Screening for and Detection of Depression, Panic Disorder, and PTSD in Public-Sector Obstetric Clinics
Abstract
OBJECTIVE: This study assessed rates of detection and treatment of minor and major depressive disorder, panic disorder, and posttraumatic stress disorder among pregnant women receiving prenatal care at public-sector obstetric clinics. METHODS: Interviewers systematically screened 387 women attending prenatal visits. The screening process was initiated before each woman's examination. After the visit, patients were asked whether their clinician recognized a mood or anxiety disorder. Medical records were reviewed for documentation of psychiatric illness and treatment. RESULTS: Only 26 percent of patients who screened positive for a psychiatric illness were recognized as having a mood or anxiety disorder by their health care provider. Moreover, clinicians detected disorders among only 12 percent of patients who showed evidence of suicidal ideation. Women with panic disorder or a lifetime history of domestic violence were more likely to be identified as having a psychiatric illness by a health care provider at some point before or during pregnancy. All women who screened positive for panic disorder had received or were currently receiving mental health treatment outside the prenatal visit, whereas 26 percent of women who screened positive for major or minor depression had received or were currently receiving treatment outside the prenatal visit. CONCLUSIONS: Detection rates for depressive disorders in obstetric settings are lower than those for panic disorder and lower than those reported in other primary care settings. Consequently, a large proportion of pregnant women continue to suffer silently with depression throughout their pregnancy. Given that depressive disorders among perinatal women are highly prevalent and may have profound impact on infants and children, more work is needed to enhance detection and referral.
Approximately 21 percent of women experience a mood disorder and 30 percent an anxiety disorder at some point in their lives (1). Although historically it was believed that pregnant women were at lower risk of mood and anxiety disorders (2,3), recent studies do not support this belief. Rather, between 10 and 27 percent of women experience depressive symptoms during pregnancy (2,4,5,6,7,8,9,10,11,12,13,14), including 2 to 11 percent who experience major depressive disorder (2,15,16,17). It remains to be determined whether rates of anxiety syndromes differ between gravid and nongravid women.
Regardless of whether pregnancy influences the course of depressive or anxiety disorders, obstetric practitioners frequently encounter women with these conditions. The disorders are especially common among women with low incomes, who often obtain health care only when they are pregnant and are covered by health insurance that is not available to them at other times. In fact, more than 60 percent of women with low incomes receive health care exclusively from their obstetric clinician (18).
Nevertheless, less attention has been devoted to the detection and treatment of mood and anxiety disorders among obstetric-gynecologic patients (19,20,21,22,23). In a recent study of 3,000 obstetric and gynecology patients, 20 percent of the patients met criteria for a psychiatric diagnosis, but among 77 percent of the patients a disorder was not recognized by their health care provider (22). The only study to prospectively investigate rates of identification of psychiatric illness and referral for depression, anxiety, and substance abuse among pregnant patients (24) found that half of patients who screened positive for a psychiatric diagnosis in an independent screening did not receive a diagnosis from their physicians and that three-quarters were not treated. No study of pregnant women has presented detection rates specific to type of psychiatric illness; nor has any study examined detection and referral for posttraumatic stress disorder (PTSD).
The main aim of the study reported here was to extend previous findings by systematically evaluating rates of detection and treatment of minor and major depressive disorder, panic disorder, and PTSD among women receiving prenatal care at publicly supported clinics.
Methods
Sample and data collection
Women were eligible to participate in the study if they were pregnant, spoke English or Spanish, and were receiving prenatal care from either of the two federally funded hospital-based obstetric clinics or two affiliated community health center obstetric programs in the New Haven, Connecticut, area. A majority of the providers (25 providers, or 58 percent) administering prenatal care at the clinics were obstetrician-gynecologists. Seven providers (16 percent) were obstetric-gynecologic residents. Other providers included certified nurse midwives (ten providers, or 23 percent) and one physician assistant (2 percent). Four providers (9 percent) were bilingual in English and Spanish.
Pregnant women were approached during their usual prenatal appointment during a six-month period from November 2001 through April 2002 on selected clinic days that changed weekly, depending on patient flow. Prenatal care providers were told that a study of moods during pregnancy was being conducted at their clinic but were not specifically told that the study involved screening for depression, PTSD, or panic disorder. Institutional review board approval was obtained from Yale University and from each participating site's institutional review board. The women were asked to provide written informed consent after the study was fully explained.
The women were screened in a private section of the waiting room, an examination room, or a private office in the clinic and received a package of diapers on completion of the interview. Screening occurred only once, at any point in the pregnancy; this approach yielded cross-sectional rates of illness. Participants included 387 pregnant women, or 98 percent of those approached. Women were on average 23.8±11.2 weeks pregnant when evaluated (range, 6.7 to 41.1 weeks). Eighty women (23 percent) were seen during the first trimester, 144 (34 percent) during the second trimester, and 163 (43 percent) during the third trimester. If suicidal ideation was identified at any point during the screening process, the patient's health care provider was notified.
Measures
Trained research assistants (social workers with educational qualifications ranging from B.A. to M.S.W.) administered a structured questionnaire before each patient saw her health care provider. The questionnaire collected information about psychiatric history (whether the participant had previously received a diagnosis of depression, anxiety, PTSD, or any other mental disorder), the patient's awareness of the clinician's diagnosis, the time at which a diagnosis was made (more than a year ago, during the current pregnancy, or during the previous year but not during current pregnancy), and whether the participant had received mental health treatment. All questionnaires were administered in an interview format. A total of 107 screenings (28 percent) were conducted in Spanish.
All patients were administered the Primary Care Evaluation of Mental Disorders (PRIME-MD) Brief Patient Health Questionnaire (BPHQ) (25,26), which recorded diagnoses of major depressive disorder, minor depressive disorder, or panic disorder. This questionnaire was augmented with the PTSD module from the MINI International Neuropsychiatric Interview (MINI) (27). The BPHQ and the MINI have been independently validated (22,26,27). The BPHQ has been used in obstetric-gynecologic settings and correlates highly with the Structured Clinical Interview for DSM-III-R (SCID). The overall reliability between the BPHQ and the SCID for major depressive disorder was 92 percent, for minor depression was 89 percent, and for panic disorder was 96 percent (26). Both the BPHQ and the MINI have been validated in Spanish (22,28).
A diagnosis of major depressive disorder was assigned to women who met a minimum of five of the DSM-IV criteria, including either depressed mood or anhedonia, for more than half the days in a two-week interval. A diagnosis of minor depression was made for women who endorsed two to four symptoms of depression, including depressed mood or anhedonia, for more than half the days in a minimum period of two weeks. A diagnosis of panic disorder was given to women who responded "yes" to the following four items: they experienced a panic attack, the attack "came out of the blue," the attack resulted in a change of behavior, and the attack was associated with somatic symptoms. A diagnosis of PTSD was made for traumatized women who responded "yes" to reexperiencing a traumatic event and at least four PTSD symptoms—irritability, avoidance, amnesia, detachment, dissociation, foreshortened future, difficulty concentrating, and easily startled—for "several days" or more. A time frame of one month was applied for panic disorder and PTSD.
Study participants were questioned again after their prenatal visit and were asked whether they had discussed depression, panic, posttraumatic stress disorder, or any other mental disorder with their health care provider. In addition, they were asked whether they had been referred for treatment.
A medical record review using a standardized form of the patient's prenatal chart and entire medical record both from the prenatal care site and from the hospital at which the patient delivered was also performed to identify clinicians' documentation of psychiatric illness, treatment for a psychiatric illness, number of prenatal care visits attended, presence of domestic violence (previous or current), pregnancy history, major medical illnesses, and other medical problems during the current pregnancy.
Data for women who screened positive on the BPHQ for minor or major depression, PTSD, or panic disorder (N=99) were combined to assess the women as a group for current and previous health care use. If the patient's medical record documented symptoms, even when no treatment was indicated, the patient was considered to have a mental condition.
Statistical analysis
The frequencies of depressive disorder, panic disorder, and PTSD were calculated. Differences in the prevalence of mood disorders between racial or ethnic groups were examined by using chi square tests calculated by using SAS (29). There were too few women with anxiety disorders to explore differences in rates between racial or ethnic groups.
Bivariate associations between illness identification and other maternal demographic and medical risk variables, including psychiatric disorders, were computed for the cohort of 387 women by using the chi square statistic or, for expected cell sizes of less than 5, Fisher's exact test. Logistic regression (proc logistic) was used to determine which variables increased the likelihood of case identification by any health care provider among the 99 women who screened positive for a disorder. Independent variables entered into the model included those that were significant at a .1 level on bivariate testing. The final model included covariates significant at .05 or variables that were effect modifiers. For all nine women with panic disorder, the disorder was detected before or at the time of screening, bivariate odds ratios were not computed. Therefore, the combined independent variable of PTSD or panic disorder was entered into the model.
Results
The mean±SD number of prenatal care appointments women attended at the time of screening was 6±4.4. A majority of the cohort was African American or Hispanic and insured through Medicaid.
Illness rates
Nearly a quarter of the women assessed (90 women, or 23 percent) screened positive at their prenatal visit for a current depressive disorder, nine (2 percent) screened positive for panic disorder, and ten (3 percent) screened positive for PTSD, as can be seen in Table 1. Seventeen women (19 percent) who screened positive for a depressive disorder replied "sometimes" or "more than half the days" when asked whether they had had thoughts about harming themselves. Ten women (3 percent) had a depressive and comorbid psychiatric disorder at assessment. The most common concomitant psychiatric disorders were depressive disorders with PTSD (five women, or 1 percent). Demographic and medical characteristics of the women screened are summarized in Table 2.
Significant differences were found in rates of depression between racial groups. Forty-seven African-American women (31 percent) were found to have a mood disorder, including 11 (7 percent) who had major depressive disorder and 32 (23 percent) who had minor depressive disorder. Among Hispanic women, 32 (19 percent) met criteria for a mood disorder—nine (6 percent) for major depressive disorder and 23 (14 percent) for minor depressive disorder. The difference between the African-American and Hispanic groups for minor depressive disorder was significant (χ2=4.76, df=1, p=.03).
Illness detection by prenatal care provider
Ninety-nine women (26 percent) scored positive for a depressive disorder or an anxiety disorder before their prenatal care visit. Patient questionnaires showed that only two women with a depressive disorder (2 percent) were identified or referred for treatment during their prenatal visit (Table 1). In addition, only two of the 17 women who showed evidence of suicidal ideation were detected or referred for treatment by their clinician at their prenatal visit. For the anxiety disorders, one woman with panic disorder was identified and referred for care. However, none of the ten women with PTSD were identified by a health care provider at the prenatal visit.
Although none of the women who screened positive for PTSD at their prenatal visit were identified by a health care professional, three women who did not screen positive for PTSD were given this diagnosis by their clinician; two of these women were referred for treatment. It was discovered on review of the medical records of these three women that two of the women had told their prenatal care provider that they were in domestic violence situations and needed treatment. Both women were referred to domestic violence services.
Lifetime treatment
Among the 387 women who were screened, the prenatal medical records and patient self-reports indicated that 56 (15 percent) had previous or current treatment for a psychiatric illness. As shown in Table 2, at the time of screening, 26 (26 percent) of all women who screened positive for a mental diagnosis were receiving or had received treatment according to their medical record or patient self-report. For 24 women with a diagnosis of a depressive disorder (27 percent), treatment was documented in the record. Five (50 percent) of the women who screened positive for PTSD and all nine (100 percent) of the women who screened positive for panic disorder either reported receiving treatment or had documentation of treatment in their medical record (Table 2).
The bivariate analyses of data for the 99 women who screened positive for a psychiatric disorder, presented in Table 3, showed a significant association between identification of a depressive or anxiety disorder and the following variables: race (white versus not white), number of psychiatric diagnoses (one or more than one), previous adverse perinatal outcome, substance use (previous or current use of alcohol or drugs), domestic violence (previous or current), minor depression, and PTSD or panic disorder.
The final logistic regression predicting which women were likely to be identified and referred for treatment is presented in Table 4. Women who screened positive for a psychiatric diagnosis and who reported current or lifetime domestic violence were almost five times as likely to be identified as having a psychiatric disorder at their prenatal visits (OR=5.75, 95 percent CI=1.71 to 19.28).
Discussion
Our findings show that mood and anxiety disorders are highly prevalent and constitute significant morbidity among low-income pregnant patients treated in publicly funded clinics. The rates of major depressive disorder (6 percent) and panic disorder (2 percent) found in this study are within the range of estimates reported elsewhere for low-income populations (7,17,18,24). To our knowledge, this is the first study to explore the likelihood that PTSD will be identified and treated in a pregnant population. The rate of PTSD we report (3 percent) was within the range reported in other epidemiologic studies. For example, the one-month prevalence of PTSD among women included in the National Comorbidity Survey was 2.8 percent.
In our cohort, all but a minority of symptomatic depressed women remained undiagnosed and untreated, despite the fact that women were seen an average of six times in as many months by a health care professional. This finding is even more sobering when one considers that 18 percent of women with undetected depression had suicidal ideation that was experienced at least several times a week. Only 2 percent of the women with a depressive disorder, none of the women with PTSD, and 11 percent of the women with panic disorder received a diagnosis from a health care professional at their prenatal visit.
When we evaluated rates of any detection of psychiatric illness, operationalized as patient report or documentation in the medical chart of any symptoms or treatment, only 26 percent of psychiatrically ill patients were recognized as having a mood or anxiety disorder. On the other hand, it is notable that all nine women who screened positive for panic disorder reported receiving mental health treatment before or at the time of screening. Rates of anxiety disorder detection in primary care settings are typically quite low (22). Therefore, it is unusual to find that the nine cases of panic disorder were detected in an obstetric setting. One reason may be that panic disorder typically presents in the form of physical symptoms, such as breathing difficulties or tightness in the chest, that can mimic catastrophic illnesses such as heart attacks or pulmonary emboli. It may be that prenatal health care providers are more watchful of serious general medical conditions that affect the mother or the fetus and thus thoroughly evaluate somatic symptoms like shortness of breath and chest pain.
Women were more likely to have their depressive or anxiety disorder identified by a health care provider if they reported previous or current domestic violence. Although this finding needs to be confirmed in a larger sample, it suggests that women with severe forms of psychosocial stress are more likely to receive a diagnosis. Kelly and associates (24) found a similar result in that concurrent pregnancy risk factors, such as not living with a partner, involvement of child protective services, and history of abortion, increased the likelihood of chart-documented mental health evaluation or treatment. Furthermore, detection could also be higher among women who have been the victims of domestic violence, because they are more likely to seek medical attention (30).
Although detection rates for depression in obstetric-gynecologic practices are moderate (15 percent to 30 percent) (19,20,21,22,23) and are somewhat lower than those for other primary care providers (35 percent to 56 percent) (31,32,33,34), the recognition of depressive and anxiety disorders among pregnant patients (27 percent) was less than that found in other reproductive health settings (22,24,32). One of the few studies to examine detection and treatment of depression, substance abuse, and panic disorder among pregnant women (N=186) noted that only 18 percent of those who had a diagnosis were identified by clinicians and that only 37 percent of those identified had any symptom recorded in the patient chart (24). Our results are in line with these findings, although we did find higher detection rates specifically for panic disorder and PTSD. Our study differed from the one mentioned above in that we used patients' self-reported diagnoses in addition to diagnostic information from medical record reviews to determine whether clinicians identified a patient as psychiatrically ill.
The low detection and referral rates for depression among pregnant patients may be a result of a number of factors. Clinicians may be reluctant to ask questions, and patients may avoid reporting problems that arise from depression or anxiety. Symptoms of depression during pregnancy may not raise clinicians' or patients' concerns given that several of these experiences—for example, disturbances in appetite, sleep, and energy levels—are normative for many pregnant women (15,35).
Other possible contributions include time constraints, insurance and referral limitations, and provider education and training. Large survey studies have shown that a majority of obstetric-gynecologic residents neither received training about clinical depression during their residency (80 percent) nor completed a continuing medical education course on the treatment of clinical depression among women (60 percent) (23,36). Approximately 50 percent of obstetrician-gynecologists cite incomplete knowledge of diagnostic criteria as a barrier to identification of depression (23). The expectation that obstetric and gynecologic practitioners will diagnose and treat common mental health disorders is of recent origin, and many providers may not think that it should be part of their clinical responsibilities (36).
In addition, as in other studies of primary care, nonpsychiatric providers may be less familiar with psychiatric diagnostic codes or may fear that patients will be stigmatized if they are given a chart-recorded diagnosis (37,38). In our cohort and in many obstetric settings, a large proportion of women see certified nurse midwives. It is not clear that the training of midwives adequately addresses the identification and management of mood and anxiety disorders (39,40).
There are important considerations in interpreting the results of this study. The study was not designed as a prevalence study, and it is not known whether our rates are similar to those in other community settings. Nevertheless, illness rates are consistent among studies that screened for depression in obstetric settings (41). However, one might hypothesize that because depressed women initiate prenatal care later than women who are not depressed (24,42), studies may underestimate the illness rates and treatment need.
Our method for assessing rates of identification should also be considered. We deemed a patient as having a "detected" disorder if she reported detection or if there was documentation in the medical chart. Therefore, the results of this study are subject to reporting bias. It is possible that providers made a diagnosis and referred the patient but that the patient did not accurately report the diagnosis and referral and the clinician did not document them in the chart. In addition, because the BPHQ relies on patient self-report, definitive psychiatric diagnosis must be verified by a clinician to determine how well the patient understood the questionnaire and other relevant clinical information. Although the BPHQ performs well in validity studies (22,26) with DSM-IV, it is possible that it overestimated or underestimated the rate of depression and panic disorder in this study.
Finally, an additional limitation of the study is that we did not determine the duration of a depressive episode. Thus women could have been nondepressed at five of the average six visits. We believe that this is unlikely given that the mean and median duration of major depressive disorder has been found to be about ten weeks (43). The high rate for endorsement of suicidal symptoms in our cohort indicates substantial morbidity and severity rather than mild and transient episodes of illness.
Conclusions
Depressive and anxiety disorders among perinatal women can have a profound impact on children from socioeconomically disadvantaged backgrounds (44,45,46,47,48). Mothers from this group lack financial and social resources—for example, assistance from other caretakers—that can counterbalance the deprivation that occurs when they are emotionally or physically unavailable because of depression. Thus it is critical that efforts be made to address these disorders and offer assistance to these less advantaged women. The fact that many pregnant women who have low incomes lose their insurance benefits after their prenatal period further argues for the need to identify and treat mood and anxiety disorders during pregnancy.
The shortcomings noted in the rate of detection and treatment of illness are not cause for assigning blame. Furthermore, it is not clear that detecting the illness will alone lead to higher rates of treatment referral or that patients will follow treatment recommendations. The rate of treatment use (25 percent) for depression found in a recent study of women from minority backgrounds who were receiving care in reproductive health clinics is similar to what we found (49). Finally, limitations in treatment options, especially for women with low incomes, need to be acknowledged. Even though many of our patients had insurance by virtue of their pregnancy, there are few managed Medicaid providers who will accept the low reimbursement rates and the risks attendant in treating pregnant psychiatric patients. Thus it is possible that even with optimal detection and referral, patient and system features may mitigate against adequate treatment. Future work needs to investigate optimal ways of identifying pregnant women who have psychiatric illness but also needs to address systems of care so that symptomatic women are able to receive the care they require.
Acknowledgments
This project was sponsored by grant MH-01908-04 from the National Institute of Mental Health, grant 1H78-MC-00028-01 from the Health Resources and Services Administration of the U.S. Department of Health and Human Services, and a grant from the Yale-Griffin Prevention Research Center.
The authors are affiliated with the department of psychiatry at Yale School of Medicine in New Haven, Connecticut. Send correspondence to Dr. Yonkers at 142 Temple Street, Suite 301, New Haven, Connecticut 06510 (e-mail, [email protected]).
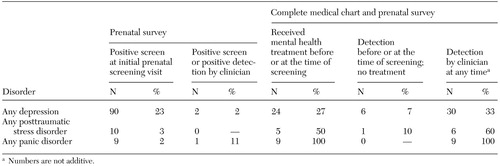 |
Table 1. Clinician follow-up among 99 patients who screened positive for a depressive or anxiety disorder in public-sector obstetric clinics
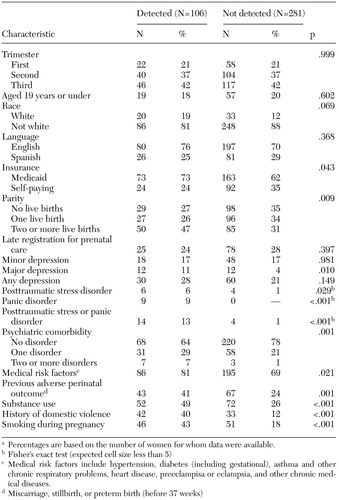 |
Table 2. Characteristics associated with identification of depressive and anxiety disorders among pregnant women in public-sector obstetric clinicsa
a Percentages are based on the number of women for whom data were available.
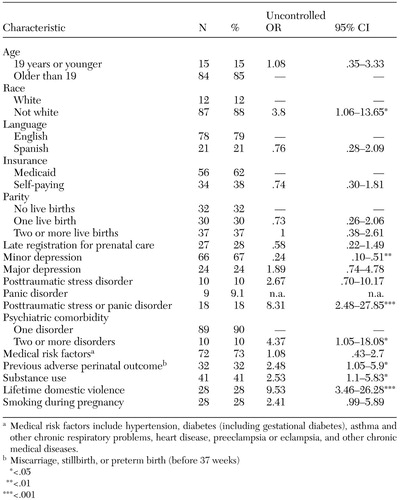 |
Table 3. Factors associated with identification of any mood or anxiety disorder in a sample of 99 pregnant women at public-sector obstetric clinics
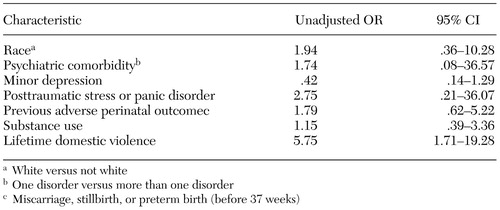 |
Table 4. Logistic regression of predictors of identification of any mood or anxiety disorder in a sample of 99 pregnant women at public-sector obstetric clinics
1. Kessler R, McGonagle K, Zhao S, et al: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Archives of General Psychiatry 51:8–19, 1994Crossref, Medline, Google Scholar
2. O'Hara MW, Zekoski EM, Philipps LH, et al: Controlled prospective study of postpartum mood disorders: comparison of childbearing and nonchildbearing women. Journal of Abnormal Psychology 99:3–15, 1990Crossref, Medline, Google Scholar
3. Cohen L, Sichel D, Faraone S, et al: Course of panic disorder during pregnancy and the puerperium: a preliminary study. Biological Psychiatry 39:950–954, 1996Crossref, Medline, Google Scholar
4. Cooper PJ, Murray L, Hooper R, et al: The development and validation of a predictive index for postpartum depression. Psychological Medicine 26:628–634, 1996Google Scholar
5. Troutman BR, Cutrona CE: Nonpsychotic postpartum depression among adolescent mothers. Journal of Abnormal Psychology 99:69–78, 1990Crossref, Medline, Google Scholar
6. Appleby L, Gregoire A, Platz C, et al: Screening women for high risk of postnatal depression. Journal of Psychosomatic Research 38:539–545, 1994Crossref, Medline, Google Scholar
7. Kumar R, Robson KM: A prospective study of emotional disorders in childbearing women. British Journal of Psychiatry 144:35–47, 1984Crossref, Medline, Google Scholar
8. O'Hara MW, Swain AM: Rates and risk of postpartum depression: a meta-analysis. International Review of Psychiatry 8:37–54, 1996Crossref, Google Scholar
9. Reighard FT, Evans ML: Use of the Edinburgh Postnatal Depression Scale in a southern, rural population in the United States. Progress in Neuro-Psychopharmacology and Biological Psychiatry 19:1219–1224, 1995Crossref, Medline, Google Scholar
10. Roy A, Gang P, Cole K, et al: Use of Edinburgh Postnatal Depression Scale in a North American population. Progress in Neuro-Psychopharmacology and Biological Psychiatry 17:501–504, 1993Crossref, Medline, Google Scholar
11. Whiffen VE: Vulnerability of postpartum depression: a prospective multivariate study. Journal of Abnormal Psychology 97:467–474, 1988Crossref, Medline, Google Scholar
12. Demyttenaere K, Lenaerts H, Nijs P, et al: Individual coping style and psychological attitudes during pregnancy predict depression levels during pregnancy and postpartum. Acta Psychiatrica Scandinavica 91:95–102, 1995Crossref, Medline, Google Scholar
13. Terry DJ, Mayocchi L, Hynes GJ: Depressive symptomatology in new mothers: a stress and coping perspective. Journal of Abnormal Psychology 105:220–231, 1996Crossref, Medline, Google Scholar
14. Cox JL, Connor Y, Kendell RE: Prospective study of the psychiatric disorders of childbirth. British Journal of Psychiatry 140:111–117, 1982Crossref, Medline, Google Scholar
15. Klein MH, Essex MJ: Pregnant or depressed? The effect of overlap between symptoms of depression and somatic complaints of pregnancy on rates of major depression in the second trimester. Depression 2:308–314, 1995Crossref, Google Scholar
16. Watson JP, Elliott SA, Rugg AJ, et al: Psychiatric disorder in pregnancy and the first postnatal year. British Journal of Psychiatry 144:453–462, 1984Crossref, Medline, Google Scholar
17. Hobfoll SE, Ritter C, Lavin J, et al: Depression prevalence and incidence among inner-city pregnant and postpartum women. Journal of Consulting and Clinical Psychology 63:445–453, 1995Crossref, Medline, Google Scholar
18. Miranda J, Azocar F, Komaromy M, et al: Unmet mental health needs of women in public-sector gynecologic clinics. American Journal of Obstetrics and Gynecology 178:212–217, 1998Crossref, Medline, Google Scholar
19. Buekens P, Heeringen K, Boutsen M, et al: Depressive symptoms are often unrecognized in gynaecological practice. European Journal of Obstetrics and Gynecology and Reproductive Biology 81:43–45, 1998Crossref, Medline, Google Scholar
20. Bixo M, Sundstrom-Poromaa I, Astrom M: Patients with psychiatric disorders in gynecologic practice. American Journal of Obstetrics and Gynecology 185:396–402, 2001Crossref, Medline, Google Scholar
21. Sundstrom I, Bixo M, Bjorn I, et al: Prevalence of psychiatric disorders in gynecologic outpatients. American Journal of Obstetrics and Gynecology 184:8–13, 2001Crossref, Medline, Google Scholar
22. Spitzer R, Williams J, Kroenke K, et al: Validity and utility of the Patient Health Questionnaire (PHQ) in assessing 3000 obstetric gynecology patients: the Prime-MD PHQ obstetric gynecology study. American Journal of Obstetric Gynecology 183:759–769, 2000Crossref, Medline, Google Scholar
23. Williams JWJ, Rost K, Dietrich AJ, et al: Primary care physicians' approach to depressive disorders: effects of physician specialty and practice structure. Archives of Family Medicine 8:58–67, 1999Crossref, Medline, Google Scholar
24. Kelly R, Zatzick D, Anders T: The detection and treatment of psychiatric disorders and substance abuse among pregnant women cared for in obstetrics. American Journal of Psychiatry 158:213–219, 2001Link, Google Scholar
25. Spitzer RL, Williams JBW, Kroenke K: Utility of a new procedure for diagnosing mental disorders in primary care: the PRIME-MD 1000 Study. JAMA 272:1749–1756, 1994Crossref, Medline, Google Scholar
26. Spitzer R, Kroenke K, Williams J: Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. JAMA 282:1737–1744, 1999Crossref, Medline, Google Scholar
27. Sheehan D, Lecrubier Y, Janavs J, et al: Mini International Neuropsychiatric Interview (MINI). Tampa, University of South Florida, National Screening Disorders Screening Project, 1996Google Scholar
28. Sheehan D, Lecrubier Y: Mini International Neuropsychiatric Interview (MINI). Tampa, University of South Florida, National Anxiety Disorders Screening Project, 1998Google Scholar
29. SAS Windows. Cary, NC, SAS Institute, 1999Google Scholar
30. Ulrich Y, Cain K, Sugg N, et al: Medical care utilization patterns in women with diagnosed domestic violence. American Journal of Preventative Medicine 24(1):9–15, 2003Google Scholar
31. Magruder-Habib K, Zung WWK, Feussner JR: Improving physicians' recognition and treatment of depression in general medical care: results from a randomized clinical trial. Medical Care 18:239–250, 1990Crossref, Google Scholar
32. Robbins J, Kirmayer L, Cathebras P, et al: Physician characteristics and the recognition of depression and anxiety in primary care. Medical Care 32:795–812, 1994Crossref, Medline, Google Scholar
33. Ormel J, Van Den Brink W, Koeter M, et al: Recognition, management, and outcome of psychological disorders in primary care: a naturalistic follow-up study. Psychological Medicine 20:909–923, 1990Crossref, Medline, Google Scholar
34. Coyne J, Schwenk T, Fechner-Bates S: Nondetection of depression by primary care physicians reconsidered. General Hospital Psychiatry 17:3–12, 1995Crossref, Medline, Google Scholar
35. Sugawara M, Sakamoto S, Kitamura T, et al: Structure of depressive symptoms in pregnancy and the postpartum period. Journal of Affective Disorders 54:161–169, 1999Crossref, Medline, Google Scholar
36. Schmidt LA, Greenberg BD, Holzman GB, et al: Treatment of depression by obstetrician-gynecologists: a survey study. Journal of the American College of Obstetricians and Gynecologists 90:296–300, 1997Google Scholar
37. Jencks S: Recognition of mental distress and diagnosis of mental disorder in primary care. JAMA 253:1903–1907, 1985Crossref, Medline, Google Scholar
38. Rost K, Smith GR, Matthews DB, et al: The deliberate misdiagnosis of major depression in primary care. Archives of Family Medicine 3:333–337, 1994Crossref, Medline, Google Scholar
39. Plummer S, Gournay K, Goldberg D, et al: The detection of psychological distress by practice nurses. Psychological Medicine 30:1233–1237, 2000Crossref, Medline, Google Scholar
40. Payne F, Harvey K, Jessopp L, et al: Knowledge, confidence, and attitudes towards mental health of nurses working in NHS Direct and the effects of training. Journal of Advanced Nursing 40:549–559, 2002Crossref, Medline, Google Scholar
41. Marcus S, Flynn H, Blow F, et al: Depressive symptoms among pregnant women screened in obstetrics settings. Journal of Women's Health 12:373–380, 2003Crossref, Medline, Google Scholar
42. Kitamura T, Shima S, Sugawara M, et al: Psychological and social correlates of the onset of affective disorders among pregnant women. Psychological Medicine 23:967–975, 1993Crossref, Medline, Google Scholar
43. Mueller T, Leon A, Keller M, et al: Recurrence after recovery from major depressive disorder during 15 years of observational follow-up. American Journal of Psychiatry 156:1000–1006, 1999Abstract, Google Scholar
44. Murray L, Cooper PJ: Postpartum depression and child development. Psychological Medicine 27:253–260, 1997Crossref, Medline, Google Scholar
45. Campbell SB, Cohn JF, Meyers T: Depression in first-time mothers: mother-infant interaction and depression chronicity. Developmental Psychology 31:349–357, 1995Crossref, Google Scholar
46. Field T, Sandberg D, Garcia R, et al: Pregnancy problems, postpartum depression, and early mother infant interactions. Developmental Psychology 21:1152–1156, 1985Crossref, Google Scholar
47. Field T, Healy B, Goldstein S, et al: Behavior-state matching and synchrony in mother-infant interactions of nondepressed versus depressed dyads. Developmental Psychology 26:7–14, 1990Crossref, Google Scholar
48. Field T, Healy B, Goldstein S, et al: Infants of depressed mothers show "depressed" behavior even with nondepressed adults. Child Development 59:1569–1579, 1988Crossref, Medline, Google Scholar
49. Miranda J, Chung J, Green B, et al: Treating depression in predominantly low-income young minority women. JAMA 290:57–65, 2003Crossref, Medline, Google Scholar



