The Prevalence of DSM-IV Personality Disorders in Psychiatric Outpatients
Abstract
OBJECTIVE: The largest clinical epidemiological surveys of personality disorders have been based on unstructured clinical evaluations. However, several recent studies have questioned the accuracy and thoroughness of clinical diagnostic interviews; consequently, clinical epidemiological studies, like community-based studies, should be based on standardized evaluations. The Rhode Island Methods to Improve Diagnostic Assessment and Services project is one of the largest clinical epidemiological studies to use semistructured interviews to assess a wide range of psychiatric disorders conducted in general clinical outpatient practice. In the present report, the authors examined the frequency of DSM-IV personality disorders in a patient group and the comorbidity among them. METHOD: Eight hundred fifty-nine psychiatric outpatients were interviewed with the Structured Interview for DSM-IV Personality upon presentation for treatment. RESULTS: Slightly less than one-third of the patients were diagnosed with one of the 10 official DSM-IV personality disorders (N=270, 31.4%). When the patients with personality disorder not otherwise specified were included, the rate of any personality disorder increased to almost half of the group (N=391, 45.5%). The majority of patients meeting criteria for one of the specific personality disorders were diagnosed with more than one. Avoidant, borderline, and obsessive-compulsive personality disorder were the most frequent specific diagnoses. CONCLUSIONS: Personality disorders, as a group, are among the most frequent disorders treated by psychiatrists. They should be evaluated in all psychiatric patients because their presence can influence the course and treatment of the axis I disorder that patients typically identify as their chief complaint.
Community-based epidemiological studies of psychiatric disorders provide important information about the public health burden of these problems. Although the frequency of treatment seeking for psychiatric disorders may be increasing (1), epidemiological studies have indicated that most patients in the community do not get treatment for psychiatric disorders (2, 3). Treatment seeking is related to a number of clinical and demographic factors (4, 5); consequently, studies of the frequency and correlates of psychiatric disorders in the general population should be replicated in clinical populations to provide the practicing clinician with information that might have more direct clinical use.
Differences between the general population and clinical epidemiological studies might be greatest when we examine the prevalence of disorders and diagnostic comorbidity. It is not appropriate to extrapolate from community-based prevalence rates to clinical settings, where the disorder rates are higher. Comorbidity rates are also expected to be higher in clinical settings because help seeking is related to comorbidity (6).
Diagnosing a co-occurring personality disorder in psychiatric patients with an axis I disorder is clinically important because of their association with the duration, recurrence, and outcome of axis I disorders (7–9). Differential diagnosis among the personality disorders has implications for psychotherapeutic and pharmacological approaches (10). An axis II diagnosis, similar to an axis I diagnosis, succinctly communicates important clinical information from one clinician to another. In addition to clinicians benefiting from such communication, patients may also benefit in a therapeutic fashion after being informed that they meet criteria for an axis II diagnosis (11).
The largest clinical epidemiological surveys of personality disorders have been based upon unstructured clinical evaluations (12–14). However, several more recent studies have questioned the accuracy and thoroughness of clinical diagnostic interviews (15, 16). Therefore, it is not surprising that the frequency of personality disorders reported in some clinical epidemiological studies was low (13, 14). In fact, the 11% rate of any personality disorder in the study by Oldham and Skodol (14) of more than 125,000 patients (approximately 60% outpatients) in the New York State mental health system was similar to the rates that have been reported in community-based epidemiological studies (17). Oldham and Skodol (14) suggested that personality disorders were underdiagnosed by the clinicians in their study.
Despite the aforementioned importance in diagnosing personality disorders, clinicians are sometimes reluctant to diagnose them (18). This may be because of a belief that scattering symptoms over two axes is not fruitful, that axis II has substantial overlap within it, that personality disorder diagnoses are particularly stigmatizing, or that a personality disorder diagnosis does not substantially alter the treatment plan (19). Also, assessment methodology is related to diagnostic frequency.
Zimmerman and Mattia (20) directly examined the impact of assessment methods on diagnostic prevalence rates and found that borderline personality disorder was much less frequently diagnosed with an unstructured clinical evaluation than with a semistructured diagnostic interview. The validity of the semistructured diagnostic interview was suggested by the finding that when the information from the semistructured interview was presented to the treating clinicians, borderline personality disorder was much more likely to be diagnosed. Further evidence of the validity of diagnosis by semistructured research interview came from a comparison of the demographic and clinical characteristics of the patients with and without borderline personality disorder, in which predicted differences were found (21).
Clinical epidemiological studies, similar to other diagnostic research, should be based on structured research evaluations because structured interviews improve diagnostic reliability, and adequate reliability is a prerequisite for diagnostic validity. It should be noted that there is currently debate in the field regarding the most valid method of assessing personality disorders. Specifically, the validity of semistructured diagnostic interviews to assess personality disorders has recently been challenged because these interviews, which rely on direct questions to ascertain the presence or absence of the personality disorder criteria, differ from the methods clinicians use to diagnose personality disorders (22). Clinicians, rather than relying on direct questioning at a single interview, typically use a longitudinal perspective to determine the presence or absence of a personality disorder, and their judgments are based on the real-life vignettes patients describe during the course of treatment and the behaviors and attitudes patients display during the treatment sessions. Although there is some controversy as to how to best assess personality disorders, at present, the semistructured interview remains the most widely used method in research. Moreover, a large literature examining the treatment, prognostic, familial, and biological correlates of personality disorders indicates that diagnosing personality disorders with a semistructured interview is valid (23).
To obtain accurate disorder prevalence rates in clinical settings, it is important to assess a broad range of pathology in contrast to a single disorder. Melartin and colleagues (24) suggested that studies that focus on a single disorder find higher rates of that disorder compared to studies that assess a range of disorders. It is possible that researchers who have expertise in the study of a particular disorder may be inclined to more frequently diagnose that disorder.
The Rhode Island Methods to Improve Diagnostic Assessment and Services (MIDAS) project is one of the largest clinical epidemiological studies to use semistructured interviews to assess a wide range of psychiatric disorders conducted in a general clinical outpatient practice (25). Among the strengths of the study are that diagnoses are based on the reliable and valid procedures used in research studies and that the patients are presenting to a community-based psychiatric outpatient practice rather than to a research clinic specializing in the treatment of one or a few disorders. In the present study, we report the frequency of DSM-IV personality disorders found in our study group and examine the comorbidity among those personality disorders.
Method
To date, 1,500 patients have been recruited into the MIDAS project from the Rhode Island Hospital Department of Psychiatry outpatient practice. This private practice group predominantly treats individuals with medical insurance (including Medicare but not Medicaid) on a fee-for-service basis, and it is distinct from the hospital’s outpatient residency training clinic that predominantly serves lower-income and uninsured patients and those receiving medical assistance.
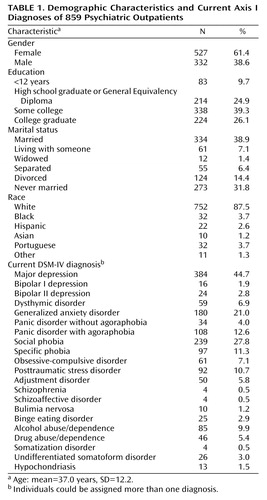
The MIDAS project represents an integration of research methods into a community-based outpatient practice affiliated with an academic medical center (25). A comprehensive diagnostic evaluation is conducted upon presentation for treatment. During the course of the MIDAS project, the assessment battery has changed. The assessment of all DSM-IV personality disorders was not introduced until the study was well under way, and the procedural details of incorporating research interviews into our clinical practice had been well established. The present report is based on the 859 patients interviewed with the full Structured Interview for DSM-IV Personality (SIDP-IV) (26). The data in Table 1 show the demographic and diagnostic characteristics of the group. The majority of the subjects were white, female, married or single, and had some college education. The mean age of the group was 37.0 years (SD=12.2). The most frequent DSM-IV diagnoses were major depressive disorder (44.7%), social phobia (27.8%), generalized anxiety disorder (21.0%), and panic disorder (16.6%).
The patients were interviewed by a diagnostic rater who administered the Structured Clinical Interview for DSM-IV (SCID) (27) and the SIDP-IV. The diagnostic raters are highly trained and monitored throughout the project to minimize rater drift. The diagnostic raters included doctoral-level psychologists and research assistants with college degrees in the social or biological sciences (L.R. and I.C., among others). The research assistants received 3–4 months of training, during which they observed at least 20 interviews, and they were observed and supervised during their administration of more than 20 evaluations. The psychologists observed only five interviews; however, they, too, were observed and supervised during their administration of 15 to 20 evaluations. During the course of training, M.Z. met with each rater to review the interpretation of every item on the SCID and the SIDP-IV. Also, during training, every interview was reviewed on an item-by-item basis by the senior rater, who observed the evaluation, and by M.Z., who reviewed the case with the interviewer. At the end of the training period, the raters were required to demonstrate exact—or near-exact—agreement with a senior diagnostician on five consecutive evaluations. Throughout the MIDAS project, ongoing supervision of the raters consisted of weekly diagnostic case conferences involving all members of the team. In addition, the item ratings of every case were reviewed by M.Z. The Rhode Island Hospital institutional review committee approved the research protocol, and all patients provided written informed consent.
The SIDP-IV focuses on the individual’s “usual self” over the past 5 years. Each DSM-IV criterion is rated 0 (not present), 1 (subthreshold, some evidence of trait but not sufficiently pervasive or severe to be considered present), 2 (present, clearly evident for the last 5 years at least 50% of the time), or 3 (strongly present). The questions on the SIDP-IV are grouped thematically into similar content areas, such as interpersonal relationships, interests and activities, social conformity, and emotions. Such an interview is less prone to halo effects, in which the ratings for individual criteria are influenced by how close the individual is to meeting the criteria for a particular disorder. Because of this thematic organization, the instrument may be more appropriate for studies of comorbidity.
The full SIDP-IV assesses the 10 DSM-IV personality disorders, two personality disorders listed in the appendix of DSM-IV as disorders requiring further study (depressive and passive-aggressive personality disorders), and DSM-III-R self-defeating personality disorder. The present report focuses on the 10 DSM-IV personality disorders and the residual category of personality disorder not otherwise specified. We operationally defined personality disorder not otherwise specified as falling one criterion below the DSM-IV diagnostic threshold for two or more personality disorders.
As an ongoing part of the MIDAS project, joint-interview diagnostic reliability information was collected on 47 participants, 29 of whom were interviewed with the full SIDP-IV. (The first 18 patients included in the reliability study participated in the MIDAS project before the introduction of the full SIDP-IV.) The reliabilities of any personality disorder (kappa=0.77, N=29), and any cluster A (kappa=1.00, N=29), B (kappa=0.61, N=29), or C (kappa=0.87, N=29) personality disorder were good to excellent. Too few patients were diagnosed with individual personality disorders to calculate kappa coefficients for individual personality disorders. However, intraclass correlation coefficients (ICCs) of dimensional scores, computed with a two-way mixed alpha model with SPSS release 8.0.0 (SPSS, Chicago), were high (paranoid: ICC=0.95; schizoid: ICC=0.92; schizotypal: ICC=0.89; antisocial: ICC=0.93; borderline: ICC=0.96; histrionic: ICC=0.93; narcissistic: ICC=0.90; avoidant: ICC=0.96; dependent: ICC=0.97; and obsessive-compulsive: ICC=0.91).
The association between pairs of personality disorders was determined by computing the odds ratios. When a cell in the two-by-two contingency table had a value of zero, the odds ratio was computed after adding a 0.5 constant to all cells (28). The Yates-corrected chi-square test was used to determine whether the odds ratios were significantly different from 1.0.
Results
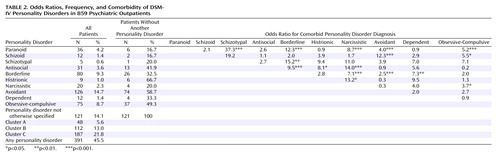
Slightly less than one-third of the patients were diagnosed with one of the 10 DSM-IV personality disorders (N=270, 31.4%). When the patients with personality disorder not otherwise specified were included, the rate of any personality disorder increased to almost half of the group (N=391, 45.5%). Of the 270 patients meeting the criteria for one of the specific personality disorders, 60.4% (N=163) had more than one personality disorder and 25.2% (N=68) had two or more personality disorders. The data in Table 2 indicate that the most frequent specific personality disorder was avoidant (N=126, 14.7%). Personality disorder not otherwise specified and avoidant personality disorder were the only personality disorders diagnosed in more than 10% of the patients, and seven personality disorders were diagnosed in less than 5%. Histrionic and avoidant personality disorder were the most likely to be diagnosed as the sole personality disorder, whereas more than half the patients diagnosed with each of the other personality disorders were diagnosed with another personality disorder.
Borderline personality disorder was significantly associated with six of the other nine personality disorders (all except schizoid, histrionic, and obsessive-compulsive) (Table 2). Paranoid and narcissistic personality disorders were also associated with more than half of the personality disorders. In contrast, dependent personality disorder was significantly associated with only one other personality disorder.
The data in Table 3 show the frequency of personality disorders in patients with and without six of the most common axis I disorders in our study: major depressive disorder, generalized anxiety disorder, panic disorder, social phobia, posttraumatic stress disorder, and alcohol disorders. The presence of each of the axis I disorders was significantly associated with greater personality pathology, although there were some differences between the axis I disorders. For example, alcohol use disorders were associated with significantly higher rates of borderline and antisocial personality, whereas generalized anxiety disorder was associated with a significantly higher rate of each of the cluster C personality disorders but not with a higher frequency of either borderline or antisocial personality disorder.
Discussion
Personality disorders are frequent in psychiatric outpatients. Exactly how frequent depends, in part, on the breadth of definition. When limited to the 10 DSM-IV personality disorders defined by specified criteria, approximately one-third of the patients were diagnosed with a personality disorder. The prevalence increased by about 15% to 45.5% when the residual category of personality disorder not otherwise specified was included. We did not include the DSM-IV appendix diagnoses in our prevalence estimate, although other authors have done so (29). Elsewhere we examined the validity of depressive personality disorder and reported that its prevalence was 22.0% (30), which would have made it the most frequent personality disorder among our patients. We chose not to include the appendix diagnoses because they are not part of the official nomenclature. Their inclusion would have, of course, increased the overall prevalence of any personality disorder. Thus, the seemingly straightforward question of the prevalence rate of personality disorders is complicated by the decision of how wide a net to cast in defining a personality disorder.
Other methodological issues that can influence the prevalence rates of personality disorder include the timing of the assessment, the presence of axis I disorders, the source of the information, and the instrument used (31). We conducted the assessment when the patients were seen for treatment and thus were symptomatic with an axis I disorder. An acute psychiatric state can inflate personality disorder estimates, although semistructured interviews are less prone to this bias than self-administered questionnaires. Despite the potential for false positive diagnoses, we assessed personality disorders at presentation because delaying the assessment until symptom abatement would result in the exclusion of patients who either never improved or who relapsed and were symptomatic after an earlier period of improvement. Because axis II pathology is associated with the chronicity of axis I disorders (32, 33), a study requiring improvement in axis I symptom severity would disproportionately exclude patients with personality disorders, thereby artificially reducing the personality disorder prevalence rate. Studies of personality disorders in psychiatric patients need to balance the potential confounding influence of psychiatric state with the potential lack of generalizability of results based on patients who have improved during treatment.
Another reason for conducting axis II assessments during the initial evaluation is that this is when treatment decisions are usually made. A thorough personality disorder assessment at the time of the initial evaluation aids case formulation and decisions about treatment approaches. Finally, despite the possible bias from state effects, assessments made when patients are symptomatic have strong, consistent prognostic value (9).
Another methodological issue that can affect prevalence rates is the source of the information. Several studies have found poor levels of agreement between patients and informants in diagnosing personality disorders (34–37). Adding information from an informant interview to the information already ascertained from patients nearly doubles the prevalence of personality disorders (38). However, the validity of personality disorder diagnoses based on patient information alone was as high as that based on information from both patients and informants (39). We are not aware of any study suggesting that information from informants increases the validity of personality disorder diagnoses based on patient information alone; thus, we limited our assessment to patient information.
Personality disorder prevalence rates are affected by the type of diagnostic interview conducted. More diagnoses are made according to semistructured interviews than unstructured clinical evaluations. Table 4 summarizes the results of 11 clinical epidemiological studies. Although the methods of these studies varied, it is clear that the rate of any personality disorder is lower in studies using an unstructured clinical evaluation than in studies using semistructured diagnostic interviews. The only study that directly compared prevalence rates as a function of assessment methods in patients ascertained from the same setting was the one from our laboratory on borderline personality disorder (20). The results clearly demonstrated that more diagnoses were made with the semistructured interview.
Final factors that can influence the prevalence rates of personality disorder are the demographic and clinical profiles of the patients evaluated. Questions of generalizability can be raised about the present study, as with every other clinical epidemiology study. In contrast to community-based epidemiological studies, which use sophisticated sampling methods to ensure representation of the general population, clinical epidemiological studies are generally single-site studies of convenience groups. Patients who are applicants for psychoanalysis (44) or for long-term inpatient treatment of personality disorders (44) are likely to have higher rates of personality disorders than unselected patient series. A limitation of the present study was that the majority of the patients were white high school graduates who had health insurance. The most frequent current axis I diagnoses in the group were mood and anxiety disorders, and relatively few patients had eating, somatoform, impulse-control, substance use, and psychotic disorders. However, the rank order of the frequency of axis I disorders was generally similar to the findings in community-based epidemiological studies (47).
Variability in methods, samples, and diagnostic criteria makes it difficult to assimilate the results of the present study with other clinical epidemiological studies of patients with a mixture of axis I disorders (Table 4). Most studies are of inpatients only (40, 42) or of inpatients combined with outpatients (12, 13, 29, 41, 44–46). We are not aware of a study that is comparable to the MIDAS project in which semistructured interviews have been integrated into a community-based outpatient practice. Clinical epidemiological studies using semistructured interviews tend to be performed in inpatient settings because the patients are a captive audience. Integrating research-quality evaluations into an outpatient practice requires that more obstacles are overcome (25). Diagnostic interviewers in the studies listed in Table 4 included psychiatric residents (12, 13, 42), trained research interviewers with undescribed levels of experience and professional training (29, 41), and psychiatrists with extensive prior experience with semistructured diagnostic interviews (45). The samples also differed in the most frequent axis I disorders and the diagnostic system used. Despite these differences, some conclusions can be drawn from these studies. Studies using standardized interviews consistently diagnosed almost half or more of the patients with a personality disorder. Thus, the frequency of personality disorders is high, and clinicians need to be vigilant to their presence because of the potential impact on treatment planning and prognosis. Borderline personality disorder was one of the two most frequent diagnoses in every study, including the present one, whereas schizoid personality disorder was infrequently diagnosed in all studies. This is consistent with the general pattern of cluster B diagnoses being the most frequent and cluster A diagnoses being the least frequent disorders.
Personality disorder not otherwise specified, operationally defined as being within one criterion of the DSM-IV threshold for two or more specific personality disorders, was the most frequent diagnosis in our group. Perhaps interviews such as the SIDP-IV, which are thematically organized around content areas rather than by diagnosis, increase the probability of “subthreshold” diagnoses. Interviews such as the SIDP-IV were intended to be less prone to halo effects, in which ratings of individual criteria are influenced by how close the individual is to meeting the criteria for the disorder. Most clinical epidemiological studies of outpatients did not include the category of personality disorder not otherwise specified, although in two other studies—one using a thematically organized interview (41) and the other using an unstructured clinical evaluation (13)—personality disorder not otherwise specified was one of the most common diagnoses. From a nosological perspective, the relatively high frequency of subthreshold diagnoses lends support to the dimensional rather than categorical approach toward classification.
In conclusion, personality disorders are frequent in psychiatric settings. A summary of other clinical epidemiological studies using semistructured diagnostic interviews indicated that at least half of the patients had a personality disorder, thus making these disorders, as a group, among the most frequent disorders treated by psychiatrists. Personality disorders should be evaluated in every patient because their presence can influence the course and treatment of the axis I disorder that patients typically identify as their chief complaint.
 |
 |
 |
 |
Received June 10, 2003; revisions received March 9 and Oct. 1, 2004; accepted Oct. 26, 2004. From the Department of Psychiatry and Human Behavior, Rhode Island Hospital, Brown University School of Medicine, Providence, R.I. Address correspondence and reprint requests to Dr. Zimmerman, Bayside Medical Center, 235 Plain St., Providence, RI 02905; [email protected] (e-mail). Supported in part by NIMH grants MH-48732 and MH-56404.
1. Olfson M, Marcus SC, Druss B, Elinson L, Tanielian T, Pincus HA: National trends in the outpatient treatment of depression. JAMA 2002; 287:203–209Crossref, Medline, Google Scholar
2. Kessler RC, Zhao S, Katz SJ, Kouzis AC, Frank RG, Edlund M, Leaf P: Past-year use of outpatient services for psychiatric problems in the National Comorbidity Survey. Am J Psychiatry 1999; 156:115–123Link, Google Scholar
3. Narrow WE, Regier DA, Rae DS, Manderscheid RW, Locke BZ: Use of services by persons with mental and addictive disorders: findings from the National Institute of Mental Health Epidemiologic Catchment Area Program. Arch Gen Psychiatry 1993; 50:95–107Crossref, Medline, Google Scholar
4. Goodwin RD, Hoven CW, Lyons JS, Stein MB: Mental health service utilization in the United States: the role of personality factors. Soc Psychiatry Psychiatr Epidemiol 2002; 37:561–566Crossref, Medline, Google Scholar
5. Alegria M, Bijl RV, Lin E, Walters EE, Kessler RC: Income differences in persons seeking outpatient treatment for mental disorders: a comparison of the United States with Ontario and The Netherlands. Arch Gen Psychiatry 2000; 57:383–391Crossref, Medline, Google Scholar
6. Berkson J: Limitations of the application of fourfold table analysis to hospital data. Biometric Bulletin 1946; 2:47–53Crossref, Medline, Google Scholar
7. Farmer R, Nelson-Gray RO: Personality disorders and depression: hypothetical relations, empirical findings, and methodological considerations. Clin Psychol Rev 1990; 10:453–476Crossref, Google Scholar
8. Alnaes R, Torgersen S: Personality and personality disorders predict development and relapses of major depression. Acta Psychiatr Scand 1997; 95:336–342Crossref, Medline, Google Scholar
9. McDermut W, Zimmerman M: The effects of personality disorders on outcome in the treatment of depression, in Mood and Anxiety Disorders. Edited by Rush AJ. Baltimore, Williams & Wilkins, 1998, pp 321–338Google Scholar
10. Shea MT, Widiger TA, Klein MH: Comorbidity of personality disorders and depression: implications for treatment. J Consult Clin Psychol 1992; 60:857–868Crossref, Medline, Google Scholar
11. Yeomans FE, Clarkin JF, Kernberg OF: A Primer of Transference Focused Psychotherapy for the Borderline Patient. Northvale, NJ, Jason Aronson, 2002Google Scholar
12. Kass F, Skodol AE, Charles E, Spitzer RL, Williams JB: Scaled ratings of DSM-III personality disorders. Am J Psychiatry 1985; 142:627–630Link, Google Scholar
13. Koenigsberg HW, Kaplan RD, Gilmore MM, Cooper AM: The relationship between syndrome and personality disorder in DSM-III: experience with 2,462 patients. Am J Psychiatry 1985; 142:207–212Link, Google Scholar
14. Oldham JM, Skodol AE: Personality disorders in the public sector. Hosp Community Psychiatry 1991; 42:481–487Abstract, Google Scholar
15. Shear MK, Greeno C, Kang J, Ludewig D, Frank E, Swartz HA, Hanekamp M: Diagnosis of nonpsychotic patients in community clinics. Am J Psychiatry 2000; 157:581–587Link, Google Scholar
16. Miller PR, Dasher R, Collins R, Griffiths P, Brown F: Inpatient diagnostic assessments, I: accuracy of structured vs unstructured interviews. Psychiatry Res 2001; 105:255–264Crossref, Medline, Google Scholar
17. Mattia JI, Zimmerman M: Epidemiology, in Handbook of Personality Disorders: Theory, Research, and Treatment. Edited by Livesley WJ. New York, Guilford, 2001, pp 107–123Google Scholar
18. Hillman J, Stricker G, Zweig R: Clinical psychologists’ judgments of older adult patients with character pathology: implications for practice. Prof Psychol Res Pr 1997; 28:179–183Crossref, Google Scholar
19. Westen D: Case formulation and personality diagnosis: two processes or one? in Making Diagnosis Meaningful: Enhancing Evaluation and Treatment of Psychological Disorders. Edited by Barron JW. Washington, DC, American Psychological Association, 1998, pp 111–138Google Scholar
20. Zimmerman M, Mattia JI: Differences between clinical and research practices in diagnosing borderline personality disorder. Am J Psychiatry 1999; 156:1570–1574Link, Google Scholar
21. Zimmerman M, Mattia JI: Axis I diagnostic comorbidity and borderline personality disorder. Compr Psychiatry 1999; 40:245–252Crossref, Medline, Google Scholar
22. Westen D: Divergences between clinical and research methods for assessing personality disorders: implications for research and the evolution of axis II. Am J Psychiatry 1997; 154:895–903Link, Google Scholar
23. Livesley WJ: A Handbook of Personality Disorders: Theory, Research, and Treatment. New York, Guilford, 2001Google Scholar
24. Melartin TK, Rytsala HJ, Leskela US, Lestela-Mielonen PS, Sokero TP, Isometsa ET: Current comorbidity of psychiatric disorders among DSM-IV major depressive disorder patients in psychiatric care in the Vantaa Depression Study. J Clin Psychiatry 2002; 63:126–134Crossref, Medline, Google Scholar
25. Zimmerman M: Integrating the assessment methods of researchers in routine clinical practice: the Rhode Island Methods to Improve Diagnostic Assessment and Services (MIDAS) project, in Standardized Evaluation in Clinical Practice, vol 22. Edited by First MB. Washington, DC, American Psychiatric Publishing, 2003, pp 29–74Google Scholar
26. Pfohl B, Blum N, Zimmerman M: Structured Interview for DSM-IV Personality: SIDP-IV. Washington, DC, American Psychiatric Press, 1997Google Scholar
27. First MB, Spitzer RL, Gibbon M, Williams JBW: Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition (SCID-P), version 2. New York, New York State Psychiatric Institute, Biometrics Research, 1995Google Scholar
28. Fleiss JL: Statistical Methods for Rates and Proportions, 2nd ed. New York, John Wiley & Sons, 1981Google Scholar
29. Fossati A, Maffei C, Bagnato M, Battaglia M, Donati D, Donini M, Fiorilli M, Novella L, Prolo F: Patterns of covariation of DSM-IV personality disorders in a mixed psychiatric sample. Compr Psychiatry 2000; 41:206–215Crossref, Medline, Google Scholar
30. McDermut W, Zimmerman M, Chelminski I: The construct validity of depressive personality disorder. J Abnorm Psychol 2003; 112:49–60Crossref, Medline, Google Scholar
31. Zimmerman M: Diagnosing personality disorders: a review of issues and research methods. Arch Gen Psychiatry 1994; 51:225–245Crossref, Medline, Google Scholar
32. Reich JH, Green AI: Effect of personality disorders on outcome of treatment. J Nerv Ment Dis 1991; 179:74–82Crossref, Medline, Google Scholar
33. Rothschild L, Zimmerman M: Interface between personality and depression, in Handbook of Chronic Depression: Diagnosis and Therapeutic Management. Edited by Alpert JE, Fava M. New York, Marcel Dekker, 2004, pp 19–48Google Scholar
34. Modestin J, Puhan A: Comparison of assessment of personality disorder by patients and informants. Psychopathology 2000; 33:265–270Crossref, Medline, Google Scholar
35. Molinari V, Kunik ME, Mulsant B, Rifai AH: The relationship between patient, informant, social worker, and consensus diagnoses of personality disorder in elderly depressed inpatients. Am J Geriatr Psychiatry 1998; 6:136–144Crossref, Medline, Google Scholar
36. Bernstein DP, Kasapis C, Bergman A, Weld E, Mitropoulou V, Horvath T, Klar HM, Silverman J, Siever LJ: Assessing axis II disorders by informant interview. J Personal Disord 1997; 11:158–167Crossref, Medline, Google Scholar
37. Riso LP, Klein DN, Anderson RL, Ouimette PC, Lizardi H: Concordance between patients and informants on the Personality Disorder Examination. Am J Psychiatry 1994; 151:568–573Link, Google Scholar
38. Zimmerman M, Pfohl B, Coryell W, Stangl D, Corenthal C: Diagnosing personality disorder in depressed patients: a comparison of patient and informant interviews. Arch Gen Psychiatry 1988; 45:733–737Crossref, Medline, Google Scholar
39. Zimmerman M, Pfohl B, Coryell W, Stangl D, Corenthal C: Personality disorder diagnoses: who should we interview? in Abstracts of the 1990 Annual Meeting. Washington, DC, American Psychiatric Association, 1990, p 102Google Scholar
40. Dahl AA: Some aspects of DSM-III personality disorders illustrated by a consecutive sample of hospitalized patients. Acta Psychiatr Scand Suppl 1986; 328:61–67Crossref, Medline, Google Scholar
41. Grilo CM, McGlashan TH, Quinlan DM, Walker ML, Greenfeld D, Edell WS: Frequency of personality disorders in two age cohorts of psychiatric inpatients. Am J Psychiatry 1998; 155:140–142Link, Google Scholar
42. Marinangeli MG, Butti G, Scinto A, Di Cicco L, Petruzzi C, Daneluzzo E, Rossi A: Patterns of comorbidity among DSM-III-R personality disorders. Psychopathology 2000; 33:69–74Crossref, Medline, Google Scholar
43. Mezzich JE, Coffman GA, Goodpastor SM: A format for DSM-III diagnostic formulation: experience with 1,111 consecutive patients. Am J Psychiatry 1982; 139:591–596Link, Google Scholar
44. Oldham JM, Skodol AE, Kellman HD, Hyler SE, Doidge N, Rosnick L, Gallaher PE: Comorbidity of axis I and axis II disorders. Am J Psychiatry 1995; 152:571–578Link, Google Scholar
45. Ottosson H, Bodlund O, Ekselius L, Grann M, von Knorring L, Kullgren G, Lindstrom E, Soderberg S: DSM-IV and ICD-10 personality disorders: a comparison of a self-report questionnaire (DIP-Q) with a structured interview. Eur Psychiatry 1998; 13:246–253Crossref, Medline, Google Scholar
46. Stangl D, Pfohl B, Zimmerman M, Bowers W, Corenthal C: A structured interview for the DSM-III personality disorders: a preliminary report. Arch Gen Psychiatry 1985; 42:591–596Crossref, Medline, Google Scholar
47. Zimmerman M, Mattia JI: Principal and additional DSM-IV disorders for which outpatients seek treatment. Psychiatr Serv 2000; 51:1299–1304Link, Google Scholar



