A Reevaluation of the Exclusion Criteria Used in Antidepressant Efficacy Trials
Abstract
OBJECTIVE: Antidepressant efficacy trials use multiple exclusion criteria that are intended primarily to maximize differences between the drug and placebo. These exclusion criteria were implemented prior to having undergone rigorous testing, however, and it is unclear whether they accomplish their intended goal. The authors review the current state of knowledge about treatment response rates in individuals who are typically excluded from antidepressant efficacy trials. METHOD: After reviewing 31 antidepressant efficacy trials published between 1994 and 1998, the authors identified 10 commonly used exclusion criteria. A computerized MEDLINE search and a manual search were used to identify studies evaluating the efficacy of antidepressant medications in populations of subjects typically excluded from antidepressant efficacy trials. RESULTS: Three exclusion criteria—short episode duration, mild severity of illness, and positive response during the placebo lead-in phase—are used primarily to reduce placebo response rates. Preliminary evidence suggests that, of those three criteria, only a short episode duration has been associated with less robust differences between drug and placebo response rates. The seven other exclusion criteria, including various psychiatric comorbidities, long duration of illness, medical comorbidity, and prior nonresponse to treatment, are used because individuals who meet those criteria are believed to have lower response rates to somatic therapy. Although such individuals are often found to have lower response rates to somatic therapy, they also appear to have lower response rates to placebo, and there is little evidence to suggest that drug-placebo differences are any less robust in these individuals. CONCLUSIONS: Many of the standard exclusion criteria currently used in antidepressant efficacy trials may not be achieving their intended goal of maximizing drug-placebo differences. The practice of excluding subjects with particular clinical profiles, which greatly reduces the generalizability of antidepressant efficacy trials, appears to lack empirical support.
The primary aim of an antidepressant efficacy trial is to demonstrate drug-placebo differences. Consistent with this aim, antidepressant efficacy trials routinely exclude subjects believed to have high placebo response rates (e.g., subjects with mild depression) or low drug response rates (e.g., those with long-term depression or with comorbid anxiety, personality, or substance use disorders). The exclusion of these subjects significantly increases recruitment costs (1) and limits the generalizability of antidepressant efficacy trials to a narrow population of “pure” depressed patients.
Few published accounts of antidepressant efficacy trials present the percentage of individuals applying for entry who are screened out. Partonen et al. (2) reported that 381 of 612 subjects (62%) applying to participate in two separate antidepressant efficacy trials were excluded for a variety of reasons. Keitner et al. (3) found that only 60 of 866 antidepressant efficacy trial applicants (7%) screened in telephone interviews were ultimately randomly assigned to treatment groups. A survey of 18 clinical trial investigators found that an estimated 80% of applicants to antidepressant efficacy trials overseen by the investigators were excluded (1). Exact exclusion rates are difficult to determine, however, because eligibility is ascertained through a sequence of screening stages, and many ineligible subjects may not even be referred to such trials. We reported elsewhere that less than 15% of the depressed patients from our outpatient practice would be eligible to participate in an antidepressant efficacy trial due to various exclusion criteria (4).
Considering the cost and the limits to generalizability associated with the exclusion criteria that have been employed in antidepressant efficacy trials, some researchers have begun to question the wisdom of their use (5, 6). Since most exclusion criteria were implemented before rigorous testing, we wondered whether the current state of knowledge would support their continued use. The goal of the present report was to review the empirical research on the efficacy of antidepressant medications in subjects typically excluded from antidepressant efficacy trials. If comparable drug-placebo differences are found in these individuals, the standard exclusion criteria could perhaps be loosened without jeopardizing the overall aims of these studies.
Method
Review of Antidepressant Efficacy Trials
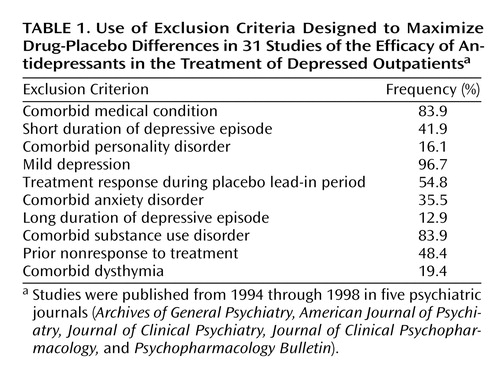
Details of our review of published antidepressant efficacy trials were presented elsewhere (4). Briefly, we reviewed the inclusion and exclusion criteria used in treatment efficacy studies of depression published from 1994 through 1998 in five psychiatric journals (Archives of General Psychiatry, American Journal of Psychiatry, Journal of Clinical Psychiatry, Journal of Clinical Psychopharmacology, and Psychopharmacology Bulletin). We identified 31 studies of outpatients that were not limited to a particular demographic group such as elderly patients. We evaluated how frequently each exclusion criterion was used in these 31 studies. No standard inclusion and exclusion criteria set exists. Among the 31 studies, no two employed the same inclusion and exclusion criteria set. Fourteen exclusion criteria were identified, and the 10 most common ones (mild depression, short episode duration, long episode duration, comorbid dysthymia, comorbid anxiety disorders, comorbid substance use disorders, comorbid personality disorders, medical comorbidity, prior nonresponse to treatment, and a positive response during the placebo lead-in phase) form the basis of our review (Table 1). Because the present report focused on exclusion criteria designed primarily to maximize drug-placebo differences, exclusion criteria used for other reasons are not considered. Thus, although exclusion criteria such as a diagnosis of bipolar disorder, psychotic features, suicidal ideation, age under 18 or over 65 years, and an inability to speak English are also common in antidepressant efficacy trials, these are not considered in the present review because the rationale for their use is distinct.
Literature Review
A computerized MEDLINE search, independent of the one used to identify the antidepressant efficacy trials, of all studies published from 1966 to December 2000 was performed with each of the 10 exclusion criteria used as key words and cross-referenced with “antidepressants.” All relevant articles were obtained, and a manual search was performed after each of these articles was reviewed. Because of the volume and breadth of the studies involved in the review, it is not possible to present the results of each study. Instead, we synthesized our findings and placed the greatest emphasis on double-blind, placebo-controlled studies that focused specifically on the efficacy of somatic therapy in the populations of interest. We also included studies that were not placebo controlled, placing the greatest emphasis on (in descending order) post hoc analyses derived from placebo-controlled studies, open-label trials, and naturalistic follow-up studies. More emphasis was also placed on studies that had adequate sample sizes, employed reasonable controls, and randomly assigned subjects to study groups.
In the present review, “efficacy,” as opposed to “effectiveness,” refers specifically to outcomes derived from placebo-controlled trials.
Results
Mild Depression
Several early antidepressant efficacy studies found that medications were no more effective than placebo in treating mild depression (7–9). Especially high placebo response rates (10, 11) and high spontaneous remission rates (12) in mild depression were believed to account for the lack of drug-placebo differences. In the National Institute of Mental Health (NIMH) Treatment of Depression Collaborative Research Program, subjects with mild depression who received imipramine plus clinical management fared no better than those who received clinical management alone (13). Largely on the basis of these results, it has generally been concluded that antidepressants are not efficacious for mild depression.
The Treatment of Depression Collaborative Research Program, however, was a 16-week study, and this amount of time could have been sufficient for many depressive episodes to spontaneously remit. Some have also questioned whether subjects in the research program may have derived significant benefit from “clinical management,” which would have undermined the ability of this cohort to serve as a control group. Last, Stewart et al. (6) have argued that the Treatment of Depression Collaborative Research Program sample sizes lacked sufficient power to assert that drug-placebo differences were not present. Larger studies focusing specifically on patients with mild depression, i.e., those with Hamilton Rating Scale for Depression scores of 13–17, have shown that antidepressants are efficacious for these patients (6, 14–18). However, there are conflicting data on whether they are efficacious for very mild depression, i.e., conditions associated with Hamilton depression scale scores of 12 or less (6, 15).
Episode Duration of 4 Weeks or Less
The DSM-IV diagnosis of major depressive disorder requires a minimum duration of symptoms of at least 2 weeks. Therefore, this exclusion criterion affects only patients whose episode has lasted 2–4 weeks. No studies have directly examined the impact of this cutoff. Placebo responders have generally been found to have a shorter duration of illness, and an episode duration of 3 months or less has consistently been found to predict high placebo response rates (19–22). Two analyses of separate cohorts of untreated subjects from the NIMH Collaborative Program on the Psychobiology of Depression found that spontaneous remission was also most likely to occur within the first 3 months of a depressive illness (23, 24). Thus, because of the high rates of placebo response and spontaneous remission in these patients, it is likely that drug-placebo differences are significantly less robust in patients with a short episode duration.
Long Episode Duration
A long episode duration at baseline is generally considered to be one of the strongest predictors of nonresponse to both somatic therapy (25, 26) and placebo (8, 19, 22, 27–30). One prospective study found that the duration of illness at baseline accounted for 45% of the variance in the time to eventual recovery (31). On the other hand, several studies have reported good response rates to somatic therapy in patients with chronic depression. For example, 92 of 167 patients with chronic depression (55%) responded to a 12-week open-label trial of nefazodone (32). In a double-blind, placebo-controlled trial, Kocsis et al. (33) found that 45% of patients with chronic depressive symptoms responded to imipramine (N=29), compared to only 12% who responded to placebo (N=25). In a post hoc analysis, Khan et al. (30) found that 56% of patients with chronic depression responded to antidepressant medications, which was only slightly less than the response rate in patients who were ill for less than 1 year (61%). Placebo response rates, on the other hand, were 45% in the latter cohort, compared to 23% in the patients with longer-term depression. In another post hoc analysis, paroxetine was found to be significantly more efficacious than placebo for depressed subjects whose episode had lasted 1 year or more, compared to those whose episode had lasted less than 1 year (34). Thus, while naturalistic studies have found that overall response rates to somatic therapy are lower in patients with chronic depression, compared to those with a shorter duration of depression, several controlled trials suggest that drug-placebo differences may be no less robust.
Comorbid Dysthymic Disorder
Depression complicated by dysthymia (“double depression”) is associated with a lower level of functioning (35, 36) and a worse long-term prognosis than depression alone (36–38). In a study by Kocsis and colleagues (33), all subjects had diagnoses of major depression and comorbid dysthymia. Response rates were significantly higher for subjects treated with imipramine than for those who received placebo. In an 8-week trial involving 102 subjects with “double depression” randomly assigned to receive moclobemide, imipramine, or placebo, both active treatments were superior to placebo (39). In another study involving 89 subjects with “double depression,” approximately two-thirds responded to active medication and one-third to placebo; these rates were comparable to those reported in patients with a diagnosis of dysthymia alone or with major depression in partial remission (40).
Comorbid Anxiety Disorders
When a diagnosis of a comorbid anxiety disorder is made in depressed patients, the depressive episode tends to be more severe and to be associated with a lower level of functioning (41–44). Most studies, but not all (45–47) have found that high levels of baseline anxiety are associated with lower response rates to somatic therapy (48–50) and a poorer overall prognosis (41, 42, 44, 51). Four naturalistic follow-up studies have shown that depressed patients with comorbid panic disorder respond less well to antidepressant therapy than those with a diagnosis of major depression alone (52–55).
To our knowledge, no double-blind, placebo-controlled studies have been designed specifically to evaluate the efficacy of antidepressant medications in depressed patients with a comorbid anxiety disorder. One double-blind, placebo-controlled study involving depressed subjects with moderate to severe levels of baseline anxiety, i.e., a Covi Anxiety Scale rating of ≥7, found that fluoxetine and extended-release venlafaxine were both superior to placebo (56). A post hoc analysis of this data set involving a subset of subjects with comorbid generalized anxiety disorder found that extended-release venlafaxine was superior to placebo at the 12-week follow-up visit (57). Antidepressant medications have also repeatedly been shown to ameliorate comorbid anxiety in depressed patients (46, 56, 58–60).
Several treatment studies utilizing antidepressant medications for primary anxiety disorders have provided further evidence that antidepressants may be efficacious for the treatment of depression confounded by anxiety. In a study of 126 subjects with panic disorder and a concurrent mood disorder (major depression, dysthymia, or depressive disorder not otherwise specified) treated for 16 weeks with imipramine, alprazolam, or placebo, both active medications were found to be efficacious in treating the comorbid major depression (61). A reanalysis of this data set revealed that imipramine was specifically beneficial for depressive symptoms, whereas alprazolam produced most of its benefits in the domains of sleep and anxiety (62). A post hoc analysis by Zajecka (63) of data for 55 subjects with panic disorder and comorbid major depression found that nefazodone was superior to placebo in treating the comorbid depressive disorder. Placebo-controlled studies involving subjects with posttraumatic stress disorder (64–66), obsessive-compulsive disorder (67–70), and generalized anxiety disorder (71) have suggested that antidepressants may be efficacious for comorbid major depression in these disorders as well.
In summary, the presence of comorbid anxiety appears to be associated with lower response rates to somatic therapy. The few placebo-controlled studies that have included patients with comorbid anxiety have suggested that antidepressants may be efficacious for depression confounded by anxiety. However, to our knowledge, no studies have been specifically designed to assess the efficacy of antidepressant medications in patients with a comorbid anxiety disorder.
Comorbid Substance Use Disorders
Some studies have found that comorbid substance abuse is associated with a lower recovery rate from depression (72, 73), while others have not found this association (74). Early placebo-controlled studies did not find that antidepressants were helpful for depressive symptoms in subjects with active alcoholism (75, 76). More recently, placebo-controlled studies have shown that antidepressants are efficacious in treating depressive symptoms in recently abstinent alcoholics (77–80) as well as in actively drinking alcohol-dependent patients (81, 82). One double-blind, placebo-controlled study found that fluoxetine was efficacious for depressive symptoms in 22 depressed alcoholic marijuana users (83).
Data on the benefits of antidepressants for active drug abusers are mixed. Three double-blind, placebo-controlled studies have found tricyclic antidepressants to be efficacious for depressed opioid addicts (84–86), while two other studies found no advantage for tricyclics over placebo in methadone-maintained addicts (87, 88). We are not aware of any placebo-controlled studies evaluating the efficacy of antidepressant medications for major depression in recently detoxified (rather than active) drug abusers.
Comorbid Personality Disorders
The overwhelming majority of studies assessing the impact of comorbid personality pathology on antidepressant response rates have found that the presence of a comorbid personality disorder conveys a worse prognosis (50, 89–94). Short-term response rates to somatic therapy in naturalistic follow-up studies have ranged from 9% to 52% (95). No consistent pattern of nonresponse exists among the personality disorder clusters (95), and the presence of several personality disorder diagnoses appears to convey a worse prognosis than any single personality disorder (96). Nevertheless, treatment with antidepressant medications appears to diminish dysfunctional attitudes and decrease rates of posttreatment personality disorder diagnoses (97). We were unable to locate any studies that have directly addressed placebo response rates in depressed personality disorder patients. Weissman et al. (98) reported that high neuroticism scores on the Maudsley Personality Inventory predicted poor outcome in a cohort of comparison (i.e., untreated) subjects with major depression “to a highly significant degree.” It was also noted that medications and psychotherapy appeared to ameliorate the negative impact that a high level of neuroticism has on outcome.
We are not aware of any placebo-controlled studies designed specifically to evaluate the efficacy of antidepressant medications in depressed patients with a comorbid personality disorder diagnosis. Soloff and colleagues (99, 100) performed a series of studies comparing the efficacy of antidepressants, haloperidol, and placebo in patients with borderline personality disorder. The patients in these studies did not necessarily suffer from major depression, although depressive symptoms were prominent in many patients. Antidepressant medications were found to be of marginal benefit. These studies are limited because they took place on inpatient units, and the therapeutic effects of hospitalization may have inflated placebo response rates.
In a post hoc analysis, Parsons et al. (101) found extremely robust antidepressant response rates in depressed patients with atypical features and a comorbid borderline personality disorder diagnosis. Depending on the diagnostic threshold used to define borderline personality disorder, approximately 90% of subjects responded to a trial of phenelzine, 40% to imipramine, and only 20% to placebo. A study by Tyrer and colleagues (102) was unable to replicate the efficacy of phenelzine for depressed patients with personality pathology.
In summary, studies have consistently shown that personality pathology predicts inferior rates of response to somatic therapy. However, data on response rates to placebo and drug-placebo differences are insufficient to draw any conclusions.
Comorbid Medical Conditions
Prospective, naturalistic studies have found that medical comorbidity conveys a worse long-term prognosis (72, 103). In an open-label study involving 50 medically ill inpatients treated for major depression, only 40% responded to an adequate antidepressant trial (104). Although no comparison group was included, the low response rate suggests that medical comorbidity may limit the therapeutic benefits of antidepressant medications. Supporting this contention, Hall et al. (105) found that nearly one-half of all depressed patients who did not respond to an antidepressant trial had some underlying medical condition that might have accounted for the lack of response. The authors reported that addressing the medical condition often ameliorated the depressive symptoms.
Nevertheless, at least eight placebo-controlled studies have supported the efficacy of antidepressant medications in treating depression associated with such diverse illnesses as cancer (106), multiple sclerosis (107), chronic obstructive pulmonary disease (108), stroke (109, 110), diabetes (111, 112), and cardiac disease (113). Two other randomized controlled trials involving “physically ill” patients also found antidepressants to be superior to placebo (114, 115). Antidepressants were not found to be efficacious in two studies involving patients with Alzheimer’s disease (116) and epilepsy (117).
Prior Nonresponse to Multiple Antidepressant Trials
Prior nonresponse to treatment is associated with lower drug and placebo response rates (8, 22, 27, 50). Thase and Rush (118) have argued that patients who have failed three or more adequate antidepressant trials have less than a 30% chance of responding to a fourth. Prior exposure to psychotropic medications is associated with improved compliance (119), however. One study found that drug-placebo differences were greatest in patients who had undergone at least two previous medication trials (119). Furthermore, individuals who have had a positive response to somatic therapy in the past may be more likely to subsequently respond to placebo (27, 120). Thus, the exclusion of individuals who have failed multiple antidepressant trials may result in exclusion of individuals who are more likely to comply with the protocol and less likely to respond to placebo. Although these subjects would also be expected to have a lower response rate to somatic therapy, it is unclear whether drug-placebo differences would be affected.
Response to Placebo Lead-In
The majority of antidepressant efficacy trials use a placebo lead-in period (121). Individuals who demonstrate clinical improvement during this period are often excluded from the active phase of treatment despite meeting all other eligibility requirements. The potential value of a placebo lead-in period was depicted in a 1966 study by Jones and Ainslie (122), who showed that the placebo response tends to occur within the first 2 weeks of treatment. By using the week 3 ratings as baseline rather than week 1 ratings, the authors demonstrated that placebo response rates could be significantly reduced without significantly affecting drug response rates. The practice of excluding placebo lead-in responders did not occur until two decades later, and the origins of this practice remain unclear (20, 121). Most likely, it was presumed that individuals who improved on placebo during the lead-in phase would be the same ones to improve during the active phase. If so, the inclusion of such individuals would be expected to obscure drug-placebo differences.
Although this reasoning is logical and intuitively appealing, one study that compared placebo lead-in responders with 6-week placebo responders found that the two cohorts had distinct demographic characteristics, suggesting that placebo lead-in responders may not be isomorphic with subjects who respond to placebo during the active phase of treatment (28). Reimherr and Ward (123) examined the impact of including subjects who demonstrated significant improvement on self-rating scales during the placebo lead-in phase but who were included in the active phase because clinicians’ ratings did not reflect improvement (“hidden placebo responders”). Inclusion of these subjects did not affect drug-placebo differences. In fact, the hidden placebo responders demonstrated larger drug-placebo differences than nonresponders to the placebo lead-in. In a meta-analysis that compared 39 antidepressant efficacy trials that used a placebo lead-in and 33 that did not, Trivedi and Rush (121) found that the response to placebo during the active phase was nearly identical in both cohorts (27.8% versus 28.5%). These findings suggest that the placebo lead-in does not diminish placebo response rates during the active phase. Furthermore, drug-placebo differences were found to be slightly less in studies that used a placebo lead-in. Some investigators have even speculated that improvement during the placebo lead-in may serve to mitigate further improvement in patients who receive placebo during the active phase of the trial (20, 124).
Discussion
For years, investigators have raised concerns over the generalizability of antidepressant efficacy trials. Although some of the exclusion criteria used in antidepressant efficacy trials are clearly necessary, others are implemented primarily to maximize drug-placebo differences. This practice greatly reduces the generalizability of these studies but perhaps can be justified if it decreases the likelihood of obtaining a type II error, i.e., not finding drug-placebo differences when real differences are present. However, if drug-placebo differences are in fact no less robust in these populations, then the rationale for excluding these subjects becomes less tenable.
Three cohorts of subjects—those with mild depression, those with an episode duration of less than 4 weeks, and those who improve during the placebo lead-in period—are excluded to minimize placebo response rates. Although early studies suggested that subjects with mild depression may not respond any better to antidepressant medication than to placebo, these studies had several shortcomings, including a lack of statistical power in failing to reject the null hypothesis. More recent studies, though few in number, have shown that antidepressants may be efficacious for mild depression. Similarly, the practice of excluding placebo lead-in responders has never been shown to magnify drug-placebo differences, and all available evidence suggests that this exclusion criterion has no discernable impact on differential response rates. Although studies have consistently shown that a short episode duration is associated with high placebo response rates, a 3-month or less episode duration would appear to be a more empirically validated cutoff than 4 weeks.
The remaining seven exclusion criteria that we reviewed—chronic depression, comorbid dysthymia, comorbid anxiety disorders, comorbid substance use disorders, comorbid personality disorders, comorbid medical conditions, and prior nonresponse to treatment—were originally implemented after naturalistic studies had shown that patients with these features responded less well to somatic therapy and had a worse overall prognosis. Without a placebo comparison group, however, a lack of drug-placebo differences cannot be inferred. Even now, few placebo-controlled studies have been performed to specifically address the efficacy of antidepressant medications in depressed patients with these features. The few studies that have been performed have suggested that placebo response rates are also lower in these patients.
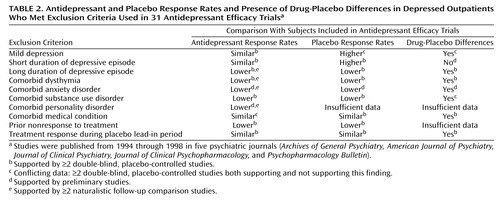
In summary, our review suggests a paucity of empirical support justifying the use of the 10 exclusion criteria considered in the present report (Table 2). For individuals with chronic depression, comorbid dysthymia, or medical comorbidity and for placebo lead-in responders, our review suggests that drug-placebo differences may be no less robust in these subjects than in individuals who qualify for antidepressant efficacy trials. For subjects with mild depression, a comorbid anxiety disorder, a comorbid substance use disorder, a comorbid personality disorder, or a history of nonresponse to treatment, the data are either conflicting or too preliminary to determine whether the magnitude of drug-placebo differences is any less. It remains unknown whether antidepressant medications are superior to placebo in patients with a short episode duration, but the high placebo and spontaneous response rates in these individuals make it likely that drug-placebo differences are significantly less robust.
Further evidence to support the efficacy of antidepressant medications in less rarefied populations is provided by placebo-controlled studies in primary care settings where standard exclusion criteria are not employed. Although only a handful of such studies have been performed with methods comparable to those in antidepressant efficacy trials, these studies have consistently found antidepressants to be efficacious in relatively unselected populations of depressed patients (14, 58, 119, 125). Depressed patients in primary care settings have less psychiatric comorbidity and lower rates of treatment resistance than psychiatric patients, however, and these results can not necessarily be generalized to psychiatric patients.
In interpreting the results of the present review, several important caveats should be kept in mind. First, the review was limited by the scarcity of controlled studies involving the populations of interest. For example, it was our intention to statistically compare outcomes of subjects who are excluded from antidepressant efficacy trials with the outcomes of subjects who are typically included. However, the limited number of studies precluded any meaningful effect size comparisons. Second, although preliminary evidence has suggested that drug-placebo differences exist in many of the populations excluded from antidepressant efficacy trials, we do not know whether the magnitude of their response is comparable to that of those included in the trials. If the magnitude of drug-placebo differences were less in the excluded individuals, even if drug-placebo differences exist, then the exclusion of these individuals would still decrease the likelihood of obtaining a type II error. Third, our review includes only published studies and is therefore susceptible to the “file drawer” bias, since studies with negative results are less likely to be published. Because the number of placebo-controlled studies that have been performed in each of the populations reviewed here is small, only a handful of negative, unpublished studies would be needed to undermine our principal conclusions (126). It should also be pointed that easing the inclusion/exclusion criteria of antidepressant efficacy trials would increase the heterogeneity of the population studied, and, therefore, the variance in base response rates would likely increase. When this occurs, the power to detect differences decreases. At this time, it is difficult to estimate the impact of this variance in base response rates on the results of antidepressant efficacy trials.
In conclusion, our review suggests that the rationale for employing many of the exclusion criteria used in standard antidepressant efficacy trials lacks a clear empirical basis. It is somewhat shocking that after 50 years following the introduction of antidepressant medications, there has yet to be a single published study that was designed specifically to evaluate their efficacy in depressed patients with a comorbid anxiety disorder or a comorbid personality disorder—patients who constitute perhaps that majority of those encountered in routine clinical practice. Other populations of patients, such as those with mild depression or chronic depression, have only rarely been the focus of systematic inquiry. Clearly, there is a need to move beyond the traditional model of how antidepressant efficacy trials are conducted.
 |
 |
Received May 7, 2001; revision received Sept. 17, 2001; accepted Oct. 9, 2001. From the Department of Psychiatry and Human Behavior, Brown University School of Medicine. Address reprint requests to Dr. Posternak, Department of Psychiatry and Human Behavior, Brown University School of Medicine, Rhode Island Hospital, 235 Plain St., Suite 501, Providence, RI 02905; [email protected] (e-mail).
1. Bielski RJ, Lydiard RB: Therapeutic trial participants: where do we find them and what does it cost? Psychopharmacol Bull 1997; 33:75-78Medline, Google Scholar
2. Partonen T, Sihvo S, Lonnqvist JK: Patients excluded from an antidepressant efficacy trial. J Clin Psychiatry 1996; 57:572-575Crossref, Medline, Google Scholar
3. Keitner GI, Ryan CE, Miller IW, Solomon DA: Who gets into clinical trials? in 1999 Annual Meeting New Research Program and Abstracts. Washington, DC, American Psychiatric Association, 1999, p 242Google Scholar
4. Zimmerman M, Mattia JI, Posternak MA: Are subjects in pharmacological treatment trials of depression representative of patients in routine clinical practice? Am J Psychiatry (in press)Google Scholar
5. Angst J, Bech P, Bruinvels H, Engel R, Helmchen H, Hippius H, Lingjaerde O, Racoagni G, Saletu B, Sedvall G, Silverstone JT, Stefanis CN, Stoll K, Woggon B: Consensus conference on the methodology of clinical trials of antidepressants, Zurich, March 1988: report of the consensus committee. Pharmacopsychiatry 1989; 22:3-7Crossref, Google Scholar
6. Stewart JW, McGrath PJ, Quitkin FM: Can mildly depressed outpatients with atypical depression benefit from antidepressants? Am J Psychiatry 1992; 149:615-619Link, Google Scholar
7. DiMascio A, Meyer RE, Stifler L: Effects of imipramine on individuals varying in level of depression. Am J Psychiatry 1968; 124(Feb suppl):55-58Google Scholar
8. Downing RW, Rickels K: Predictors of response to amitriptyline and placebo in three outpatient treatment settings. J Nerv Ment Dis 1973; 156:109-129Crossref, Medline, Google Scholar
9. Raskin A, Crook TH: The endogenous-neurotic distinction as a predictor of response to antidepressant drugs. Psychological Med 1976; 6:59-70Crossref, Medline, Google Scholar
10. Brown WA: Predictors of placebo response in depression. Psychopharmacol Bull 1988; 24:14-17Medline, Google Scholar
11. Peselow ED, Sanfilipo MP, Difiglia C, Fieve RR: Melancholic/endogenous depression and response to somatic treatment and placebo. Am J Psychiatry 1992; 149:1324-1334Link, Google Scholar
12. Barrett JE, Hurst MW: Short-term symptom change in outpatient psychiatric disorders. Arch Gen Psychiatry 1982; 39:849-854Crossref, Medline, Google Scholar
13. Elkin I, Gibbons RD, Shea MT, Sotsky SM, Watkins JT, Pilkonis PA, Hedeker D: Initial severity and differential treatment outcome in the National Institute of Mental Health Treatment of Depression Collaborative Research Program. J Consult Clin Psychol 1995; 63:841-847Crossref, Medline, Google Scholar
14. Hollyman JA, Freeling P, Paykel ES, Bhat A, Sedgwick P: Double-blind placebo-controlled trial of amitriptyline among depressed patients in general practice. J R Coll Gen Pract 1988; 38:393-397Medline, Google Scholar
15. Paykel ES, Freeling P, Hollyman JA: Are tricyclic antidepressants useful for mild depression? a placebo controlled trial. Pharmacopsychiatry 1988; 21:15-18Crossref, Medline, Google Scholar
16. Dunlop SR, Dornseif BE, Wernick JF, Potvin JH: Pattern analysis shows beneficial effect of fluoxetine treatment in mild depression. Psychopharmacol Bull 1990; 26:173-180Medline, Google Scholar
17. Pande AC, Sayler ME: Severity of depression and response to fluoxetine. Int Clin Psychopharmacol 1993; 8:243-245Crossref, Medline, Google Scholar
18. Ose E, Holm P: Moclobemide and placebo in mild major depression: a double-blind randomized trial. Psychopharmacology (Berl) 1992; 106(suppl 1A):S114-S115Google Scholar
19. Brown WA, Dornseif BE, Wernicke JF: Placebo response in depression: a search for predictors. Psychiatry Res 1988; 26:259-264Crossref, Medline, Google Scholar
20. Fairchild CJ, Rush AJ, Vasavada N, Giles DE, Khatami M: Which depressions respond to placebo? Psychiatry Res 1986; 18:217-226Crossref, Medline, Google Scholar
21. Stewart JW, Quitkin FM, Liebowitz MR, McGrath PJ, Harrison WM, Klein DF: Efficacy of desipramine in depressed outpatients: response according to research diagnosis criteria diagnoses and severity of illness. Arch Gen Psychiatry 1983; 40:202-207Crossref, Medline, Google Scholar
22. Rickels K, Lipman R, Raab E: Previous medication, duration of illness and placebo response. J Nerv Ment Dis 1966; 142:548-554Crossref, Medline, Google Scholar
23. Coryell W, Akiskal HS, Leon AC, Winokur G, Maser JD, Mueller TI, Keller MB: The time course of nonchronic major depressive disorder: uniformity across episodes and samples. Arch Gen Psychiatry 1994; 51:405-410Crossref, Medline, Google Scholar
24. Posternak MA, Solomon DA, Leon AC, Mueller TI, Shea MT, Keller MB: The naturalistic course of untreated major depression, in 2001 Annual Meeting New Research Program and Abstracts. Washington, DC, American Psychiatric Association, 2001, p 27Google Scholar
25. Bielski RJ, Friedel RO: Prediction of tricyclic antidepressant response. Arch Gen Psychiatry 1976; 33:1479-1489Crossref, Medline, Google Scholar
26. Berman RM, Narasimhan M, Charney DS: Treatment-refractory depression: definitions and characteristics. Depress Anxiety 1997; 5:154-164Crossref, Medline, Google Scholar
27. Brown WA, Johnson MF, Chen M: Clinical features of depressed patients who do and do not improve with placebo. Psychiatry Res 1992; 41:203-214Crossref, Medline, Google Scholar
28. Rabkin JG, Stewart JW, McGrath PJ, Markowitz JS, Harrison W, Quitkin FM: Baseline characteristics of 10-day placebo washout responders in antidepressant trials. Psychiatry Res 1987; 21:9-22Crossref, Medline, Google Scholar
29. Rabkin JG, McGrath PJ, Quitkin FM, Tricamo E, Stewart JW, Klein DF: Effects of pill-giving on maintenance of placebo response in patients with chronic mild depression. Am J Psychiatry 1990; 147:1622-1626Link, Google Scholar
30. Khan A, Dager SR, Cohen S, Avery DH, Scherzo B, Dunner DL: Chronicity of depressive episode in relation to antidepressant-placebo response. Neuropsychopharmacology 1991; 4:125-130Medline, Google Scholar
31. Scott J, Eccleston D, Boys R: Can we predict the persistence of depression? Br J Psychiatry 1992; 161:633-637Crossref, Medline, Google Scholar
32. Keller MB, McCullough JP, Klein DN, Arnow B, Dunner DL, Gelenberg AJ, Markowitz JC, Nemeroff CB, Russell JM, Thase ME, Trivedi MH, Zajecka J: A comparison of nefazodone, the cognitive behavioral-analysis system of psychotherapy, and their combination for the treatment of chronic depression. N Engl J Med 2000; 342:1462-1470Crossref, Medline, Google Scholar
33. Kocsis JH, Frances AJ, Voss C, Mann JJ, Mason BJ, Sweeney J: Imipramine treatment for chronic depression. Arch Gen Psychiatry 1988; 45:253-257Crossref, Medline, Google Scholar
34. Smith WT, Glaudin V: A placebo-controlled trial of paroxetine in the treatment of major depression. J Clin Psychiatry 1992; 53(suppl 2):36-39Google Scholar
35. Keller MB, Lavori PW, Mueller TI, Endicott J, Coryell W, Hirschfeld RMA, Shea T: Time to recovery, chronicity, and levels of psychopathology in major depression: a 5-year prospective follow-up of 431 patients. Arch Gen Psychiatry 1992; 49:809-816Crossref, Medline, Google Scholar
36. Wells KB, Burnam MA, Rogers W, Hays R, Camp P: The course of depression in adult outpatients: results from the Medical Outcomes Study. Arch Gen Psychiatry 1992; 49:788-794Crossref, Medline, Google Scholar
37. Klein DN, Taylor EB, Harding K, Dickstein S: Double depression and episodic major depression: demographic, clinical, familial, personality, and socioenvironmental characteristics and short-term outcome. Am J Psychiatry 1988; 145:1226-1231Link, Google Scholar
38. Keller MB, Shapiro RW: “Double depression”: superimposition of acute depressive episodes on chronic depressive disorders. Am J Psychiatry 1982; 139:438-442Link, Google Scholar
39. Versiani M, Amrein R, Stabl M: Moclobemide and imipramine in chronic depression (dysthymia): an international double-blind, placebo-controlled trial. Int Clin Psychopharmacol 1997; 12:183-193Crossref, Medline, Google Scholar
40. Lecrubier Y, Boyer P, Turjanski S, Rein W: Amisulpride versus imipramine and placebo in dysthymia and major depression. J Affect Disord 1997; 43:95-103Crossref, Medline, Google Scholar
41. Clayton PJ, Grove WM, Coryell W, Keller M, Hirschfeld R, Fawcett J: Follow-up and family study of anxious depression. Am J Psychiatry 1991; 148:1512-1517Link, Google Scholar
42. Coryell W, Endicott J, Andreasen NC, Keller MB, Clayton PJ, Hirschfeld RMA, Scheftner WA, Winokur G: Depression and panic attacks: the significance of overlap as reflected in follow-up and family study data. Am J Psychiatry 1988; 145:293-300Link, Google Scholar
43. Woody S, McLean PD, Taylor S, Koch WJ: Treatment of major depression in the context of panic disorder. J Affect Disord 1999; 53:163-174Crossref, Medline, Google Scholar
44. Brown C, Schulberg HC, Madonia MJ, Shear MK, Houck PR: Treatment outcomes for primary care patients with major depression and lifetime anxiety disorders. Am J Psychiatry 1996; 153:1293-1300Link, Google Scholar
45. Tollefson GD, Holman SL, Sayler ME, Potvin JH: Fluoxetine, placebo, and tricyclic antidepressants in major depression with and without anxious features. J Clin Psychiatry 1994; 55:50-59Medline, Google Scholar
46. Fava M, Rosenbaum JF, Hoog SL, Tepner RG, Kopp JB, Nilsson ME: Fluoxetine versus sertraline and paroxetine in major depression: tolerability and efficacy in anxious depression. J Affect Disord 2000; 59:119-126Crossref, Medline, Google Scholar
47. Joffe RT, Bagby RM, Levitt A: Anxious and nonanxious depression. Am J Psychiatry 1993; 150:1257-1258Link, Google Scholar
48. Kupfer DJ, Spiker DG: Refractory depression: prediction of non-response by clinical indicators. J Clin Psychiatry 1981; 42:307-312Medline, Google Scholar
49. Roose SP, Glassman AH, Walsh BT, Woodring S: Tricyclic nonresponders: phenomenology and treatment. Am J Psychiatry 1986; 143:345-348Link, Google Scholar
50. Nelson JC, Mazure CM, Jatlow PI: Characteristics of desipramine-refractory depression. J Clin Psychiatry 1994; 55:12-19Medline, Google Scholar
51. Gaynes BN, Magruder KM, Burns BJ, Wagner HR, Yarnall KSH, Broadhead WE: Does a coexisting anxiety disorder predict persistence of depressive illness in primary care patients with major depression? Gen Hosp Psychiatry 1999; 21:158-167Crossref, Medline, Google Scholar
52. Grunhaus L, Rabin D, Greden JF: Simultaneous panic and depressive disorders: response to antidepressant treatments. J Clin Psychiatry 1986; 47:4-7Medline, Google Scholar
53. Grunhaus L, Harel Y, Krugler T, Pande AC, Haskett RF: Major depressive disorder and panic disorder: effects of comorbidity on treatment outcome with antidepressant medications. Clin Neuropharmacol 1988; 11:454-461Crossref, Medline, Google Scholar
54. Levitt AJ, Joffe RT, Brecher D, MacDonald C: Anxiety disorders and anxiety symptoms in a clinic sample of seasonal and non-seasonal depressives. J Affect Disord 1993; 28:51-56Crossref, Medline, Google Scholar
55. van Valkenburg C, Akiskal JS, Puzantian V, Rosenthal T: Anxious depressions: clinical, family history, and naturalistic outcome—comparisons with panic and major depressive disorders. J Affect Disord 1984; 6:67-82Crossref, Medline, Google Scholar
56. Silverstone PH, Ravindran A: Once-daily venlafaxine extended release (XR) compared with fluoxetine in outpatients with depression and anxiety. J Clin Psychiatry 1999; 60:22-28Crossref, Google Scholar
57. Silverstone PH, Salinas E: Efficacy of venlafaxine extended release in patients with major depressive disorder and comorbid generalized anxiety disorder. J Clin Psychiatry 2001; 62:523-529Crossref, Medline, Google Scholar
58. Blashki TG, Mowbray R, Davies B: Controlled trial of amitriptyline in general practice. Br Med J 1971; 1:133-138Crossref, Medline, Google Scholar
59. Sheehan D, Dunbar GC, Fuell DL: The effect of paroxetine on anxiety and agitation associated with depression. Psychopharmacol Bull 1992; 28:139-143Medline, Google Scholar
60. Dunbar GC, Cohn JB, Fabre LF, Feighner JP, Fieve RR, Mendels J, Shrivastava R: A comparison of paroxetine, imipramine, and placebo in depressed outpatients. Br J Psychiatry 1991; 159:394-398Crossref, Medline, Google Scholar
61. Keller MB, Lavori PW, Goldenberg IM, Baker LA, Pollack MH, Sachs GS, Rosenbaum JF, Deltito JA, Leon A, Shear K, Klerman GL: Influence of depression on the treatment of panic disorder with imipramine, alprazolam and placebo. J Affect Disord 1993; 28:27-38Crossref, Medline, Google Scholar
62. Leon AC, Shear K, Portera L, Klerman GL: Effect size as a measure of symptom-specific drug change in clinical trials. Psychopharmacol Bull 1993; 29:163-167Medline, Google Scholar
63. Zajecka JM: The effect of nefazodone on comorbid anxiety symptoms associated with depression: experience in family practice and psychiatric outpatient settings. J Clin Psychiatry 1996; 57(suppl 2):10-14Google Scholar
64. Brady K, Pearlstein T, Asnis GM, Baker D, Rothbaum B, Sikes CR, Farfel GM: Efficacy and safety of sertraline treatment of posttraumatic stress disorder: a randomized controlled trial. JAMA 2000; 283:1837-1844Crossref, Medline, Google Scholar
65. Davidson J, Kudler H, Smith R, Mahorney SL, Lipper S, Hammett E, Saunders WB, Cavenar JO Jr: Treatment of posttraumatic stress disorder with amitriptyline and placebo. Arch Gen Psychiatry 1990; 47:259-266Crossref, Medline, Google Scholar
66. Reist C, Kauffmann CD, Haier RJ, Sangdahl C, DeMet EM, Chicz-DeMet A, Nelson JN: A controlled trial of desipramine in 18 men with posttraumatic stress disorder. Am J Psychiatry 1989; 146:513-516Link, Google Scholar
67. Foa EB, Kozak MJ, Steketee GS, McCarthy PR: Treatment of depressive and obsessive-compulsive symptoms in OCD by imipramine and behaviour therapy. Br J Clin Psychol 1992; 31:279-292Crossref, Medline, Google Scholar
68. Ackerman DL, Greenland S, Bystritsky A: Clinical characteristics of response to fluoxetine treatment of obsessive-compulsive disorder. J Clin Psychopharmacol 1998; 18:185-193Crossref, Medline, Google Scholar
69. Goodman WK, Price LH, Rasmussen SA, Delgado PL, Heninger GR, Charney DS: Efficacy of fluvoxamine in obsessive-compulsive disorder: a double-blind comparison with placebo. Arch Gen Psychiatry 1989; 46:36-44Crossref, Medline, Google Scholar
70. Insel TR, Murphy DL, Cohen RM, Alterman I, Kilts C, Linnoila M: Obsessive-compulsive disorder: a double-blind trial of clomipramine and clorgyline. Arch Gen Psychiatry 1983; 40:605-612Crossref, Medline, Google Scholar
71. Sramek JJ, Tansman M, Suri A, Hornig-Rohan M, Amsterdam JD, Stahl SM, Weisler RH, Cutler NR: Efficacy of buspirone in generalized anxiety disorder with coexisting mild depressive symptoms. J Clin Psychiatry 1996; 57:287-291Medline, Google Scholar
72. Akiskal H: Factors associated with incomplete recovery in primary depressive illness. J Clin Psychiatry 1982; 43:266-271Medline, Google Scholar
73. MacEwan GW, Remick RA: Treatment resistant depression: a clinical perspective. Can J Psychiatry 1988; 33:788-792Crossref, Medline, Google Scholar
74. Hirschfeld RMA, Kosier T, Keller MB, Lavori PW, Endicott J: The influence of alcoholism on the course of depression. J Affect Disord 1989; 16:151-158Crossref, Medline, Google Scholar
75. Shaw JA, Donley P, Morgan DW, Robinson JA: Treatment of depression in alcoholics. Am J Psychiatry 1975; 132:641-644Link, Google Scholar
76. Ciraulo DA, Haffe JH: Tricyclic antidepressants in the treatment of depression associated with alcoholism. J Clin Psychopharmacol 1981; 1:146-150Crossref, Medline, Google Scholar
77. Mason BJ: Desipramine treatment of alcoholism. Psychopharmacol Bull 1991; 27:155-161Medline, Google Scholar
78. Kranzler HR, Burleson JA, Korner P, DelBoca FK, Bohn MJ, Brown J, Liebowitz N: Placebo-controlled trial of fluoxetine as an adjunct to relapse prevention in alcoholics. Am J Psychiatry 1995; 152:391-397Link, Google Scholar
79. Mason BJ, Cocsis JH, Ritvo EC, Cutler RB: A double-blind, placebo-controlled trial of desipramine for primary alcohol dependence stratified on the presence or absence of major depression. JAMA 1996; 275:761-767Crossref, Medline, Google Scholar
80. Roy A: Placebo-controlled study of sertraline in depressed recently abstinent alcoholics. Biol Psychiatry 1998; 44:633-637Crossref, Medline, Google Scholar
81. McGrath PJ, Nunes EV, Stewart JW, Goldman D, Agosti V, Ocepek-Welikson K, Quitkin FM: Imipramine treatment of alcoholics with primary depression: a placebo-controlled clinical trial. Arch Gen Psychiatry 1996; 53:232-240Crossref, Medline, Google Scholar
82. Roy-Byrne PP, Pages KP, Russo JE, Jaffe C, Blume AW, Kingsley E, Cowley DS, Ries RK: Nefazodone treatment of major depression in alcoholic-dependent patients: a double-blind, placebo-controlled trial. J Clin Psychopharmacol 2000; 20:129-136Crossref, Medline, Google Scholar
83. Cornelius JR, Salloum IM, Haskett RF, Ehler JG, Jarrett PJ, Thase ME, Perel JM: Fluoxetine versus placebo for the marijuana use of depressed alcoholics. Addict Behav 1998; 24:111-114Crossref, Google Scholar
84. Woody GE, O’Brien BP, Rickels K: Depression and anxiety in heroin addicts: a placebo-controlled study of doxepin in combination with methadone. Am J Psychiatry 1975; 132:447-450Link, Google Scholar
85. Arndt IO, Dorozynsky L, Woody GE, McLellan AT, O’Brien CP: Desipramine treatment of cocaine dependence in methadone-maintained patients. Arch Gen Psychiatry 1992; 49:888-893Crossref, Medline, Google Scholar
86. Giannini JA, Malone DA, Giannini MC, Price WA, Loiselle RH: Treatment of depression in chronic cocaine and phencyclidine abuse with desipramine. J Clin Pharmacol 1986; 26:211-214Crossref, Medline, Google Scholar
87. Kleber HD, Weissman MM, Rounsaville BJ, Wilber CH, Prusoff BA, Riordan CE: Imipramine as treatment for depression in addicts. Arch Gen Psychiatry 1983; 40:649-653Crossref, Medline, Google Scholar
88. Petrakis I, Carroll KM, Nich C, Gordon L, Kosten T, Rounsaville B: Fluoxetine treatment of depressive disorders in methadone-maintained opioid addicts. Drug Alcohol Depend 1998; 50:221-226Crossref, Medline, Google Scholar
89. Black DW, Bell S, Hulbert J, Nasrallah A: The importance of axis II in patients with major depression: a controlled study. J Affect Disord 1988; 14:115-122Crossref, Medline, Google Scholar
90. Charney DS, Nelson JC, Quinlan DM: Personality traits and disorder in depression. Am J Psychiatry 1981; 138:1601-1604Link, Google Scholar
91. Pfohl B, Stangl D, Zimmerman M: The implications of DSM-III personality disorders for patients with major depression. J Affect Disord 1984; 7:309-318Crossref, Medline, Google Scholar
92. Peselow ED, Fieve RR, DiFiglia C: Personality traits and response to desipramine. J Affect Disord 1992; 24:209-216Crossref, Medline, Google Scholar
93. Zimmerman M, Coryell W, Pfohl B, Corenthal C, Stangl D: ECT response in depressed patients with and without a DSM-III personality disorder. Am J Psychiatry 1986; 143:1030-1032Link, Google Scholar
94. Sauer H, Kick H, Minne HW, Schneider B: Prediction of amitriptyline response: psychopathology vs neuroendocrinology. Int Clin Psychopharmacol 1986; 1:284-295Crossref, Medline, Google Scholar
95. Ilardi SS, Craighead WE: Personality pathology and response to somatic treatments for major depression: a critical review. Depression 1994/1995; 2:200-217Google Scholar
96. Sato T, Sakado K, Sato S, Morikawa T: Cluster A personality disorder: a marker of worse treatment outcome of major depression? Psychiatry Res 1993; 53:153-159Crossref, Google Scholar
97. Fava M, Bless EB, Otto MW, Pava JA, Rosenbaum JF: Dysfunctional attitudes in major depression. J Nerv Ment Dis 1994; 182:45-49Medline, Google Scholar
98. Weissman MM, Prussoff BA, Klerman GL: Personality and the prediction of long-term outcome of depression. Am J Psychiatry 1978; 135:797-800Link, Google Scholar
99. Soloff PH, George A, Nathan S, Schulz PM, Cornelius JR, Herring J, Perel JM: Amitriptyline versus haloperidol in borderlines: final outcomes and predictors of response. J Clin Psychopharmacol 1983; 9:238-246Crossref, Google Scholar
100. Soloff PH, Cornelius J, George A, Nathan S, Perel JM, Ulrich RF: Efficacy of phenelzine and haloperidol in borderline personality disorder. Arch Gen Psychiatry 1993; 50:377-385Crossref, Medline, Google Scholar
101. Parsons B, Quitkin FM, McGrath PJ, Stewart JW, Tricamo E, Ocepek-Welikson K, Harrison W, Rabkin JG, Wager SG, Nunes E: Phenelzine, imipramine, and placebo in borderline patients meeting criteria for atypical depression. Psychopharmacol Bull 1989; 25:524-534Medline, Google Scholar
102. Tyrer P, Casey P, Gall J: Relationship between neurosis and personality disorder. Br J Psychiatry 1983; 142:404-408Crossref, Medline, Google Scholar
103. Keitner GI, Ryan CE, Miller IW, Kohn R, Epstein NB: 12-month outcome of patients with major depression and comorbid psychiatric or medical illness (compound depression). Am J Psychiatry 1991; 148:345-350Link, Google Scholar
104. Popkin MK, Callies AL, Mackenzie TB: The outcome of antidepressant use in the medically ill. Arch Gen Psychiatry 1985; 42:1160-1163Crossref, Medline, Google Scholar
105. Hall RC, Gardner ER, Stickney SK, LeCann AF, Popkin MK: Physical illness manifesting as psychiatric disease, II: analysis of a state hospital inpatient population. Arch Gen Psychiatry 1980; 37:989-995Crossref, Medline, Google Scholar
106. Costa D, Mogos I, Toma T: Efficacy and safety of mianserin in the treatment of depression of women with cancer. Acta Psychiatr Scand 1985; 72:85-92Crossref, Google Scholar
107. Schiffer RB, Wineman NM: Antidepressant pharmacotherapy of depression associated with multiple sclerosis. Am J Psychiatry 1990; 147:1493-1497Link, Google Scholar
108. Borson S, McDonald GJ, Gayle T, Deffebach M, Lakshminarayan S, Tuinen CV: Improvement in mood, physical symptoms, and function with nortriptyline for depression in patients with chronic obstructive pulmonary disease. Psychosomatics 1992; 33:190-201Crossref, Medline, Google Scholar
109. Wiart L, Petit H, Joseph PA, Mazaux HM, Barat M: Fluoxetine in early poststroke depression: a double-blind placebo-controlled study. Stroke 2000; 8:1829-1832Crossref, Google Scholar
110. Andersen G, Vestergaard K, Lauritzen L: Effective treatment of poststroke depression with the selective serotonin reuptake inhibitor citalopram. Stroke 1994; 25:1099-1104Crossref, Medline, Google Scholar
111. Lustman PJ, Griffith LS, Clouse RE, Freedland KE, Eisen SA, Rubin EH, Carney RM, McGill JB: Effects of nortriptyline on depression and glycemic control in diabetes: results of a double-blind, placebo-controlled trial. Psychosom Med 1997; 59:241-250Crossref, Medline, Google Scholar
112. Lustman PJ, Freedland KE, Griffith LS, Clouse RE: Fluoxetine for depression in diabetes: a randomized double-blind placebo-controlled trial. Diabetes Care 2000; 23:618-623Crossref, Medline, Google Scholar
113. Strikk JJ, Honig A, Lousberg R, Lousberg AH, Cheriex EC, Tuynman-Qua HG, Kuipers PM, Wellens HJ, Praag HMV: Efficacy and safety of fluoxetine in the treatment of patients with major depression after first myocardial infarction: findings from a double-blind placebo-controlled trial. Psychosom Med 2000; 62:783-789Crossref, Medline, Google Scholar
114. Small GW, Birkett M, Meyers BS, Koran LM, Bystritsky A, Nemeroff CB: Impact of physical illness on quality of life and antidepressant response in geriatric major depression. J Am Geriatr Soc 1996; 44:1220-1225Crossref, Medline, Google Scholar
115. Rifkin A, Reardon G, Siris S, Karagji B, Kim YS, Hackstaff L, Endicott N: Trimipramine in physical illness with depression. J Clin Psychiatry 1985; 46:4-8Medline, Google Scholar
116. Reifler BV, Teri L, Raskind M, Veith R, Barnes R, White E, McLean P: Double-blind trial of imipramine in Alzheimer’s disease patients with and without depression. Am J Psychiatry 1989; 146:45-49Link, Google Scholar
117. Robertson MM, Trimble MR: The treatment of depression in patients with epilepsy. J Affect Disord 1985; 9:127-131Crossref, Medline, Google Scholar
118. Thase ME, Rush AJ: Treatment resistant depression, in Psychopharmacology: The Fourth Generation of Progress. Edited by Bloom F, Kupfer DJ. New York, Raven Press, 1995, pp 1081-1097Google Scholar
119. Rickels K, Gordon P, Jenkins BW, Perloff M, Sachs T, Stepansky W: Drug treatment in depressive illness. Dis Nerv Syst 1970; 1:30-42Google Scholar
120. Moertel CG, Taylor WF, Roth A, Tyce FAJ: Who responds to sugar pills? Mayo Clin Proc 1976; 51:96-100Medline, Google Scholar
121. Trivedi MH, Rush J: Does a placebo run-in or a placebo treatment cell affect the efficacy of antidepressant medications? Neuropsychopharmacology 1994; 11:33-43Crossref, Medline, Google Scholar
122. Jones MB, Ainslie JD: Value of a placebo wash-out. Dis Nerv Syst 1966; 27:393-396Google Scholar
123. Reimherr FW, Ward MF: The introductory placebo washout: a retrospective evaluation. Psychiatry Res 1989; 30:191-199Crossref, Medline, Google Scholar
124. Molcan J, Heretik V, Novotny K, Vajdickova K, Zucha I: The influence of experience with placebo on the placebo effect. Act Nerv Super (Praha) 1981; 23:184-185Google Scholar
125. Thompson J, Rankin H, Ashcroft GW, Yates CM, McQueen J, Cummings SW: The treatment of depression in general practice: a comparison of l-tryptophan, amitriptyline, and a combination of l-tryptophan and amitriptyline with placebo. Psychol Med 1982; 12:741-751Crossref, Medline, Google Scholar
126. Rosenthal R: The “file drawer problem” and tolerance for null results. Psychol Bull 1979; 86:638-641Crossref, Google Scholar



