizing and externalizing problem-behavior scores, measures of family functioning, and indicators of peer environment were simultaneously evaluated by using MANOVA. The effects of paternal status grouping on these measures were found to be significant (Pillai’s trace=0.24, F=2.83, df=22, 448, p<0.001), with significant between-group effects found for the indicators. Post hoc multiple comparison testing was performed with Tukey’s honestly significant difference test.
As shown in Table 2, families with paternal substance dependence in general functioned significantly worse (had higher scores) than those without paternal substance dependence for task accomplishment, role performance, communication, affective expression, and overall functioning. However, families with paternal substance dependence with and without antisocial personality disorder did not differ significantly from each other on average. The proportions of families with T scores of overall functioning of 60 or more were 4.8% (N=5) for the families with no paternal substance dependence and no antisocial personality disorder, 13.1% (N=11) for those with substance dependence without antisocial personality disorder, and 20.6% (N=7) for those with substance dependence and antisocial personality disorder (χ2=7.96, df=2, p<0.05). For affective involvement and control, the average scores for children of fathers with substance dependence and antisocial personality disorder were found to differ significantly from scores for the children of fathers without either condition. However, scores for the children of fathers with substance dependence without antisocial personality disorder were not found to be significantly different from either of the other two groups after use of post hoc tests.
In terms of the scale measuring the conventional activities of friends, the children of fathers with antisocial personality disorder and substance dependence had significantly lower scores reflecting peer conventionality than did the children of fathers without either condition. The children in families with substance dependence but not antisocial personality disorder did not differ significantly from either those without paternal substance dependence or antisocial personality disorder or those with both substance dependence and antisocial personality disorder in the degree of conventionality among their peers. Mean z scores by group are displayed in Table 2.
The peer delinquency scale demonstrated an ordering of the magnitude of delinquency among peers, such that the children of fathers with antisocial personality disorder and substance dependence scored the highest, followed by the children of fathers with substance dependence without antisocial personality disorder, who scored significantly higher than the children of fathers without either condition. Mean z scores by group are displayed in Table 2.
Consistent with our previous report (13), the children of fathers with antisocial personality disorder and substance dependence scored significantly higher than those with substance dependence without antisocial personality disorder and those without either condition on combined scores for the mother-teacher Child Behavior Checklist scale, independently for both internalizing and externalizing problem behaviors. However, scores for the children of fathers with substance dependence without antisocial personality disorder and those without either condition did not differ from each other. The mean scores are displayed in Table 2.
Initially, the effects of interactions among the predictor variables were examined; however, none was found to be significant for either internalizing or externalizing problem behaviors. Consequently, we proceeded to a main effects model. Here, we included all paternal, family, and peer variables and used type 1 sums of squares, since we were interested in the extent to which fit is improved by the addition of covariates. Once a final model was determined, the significance, magnitude, and direction of the effects of paternal, family, and peer variables on problem-behavior scores were estimated by using the group with substance dependence plus antisocial personality disorder as a reference.
For the child’s scores on internalizing problems, the best explanatory model included the paternal substance dependence/antisocial personality disorder variable, the overall family functioning variable, and both the conventional activities of friends and peer delinquency variables. Jointly, these explained about 12% of the variance in internalizing problem-behavior scores. Examination of the parameter estimates for this model revealed that the group without paternal substance dependence or antisocial personality disorder was found to score 0.19 T units lower on internalizing problem scores than the group with both paternal substance dependence and antisocial personality disorder. The estimate for the group with paternal substance dependence without antisocial personality disorder was found to score –0.23 T units lower than the group with both paternal conditions, although with the inclusion of family and peer covariates, these effects were not statistically significant. Given the effects of paternal status, an increase in score for internalizing problems (0.28 T units) was found to be associated with the peer delinquency covariate, and a significant but negligible increase (0.02 T units) was found to be associated with the overall family functioning covariate. It is noteworthy that there was a modest correlation (r=–0.3, p<0.05) between scores for the conventional activities of friends and peer delinquency. When both variables are used in the regression, the effects of peer delinquency are sufficiently strong that the measure for conventional activities of friends becomes nonsignificant.
For the child’s externalizing problem-behavior scores, the best explanatory model included the paternal substance dependence/antisocial personality disorder variable, the overall family functioning variable, and both variables for the conventional activities of friends and peer delinquency. Jointly, these explained about 17% of the variance in externalizing problem-behavior scores. Examination of the parameter estimates for this model revealed that the group without either paternal condition was found to score 0.47 T units lower on externalizing problem behavior than the group with both paternal substance dependence and antisocial personality disorder. The estimate for the group with paternal substance dependence without antisocial personality disorder was found to score 0.40 T units lower than the group with both paternal substance dependence and antisocial personality disorder. These estimates were significant. Given paternal status, an increase in score on externalizing problem behavior was found to be associated with the peer delinquency covariate (0.43 T units), and a significant but negligible increase was found for the overall family functioning covariate (0.02 T units). Again, because of the modest correlation between the variables for conventional activities of friends and peer delinquency and the strength of the effect of peer delinquency when both variables are used in the regression, the effect of the measure for conventional activities of friends becomes nonsignificant.
Discussion
The results of this investigation confirm that family functioning is comparatively worse in families in which there is parental substance dependence (e.g., references 1, 2, 7–9). Of importance, all paternal subgroups had average T scores that fell within the “normal” range on the Family Assessment Measure scales. Thus, we cannot confirm the hypothesis that families with paternal substance abuse, on average, are technically dysfunctional. While our a priori hypothesis was that families with paternal antisocial personality disorder would be more dysfunctional, the results did not support this contention. Families with both substance dependence and antisocial personality disorder did not differ significantly from families with substance dependence without antisocial personality disorder on key functional dimensions of family task accomplishment, role performance, communication, and affective expression. However, for measures of affective involvement and control, families with paternal substance dependence and antisocial personality disorder were found to score significantly worse than families with paternal substance dependence without antisocial personality disorder, while scores for families with paternal substance dependence without antisocial personality disorder were not found to be significantly different from either group.
In terms of the peer environment, it was anticipated that the children of fathers with substance dependence and antisocial personality disorder would have fewer conventional friends and more delinquent peers. The antisocial peer environment is consistent with Patterson and colleagues’ developmental theory of the etiology of antisociality (10, 11). Specifically, they suggest that mainstream peers reject antisocial children, who tend to drift toward an association with each other in order to form groups that promote antisocial behavior (25). Thus, there is an enhanced affiliation with antisocial peers that further promotes deviancy and places the child on a more extreme developmental trajectory toward an adverse outcome. This affiliation with deviant peers is also thought to be developmentally preceded by family dysfunction in the form of harsh and inconsistent discipline, little positive parent involvement with the child, and poor monitoring and supervision of the child’s activities (10, 26). Of interest, in this study, we found that affiliation with delinquent peers was a powerful predictor of internalizing and externalizing problem-behavior scores, while having friends who engage in more conventional and prosocial activities functioned as a less robust buffer against psychopathology.
Our regression analysis suggests a convergence of adverse factors that is consistent with Patterson’s theory of the development of antisocial problem behaviors (10, 11). A less functional family environment, a deviant peer environment, and paternal antisociality linearly interact to account for a greater degree of psychopathology in the child. However, for internalizing problems, these relationships explained about 12% of the variance, while for externalizing problems, the model explained about 17% of the variance. Thus, a substantial degree of the phenotypic variability in these target problems remains unexplained by this analysis. Perhaps other genetically mediated factors account for some proportion of the unexplained variability; however, the design of this study does not permit the disentanglement of genetic from environmental influences.
There are several significant limitations of this study. A fundamental limitation is its cross-sectional nature. While associations between child behavior, family functioning, and the peer environment can be ascertained, direct causal associations cannot be drawn from these analyses. Thus, a developmental interpretation cannot be drawn. Furthermore, the complex reciprocity of child behavior, family functioning, and peer affiliations cannot be demonstrated in this report.
An additional limitation to this research involves our inability to address the issue of sex differences in the relationships between child behavior, peers, and family. As noted in our previous report (13), the small number of girls in the group with both substance dependence and antisocial personality disorder and the focus on paternal—but not maternal—substance dependence as an ascertainment criterion precludes any investigation of sex-specific effects of transmission on psychopathology in offspring. Western sex roles result in mothers spending substantially more time with their children than do fathers. The importance of maternal attachment is well recognized. Consequently, maternal influences may be more important than paternal influences in the genesis of the shared environment of the family. Additionally, same-sex modeling of behavior and the phenomenon of genetic imprinting may contribute to sex heterogeneity in the transmission of psychopathology from parents to children. It is regrettable that the data are not informative on any of these issues.
The role of social status and its impact on parent, child, and their respective environments also remain problematic. As we previously noted, lower socioeconomic status is a priori associated with substance use and antisocial disorders (5) and is therefore confounded with our paternal substance dependence/antisocial personality disorder groupings. Socioeconomic deprivation, social-strata-specific cultural norms, and adverse living environments could contribute significantly to a child’s developmental deviation and risk for later social dysfunction. Had we used socioeconomic status as a covariate in our analyses, it might have attenuated or obscured the effects produced by paternal substance abuse and antisociality status on family, child behaviors, and peer environments. In fact, we have examined these data with and without socioeconomic status as a covariate (data not shown), and although its inclusion alters the magnitude of some effects, it essentially leaves the basic conclusions unchanged.
Children of fathers with antisocial personality disorder and substance dependence clearly have greater externalizing and internalizing problem behaviors than children of fathers with substance dependence without antisocial personality disorder and children of fathers without either condition. From a developmental perspective, these children are at substantial risk for adolescent and adult antisociality and substance dependence. Thus, these children of fathers with antisocial personality disorder and substance dependence represent a group of well-defined, high-risk children who should be the vigorous target of prevention interventions. However, the nature and timing of etiologically appropriate interventions remain unclear. If the conceptualization of Patterson and colleagues (10, 11) is correct, then the appropriate timing for an efficacious family intervention would be when the child first manifests problem behaviors and temperamental difficulties. Enhancing family functioning at this time point might impede the development of a coercive relationship between parent and child, rejection by normal peers, affiliation with deviant peers, and a life course trajectory of deviancy. Among children in the current 10–12-year-old age group, the strongest association with problem behaviors is the child’s affiliation with deviant peers. By this age, these children may already be on an adverse life trajectory. Despite the application of a host of interventions designed to improve social skills and social information processing, reductions in actual aggressiveness or improvements in the social status of high-risk children has been largely resistant to change (27). More research is clearly needed to develop and evaluate ontogenetically appropriate interventions that target a child’s problematic behaviors, the parents’ ability to cope and discipline appropriately, and the child’s acquisition of social peers.
 |
 |
 |
Received July 10, 2000; revisions received May 1 and Sept. 14, 2001; accepted Nov. 15, 2001. From the Center for Education and Drug Abuse Research (a consortium of the University of Pittsburgh and St. Francis Medical Center), Pittsburgh; the Treatment Research Center, University of Pennsylvania; the Department of Nursing, University of Delaware, Newark; and the Department of Psychiatry, Temple University School of Medicine, Philadelphia. Address reprint requests to Dr. Moss, Treatment Research Center, University of Pennsylvania Health System, 3900 Chestnut St., Philadelphia, PA 19104-6178; [email protected] (e-mail). Supported in part by a grant from the National Institute on Drug Abuse (DA-05605) and a Senior Scientist Award to Dr. Moss (DA-00308).
1. Kandel D, Kessler R, Margulies R: Antecedents of adolescent initiation into stages of drug use: a developmental analysis. J Youth Adolesc 1978; 7:13-40Crossref, Medline, Google Scholar
2. Labouvie EW, Pandina RJ, Johnson V: Developmental trajectories of substance use in adolescence: differences and predictors. Int J Behavioral Development 1991; 14:305-328Crossref, Google Scholar
3. Brook JS, Lukoff IF, Whiteman M: Family socialization and adolescent personality and their association with adolescent use of marijuana. J Genet Psychol 1978; 133:261-271Crossref, Medline, Google Scholar
4. Brook J, Whiteman M, Gordon A: Stages of drug use in adolescence: personality, peer and family correlates. Dev Psychol 1983; 19:269-277Crossref, Google Scholar
5. Brook J, Whiteman M, Balka E, Cohen P: Parent drug use, parent personality, and parenting. J Genet Psychol 1995; 156:137-151Crossref, Medline, Google Scholar
6. Cadoret R, Troughton E, O’Gorman T, Heywood E: An adoption study of genetic and environmental factors in drug abuse. Arch Gen Psychiatry 1986; 43:1131-1136Crossref, Medline, Google Scholar
7. Rutter M: Family and social influences on behavioral development. J Child Psychol Psychiatry 1985; 26:349-368Crossref, Medline, Google Scholar
8. Hawkins D, Lishner D, Catalano R, Howard W: Childhood predictors of adolescent substance abuse: toward empirically grounded theory. J Children in Contemporary Society 1985; 18:11-48Crossref, Google Scholar
9. Steinhauer P, Santa-Barbara J, Skinner H: The process model of family functioning. Can J Psychiatry 1984; 29:77-88Crossref, Medline, Google Scholar
10. Patterson G, DeBaryshe B, Ramsey E: A developmental perspective on antisocial behavior. Am Psychol 1989; 44:329-335Crossref, Medline, Google Scholar
11. Dishion T, Patterson G, Stoolmiller M, Skinner M: Family, school and behavioral antecedents to early adolescent involvement with antisocial peers. Dev Psychol 1991; 27:172-180Crossref, Google Scholar
12. Vuchinich S, Bank L, Patterson G: Parenting, peers, and the stability of antisocial behavior in preadolescent boys. Dev Psychol 1992; 28:510-521Crossref, Google Scholar
13. Moss HB, Baron DA, Hardie TL, Vanyukov MM: Preadolescent children of substance-dependent fathers with antisocial personality disorder: psychiatric disorders and problem behaviors. Am J Addict 2001; 10:269-278Crossref, Medline, Google Scholar
14. Clark D, Moss HB, Kirisci L, Mezzich A, Ott P: Psychopathology in preadolescent sons of fathers with substance use disorders. J Am Acad Child Adolesc Psychiatry 1997; 36:495-502Crossref, Medline, Google Scholar
15. Dohrenwend B, Levav I, Shrout PE, Schwartz S, Naveh G, Link BG, Skodol AE, Stueve A: Socioeconomic status and psychiatric disorders: the causation-selection issue. Science 1992; 255:946-952Crossref, Medline, Google Scholar
16. Spitzer RL, Williams JBW, Gibbon M: Structured Clinical Interview for DSM-III-R Personality Disorders (SCID-II). New York, New York State Psychiatric Institute, Biometrics Research, 1987Google Scholar
17. Orvaschel H, Puig-Antich J, Chambers WJ, Tabrizi MA, Johnson R: Retrospective assessment of prepubertal major depression with the Kiddie-SADS-E. J Am Acad Child Psychiatry 1982; 21:4:392-397Google Scholar
18. Leckman JF, Scholomskas D, Thompson WD, Belanger A, Weissman MM: Best estimate of lifetime psychiatric diagnosis: a methodological study. Arch Gen Psychiatry 1982; 39:879-883Crossref, Medline, Google Scholar
19. Achenbach TM, Edelbrock C: Manual for the Child Behavior Checklist and Revised Child Behavior Profile. Burlington, University of Vermont, Department of Psychiatry, 1983Google Scholar
20. Achenbach T, McConaughy SH, Howell CT: Child/adolescent behavorial and emotional problems: implications of cross-informant correlation for situational specificity. Psychol Bull 1987; 101:213-232Crossref, Medline, Google Scholar
21. Mattison RE, Bagnato SJ, Strickler E: Diagnostic importance of combined mother and teacher ratings on the revised behavior problem checklist. J Abnorm Child Psychol 1987; 15:617-628Crossref, Medline, Google Scholar
22. Skinner H, Steinhauer P, Santa-Barbara J: The Family Assessment Measure. Can J Community Ment Health 1983; 2:91-105Crossref, Google Scholar
23. Halvorsen J: Self-report family assessment instruments: an evaluative review. Fam Pract Res J 1991; 11:21-55Medline, Google Scholar
24. Loeber R, Farrington DP, Stouthamer-Loeber M, Van Kammen WB: Antisocial Behavior and Mental Health Problems: Explanatory Factors in Childhood and Adolescence. Mahwah, NJ, Lawrence Erlbaum Associates, 1998Google Scholar
25. Dishion T: The family ecology of boys’ peer relations in middle childhood. Child Dev 1990; 61:874-892Crossref, Medline, Google Scholar
26. Loeber R, Dishion T: Early predictors of male delinquency: a review. Psychol Bull 1983; 94:68-99Crossref, Medline, Google Scholar
27. Reid J: Prevention of conduct disorder before and after school entry: relating interventions to developmental findings. Dev Psychopathol 1993; 5:243-262Crossref, Google Scholar



