Dimensional Representations of DSM-IV Personality Disorders: Relationships to Functional Impairment
Abstract
OBJECTIVE: This study compared three-dimensional representations of DSM-IV personality disorders and standard categories with respect to their associations with psychosocial functioning. METHOD: Six hundred sixty-eight patients with semistructured interview diagnoses of schizotypal, borderline, avoidant, or obsessive-compulsive personality disorders or with major depressive disorder and no personality disorder completed questionnaires assessing three-factor and five-factor dimensional models of personality. Personality disorder categories, dimensional representations of the categories based on criteria counts, and three- and five-factor personality dimensions were compared on their relationships to impairment in seven domains of functioning, as measured by the Longitudinal Interval Follow-up Evaluation—Baseline Version. RESULTS: Both the categorical and dimensional representations of DSM-IV personality disorders had stronger relationships to impairment in functioning in the domains of employment, social relationships with parents and friends, and global social adjustment and to DSM-IV axis V ratings than the three- and five-factor models. DSM-IV dimensions predicted functional impairment best of the four approaches. Although five-factor personality traits captured variance in functional impairment not predicted by DSM-IV personality disorder dimensions, the DSM-IV dimensions accounted for significantly more variance than the measures of personality. CONCLUSIONS: Scores on dimensions of general personality functioning do not appear to be as strongly associated with functional impairment as the psychopathology of DSM personality disorder. A compromise in the ongoing debate over categories versus dimensions of personality disorder might be the dimensional rating of the criteria that comprise traditional categories.
Despite progress made in understanding the importance of personality disorders, dissatisfaction has been expressed with the use of a categorical approach to their diagnosis (1, 2). Critics of the categorical system point to arbitrary thresholds for diagnosis, loss of potentially important clinical information by the use of all-or-nothing diagnostic categories, considerable heterogeneity within categories, extensive overlap or comorbidity among categories, indistinct boundaries with normal personality, and incomplete coverage of personality psychopathology.
Many dimensional models of personality have been described, including interpersonal circumplex models (3, 4), three-factor models (5), four-factor models (6, 7), the “big five” five-factor model (8), and a seven-factor model (9). Dimensional models view personality traits as continuously distributed in populations and personality psychopathology as extreme variants of these personality traits. Proponents of dimensional approaches to personality disorders argue that they are more faithful representations in that they set no arbitrary thresholds for abnormality, capture clinical heterogeneity and comorbidity well, and provide useful descriptions of all types of patients (10).
A dimensional system for describing personality disorders was considered for DSM-IV, but a lack of information about the clinical use of such a system resulted in the continuation of the standard categories, with a proposal for a dimensional approach placed in an appendix (11). A relatively simple and conservative revision considered was the conversion of current personality disorder categories into dimensions by allowing for clinically significant traits and subthreshold disorders, as well as disorders meeting criteria at different degrees of severity or extensiveness to be noted. This proposal was first made by Kass and associates (12) and was later elaborated on by others (13, 14). The actual dimensional system proposed in the appendix of DSM-IV was an amalgam of three-factor, five-factor, and seven-factor models of personality made possible by the considerable conceptual overlapping of factors in these models. Determining whether a dimensional approach should replace the current categorical approach to the diagnosis of all mental disorders has been identified as one of seven basic questions to be addressed by a “research agenda for DSM-V” (15, 16). Evaluation of the comparative clinical uses of dimensional versus categorical approaches to personality disorders has been designated as an appropriate first step (15, 17).
Since impairment in psychosocial functioning is a fundamental aspect of personality disorder that distinguishes it from normal personality, the comparative abilities of competing schemes to predict impairment offer a way to examine their merits. The purpose of the present study was to compare three different dimensional representations of four DSM-IV personality disorders to the categories themselves on their relationships to measures of functional impairment. The three dimensional approaches chosen were a slightly modified version of the dimensional representation of DSM-IV categories by Widiger (2) and Oldham and Skodol (14), a three-factor model (18), and the five-factor model (8). The four personality disorders studied were schizotypal, borderline, avoidant, and obsessive-compulsive. The three-factor model tested in this study is that described by Watson et al. (19) and includes the personality dimensions of negative temperament, positive temperament, and disinhibition. The five-factor model (8) includes factors of neuroticism, extraversion, agreeableness, openness to experience, and conscientiousness.
Method
Subjects
Participants ages 18 to 45 were recruited primarily from clinical services affiliated with each of the four recruitment sites of the Collaborative Longitudinal Personality Disorders Study. The aims of that study are to determine the stability of the psychopathology and impairments in psychosocial functioning associated with four representative personality disorders and to elucidate factors that affect prognosis. In all, 668 patients with at least one of four personality disorders (schizotypal, borderline, avoidant, or obsessive-compulsive) or with major depressive disorder and no personality disorder were included. All were previously or currently in treatment or seeking treatment. Potential participants with active psychosis, acute substance intoxication or withdrawal, other confusional states, or a history of schizophrenia or schizoaffective disorder were excluded. All participants signed written informed consent after the research procedures had been fully explained.
Forty-three percent of the participants were outpatients in mental health settings, 12% were psychiatric inpatients, 5% were from other mental health or medical settings, and 40% were self-referred. Sixty-four percent were women, and 75% were white. They had a mean age of 32.7 years (SD=8.1).
Assessment
The patients were interviewed by experienced raters with the Diagnostic Interview for DSM-IV Personality Disorders (20). The raters were trained with live or videotaped interviews under the supervision of the first author of the Diagnostic Interview for DSM-IV Personality Disorders (M.C.Z.). Interrater and test-retest reliabilities were as follows: schizotypal personality disorder—interrater agreement=100%, N=3, test-retest kappa=0.64; borderline personality disorder—interrater agreement kappa=0.68, test-retest kappa=0.69; avoidant personality disorder—interrater agreement kappa=0.68, test-retest kappa=0.73; obsessive-compulsive personality disorder—interrater agreement kappa=0.71, test-retest kappa=0.74 (21).
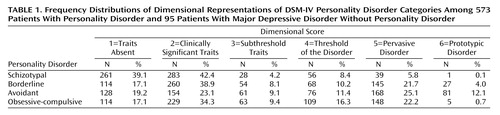
Dimensional representations of the four personality disorders were created according to the proposal outlined by Oldham and Skodol (14). In this system, each personality disorder is described according to six terms (on 6-point scales), based on the number of criteria met: absent traits=0; clinically significant traits=1, 2, or 3 (depending on whether the diagnostic threshold is at 4 or 5); subthreshold traits=3 or 4; threshold of the disorder=4 or 5; pervasive disorder=5, 6, 7, or 8; and prototypic disorder=7, 8, or 9 (depending on the total number of criteria for a given disorder). Intraclass correlation coefficients (ICCs) for the four personality disorder scales were calculated from ratings on 24 videotaped Diagnostic Interviews for DSM-IV Personality Disorders rated by four or more of the trained interviewers and were as follows: schizotypal personality disorder: ICC=0.66, borderline personality disorder: ICC=0.71, avoidant personality disorder: ICC=0.65, and obsessive-compulsive personality disorder: ICC=0.67.
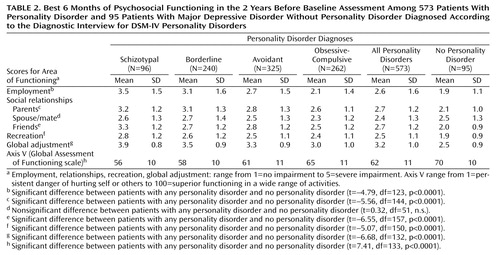
To assess psychosocial functioning, the interviewers administered the Longitudinal Interval Follow-Up Evaluation—Baseline Version (22). This measure assesses functioning in work, interpersonal relationships, recreation, and global functioning. Most areas of functioning are rated on 5-point scales of severity ranging from 1=no impairment, high level of functioning, or very good functioning to 5=severe impairment or very poor functioning. A Global Assessment of Functioning Scale (GAF) rating is on a 100-point scale, with 100 indicating the highest possible level of functioning. Ratings were made for each patient’s best 6 months of functioning in the 2 years before the evaluation. The reliability of the social functioning scales of the Longitudinal Interval Follow-Up Evaluation—Baseline Version (22, 23) has been previously established.
The patients were given the 240-item, self-report Revised NEO Personality Inventory (24), on which they rated statements on 5-point Likert scales, from strongly agree to strongly disagree, to describe themselves according to the five-factor model. Consistent with previous findings, internal consistency reliabilities in our study group for the five-factor domains ranged from 0.87 to 0.92 (median=0.89). The temporal stability of the Revised NEO Personality Inventory has been demonstrated over periods of several years, and high correlations have been obtained between self-reports and observer ratings (25, 26). To assess the patients according to the three-factor model, the patients were given the 375-item, true/false Schedule for Nonadaptive and Adaptive Personality (18), which measures the three factors in addition to other personality dimensions. Internal consistency reliabilities for the three higher-order traits have been in the range of 0.80 to 0.90 in student and patient populations (18), and in our group, they ranged from 0.81 (disinhibition) to 0.90 (negative temperament).
More detailed descriptions of the Collaborative Longitudinal Personality Disorders Study’s rationale, recruitment, demographic characteristics, diagnostic assessments, reliability, and axis I comorbidity are available elsewhere (21, 27, 28).
Analyses
Seven Longitudinal Interval Follow-Up Evaluation—Baseline Version scales (employment; social relationships with parents, spouse/mate, and friends; recreation; global adjustment; and global assessment of functioning) that had previously been found to discriminate functional impairment in the month before the evaluation between personality disorders and major depressive disorder or among the four types of personality disorder (29) were selected. Means and standard deviations on each of these scales were calculated for the best 6 months of the 2 years before intake.
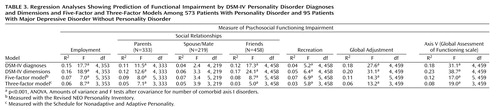
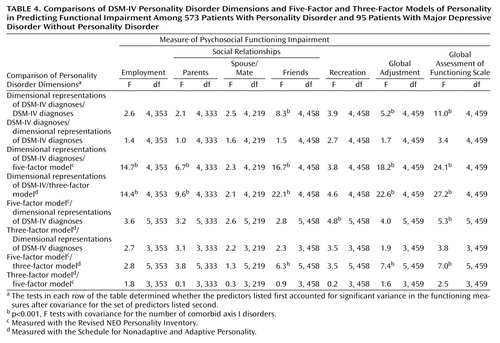
Correlation coefficients (Pearson’s r) were calculated for the relationships among the seven social functioning scales and the DSM-IV categorical diagnoses of schizotypal personality disorder, borderline personality disorder, avoidant personality disorder, and obsessive-compulsive personality disorder; the four disorders represented dimensionally; the five higher-order traits of the five-factor model; and the three higher-order traits of the three-factor model. Multiple regression analyses were performed to determine 1) the ability of the DSM-IV diagnoses, dimensional representations, five-factor model traits, and three-factor model traits to predict impairment in functioning in each of the seven domains and 2) the relative contributions to the prediction of functional impairment when the four approaches were compared two at a time. Since approximately 90% of the patients had one or more current comorbid axis I disorder (mean=2.2, SD=1.5), all regression analyses controlled for the number of comorbid axis I disorders. In the pairwise comparison analyses, we tested for the effect of one set of predictors after covarying for the other. To adjust for making multiple comparisons, we set the significance level at p=0.001.
Results
Table 1 shows the distributions of dimensional representations of each of the four DSM-IV personality disorders, based on criteria counts: 14.3% of the group scored at or above the threshold for a diagnosis of schizotypal personality disorder, 35.9% for borderline personality disorder, 48.6% for avoidant personality disorder, and 39.2% for obsessive-compulsive personality disorder. In addition, from 5.9% (schizotypal personality disorder) to 37.2% (avoidant personality disorder) had more than the minimum number of criteria needed, depending on the diagnosis, and from 32.2% (avoidant personality disorder) to 47.0% (borderline personality disorder) had subthreshold—but clinically significant—traits.
Table 2 shows the mean levels of functional impairment in the best 6 months of the 2 years before the baseline assessments for the patients receiving diagnoses of the four personality disorders, any personality disorder, or major depressive disorder and no personality disorder. The patients with any personality disorder were significantly more impaired in virtually all domains (p<0.0001) than were patients with major depressive disorder and no personality disorder. For most variables, the patients with schizotypal personality disorder and borderline personality disorder had greater impairment in functioning than did the patients with obsessive-compulsive personality disorder. The patients with avoidant personality disorder were at the intermediate level.
Schizotypal and avoidant dimensions were consistently correlated with all measures of functional impairment (r=0.18–0.39, p<0.001) except for social relationships with spouse/mate (r=0.10, n.s.); the borderline personality disorder dimension showed significant correlations with all (r=0.17–0.36, p<0.001) but social relationships with spouse/mate (r=0.17, n.s.) and social relationships with friends (r=0.10, n.s.). The obsessive-compulsive personality dimension showed a negative relationship with impairment in employment only (r=–0.15, p<0.001). Correlations among personality disorder dimensions and functioning variables were generally stronger for the patients with “pure” personality disorder (i.e., without another personality disorder) than for the patients with comorbid personality disorder. Neuroticism from the five-factor model (r=0.16–0.28, p<0.001, for six of seven domains) and, to a lesser extent, negative temperament from the three-factor model (r=0.19–0.25, p<0.001, for four of seven domains) had relationships to impairment similar to those of the dimensional representations of the disorders. Extraversion (from the five-factor model) and—to a lesser extent—openness (the five-factor model), conscientiousness (the five-factor model), and positive temperament (the three-factor model) were inversely related to measures of functional impairment. Agreeableness (five-factor model) and disinhibition (three-factor model) were related only to global social adjustment. (Complete results are available upon request from the first author.)
Table 3 shows regression analyses with DSM-IV diagnoses and dimensions and five-factor and three-factor model predictions of functional impairment in the seven domains. All models of personality and personality disorders predicted significant variance in each domain except for social relationships with spouse/mate. Except for recreation, the magnitude of the effects was greater, however, for the DSM-IV diagnoses and dimensions.
Table 4 presents direct comparisons of the models’ predictions of relationships to functional impairment. The top two rows show the following: 1) DSM-IV personality disorder dimensional representations accounted for significant additional variance after we covaried for DSM-IV personality disorder categories when predicting impairment in social relationships with friends, global social adjustment, and axis V GAF ratings; 2) however, no additional variance was accounted for by the diagnoses after we covaried for the dimensions. As the next two rows reveal, when the DSM-IV personality disorder dimensional representations were added to models with either the five-factor or three-factor models alone, significant additional variance was predicted in employment, social relationships with parents and friends, global adjustment, and GAF ratings. In the reverse comparison, i.e., when we added factors from the five-factor model or the three-factor model to models with DSM dimensions alone, factors from the five-factor model accounted for additional variance only for recreation and GAF score. Head-to-head comparisons of the five- and three-factor models showed an advantage for the five-factor model over the three-factor model for relationships with friends, global adjustment, and GAF ratings.
Discussion
The results of this study support the clinical use of dimensional representations of DSM-IV personality disorders. Consistent with the findings of Kass and associates (12), personality disorder dimensions convey more clinically relevant descriptive information about the maladaptive personality traits of patients than do categories. A substantial proportion of the patients had clinically significant traits that were below the threshold for diagnosis. For the patients with a diagnosis, a significant fraction of all except those with schizotypal personality disorder had pervasive or prototypic personality disorders.
The dimensional representations also bear a stronger relationship to measures of functional impairment than the categories and thus have greater validity in their ability to capture a key aspect of disordered personality that differentiates it from a normal personality. Heumann and Morey (30) demonstrated that dimensional scales to measure personality disorder were more reliable than categorical diagnoses. Widiger (31) examined results in 16 personality disorder studies and found that reliability or validity was better in all but one study when data were analyzed dimensionally rather than categorically.
Two alternative dimensional approaches to the conceptualization of personality disorder, based on measures of general personality traits, were also evaluated in this study. According to the five-factor model, most personality disorders are characterized by extreme neuroticism, that is, vulnerability to stress, impulse dyscontrol, and negative emotionality (32). In a study by Lynam and Widiger (33), experts rated prototypic borderline personality disorder as characteristically high on virtually all facets of neuroticism and certain facets of openness (feelings, actions) and low on deliberation, a facet of conscientiousness. Schizotypal personality disorder and avoidant personality disorder were rated high on facets of neuroticism and low on facets of extraversion, and obsessive-compulsive personality disorder was rated primarily low on openness and high on conscientiousness. According to the three-factor model, negative temperament is virtually synonymous with neuroticism, positive temperament corresponds to extraversion and agreeableness, and disinhibition is the opposite of conscientiousness (34, 35).
The five-factor model has empirical support from the perspectives of convergent and discriminant validity across self, peer, and spouse ratings (36); temporal stability across time (37); cross-cultural replication (38); and heritability (39). Similar construct validity has been more elusive to attain with the current DSM-IV personality disorder categories. Dimensional models have less empirical support in areas of clinical utility, in which the personality disorder categories have been shown to be useful. Personality disorders have been shown to cause impairment in psychosocial functioning (29, 40), to be associated with the use of costly treatments (41), and to adversely affect the treatment outcome of many axis I disorders (42, 43).
From the perspective of impairment in psychosocial functioning, neither dimensional system tested here was as strong a predictor of impairment as the DSM-IV dimensional representations or categories. Consistent with the findings of this study, however, Trull and associates (44) have recently shown that a borderline index emphasizing five-factor model facets of neuroticism (e.g., impulsiveness, angry hostility, and depressiveness) accounted for global dysfunction after variance explained by more traditional measures of borderline personality disorder was accounted for.
For a dimensional approach based on general personality traits to be useful in representing personality psychopathology in patients, a separate rating of impairment in social, occupational, and leisure time functioning might be required. A semistructured interview to assess the five-factor model, the Structured Interview for the Five-Factor Model of Personality, has been developed by Trull and Widiger (45). The Structured Interview for the Five-Factor Model of Personality standardizes a clinical approach for making personality disorder diagnoses according to the five-factor model (46). First, the interviewer asks about the presence of a particular trait and then assesses impairment that might be associated with that trait. Scores from the Structured Interview for the Five-Factor Model of Personality have been shown to have internal consistency and test-retest reliability and expected correlations with other measures of personality and of personality disorder (47, 48). A separate assessment of symptom profiles and related impairments has been advocated for all mental disorders in the future to promote early detection of disorders, research into understanding the interaction of symptoms and other factors that may lead to impairment, and the development of treatments specifically for functional disabilities (49).
A limitation of this study is that only four DSM-IV personality disorder categories and their dimensional representations were examined. Other personality disorder categories might not bear as strong relationships to functional impairment. The four personality disorders studied were chosen, however, to represent major clinical categories in each of the three DSM-IV clusters, and they would account for a high percentage of patients with personality disorders in clinical settings. Future analyses should also address whether certain facets, or combinations of facets, of the five-factor or the three-factor model would have stronger relationships to functional impairment than the models’ factors themselves. It will also be important to determine whether the DSM-IV dimensional representations predict functional outcome over time in our longitudinal study better than the other models (50), as well as relationships to etiological factors or treatment response.
Our personality disorder assessments were based on patient interviews rather than on interviews with informants, which do not always agree. Which assessment is more valid remains an open question, however (51). Personality disorder and functional assessments were both made by a single clinician using interview methods, whereas dimensions of general personality functioning were measured by self-report. In a previous study comparing personality disorder groups to a group with major depression and no personality disorder (29), virtually identical patterns of results were obtained for relative levels of functional impairment by interview and by self-report methods, however, suggesting that method variance or interviewer bias were not major factors in the current study.
We conclude that the associations with impairment found in this study for the DSM-IV personality disorder categorical and dimensional representations result from the inherently more pathological nature of the phenomena described by personality disorder diagnostic criteria, which are not as adequately captured by self-report measures of general personality functioning. The descriptive advantages of dimensional representations of DSM-IV personality disorders and their enhanced relationships to functional impairment suggest that a compromise in the ongoing debate over categories versus dimensions of personality disorder might be to allow for the dimensional rating of the criteria that comprise traditional categories.
 |
 |
 |
 |
Presented in part at the 154th annual meeting of the American Psychiatric Association, New Orleans, May 5–10, 2001. Received May 30, 2002; revisions received Jan. 16, 2003, May 25, 2004, and Oct. 14, 2004; accepted Dec. 7, 2004. From the Department of Psychiatry and Human Behavior, Brown University, Providence, R.I.; the Decision Sciences Institute, Providence, R.I.; New York State Psychiatric Institute, Columbia University College of Physicians and Surgeons; McLean Hospital, Harvard Medical School, Belmont, Mass.; the Medical University of South Carolina, Charleston; the Department of Psychology, Texas A&M University, College Station; and Yale Psychiatric Research, Yale University School of Medicine, New Haven, Conn. Address correspondence and reprint requests to Dr. Skodol, Box 129, New York State Psychiatric Institute, 1051 Riverside Dr., New York, NY 10032; [email protected] (e-mail). Supported by NIMH grants MH-50837, MH-50838, MH-50839, MH-50840, and MH-50850 and MH-01654 (to Dr. McGlashan). This article has been reviewed and was approved by the publications committee of the Collaborative Longitudinal Personality Disorders Study.
1. Clark LA, Livesley WJ, Morey L: Personality disorder assessment: the challenge of construct validity. J Personal Disord 1997; 11:205–231Crossref, Medline, Google Scholar
2. Widiger TA: The DSM-III-R categorical personality disorder diagnoses: a critique and an alternative. Psychol Inquiry 1993; 4:75–90Crossref, Google Scholar
3. Wiggins J: Circumplex models of interpersonal behavior in clinical psychology, in Handbook of Research Methods in Clinical Psychology. Edited by Kendall P, Butcher J. New York, John Wiley & Sons, 1982, pp 183–221Google Scholar
4. Benjamin LS: Interpersonal Diagnosis and Treatment of Personality Disorders, 2nd ed. New York, Guilford, 1996Google Scholar
5. Eysenck HJ, Eysenck SBG: Eysenck Personality Questionnaire Manual. London, Hodder and Stoughton, 1975Google Scholar
6. Livesley WJ, Jackson DN, Schroeder ML: Factorial structure of traits delineating personality disorders in clinical and general population samples. J Abnorm Psychol 1992; 101:432–440Crossref, Medline, Google Scholar
7. Livesley WJ, Jang KL, Vernon PA: Phenotypic and genetic structure of traits delineating personality disorder. Arch Gen Psychiatry 1998; 55:941–948Crossref, Medline, Google Scholar
8. Costa PT Jr, McCrae RR: The five-factor model of personality and its relevance to personality disorders. J Personal Disord 1992; 6:343–359Crossref, Google Scholar
9. Cloninger CR, Svrakic DM, Przybeck TR: A psychobiological model of temperament and character. Arch Gen Psychiatry 1993; 50:975–990Crossref, Medline, Google Scholar
10. Widiger TA: Personality disorder dimensional models proposed for DSM-IV. J Personal Disord 1991; 5:386–398Crossref, Google Scholar
11. Widiger TA: Personality disorder dimensional models, in DSM-IV Sourcebook, vol 2. Edited by Widiger TA, Frances AJ, Pincus HA, Ross R, First MB, Davis WW. Washington, DC, American Psychiatric Association, 1996, pp 789–798Google Scholar
12. Kass F, Skodol AE, Charles E, Spitzer RL, Williams JB: Scaled ratings of DSM-III personality disorders. Am J Psychiatry 1985; 142:627–630Link, Google Scholar
13. Widiger TA, Sanderson CJ: Toward a dimensional model of personality disorder, in The DSM-IV Personality Disorders. Edited by Livesley WJ. New York, Guilford, 1995, pp 433–458Google Scholar
14. Oldham JM, Skodol AE: Charting the future of axis II. J Personal Disord 2000; 14:17–29Crossref, Medline, Google Scholar
15. Rounsaville BJ, Alarcon RD, Andrews G, Jackson JS, Kendell RE, Kendler K: Basic nomenclature issues for DSM-V, in A Research Agenda for DSM-V. Edited by Kupfer DJ, First MB, Regier DA. Washington, DC, American Psychiatric Association, 2002, pp 1–29Google Scholar
16. Helmuth L: In sickness or in health? Science 2003; 302:808–810Crossref, Medline, Google Scholar
17. First MB, Bell CC, Cuthbert B, Krystal JH, Malison R, Offord DR, Reiss D, Shea MT, Widiger T, Wisner KL: Personality disorders and relational disorders: a research agenda for addressing crucial gaps in DSM, in A Research Agenda for DSM-V. Edited by Kupfer DJ, First MB, Regier DA. Washington, DC, American Psychiatric Association, 2002, pp 123–199Google Scholar
18. Clark LA: Manual for the Schedule for Nonadaptive and Adaptive Personality (SNAP). Minneapolis, University of Minnesota Press, 1993Google Scholar
19. Watson D, Clark LA, Harkness AR: Structures of personality and their relevance to psychopathology. J Abnorm Psychol 1994; 103:18–31Crossref, Medline, Google Scholar
20. Zanarini MC, Frankenburg FR, Sickel AE, Yong L: The Diagnostic Interview for DSM-IV Personality Disorders (DIPD-IV). Belmont, Mass, McLean Hospital, 1996Google Scholar
21. Zanarini MC, Skodol AE, Bender D, Dolan R, Sanislow C, Schaefer E, Morey LC, Grilo CM, Shea MT, McGlashan TH, Gunderson JG: The Collaborative Longitudinal Personality Disorders Study: reliability of axis I and axis II diagnoses. J Personal Disord 2000; 14:291–299Crossref, Medline, Google Scholar
22. Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, Andreasen NC: The Longitudinal Interval Follow-Up Evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiatry 1987; 44:540–548Crossref, Medline, Google Scholar
23. Warshaw MG, Keller MB, Stout RL: Reliability and validity of the Longitudinal Interval Follow-Up Evaluation for assessing outcome of anxiety disorders. J Psychiatr Res 1994; 28:531–545Crossref, Medline, Google Scholar
24. Costa PT Jr, McCrae RR: Revised NEO Personality Inventory (NEO PI-R) and NEO Five-Factor Inventory (NEO-FFI): Professional Manual. Odessa, Fla, Psychological Assessment Resources, 1992Google Scholar
25. John OP, Srivastava S: The big five trait taxonomy: history, measurement, and theoretical perspectives, in Handbook of Personality: Theory and Research, 2nd ed. Edited by Pervin LA, John OP. New York, Guilford, 2001, pp 102–138Google Scholar
26. McCrae RR, Costa PT: A five-factor theory of personality. Ibid, pp 139–153Google Scholar
27. Gunderson JG, Shea MT, Skodol AE, McGlashan TH, Morey LC, Stout RL, Zanarini MC, Grilo CM, Oldham JM, Keller MB: The Collaborative Longitudinal Personality Disorders Study: development, aims, design, and sample characteristics. J Personal Disord 2000; 14:300–315Crossref, Medline, Google Scholar
28. McGlashan TH, Grilo CM, Skodol AE, Gunderson JG, Shea MT, Morey LC, Zanarini MC, Stout RL, Oldham JM, Keller MB: The Collaborative Longitudinal Personality Disorders Study: baseline patterns of DSM-IV axis I/II and II/II diagnostic co-occurrence. Acta Psychiatr Scand 2000; 102:256–264Crossref, Medline, Google Scholar
29. Skodol AE, Gunderson JG, McGlashan TH, Dyck IR, Stout RL, Bender DS, Grilo CM, Shea MT, Zanarini MC, Morey LC, Sanislow CA, Oldham JM: Functional impairment in schizotypal, borderline, avoidant, or obsessive-compulsive personality disorders. Am J Psychiatry 2002; 159:276–283Link, Google Scholar
30. Heumann K, Morey L: Reliability of categorical and dimensional judgments of personality disorder. Am J Psychiatry 1990; 147:498–500Link, Google Scholar
31. Widiger T: Categorical versus dimensional classification: implications from and for research. J Personal Disord 1992; 6:287–300Crossref, Google Scholar
32. Widiger TA, Trull TJ, Clarkin JF, Sanderson C, Costa PT: A description of the DSM-III-R and DSM-IV personality disorders with five-factor model of personality, in Personality Disorders and the Five-Factor Model of Personality. Edited by Costa PT, Widiger TA. Washington, DC, American Psychological Association, 1994, pp 41–58Google Scholar
33. Lynam DR, Widiger TA: Using the five-factor model to represent the DSM-IV personality disorders: an expert consensus approach. J Abnorm Psychol 2001; 110:401–412Crossref, Medline, Google Scholar
34. Clark LA, Livesley WJ, Schroeder ML, Irish SL: Convergence of two systems for assessing specific traits of personality disorder. Psychol Assess 1996; 8:294–303Crossref, Google Scholar
35. Schroeder ML, Wormworth JA, Livesley WJ: Dimensions of personality disorder and their relationship to the big five dimensions of personality. Psychol Assess 1992; 4:47–53Crossref, Google Scholar
36. Costa PT Jr, McCrae RR: Personality in adulthood: a six-year longitudinal study of self-reports and spouse ratings on the NEO Personality Inventory. J Pers Soc Psychol 1988; 54:853–863Crossref, Medline, Google Scholar
37. Costa PT Jr, McCrae RR: Set like plaster? evidence for the stability of adult personality, in Can Personality Change? Edited by Heatherton T, Weinberger JL. Washington, DC, American Psychological Association, 1994, pp 21–40Google Scholar
38. DeRaad B, Perugini M, Hrebickova M, Szarota P: Linqua franca of personality: taxonomies and structures based on the psycholexical approach. J Cross-Cultural Psychol 1998; 29:212–232Crossref, Google Scholar
39. Jang KL, McCrae RR, Angleitner A, Riemann R, Livesley WJ: Heritability of facet-level traits in a cross-cultural twin sample: support for a hierarchical model. J Pers Soc Psychol 1998; 74:1556–1565Crossref, Medline, Google Scholar
40. Johnson JG, Williams JBW, Goetz RR, Rabkin JG, Remien RH, Lipsitz JD, Gorman JM: Personality disorders predict onset of axis I disorders and impaired functioning among homosexual men with and at risk of HIV infection. Arch Gen Psychiatry 1996; 53:350–357Crossref, Medline, Google Scholar
41. Bender DS, Dolan RT, Skodol AE, Sanislow CA, Dyck IR, McGlashan TH, Shea MT, Zanarini MC, Oldham JM, Gunderson JG: Treatment utilization by patients with personality disorders. Am J Psychiatry 2001; 158:295–302Link, Google Scholar
42. Reich JH, Vasile RG: Effect of personality disorders on the treatment outcome of axis I conditions: an update. J Nerv Ment Dis 1993; 181:475–484Crossref, Medline, Google Scholar
43. Shea MT, Widiger TA, Klein MH: Comorbidity of personality disorders and depression: implications for treatment. J Consult Clin Psychol 1992; 60:857–868Crossref, Medline, Google Scholar
44. Trull TJ, Widiger TA, Lynam DR, Costa PT Jr: Borderline personality disorder from the perspective of general personality functioning. J Abnorm Psychol 2003; 112:193–202Crossref, Medline, Google Scholar
45. Trull TJ, Widiger TA: Structured Interview for the Five-Factor Model of Personality (SIFFM): Professional Manual. Odessa, Fla, Psychological Assessment Resources, 1997Google Scholar
46. Widiger TA, Costa PT, McCrae RR: Diagnosis of personality disorders using the five-factor model, in Personality Disorders and the Five-Factor Model, 2nd ed. Edited by Costa PT, Widiger TA. Washington, DC, American Psychological Association, 2002, pp 431–456Google Scholar
47. Trull TJ, Widiger TA, Useda JD, Holcomb J, Doan B-T, Axelrod SR, Stern BL, Gershuny BS: A structured interview for the assessment of the five-factor model of personality. Psychol Assess 1998; 10:229–240Crossref, Google Scholar
48. Trull TJ, Widiger TA, Burr R: A structured interview for the assessment of the Five-Factor Model of personality: facet-level relations to the axis II personality disorders. J Pers 2001; 69:175–198Crossref, Medline, Google Scholar
49. Lehman AF, Alexopoulos GS, Goldman H, Jeste D, Ustun B: Mental disorders and disability, in A Research Agenda for DSM-V. Edited by Kupfer DJ, First MB, Regier DA. Washington, DC, American Psychiatric Association, 2002, pp 201–218Google Scholar
50. Morey LC, Zanarini MC: Borderline personality: traits and disorder. J Abnorm Psychol 2000; 109:733–737Crossref, Medline, Google Scholar
51. Klonsky ED, Oltmanns TF, Turkheimer E: Informant-reports of personality disorder: relation to self-reports and future directions. Clin Psychol Sci Prac 2002; 9:300–311Crossref, Google Scholar



