The Detection and Treatment of Psychiatric Disorders and Substance Use Among Pregnant Women Cared for in Obstetrics
Abstract
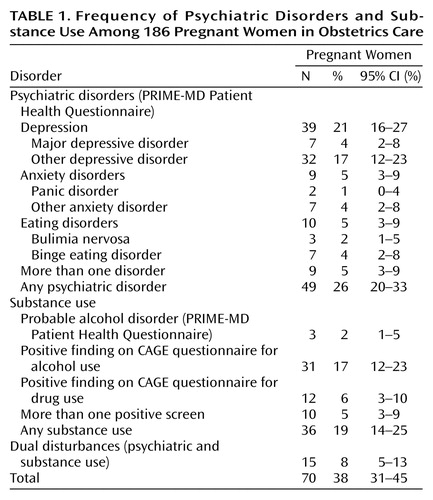
OBJECTIVE: This investigation assessed the detection and treatment of psychiatric disorders and at-risk substance use among pregnant women in the obstetric sector. METHOD: The Primary Care Evaluation of Mental Disorders Patient Health Questionnaire and modified CAGE questionnaires were used to assess current psychiatric disorders and at-risk substance use among 186 women receiving prenatal care. Medical records were reviewed for evidence of obstetrical providers’ recognition of psychiatric and substance use symptoms and diagnoses and initiation of evaluations and treatments. The associations between patient characteristics and chart-documented evaluations and treatments were ascertained. RESULTS: Seventy (38%) of the women met screening criteria for psychiatric disorders or substance use. Among women who screened positive, symptoms were recorded in 43% of the charts, diagnoses in 18%, evaluations in 35%, and treatments in only 23% Patients who screened positive for psychiatric disorders and/or substance use were significantly more likely to have a documented mental health evaluation if they were less well educated, had inadequate prenatal care, or had longer hospital stays at delivery. CONCLUSIONS: A substantial number of women treated in obstetrics have unrecognized and untreated psychiatric disorders and substance use. Given the potential impact of antenatal mental disturbances on maternal and infant outcomes, further investigations into the psychiatric evaluation and treatment of pregnant women in the obstetrical sector are required.
Over the past two decades, a series of investigations have assessed the detection, treatment, and outcomes of patients with psychiatric and substance use disorders in primary care (1–3). Reports (4–6) suggest that rates of psychiatric disturbances among pregnant women are similar to rates for women in the general population (7) and for women cared for in primary care (8). Although 3.9 million women deliver in the United States each year, few investigations have examined the detection and treatment of patients with mental disturbance in the obstetric sector.
A recent population-based investigation (9) found that psychiatric and substance use disorders were significantly underrecorded on hospital delivery records among all women delivering in California in 1992. In addition, women with chart-documented mental disorders at delivery had a twofold higher risk of inadequate prenatal care (10). However, conclusions drawn from hospital discharge data are limited by the inability to validate psychiatric diagnoses and to assess the processes of mental health care, including the temporal frame of diagnosis and provider recognition and treatment patterns throughout prenatal and hospital delivery care.
Only recently have screening tools for the detection of psychiatric and substance use disorders been developed for women cared for in gynecology and obstetrics (11, 12). Prenatal substance use screening by obstetricians has become an established public health priority (13), because of the high estimated prevalences of alcohol (18.8%) and illicit drug (5.5%) use during pregnancy among U.S. women (14). Self-report screening instruments are recommended for identifying prenatal alcohol use (15, 16). One investigation (12) found that questionnaires correctly identified 65%–70% of current prenatal drinkers, but only 20% of these patients had documentation of alcohol use in the obstetrical record.
Recent clinical studies of predominantly gynecologic outpatients have validated a primary care screening instrument for the detection of psychiatric disorders (17) and have documented high prevalences among this patient group (17–19). Spitzer et al. (17), utilizing the Primary Care Evaluation of Mental Disorders (PRIME-MD) Patient Health Questionnaire, found that approximately 20% of obstetrics/gynecology outpatients (N=3,000) met criteria for psychiatric diagnoses, and 77% of this group were not recognized by their obstetrics/gynecology provider. Two studies in ethnically diverse public-sector gynecology clinics found that between 48% and 73% of women met PRIME-MD criteria for psychiatric diagnoses (18, 19); of these women, less than one-third reported participation in mental health treatment, despite the vast majority expressing interest in receiving services (19). These investigations did not focus on pregnant populations, nor did they incorporate medical record review as a tool for quality assessment.
Medical record review, using implicit and explicit criteria, has been utilized to assess processes and quality of care both in the general health and mental health sectors (20, 21). Assessments of the quality of mental health care delivery routinely combine multiple data sources, including chart review, patient and provider reports, and computerized review of administrative data (15, 21, 22).
Because untreated maternal psychiatric and substance use disturbances during pregnancy and the perinatal period can adversely affect both mothers and infants (23–25), pregnant women represent a particularly vulnerable population that warrants an intensive investigative focus. This investigation focused specifically on a cohort of pregnant women and used medical records review and mental health self-report screening instruments to assess the processes of care for women treated in the obstetrical sector.
The primary research questions were as follows:
1. What are the frequencies of psychiatric disorders and substance use among an ethnically diverse group of pregnant women receiving prenatal care in the obstetrics sector?
2. What proportion of pregnant women with psychiatric disorders and at-risk substance use have mental health symptoms, diagnoses, evaluations, or treatments documented in their prenatal and delivery charts?
3. What patient demographic and obstetrical factors predict the presence of psychiatric disorders, substance use, and detection and treatment by obstetrical providers?
4. Are women with antenatal psychiatric disorders and/or substance use more likely to underutilize prenatal care?
Method
Participants in this study were 186 pregnant English-speaking women over 18 years who were receiving prenatal care in a university-based obstetrics clinic. A total of 37% identified themselves as Caucasian, 18% as African American, 16% as Hispanic, 10% as Asian, 2% as Native American, and 18% as mixed race or other. A total of 18% of the subjects reported a language other than English spoken in the home. A total of 64% of the women were insured by Medi-Cal, 56% had more than a high school education, and 48% were not working outside the home or enrolled as a student. Approximately 50% of the women were living with a partner or spouse. More than one-half (56%) of the group described the current pregnancy as unexpected. At the time of enrollment, the mean gestational age was 25.8 weeks (SD=6.0).
All study procedures were approved by the institutional review board of the University of California, Davis. Eligible patients at the obstetrics clinic waiting for their glucose tolerance test in the clinical laboratory were approached by the principal investigator (R.H.K.) or by a laboratory technician trained in the administration of the study consent form and questionnaires. After a complete description of the study was provided, written informed consent was obtained from all subjects. Each subject was administered a questionnaire packet and paid $5.00. Two women who were approached refused to participate, and one woman chose to discontinue participation after beginning the questionnaire. After delivery, each subject’s medical record for the period of the index pregnancy and delivery was reviewed.
Psychiatric Disorders
The PRIME-MD Patient Health Questionnaire (11) was used to assess current psychiatric disorders. This self-report measure assesses eight categories of mental disorders in primary care patients: major depressive disorder, other depressive disorder, panic disorder, other anxiety disorder, probable alcohol abuse/dependence, somatoform disorder, bulimia nervosa, and binge eating disorder. The temporal frame of Patient Health Questionnaire diagnoses are based on DSM-IV criteria: depressive symptoms over the past 2 weeks, anxiety and somatic symptoms over the past 4 weeks, and eating disorder symptoms over the past 3 months. The Patient Health Questionnaire diagnosis of probable alcohol abuse/dependence is determined by patterns and consequences of use over the past 6 months. There is good agreement between Patient Health Questionnaire diagnoses and diagnoses made by structured clinical interviews in primary care (11) and obstetrics/gynecology (17) settings (for any Patient Health Questionnaire disorder, kappa=0.65).
We categorized women as having a psychiatric disorder at the time of screening if they met criteria for any Patient Health Questionnaire diagnosis except somatoform disorder (this diagnosis requires information regarding medical conditions) and probable alcohol abuse/dependence (this diagnosis was included in the substance use category). Questions regarding demographics and psychiatric history were also administered.
Substance Use
Given the importance of detecting antenatal alcohol and drug use, we administered the Alcohol and Drug CAGE questionnaires (26) in addition to the Patient Health Questionnaire alcohol questions. The four-item, self-report modified CAGE questionnaires use the year before knowing about pregnancy as the time frame; the stem of each of the four questions reads, “In the 12 months before you found out you were pregnant….” Both instruments have utility in detecting periconceptional alcohol and heavier drug use among pregnant women at a cutoff score of 1 (26).
We categorized women as screening positive for substance use if they met criteria for Patient Health Questionnaire probable alcohol abuse/dependence or had a positive screening on the Alcohol or Drug CAGE questionnaires. Temporally, this substance use category included retrospective self-reported drug or alcohol use in the 12-month period before pregnancy, as well as alcohol use during pregnancy (up to the time of questionnaire administration).
Obstetrical Detection and Treatment
After the birth of the infant, the detection and treatment of psychiatric and substance use disturbances were determined by chart review of obstetrical records. All obstetrics chart notes for the index pregnancy and delivery were reviewed, including notes by the following providers: physicians, nurse midwives, nurses, social workers, students, and other members of the prenatal or delivery team. In addition, all screening forms, checklists, questionnaires, and summaries completed during the index pregnancy were reviewed. Any nonobstetrics visit during the index pregnancy was also reviewed, including emergency department, mental health, primary care, or specialty care visits.
Chart-documented evidence of current mental health symptoms, diagnoses, evaluations, or treatments were categorized into the following domains:
1. Psychiatric symptoms: This was a broadly defined category that included any words, phrases, or checklist responses relating patient experiences of mood states, affects, or other psychiatric symptoms recorded by providers or patients at any point during the pregnancy, including during labor and delivery (e.g., “upset”).
2. Psychiatric diagnosis: Provider-recorded psychiatric diagnosis (e.g., depression); DSM or ICD-9 codes were not required.
3. Substance use symptoms: Again, a broadly defined category that included any patient or provider reference to use of illicit drugs, alcohol, or prescription drug abuse during pregnancy (e.g., “drinking occasionally”).
4. Substance use diagnosis: Provider-recorded substance use diagnoses (e.g., alcohol abuse); DSM or ICD-9 codes were not required.
5. Evaluation: Chart evidence of more in-depth assessment of psychiatric or substance use symptoms or diagnoses by any obstetrics team provider, including clinician assessments or brief counseling, social services assessments, chaplain consultations, and child protective services reports.
6. Psychiatric treatment: Chart evidence of direct intervention or referral, including psychiatric consultation, specialty or community mental health visit, psychotropic medication, or psychotherapy provided by any mental health, obstetrical, social service, child protective services, or other provider.
7. Substance use treatment: Chart evidence of direct intervention or referral for substance use treatment including psychiatric consultation, specialty or community mental health visit for substance use, medication, or substance use treatment or self-help program provided by any provider.
A manual outlining review procedures and the seven domains of obstetrics detection and treatment was developed a priori and then applied to the review of 10 charts. After revision of the manual, the principal investigator (R.H.K) completed the first 26 reviews. Subsequently, two obstetrics nurses with prior experience abstracting over 3,000 obstetrics charts underwent training, which consisted of manual-guided group review of five complete charts, with discrepancies resolved by consensus. After the training, interrater reliability was evaluated by assessing the chart reviewers’ ability to agree on provider recording of symptoms, diagnoses, evaluations, and treatments; the chart reviewers achieved 100% agreement and thereafter coded charts independently.
In addition to detection and treatment domains, urine toxicology screening reports, child protective services referrals, obstetrical history (number of pregnancies, number of spontaneous and elective abortions), and pregnancy outcome variables (birth weight, gestational age, length of maternal hospital stay) for the index pregnancy were abstracted. The adequacy of prenatal care was assessed by using the Kotelchuck Adequacy of Prenatal Care Utilization Index (27), which rates prenatal care as inadequate, intermediate, adequate, or adequate plus. Inadequate prenatal care utilization is defined as initiation after the fourth month of pregnancy or less than 50% of the recommended visits. Intermediate prenatal care is defined as initiation by the fourth month of pregnancy and between 50% and 79% of the recommended visits. Charts with incomplete prenatal care data were excluded from prenatal care analyses.
Statistical Analysis
We first ascertained the frequencies of psychiatric disorders and positive substance use screenings. We then ascertained the frequency of chart-recorded symptoms, diagnoses, evaluations, and treatments among women with psychiatric disorders and those with at-risk substance use.
Next, we computed the bivariate associations between demographic, obstetrical, and other maternal variables and psychiatric disorders and substance use using the chi-square statistic or Fisher’s exact test (if cell size was fewer than 5) for categorical variables and t tests for continuous variables. Because of the distributions of certain variables (number of pregnancies, spontaneous abortions, elective abortions, and length of hospital stay), Mann-Whitney U tests were performed; we report the median and range for these variables. There were few significant differences between the two groups; excluding women with dual disturbances, women who screened positive for substance use were more likely to have an unexpected pregnancy and to be referred to child protective services, and women with psychiatric disorders were more likely to have had more prior pregnancies and elective abortions. For all subsequent analyses we combined women with psychiatric disorders and/or substance use into a single category.
For the combined category of women with psychiatric disorders and/or substance use, we examined the chart-recorded frequencies of any psychiatric or substance use symptoms, diagnoses, evaluations, or treatments; we then examined the bivariate associations between demographic and obstetrical variables and chart-recorded psychiatric or substance use detection and treatment domains using the chi-square statistic or Fisher’s exact test for categorical variables and t tests or the Mann-Whitney U test for continuous variables. For all proportions, 95% confidence intervals (CIs) were calculated. The statistical software package SPSS version 9.0 was used for all data analyses (28).
Prenatal or delivery records were missing or incomplete for 21 (11%) of the subjects. There were no significant differences in demographic or clinical characteristics or frequency of psychiatric diagnoses or substance use between patients with complete and incomplete charts. Excluding patients with incomplete records did not substantially affect the bivariate comparisons; therefore, data reported are for the full study group.
Results
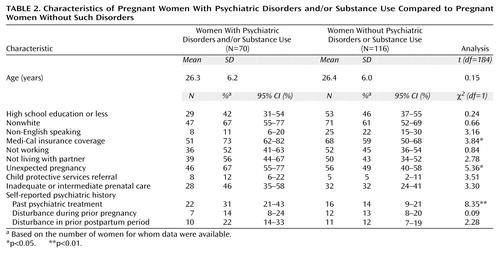
A total of 70 (38%) of the women screened positive for psychiatric disorders and/or substance use (Table 1). Women with psychiatric disorders or substance use were significantly more likely to have Medi-Cal insurance coverage, to report an unexpected pregnancy, and to have a history of psychiatric treatment than women with negative screening results (Table 2). The likelihood of a psychiatric disorder and/or substance use did not vary by level of education, racial background, primary language spoken, whether living with a partner, whether working outside the home, or age. Women with psychiatric disorders and/or substance use were more likely to have inadequate or intermediate prenatal care (p<0.07) and to be referred to child protective services during the index pregnancy (p<0.08) than women with negative screenings, although these values were not statistically significant (Table 2). There were no significant differences in obstetrical history or selected obstetrical outcomes between women who screened positive and women who screened negative for disorders.
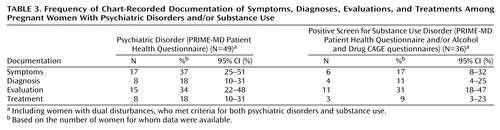
Among all 70 women who screened positive (i.e., women with psychiatric disorders and/or substance use), psychiatric or substance use symptoms were recorded in the charts of 29 of 68 women (43%, 95% CI=32%–55%), diagnosis in 12 of 68 (18%, 95% CI=11%–29%), evaluation in 23 of 66 (35%, 95% CI=25%–47%), and psychiatric or substance use treatment in 15 of 66 (23%, 95% CI=15%–34%). The women with documented symptoms (N=29) often had more than one symptom recorded: 17 (59%) had depressive symptoms, 17 (59%) had anxiety symptoms, eight (28%) had substance use symptoms, three (10%) had agitation/behavioral symptoms, three (10%) had sleep disorder symptoms, and one (3%) had eating disorder symptoms. The obstetrical team obtained urine toxicology screenings for 21 (11%) of the women prenatally and 139 of 175 (79%) of the women at delivery, resulting in three positive prenatal and one positive delivery screenings.
Table 3 presents the frequency of chart-recorded symptoms, diagnoses, evaluations, and treatments for women who screened positive for psychiatric disorders and/or substance use. Approximately one in five women with psychiatric disorders had chart documentation of psychiatric treatment. One in three women who screened positive for substance use had evidence of a psychosocial evaluation.
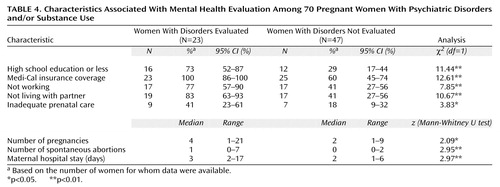
We also assessed patient characteristics that predicted chart-documented mental health or substance abuse evaluation and treatment. Patients with psychiatric disorders or substance use were more likely to be evaluated if they had less education, had Medi-Cal insurance coverage, were not working outside the home or living with a partner, had inadequate prenatal care, had had more prior pregnancies or spontaneous abortions, or had a longer hospital delivery stay (Table 4). The likelihood of receiving a mental health evaluation did not vary by age, race, or obstetrical outcome.
Among women with psychiatric disorders or substance use, in a comparison of 15 treated and 55 nontreated patients, the only predictors of chart-recorded mental health or substance abuse treatment were not living with a partner (treated patients: 80%, 95% CI=55%–93%; nontreated patients: 48%, 95% CI=35%–61%) (χ2=4.78, df=1, p<0.03), referral to child protective services during the index pregnancy (treated patients: 40%, 95% CI=20%–64%; nontreated patients: 4%, 95% CI=1%–13%) (p<0.001, Fisher’s exact test), and more prior spontaneous abortions (treated patients: median=1, range=0–3; nontreated patients: median=0, range=0–7) (z=2.36, p<0.02).
Discussion
To our knowledge, this is the first investigation to use medical record review in conjunction with validated psychiatric screening instruments to examine the detection and treatment of mental disturbances among pregnant women cared for in the obstetrical sector. Nearly 40% of the women in our group had high levels of symptoms likely to be associated with psychiatric disorders or substance use; this is comparable to prevalence rates documented among nonpregnant public-sector gynecology patients (18) and primary care populations (8). Approximately one in five pregnant women met screening criteria concerning levels of drug or alcohol use before or during pregnancy. Of all women who screened positive for psychiatric disorders or substance use, over one-half met criteria for a depressive disorder.
Despite this high frequency of psychiatric and substance use disturbance, chart-recorded detection (of symptoms or diagnoses) was evident in less than one-half of the patients who screened positive. In addition, only one in four women who screened positive had chart-documented evidence of any mental health or substance abuse treatment, and only one in three had evidence of any psychosocial evaluation by an obstetrics team.
The results of this investigation also suggest that among women with psychiatric disorders and/or positive substance use screenings, concurrent pregnancy risk factors (e.g., inadequate prenatal care, more prior pregnancies), not living with a partner, and lower socioeconomic status increase the likelihood of chart-documented mental health evaluation or treatment. Prior research in the obstetrical sector has documented practice variations in the reporting of antenatal substance use on the basis of patient sociodemographic factors (6). In addition, we observed that obstetrics providers were much more likely to refer women for treatment in cases with child protective services involvement. A child protective services referral may suggest complex maternal disturbance, concern for the safety of the infant, or legally mandated treatment.
Our recent epidemiologic investigation (10) found that women with chart-documented psychiatric and substance use diagnoses at delivery were more likely to have received inadequate or no prenatal care. Although our results demonstrated that 46% (N=28) of the women who screened positive had poor prenatal care versus 32% (N=32) of the women who screened negative, this association was not statistically significant. Our study group, however, excluded women who received no prenatal care, as well as those who were noncompliant with glucose tolerance tests, which may have weakened the association between poor prenatal care and psychiatric and substance use disturbances. Furthermore, our group size may have limited the power to detect statistically significant differences.
This investigation has a number of limitations. First, although we had a priori hypotheses, we conducted multiple bivariate comparisons, thus increasing the likelihood of finding statistically significant associations. In addition, we assessed periconceptional substance use, not current substance use disorders. Thus, our results may overestimate the number of pregnant women requiring substance abuse treatment.This in turn could underestimate the actual rates of provider detection and treatment for substance use disorders. Using higher cutoff scores for CAGE questionnaire results may more accurately represent rates of antenatal disorder (cutoff scores of 2, 3, and 4 yield rates for the Alcohol CAGE questionnaire of 7.5%, 2.2%, and 0% and rates for the Drug CAGE of 4.3%, 2.2%, and 0%, respectively). However, research suggests that because pregnant women underreport substance use (29), methods to improve detection should focus on use before conception (15, 16). Periconceptional drug (14) and alcohol (14, 15) use predicts rates of use in the first trimester, as well as at 1 year postpartum (30, 31), and significant antenatal substance use is unlikely to change without intervention (6). In addition, national estimates (14) of the prevalence of drug (5.8%) and alcohol (20%) use during pregnancy among urban populations are very similar to the periconceptional frequencies we measured using the Drug (6.5%) and Alcohol (17%) CAGE questionnaires.
Prior studies have demonstrated that medical charts underestimate physician recognition and treatment of mental disorders in primary care; various explanations have been proposed, including deficiencies in practitioner knowledge to diagnose specific psychiatric disorders (1) and provider concerns regarding patient confidentiality (1, 32). An alternative strategy for assessing processes of care is to implement provider interviews. However, obstetrics/gynecology provider questionnaires at the time of (predominantly nonpregnant) patient encounters have shown similar rates of underrecognition (77%); low treatment rates (32%) persisted even after providers were informed of patient diagnoses (17). Conversely, our broad definition of chart-documented symptoms may overestimate provider detection. Chart-documented diagnoses, psychosocial evaluations, or treatments may more accurately estimate detection.
Although we found no association between positive psychiatric and substance use screenings and poor pregnancy outcomes, these data should be interpreted with caution; analyses did not control for potential confounding factors such as maternal smoking, medical illness, and prior premature delivery. In addition, our results, derived from a university obstetrics clinic serving low-income minority women, may not accurately reflect the prevalence of mental disturbance among the general population of pregnant women. Finally, our study screened for disorders at one point in time; some mental disturbance may have been transitory or developed after the screening point.
In summary, our findings suggest that a substantial proportion of women cared for in the obstetrical sector suffer psychiatric and substance use disturbances during pregnancy. These results demonstrate that underrecording of mental disturbance is not limited to hospital discharge records (9, 10) but exists throughout prenatal care and is accompanied by low documented rates of mental health evaluation and treatment. These data suggest that pregnant women suffering from psychiatric and substance use disturbances are underdetected and undertreated by obstetrical providers.
The high frequency of disturbance and low rate of provider detection and treatment are especially of concern among this population, given that untreated psychiatric and substance use illnesses during pregnancy can have untoward consequences for both maternal and infant health (23–25). Further research is needed to identify predictors and outcomes of nonrecognition and treatment and to develop interventions that aim to improve the quality of care for women suffering from antenatal mental disturbance in the obstetrical sector.
 |
 |
 |
 |
Received Jan. 6, 2000; revision received June 27, 2000; accepted Sept. 6, 2000. From the Department of Psychiatry, University of California, Davis; and the Department of Psychiatry, University of Washington Medical Center. Address reprint requests to Dr. Kelly, Department of Psychiatry, University of Washington Medical Center, Box 356560, 1959 Pacific Ave., N.E., Seattle, WA 98195; [email protected] (e-mail). Supported by an NIMH National Research Service Award (MH-11892) (Dr. Kelly) and NIMH grants MH-01610 (Dr. Zatzick) and MH-50741 (Dr. Anders). The authors thank Wayne Katon, M.D., and Joan Russo, Ph.D., of the University of Washington and Evette Ludman, Ph.D., of the Center for Health Studies, Group Health Cooperative of Puget Sound, for their contributions to the article.
1. Jencks SF: Recognition of mental distress and diagnosis of mental disorder in primary care. JAMA 1985; 253:1903–1907Google Scholar
2. Wells KB, Hays RD, Burnam MA, Rogers W, Greenfield S, Ware JE Jr: Detection of depressive disorder for patients receiving prepaid or fee-for-service care: results from the Medical Outcomes Study. JAMA 1989; 262:3298–3302Google Scholar
3. Schulberg HC, Magruder KM, deGruy F: Major depression in primary medical care practice: research trends and future priorities. Gen Hosp Psychiatry 1996; 18:395–406Crossref, Medline, Google Scholar
4. Gotlib IH, Whiffen VE, Mount JH, Milne K, Cordy NI: Prevalence rates and demographic characteristics associated with depression in pregnancy and the postpartum. J Consult Clin Psychol 1989; 57:269–274Crossref, Medline, Google Scholar
5. O’Hara MW: Social support, life events, and depression during pregnancy and the puerperium. Arch Gen Psychiatry 1986; 43:569–573Crossref, Medline, Google Scholar
6. Chasnoff IJ, Landress HJ, Barrett ME: The prevalence of illicit drug or alcohol use during pregnancy and discrepancies in mandatory reporting in Pinellas County, Florida. N Engl J Med 1990; 332:1202–1206Google Scholar
7. Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen H, Kendler KS: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Arch Gen Psychiatry 1994; 51:8–19Crossref, Medline, Google Scholar
8. Williams J, Spitzer R, Linzer M, Kroenke K, Hahn S, deGruy F, Lazev A: Gender differences in depression in primary care. Am J Obstet Gynecol 1995; 173:654–659Crossref, Medline, Google Scholar
9. Kelly RH, Danielsen BH, Zatzick DF, Haan MN, Anders TF, Gilbert WM, Burt VK: Chart-recorded psychiatric diagnoses in women giving birth in California in 1992. Am J Psychiatry 1999; 156:955–957Link, Google Scholar
10. Kelly R, Danielsen B, Golding J, Anders T, Gilbert W, Zatzick D: Adequacy of prenatal care among women with psychiatric diagnoses giving birth in California in 1994 and 1995. Psychiatr Serv 1999; 50:1584–1590Google Scholar
11. Spitzer R, Kroenke K, Williams J: Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. JAMA 1999; 282:1737–1744Google Scholar
12. Chang G, Goetz M, Wilkins-Haug L, Berman S: Identifying prenatal alcohol use: screening instruments versus clinical predictors. Am J Addict 1999; 8:87–93Crossref, Medline, Google Scholar
13. Stratton K, Howe C, Battaglia F (eds): Institute of Medicine Summary: Fetal Alcohol Syndrome. Washington, DC, National Academy Press, 1996Google Scholar
14. National Pregnancy and Health Survey: Drug Use Among Women Delivering Livebirths:1992: NIH Publication 96-3819. Rockville, Md, Department of Health and Human Services, National Institute on Drug Abuse, 1996Google Scholar
15. Chang G, Wilkins-Haug L, Berman S, Goetz M, Behr H, Hiley A: Alcohol use and pregnancy: improving identification. Obstet Gynecol 1998; 91:892–898Crossref, Medline, Google Scholar
16. Russel M, Martier S, Sokol R, Mudar P, Jacobson S, Jacobson J: Detecting risk drinking during pregnancy: a comparison of four screening questionnaires. Am J Public Health 1996; 86:1435–1439Google Scholar
17. Spitzer RL, Williams JB, Kroenke K, Hornyak R, McMurray J: Validity and utility of the PRIME-MD patient health questionnaire in assessment of 3000 obstetric-gynecologic patients: the PRIME-MD Patient Health Questionnaire Obstetrics-Gynecology Study. Am J Obstet Gynecol 2000; 183:759–769Crossref, Medline, Google Scholar
18. Miranda J, Azocar F, Komaromy M, Golding J: Unmet mental health needs of women in public-sector gynecologic clinics. Am J Obstet Gynecol 1998; 178:212–217Crossref, Medline, Google Scholar
19. Alvidrez J, Azocar F: Distressed women’s clinic patients: preferences for mental health treatments and perceived obstacles. Gen Hosp Psychiatry 1999; 21:340–347Crossref, Medline, Google Scholar
20. Donabedian A: The Definition of Quality and Approaches to Its Assessment: Explorations in Quality Assessment and Monitoring. Ann Arbor, Mich, Health Administration Press, 1980Google Scholar
21. McGlynn E, Norquist G, Wells K, Sullivan G, Liberman R: Quality-of-care research in mental health: responding to the challenge. Inquiry—Blue Cross and Blue Shield Association 1988; 25:157–170Google Scholar
22. Young A, Sullivan G, Burnam A, Brook R: Measuring the quality of outpatient treatment for schizophrenia. Arch Gen Psychiatry 1998; 55:611–617Crossref, Medline, Google Scholar
23. Steer RA, Scholl TO, Hediger ML, Fischer RL: Self-reported depression and negative pregnancy outcomes. J Clin Epidemiol 1992; 45:1093–1099Google Scholar
24. Zuckerman B, Bauchner H, Parker S, Cabral H: Maternal depressive symptoms during pregnancy, and newborn irritability. J Dev Behav Pediatr 1990; 11:190–194Crossref, Medline, Google Scholar
25. Weinberg M, Tronick E: The impact of maternal psychiatric illness on infant development. J Clin Psychiatry 1998; 59(suppl 2):53–61Google Scholar
26. Midanik LT, Zahnd EG, Klein D: Alcohol and drug CAGE screeners for pregnant, low-income women: the California Perinatal Needs Assessment. Alcohol Clin Exp Res 1998; 22:121–125Crossref, Medline, Google Scholar
27. Kotelchuck M: An evaluation of the Kessner Adequacy of Prenatal Care Index and a proposed Adequacy of Prenatal Care Utilization Index. Am J Public Health 1994; 84:1414–1420Google Scholar
28. SPSS 9.0 for Windows. Chicago, SPSS, 1998Google Scholar
29. Sokol R, Martier S, Ager J: The T-ACE questions: practical prenatal detection of risk-drinking. Am J Obstet Gynecol 1989; 160:863–871Crossref, Medline, Google Scholar
30. Fried P, Barnes M, Drake E: Soft drug use after pregnancy compared to use before and during pregnancy. Am J Obstet Gynecol 1985; 151:787–792Crossref, Medline, Google Scholar
31. Gilchrist L, Hussey J, Gillmore M, Lohr M, Morrison D: Drug use among adolescent mothers: prepregnancy to 18 months postpartum. J Adolesc Health 1996; 19:337–344Crossref, Medline, Google Scholar
32. Rost K, Smith G, Matthews D, Guise B: The deliberate misdiagnosis of major depression in primary care. Arch Fam Med 1994; 3:333–337Crossref, Medline, Google Scholar



