Preventing the Onset of Depressive Disorders: A Meta-Analytic Review of Psychological Interventions
Abstract
Objective: A growing number of studies have tested the efficacy of preventive interventions in reducing the incidence of depressive disorders. Until now, no meta-analysis has integrated the results of these studies. Method: The authors conducted a meta-analysis. After a comprehensive literature search, 19 studies were identified that met inclusion criteria. The studies had to be randomized controlled studies in which the incidence of depressive disorders (based on diagnostic criteria) in an experimental group could be compared with that of a control group. Results: The mean incidence rate ratio was 0.78, indicating a reduction of the incidence of depressive disorders by 22% in experimental compared with control groups. Heterogeneity was low to moderate (I 2 =33%). The number needed to treat to prevent one case of depressive disorder was 22. Moderator analyses revealed no systematic differences between target populations or types of prevention (universal, selective, or indicated). The data included indications that prevention based on interpersonal psychotherapy may be more effective than prevention based on cognitive-behavioral therapy. Conclusions: Prevention of new cases of depressive disorders does seem to be possible. Prevention may become an important way, in addition to treatment, to reduce the enormous public health burden of depression in the coming years.
Depressive disorders are highly prevalent (1 , 2) and have a high incidence (3) , and they are associated with a substantial loss of quality of life for patients and their relatives (4 , 5) , increased mortality rates (6) , high levels of service use, and enormous economic costs (7 – 9) . Major depression is currently ranked fourth worldwide in disease burden, and it is expected to rank first in disease burden in high-income countries by the year 2030 (10) .
There are two ways to reduce the enormous disease burden from depressive disorders: treatment of existing disorders and prevention of new cases. By far the most research has been conducted on the treatment of depressive disorders, and relatively few studies have focused on possibilities for preventing the onset of new cases of depression (11) . Recent studies from Australia, however, have shown that existing pharmacological and psychological treatments cannot reduce the burden of disease of depressive disorders by more than 35%, even under ideal circumstances (12 , 13) .
Prevention has been examined in a considerable number of intervention studies, but only a small proportion of these have focused on possibilities for actually preventing the onset of new cases of mental disorders (14) . Most prevention trials have measured change in protective factors, such as social, cognitive, or problem-solving skills, or in intermediate outcomes, such as severity of depressive symptoms. In recent years, however, a growing number of studies have examined whether prevention programs are actually capable of reducing the incidence of cases of mental disorders as defined by diagnostic criteria. This is an important research question, both from a public health perspective and from a scientific perspective. Prevention is important because duration of the disorder is inversely related to outcome, so that by the time cases come to the attention of practitioners, they are harder to treat. If prevention is effective, it can be employed in concert with treatment in efforts to curtail the burden of disease associated with depression. From a scientific point of view, prevention is equally interesting, as it may result in knowledge about the processes leading up to the onset of depressive disorders and how interventions may curtail or delay these processes.
Although a growing number of studies have examined the effects of preventive interventions on the incidence of depressive disorders, no meta-analysis of these studies has been conducted. An earlier meta-analysis examined the effects of psychological prevention programs on the incidence of all mental disorders (14) . At that time, however, only a small number of studies (N=6) of the effects on depressive disorders could be included; in the past few years many new studies have been conducted, and in this meta-analysis we were able to include 19 studies. We focused on the effects of preventive interventions on the incidence of major depressive disorder. We also examined whether any factors can be identified that modify the effects of prevention.
Method
Search Strategy and Selection of Studies
We began by conducting a comprehensive literature search in bibliographic databases for relevant articles published from 1966 to June 2007. We examined a total of 3,833 abstracts in PubMed (N=1,205), PsycInfo (N=1,146), EMBASE (N=313), and the Cochrane Central Register of Controlled Trials (N=1,169). In order to find unpublished studies, we also examined abstracts from Digital Dissertations (N=23). We searched these databases by combining terms indicative of prevention and depression (specifying searches for both MeSH terms and text words), while limiting the search to effect studies (randomized trials, controlled trials, clinical trials). Second, we examined the references of earlier reviews and meta-analyses (14 – 20) , and we reviewed the reference lists of retrieved articles.
We included studies that used a pretest-posttest randomized controlled design and examined the effects of a preventive intervention on the incidence of new cases of depressive disorders compared with a control group that did not receive the intervention. To be included, studies had to use a standardized diagnostic interview at baseline to exclude the pretest presence of a full-blown depressive disorder and to examine the incidence of depressive disorders at follow-up. We also included studies that examined interventions aimed at reducing depressive disorders as a consequence of specific events (e.g., postnatal depression, poststroke depression) and did not have a pretest assessment of depressive disorders but did have a posttest assessment. Studies were excluded if they explicitly reported having included subjects with depressive disorders who then received the intervention. No limits were imposed on study publication language.
Quality Assessment
Although at least 25 scales are available to assess the validity and quality of randomized controlled trials (21) , there is no evidence that they provide reliable assessments of validity. We therefore preferred to use a simple approach for assessing the validity of the studies, as suggested in the Cochrane Handbook(21) , using three basic criteria: allocation to conditions by an independent (third) party; blinding of assessors of outcomes; and completeness of follow-up data. We did not use the fourth basic criterion described in the Handbook (adequacy of random allocation concealment to respondents), because it is inapplicable to studies comparing psychological interventions to no-treatment control groups.
Analyses
Because the follow-up period of the studies varied considerably, we based the calculation of incidence rates on person-years. That is, we divided the number of new cases of depressive disorders that occurred during the follow-up period (the numerator) by the total person-time units (person-years) of the group at risk (the denominator). Technically, this is known as the person-time incidence rate or the incidence density rate. The person-time incidence rate is an appropriate measure of incidence when follow-up times are unequal (22) . In two studies, this method could not be used because the number of subjects was larger than the number of person-years as a result of the brevity of the follow-up period and the relatively large number of new cases during this period. For example, when 12 persons are studied for 3 months, they generate 4 person-years. If more than four persons develop a disorder during the follow-up period, the person-years incidence rate cannot be calculated. To solve this problem, we rescaled person-years into person-quarters (3 months), then combined the study outcomes meta-analytically, and finally back-transformed the outcome into incidence rates based on person-years. For each study, we calculated the incidence rate ratio as the incidence rate of developing a depressive disorder in experimental subjects relative to the incidence rate in control subjects.
To calculate pooled mean incidence rate ratios, we used the Comprehensive Meta-Analysis software package, version 2.2.021 (Biostat, Englewood, N.J.). Because we expected considerable heterogeneity, we conducted all analyses using the random-effects model (21) , which assumes that the included studies are drawn from “populations” of studies that differ from each other systematically (thus exhibiting heterogeneity). In this model, the effect sizes resulting from included studies differ because of the random error within studies, but also because of true variation in effect size from one study to the next.
Because our analyses were based on the assumption of an underlying constant hazards model in both groups, which is not necessarily the case, we conducted several additional analyses. First, we calculated the odds ratio for each study (ignoring the differences in follow-up period between the studies) and pooled them. Second, we calculated the absolute risk differences for each study (again ignoring the differences in follow-up period); these risk differences were also pooled. Then we calculated the number needed to treat, which denotes how many people would have to receive a preventive intervention for one new case of depression to be prevented. The number needed to treat was calculated as the inverse of the absolute risk difference.
We also conducted a cumulative meta-analysis, in which the results of each new study were added to the total of the studies that had been conducted previously (23) . This method allows a determination of the point in time when the overall results of the studies became significant.
In our analyses, we tested whether there were genuine differences underlying the results of the studies (heterogeneity) or whether the variation in findings was compatible with chance alone (homogeneity) (24) . As an indicator of homogeneity, we calculated the Q statistic. A significant Q rejects the null hypothesis of homogeneity and indicates that the variability among the effect sizes is greater than what is likely to have resulted from subject-level sample error alone. We also calculated I 2 , which is an indicator of heterogeneity (in percentages) not accounted for by sample error. A value of 0% indicates no observed heterogeneity, and larger values show increasing heterogeneity, with 25% considered low, 50% moderate, and 75% high heterogeneity, suggesting that systematic factors are responsible for differences across the effect sizes of the primary studies (24) .
Subgroup and metaregression analyses were conducted according to the procedures implemented in the Comprehensive Meta-Analysis software. We used mixed-effects analyses, which pooled studies within subgroups with the random-effects model but tested for significant differences between subgroups with the fixed-effects model.
Publication bias was tested by inspecting the funnel plot on the primary outcome measure (incidence rate ratio) and by Duval and Tweedie’s trim-and-fill procedure (25) , which yields an estimate of the effect size after the publication bias has been taken into account (again, as implemented in the Comprehensive Meta-Analysis program).
Results
Description of Included Studies
We retrieved a total of 135 articles that potentially met our inclusion criteria. Of these, 116 were excluded, 81 because the presence of depressive disorders was not assessed with a formal diagnostic interview, 13 because they were treatment and not prevention studies, 17 because they did not examine psychological interventions, and five for other reasons (articles that described the design of studies without results or articles with insufficient data).
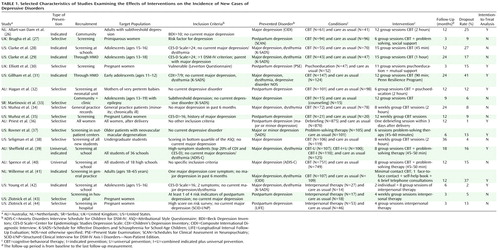
A total of 19 studies (26 – 44) met all inclusion criteria; because one of these studies used three different preventive interventions and a control group, a total of 21 comparisons could be made between a preventive intervention group and a control group. The total number of respondents in the studies was 5,806 (3,014 in the intervention conditions and 2,792 in the control conditions). Selected characteristics of the included studies are presented in Table 1 .
Seven of the 19 studies were designed to prevent postpartum depression, four dealt with prevention in school settings, two were aimed at patients with a physical disorder, two focused on primary care patients, and the remaining studies were aimed at other target groups. Seven studies focused on adolescents, and 12 targeted adults (one focusing on older adults). In 14 studies, subjects with a diagnosed depressive disorder at baseline were excluded, while the interventions in the remaining five studies (aimed at high-risk groups) did not assess the presence of a depressive disorder at baseline. Of the 14 studies in which subjects with a diagnosed depressive disorder at baseline were excluded, 12 excluded those with a current depressive disorder and two excluded those who had a depressive disorder in the previous 6 months.
We distinguished three types of prevention (45) : universal prevention, such as school programs and mass media campaigns, aimed at the general population or segments of the general population, regardless of whether they have a higher-than-average risk of developing a disorder; selective prevention, aimed at individuals in high-risk groups who have not yet developed a mental disorder; and indicated prevention, aimed at individuals who have some symptoms of a mental disorder but do not meet diagnostic criteria. Two of the 21 contrast groups we included in our meta-analysis examined universal prevention, 11 examined selective prevention, and eight examined indicated prevention. Fifteen interventions were cognitive-behavioral therapy (CBT), three were interpersonal psychotherapy, and the remaining were other types of intervention (one-session debriefing; problem-solving; and mutual support). In 18 comparisons, a group format was used, and the remaining three comparisons used an individual format. The number of sessions ranged from one to 15.
The follow-up periods in the different studies ranged from 3 to 36 months. Ten studies were conducted in the United States, four in Australia, two in the United Kingdom, two in the Netherlands, and one in Serbia.
Although the quality of the included studies was relatively high, the criteria assessing the validity of the studies did not indicate very positive results. Only seven studies reported allocation to conditions by an independent party. Blinding of assessors of outcomes was reported in eight of the 19 studies. Dropout rates ranged from 1% to 41%. In nine studies, intention-to-treat analyses were conducted.
Incidence Rate Ratios
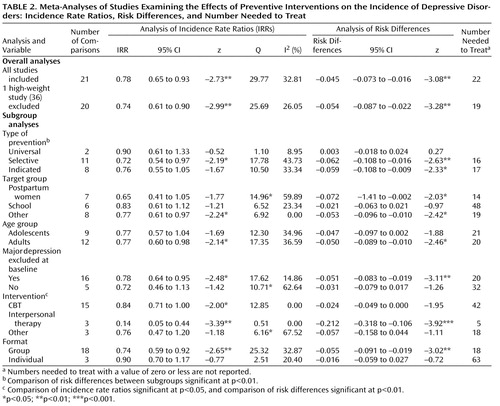
The mean incidence rate ratio for all 21 comparisons from the 19 studies was 0.78 (95% confidence interval [CI]=0.65–0.93), which was significant (p<0.01). Heterogeneity was low to moderate (Q=29.77, p<0.10; I 2 =32.81%). The results of this meta-analysis are summarized in Table 2 and Figure 1 . The cumulative meta-analysis showed that the overall results became significant after the first four studies had been published in 2000 ( Figure 1 ).
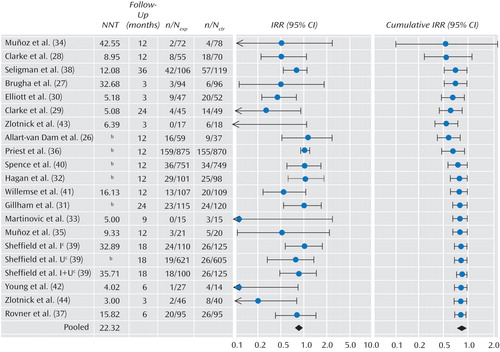
a NNT=number needed to treat; n/N exp =number of incident cases among the total group of subjects in the experimental condition; n/N ctr =number of incident cases among the total group of subjects in the control condition; IRR=incidence rate ratio.
b Numbers needed to treat with a value of zero or less are not reported.
c I=indicated prevention; U=universal prevention; I+U=combined indicated plus universal prevention.
Because the weight of one study (36) was very high (34.2%), and because this was also the study in which a very different type of intervention was used (one-session debriefing after childbirth), we examined whether removal of this study from the analysis would change the overall results. The resulting mean incidence rate ratio was 0.74 (95% CI=0.61–0.90, p<0.01), with low heterogeneity (Q=25.69, n.s.; I 2 =26.05%), which is comparable to the incidence rate ratio found in the analyses with the full sample.
In one large study (39) , three intervention conditions were compared with one control group. Because these three comparisons were not independent from each other, we examined whether removal of these comparisons would increase heterogeneity. The resulting mean incidence rate ratio was 0.74 (95% CI=0.59–0.92, p<0.01; Q=28.79, p<0.05; I 2 =40.95%).
Neither the funnel plots nor Duval and Tweedie’s trim-and-fill procedure suggested a significant publication bias. The incidence rate ratio did not change after adjustment for possible publication bias (the observed and adjusted effect sizes were the same).
Risk Differences and Number Needed to Treat
Our analyses were based on the assumption of an underlying constant hazards model in both groups, which may not be the case. We conducted several sensitivity analyses. We calculated the odds ratio for each study (ignoring the differences in follow-up period between the studies) and pooled them. The resulting odds ratio was 0.76 (95% CI=0.62–0.94; z=–2.59, p=0.01), which was comparable to the earlier analyses.
We also calculated the absolute risk differences for each study (again ignoring the differences in follow-up period). This resulted in a pooled risk difference of –0.045 (95% CI=–0.073 to –0.016, p<0.01), which corresponds to a number needed to treat of 22 ( Table 2 ). The numbers needed to treat for each study are presented in Figure 1 .
Subgroup and Metaregression Analyses
Because some heterogeneity was observed, we conducted a series of subgroup and metaregression analyses. The results of the subgroup analyses are presented in Table 2 . We examined whether the incidence rate ratio differed according to type of prevention (universal, selective, or indicated), target group (postpartum depression, students, or other), and age group (adolescents or adults). We also examined whether the studies in which subjects with a depressive disorder were excluded at baseline differed significantly from those in which high-risk groups were included without the exclusion of diagnosed cases. Then we examined whether type of intervention (CBT, interpersonal psychotherapy, or other) and format of the intervention (group or individual) were related to the incidence rate ratio.
As indicated in Table 2 , the incidence rate ratio differed significantly in only one subgroup. Studies in which interpersonal psychotherapy was used as an intervention appeared to be significantly more effective than those in which CBT or other interventions were used. Given the small number of comparisons (N=3) examining interpersonal psychotherapy, however, these results should be interpreted with caution.
In most of the subgroup analyses, heterogeneity was low or low to moderate. The subgroups of studies using CBT interventions or interpersonal psychotherapy showed no evidence of heterogeneity. Studies using other interventions had moderate to high heterogeneity, as might have been expected.
We conducted the same subgroup analyses based on the risk differences. As indicated in Table 2 , the type of intervention was again found to be associated with significant differences between subgroups. However, in these analyses, we also found that the different types of prevention (universal, selective, or indicated) differed significantly from each other (p<0.01).
Because universal prevention appeared to differ significantly from selective and indicated preventions, and prevention based on interpersonal psychotherapy differed significantly from the preventions used in the other studies, we conducted another subgroup analysis in which we excluded the two comparisons based on universal prevention and the three comparisons based on interpersonal psychotherapy. The resulting incidence rate ratio was 0.82 (95% CI=0.70–0.98, p<0.05; Q=18.28, n.s.; I 2 =17.92%), and the risk difference in this subgroup of studies was –0.035 (95% CI=–0.063 to –0.007, p<0.05; Q=18.93, n.s.; I 2 =20.74%). The pooled odds ratio (in which we ignored the differences in follow-up period between the studies) was 0.81 (95% CI=0.67–0.98, p<0.05).
We conducted a metaregression analysis to examine the relationship between incidence rate ratio and follow-up period. We found that the follow-up period was inversely related to the incidence rate ratio, although the association did not reach statistical significance (p<0.10; the point estimate of the slope was –0.023; 95% CI=–0.050 to 0.004). This result can be interpreted as an indication that the effects of the intervention become smaller over longer follow-up periods, which may indicate that the preventive interventions delay the onset of disorders rather than preventing them altogether. We also conducted a metaregression analysis to examine whether the incidence rate ratio was related to the number of sessions used in the preventive intervention, but no significant relationship was found.
Discussion
We found clear indications that preventive interventions can significantly reduce the incidence of depressive disorders by 22% compared with treatment-as-usual control groups. This means that prevention should perhaps have a larger role in the further reduction of the disease burden of depressive disorders.
Although preventive interventions appear to be effective in reducing the incidence of depressive disorders, the numbers needed to treat seem to be rather high (22 in the overall analysis). On the other hand, there are no clear guidelines for what is a high number needed to treat and what is not (46) . For example, the regular use of aspirin to reduce the risk of heart attack has become common practice, and the number needed to treat has been found to be 130 (46 , 47) . The number needed to treat associated with the use of cyclosporine in the prevention of organ rejection has been found to be 6.3 and is considered a medical breakthrough of considerable practical importance. A number needed to treat of 22 to prevent the onset of a depressive disorder does not seem unreasonably high, and it is even more favorable if we focus on selective (number needed to treat=16) and indicated prevention (number needed to treat=17).
We found no evidence that the capability of preventive interventions to reduce the incidence of major depression depends on use of specific target groups, such as women at risk of postpartum depression and school interventions directed at students. We did find indications that universal interventions were less effective than selective and indicated interventions. However, universal interventions were examined in only two studies, and pooling of these studies or a comparison with selective or indicated interventions is not very meaningful. The mean incidence rate ratio for universal interventions was not significant and approached a value of 1.0, indicating an absence of effect.
Selective (incidence rate ratio=0.72) and indicated interventions (incidence rate ratio=0.76) had comparable effects. These findings are in agreement with a recent meta-analysis of preventive interventions aimed at depression in children and adolescents (20) . Although that study examined the effects on depressive symptom severity rather than on incidence of depressive disorders, clear indications were found that selected and indicated programs had larger effects than universal programs.
We also found some indications that interventions using interpersonal psychotherapy were more effective than those using CBT. This result must be considered with caution, however, because interpersonal psychotherapy-based interventions were examined in only three studies. Furthermore, in a recent study of a preventive intervention aimed at adolescents, interpersonal psychotherapy and CBT interventions resulted in comparable effect sizes (48) . If interpersonal psychotherapy-based interventions are indeed more effective, this may be related to the fact that this type of intervention focuses more directly on existing problems and high-risk situations than does CBT. For people in high-risk situations or with subthreshold symptoms, this may be exactly what they need.
It is not clear whether the preventive interventions actually reduced the incidence or only delayed onset. Because the follow-up period in most studies did not exceed 2 years, it cannot be concluded that incidence was actually prevented. In fact, we found that the length of the follow-up period was inversely associated with the incidence rate ratio; although not statistically significant, this relationship can be seen as an indication of effect decay over time, which could point to a delay of incidence rather than prevention. From a clinical perspective, both preventing and delaying onset are important. Actual prevention of new cases would of course be preferable, as it would result in avoidance of the disease burden of all prevented cases. Delay of onset is also important, however, because the disease burden of depression is high. Every year during which a potential depressive disorder can be avoided will result in considerably less suffering by patients and their families and may entail a reduction in economic costs.
This study had several limitations. First, the number of studies examining the effects of preventive interventions on the incidence of depressive disorders was relatively small, and the quality of the included studies was not optimal. Also, the included studies examined several different interventions and target populations. However, heterogeneity in our sample of studies was low to moderate, indicating that this may be a fairly homogeneous group of studies. The differences in follow-up periods across the studies constitute another limitation. To try to overcome this limitation, we calculated the number of new cases during follow-up in terms of person-time-based incidence rate ratios, but this approach assumes that the occurrence of new onsets was distributed evenly over the follow-up period. This assumption of an underlying constant hazards model in both groups may not be correct and may have resulted in an underestimation of the incidence rate ratio in the studies with longer follow-up periods or an overestimation in those with shorter follow-up periods. On the other hand, our sensitivity analyses indicated that our results were quite robust and that the underlying constant hazards model is probably acceptable for the relatively brief follow-up periods of the included studies. Because of these limitations, the results of this study should be considered with caution.
It is encouraging to find that prevention of new cases of depressive disorders seems to be feasible. Prevention may be an important way, in addition to treatment, to reduce the enormous burden of depression in the coming years.
1. Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU, Kendler KS: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry 1994; 51:8–19Google Scholar
2. Alonso J, Angermeyer MC, Bernert S, Bruffaerts R, Brugha TS, Bryson H, de Girolamo G, Graaf R, Demyttenaere K, Gasquet I, Haro JM, Katz SJ, Kessler RC, Kovess V, Lépine JP, Ormel J, Polidori G, Russo LJ, Vilagut G, Almansa J, Arbabzadeh-Bouchez S, Autonell J, Bernal M, Buist-Bouwman MA, Codony M, Domingo-Salvany A, Ferrer M, Joo SS, Martínez-Alonso M, Matschinger H, Mazzi F, Morgan Z, Morosini P, Palacín C, Romera B, Taub N, Vollebergh WA; ESEMeD/MHEDEA 2000 Investigators, European Study of the Epidemiology of Mental Disorders (ESEMeD) Project: Prevalence of mental disorders in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr Scand Suppl 2004; 420:21–27Google Scholar
3. Waraich P, Goldner EM, Somers JM, Hsu L: Prevalence and incidence studies of mood disorders: a systematic review of the literature. Can J Psychiatry 2004; 49:124–138Google Scholar
4. Ustun TB, Ayuso-Mateos JL, Chatterji S, Mathers C, Murray CJL: Global burden of depressive disorders in the year 2000. Br J Psychiatry 2004; 184:386–392Google Scholar
5. Saarni SI, Suvisaari J, Sintonen H, Pirkola S, Koskinen S, Aromaa A, Lönnqvist J: Impact of psychiatric disorders on health-related quality of life: general population survey. Br J Psychiatry 2007; 190:326–332Google Scholar
6. Cuijpers P, Smit F: Excess mortality in depression: a meta-analysis of community studies. J Affect Dis 2002; 72:227–236Google Scholar
7. Berto P, D’Ilario D, Ruffo P, Di Virgilio, Rizzo F: Depression: cost-of-illness studies in the international literature: a review. J Ment Health Policy Econ 2000; 3:3–10Google Scholar
8. Greenberg PE, Birnbaum HG: The economic burden of depression in the US: societal and patient perspectives. Exp Opin Pharmacother 2005; 6:369–376Google Scholar
9. Smit F, Cuijpers P, Oostenbrink J, Batelaan N, de Graaf R, Beekman A: Excess costs of common mental disorders: population-based cohort study. J Ment Health Policy Econ 2006; 9:193–200Google Scholar
10. Mathers CD, Loncar D: Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 2006; 3:e442Google Scholar
11. Cuijpers P: Examining the effects of prevention programs on the incidence of new cases of mental disorders: the lack of statistical power. Am J Psychiatry 2003; 160:1385–1391Google Scholar
12. Andrews G, Wilkinson DD: The prevention of mental disorders in young people. Med J Aust 2002; 177:S97–S100Google Scholar
13. Andrews G, Issakidis C, Sanderson K, Corry J, Lapsley H: Utilising survey data to inform public policy: comparison of the cost-effectiveness of treatment of ten mental disorders. Br J Psychiatry 2004; 184:526–533Google Scholar
14. Cuijpers P, van Straten A, Smit F: Preventing the incidence of new cases of mental disorders: a meta-analytic review. J Nerv Ment Dis 2005; 193:119–125Google Scholar
15. Munoz RF: The prevention of depression: current research and practice. Appl Prev Psychol 1993; 2:21–33Google Scholar
16. Gillham JE, Shatté AJ, Freres DR: Preventing depression: a review of cognitive-behavioral and family interventions. Appl Prev Psychol 2000; 9:63–88Google Scholar
17. Anderson CS, Hackett ML, House AO: Interventions for preventing depression after stroke. Cochrane Data Syst Rev 2004; 2:CD003689 (doi: 10.1002/14651858.CD003689.pub2)Google Scholar
18. Dennis CL, Creedy D: Psychosocial and psychological interventions for preventing postpartum depression. Cochrane Data Syst Rev 2004; 4:CD001134 (doi: 10.1002/14651858.CD001134.pub2)Google Scholar
19. Merry S, McDowell H, Hetrick S, Bir J, Muller N: Psychological and/or educational interventions for the prevention of depression in children and adolescents. Cochrane Data Syst Rev 2004; 2:CD003380Google Scholar
20. Horowitz JL, Garber J: The prevention of depressive symptoms in children and adolescents: a meta-analytic review. J Consult Clin Psychol 2006; 74:401–415Google Scholar
21. Higgins JPT, Green S: Cochrane Handbook for Systematic Reviews of Interventions 4.2.6 (updated Sept 2006), in The Cochrane Library 2006, issue 4. Chichester, England, John Wiley & Sons, 2006Google Scholar
22. Rothman KJ, Greenland S: Modern Epidemiology. Philadelphia, Lippincott-Raven, 1998Google Scholar
23. Lau J, Elliott MA, Jimenez-Silva J, Kupelnick B, Mosteller F, Chalmers TC: Cumulative meta-analysis of therapeutic trials for myocardial infarction. N Engl J Med 1992; 327:248–254Google Scholar
24. Higgins JP, Thompson SG, Deeks JJ, Altman DG: Measuring inconsistency in meta-analyses. BMJ 2003; 327:557–560Google Scholar
25. Duval S, Tweedie R: Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000; 56:455–463Google Scholar
26. Allart-van Dam E, Hosman CM, Hoogduin CA, Schaap CP: Prevention of depression in subclinically depressed adults: follow-up effects on the “Coping With Depression” course. J Affect Disord 2007; 97:219–228Google Scholar
27. Brugha TS, Wheatley S, Taub NA, Culverwell A, Friedman T, Kirwan P, Jones DR, Shapiro DA: Pragmatic randomized trial of antenatal intervention to prevent post-natal depression by reducing psychosocial risk factors. Psychol Med 2000; 30:1273–1281Google Scholar
28. Clarke GN, Hawkins W, Murphy M, Sheeber LB, Lewinsohn PM, Seeley JR: Targeted prevention of unipolar depressive disorder in an at-risk sample of high school adolescents: a randomized trial of a group cognitive intervention. J Am Acad Child Adolesc Psychiatry 1995; 34:312–321Google Scholar
29. Clarke GN, Hornbrook M, Lynch F, Polen M, Gale J, Beardslee W, O’Connor E, Seeley J: A randomized trial of a group cognitive intervention for preventing depression in adolescent offspring of depressed parents. Arch Gen Psychiatry 2001; 58:1127–1134Google Scholar
30. Elliott SA, Leverton TJ, Sanjack M, Turner H, Cowmeadow P, Hopkins J, Bushnell D: Promoting mental health after childbirth: a controlled trial of primary prevention of postnatal depression. Br J Clin Psychol 2000; 39:223–241Google Scholar
31. Gillham JE, Hamilton J, Freres DR, Patton K, Gallop R: Preventing depression among early adolescents in the primary care setting: a randomized controlled study of the Penn Resiliency Program. J Abnorm Child Psychol 2006; 34:203–219Google Scholar
32. Hagan R, Evans SF, Pope S: Preventing postnatal depression in mothers of very preterm infants: a randomised controlled trial. BJOG 2004; 111:641–647Google Scholar
33. Martinovic Z, Simonovic P, Djokic R: Preventing depression in adolescents with epilepsy. Epilepsy Behav 2006; 9:619–624Google Scholar
34. Muñoz RF, Ying YW, Bernal G, Perez-Stable EJ, Sorensen JL, Hargreaves WA, Miranda J, Miller LS: Prevention of depression with primary care patients: a randomized controlled trial. Am J Community Psychol 1995; 23:199–222Google Scholar
35. Muñoz RF, Le HN, Ippen CG, Diaz MA, Urizar GG Jr, Soto J, Mendelson T, Delucchi K, Lieberman AF: Prevention of postpartum depression in low-income women: development of the Mamás y Bebés/Mothers and Babies Course. Cogn Behav Pract 2007; 14:70–83Google Scholar
36. Priest S, Henderson J, Evans S, Hagan R: Stress debriefing after childbirth: a randomized controlled trial. Med J Aust 2003; 178:542–545Google Scholar
37. Rovner BW, Casten RJ, Hegel MT, Leiby BE, Tasman WS: Preventing depression in age-related macular degeneration. Arch Gen Psychiatry 2007; 64:886–892Google Scholar
38. Seligman MEP, Schulman P, DeRubeis RJ, Hollon SD: The prevention of depression and anxiety. Prevention and Treatment 1999, vol 2 (doi: 10.1037/1522-3736.2.1.28a)Google Scholar
39. Sheffield JK, Spence SH, Rapee RM, Kowalenko N, Wignall A, Davis A, McLoone J: Evaluation of universal, indicated, and combined cognitive-behavioral approaches to the prevention of depression among adolescents. J Consult Clin Psychol 2006; 74:66–79Google Scholar
40. Spence S, Sheffield J, Donovan C: Preventing adolescent depression: an evaluation of the problem solving for life program. J Consult Clin Psychol 2003; 71:3–13Google Scholar
41. Willemse GRWM, Smit F, Cuijpers P, Tiemens BG: Minimal-contact psychotherapy for sub-threshold depression in primary care: randomised trial. Br J Psychiatry 2004; 185:416–421Google Scholar
42. Young JF, Mufson L, Davies M: Efficacy of Interpersonal Psychotherapy-Adolescent Skills Training: an indicated preventive intervention for depression. J Child Psychol Psychiatry 2006; 47:1254–1262Google Scholar
43. Zlotnick C, Johnson SL, Miller IW, Pearlstein T, Howard M: Postpartum depression in women receiving public assistance: pilot study of an interpersonal-therapy-oriented group intervention. Am J Psychiatry 2001; 158:638–640Google Scholar
44. Zlotnick C, Miller IW, Pearlstein T, Howard M, Sweeney P: A preventive intervention for pregnant women on public assistance at risk for postpartum depression. Am J Psychiatry 2006; 163:1443–1445Google Scholar
45. Mrazek PJ, Haggerty RJ: Reducing Risks for Mental Disorders: Frontiers for Preventive Intervention Research. Washington, DC, National Academies Press, 1994Google Scholar
46. Kraemer HC, Kupfer DJ: Size of treatment effects and their importance to clinical research and practice. Biol Psychiatry 2006; 59:990–996Google Scholar
47. Rosenthal R, Rosnow RL, Rubin DB: Contrasts and Effect Sizes in Behavioral Research. Cambridge, England, Cambridge University Press, 2000Google Scholar
48. Horowitz JL, Garber J, Ciesla JA, Young JF, Mufson L: Prevention of depressive symptoms in adolescents: a randomized trial of cognitive-behavioral and interpersonal prevention programs. J Consult Clin Psychol 2007; 75:693–706Google Scholar