The Occupational Burden of Mental Disorders in the U.S. Military: Psychiatric Hospitalizations, Involuntary Separations, and Disability
Abstract
OBJECTIVE: A recent study showed that among U.S. military personnel, mental disorders were the leading medical correlate of separation from military service. The reasons for this association have not been determined. The purpose of this study was to characterize the risk and reasons for service separation for soldiers hospitalized with mental disorders compared with those hospitalized for other illnesses. METHOD: Population-based electronic health care data were linked with data on separations and disability. The authors constructed a cohort of 13,971 U.S. Army soldiers first hospitalized in 1998 and followed them for up to 2 years following this first hospitalization. RESULTS: The rate of service separation 6 months after first hospitalization was 45% among personnel whose primary hospital discharge diagnosis was a mental disorder, 27% among those with a secondary mental disorder discharge diagnosis, and 11% among those hospitalized for all other medical conditions. Separation from military service due to medical disability, misconduct and other legal problems, unauthorized work absences, behavior related to personality disorders, and alcohol rehabilitation failure was significantly more common following hospitalization for a mental disorder than for other medical conditions. Mental disorders were also significantly associated with medical separations in which there was evidence that the condition existed prior to service. CONCLUSIONS: In the military, the occupational impact of mental disorders compared with other medical conditions appears to be mediated not only by greater disease chronicity and severity but also by a variety of behavioral problems including misconduct, legal problems, unauthorized absences, and alcohol/drug-related problems. The study also points to the difficulties inherent in screening for mental disorders prior to entry into military service.
Multiple studies have shown that in the general population mental disorders are associated with significant occupational morbidity including work absenteeism, reduced productivity, unemployment, and disability as well as high health care utilization and social impairment (1–7). The U.S. military represents an important segment of the general working U.S. adult population and is ideal for studies of the occupational impact of mental disorders for several reasons. First, the population comprises predominantly young working adults, a group traditionally understudied in psychiatric epidemiology studies. Second, there is universal access to excellent health care services. Finally, there is nearly complete capture of population-based demographic, occupational, and health information in electronic administrative and health records (8).
A previous study showed that among active-duty military personnel, mental disorders are the leading cause of hospitalization in men and the second leading cause in women (below pregnancy), accounting for more hospitalizations than either injuries or musculoskeletal disorders (8). Among the 1.4 million service members on active duty, 6%–10% receive treatment for a mental health problem each year (8, 9).
Mental disorders are strongly correlated with attrition (8, 9). In one study nearly 50% of service members hospitalized for a mental disorder separated from military service within 6 months compared with only 12% of those hospitalized for any of 15 other major illness categories (8). To date, the reasons for the disproportionately high attrition rates among service members with mental disorders relative to those with other medical conditions have not been systematically studied. Possible contributing factors include higher levels of disability or disease chronicity for mental disorders compared with other illness categories, career stigmatizing effects of mental disorders, and associations between mental disorders and behavioral problems that may not be conducive to military service (10).
The comprehensive electronic data systems in the military offer an unprecedented opportunity to conduct population-based research to characterize the complex relationship between utilization of health care services and occupational morbidity (10). This study presents data from an in-depth analysis of the risk factors and reasons for separation following hospitalization for mental disorders compared with hospitalizations for other illnesses among active-duty Army personnel. In addition to showing that mental disorders are independently associated with attrition after demographic variables are controlled, the study characterizes the reasons for separation and the association with disability.
Method
The Database
This study used the Total Army Injury and Health Outcomes Database (11, 12), an integrated database capturing electronic health and occupational data from all active-duty U.S. Army soldiers (in 1998, total N=512,771; enlisted N=430,474). Data from the Total Army Injury and Health Outcomes Database used in this study included 1) demographic and occupational data for all active-duty Army personnel obtained from the Defense Manpower Data Center, 2) electronic data from all hospitalizations at military treatment facilities, including dates of hospitalization and discharge diagnoses obtained from the Patient Administration System and Biostatistics Activity, and 3) data on medical disabilities from the Army Physical Disability Case Processing System. Demographic and occupational data from the Defense Manpower Data Center used in this study included age, gender, race/ethnicity, rank, education, length of service, and the reason for separation if the soldier left military service during the study period. Only aggregate data without identifiers were assembled for the research team by personnel authorized to access the databases. The study was approved by the institutional review boards of the Walter Reed Army Institute of Research and the U.S. Army Research Institute of Environmental Medicine, and the study adhered to policies for the protection of human subjects (13, 14).
Constructing the Cohort
The cohort comprised all active-duty U.S. Army enlisted soldiers who were hospitalized in 1998 and had no hospitalizations recorded in the military health care system in the two previous years (N=14,065). Excluding individuals who were hospitalized during the 2 years before the onset of the study increased the likelihood that the hospitalizations captured in this study were first hospitalizations. An exception was made for women whose only hospitalization in 1996 or 1997 was for pregnancy.
Inpatient data included dates of admission and discharge and discharge diagnoses (up to eight allowed). Diagnoses were specified per ICD-9-CM, with mental disorders coded in the 290–319 range. Mental disorders were compared with the 15 nonpsychiatric ICD-9-CM illness categories (8).
The Total Army Injury and Health Outcomes Database obtains demographic data from the Defense Manpower Data Center personnel master files on all active-duty Army service members biannually in June and December, and additional data on those who are separated from service anytime during the 6-month interval. To construct the cohort, inpatient hospitalization records were matched to the demographic data using the 6-month Defense Manpower Data Center installment that was closest to the date of hospitalization. Identifiers from approximately 2.5% of all hospitalizations did not match personnel records, and these hospitalizations were dropped from the study. These nonmatches were likely due to errors in the identifiers or in the accuracy of codes related to service status or involved trainees who were in service for less than 6 months. Of the 14,065 soldiers included in the cohort, there were 1,500 (10.7%) who had more than one hospitalization in 1998. In these cases, only the first hospitalization was included.
Cohort Grouping by Discharge Diagnosis
All first hospitalization records were categorized into three mutually exclusive categories. Group 1 consisted of those records in which an ICD-9-CM mental disorder code between 290 and 319 was listed as the primary hospital discharge diagnosis. Group 2 consisted of those records in which a mental disorder code was listed as one of the seven possible secondary discharge diagnoses and a nonpsychiatric illness code was listed as the primary diagnosis. Group 3 consisted of all other hospitalizations in which there was no mental disorder listed in any of the eight diagnosis fields. Among those included in the first group, mental disorder primary discharge diagnoses were further grouped by using previously described methods (8) to map the ICD-9-CM codes to six DSM-IV categories: mood/anxiety disorders, alcohol/substance-related disorders, personality disorders, adjustment disorders, psychotic disorders, and other mental disorders.
Military Separation Data
Records related to all service separations among active-duty Army personnel obtained from the Defense Manpower Data Center were available through the end of 1999, providing a minimum of 1 year and a maximum of 2 years of follow-up for all persons in the cohort. These records included the reason for military separation (separation program designator codes) and dates of separation, which were matched with the hospitalization dates and demographic data. Individuals were excluded if the date of separation was before the recorded hospitalization date (94 individuals), and validation was conducted to assure that soldiers who changed categories (for example from enlisted to officer) were not miscounted as military separations. The final cohort consisted of 13,971 enlisted soldiers who had at least one hospitalization in 1998.
Analysis
The three discharge diagnosis groups (primary mental disorder, secondary mental disorder, all other diagnoses) were compared in terms of rate and reasons for service separation by using chi-square tests. Cox proportional hazards models were used to assess the association between demographic risk factors and separation. The potential time for follow-up length varied among the cohort, since the start time for individuals could have occurred any time in 1998. Because of this dynamic nature of the cohort and the possibility of right censoring, standard survival analysis techniques were used to model time until service separation. Kaplan-Meier curves adjusted for demographic data were generated by using the mean of covariates method (mean values of the covariates are inserted into the survival function of the proportional hazards model to estimate survival probability). Analyses were conducted with SAS Version 8.2 statistical package and Epi-Info 6.0 software (Centers for Disease Control).
Results
Association Between Hospitalization for a Mental Disorder and Service Attrition
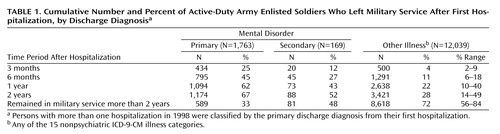
The cohort consisted of 13,971 active-duty Army enlisted soldiers with hospitalizations in 1998. Table 1 shows the cumulative number and the percent of soldiers who left military service after a mental disorder hospitalization compared with hospitalizations for other medical conditions; these data replicate findings from our previous study (8). Forty-five percent of soldiers hospitalized for the first time in 1998 with a mental disorder as their primary diagnosis left military service within 6 months after their hospitalization, compared with only 11% of those hospitalized for other medical illnesses (relative risk=4.21, 95% CI=3.91–4.52, χ2=1415.86, df=1, p<0.0001). The 6-month attrition rate for the 15 nonpsychiatric illness categories ranged from 6% to 18%, substantially lower than the 45% attrition observed for those with mental disorders. The separation rate for soldiers who received a secondary diagnosis of a mental disorder was also significantly higher than for soldiers hospitalized for nonpsychiatric illness categories (27% versus 11%) (relative risk=2.48, 95% CI=1.92–3.21, χ2=43.25, df=1, p<0.0001).
Cox proportional hazards multivariate models that included discharge diagnosis, age, gender, rank, duration of service, marital status, education, and race/ethnicity confirmed the strong association between separation from service and mental disorder relative to no mental disorder diagnosis after these other variables were controlled (primary mental disorder diagnosis: hazard ratio=3.52, 95% CI=3.29–3.78; secondary mental disorder diagnosis: hazard ratio=2.10, 95% CI=1.70–2.60). The analysis also showed that younger age, single marital status, Caucasian race, shorter duration of service, and lower rank were all significantly associated with attrition from service, whereas gender and education were not. Survival curves adjusted for these demographic variables are presented in Figure 1, showing the percentage of soldiers in each diagnostic group who remained in the Army over time. Due to colinearity between length of service and age, only age was included in this model.
Reasons for Service Separation
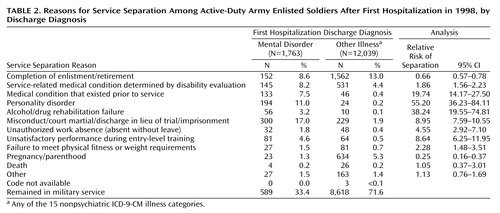
Table 2 shows the reasons for separation, per Army separation codes, for soldiers who left the service during the follow-up period after their first hospitalization. The most common reason for separation among the 12,039 soldiers hospitalized for reasons other than a mental disorder was voluntary in nature: completion of enlistment or retirement. In contrast, for those hospitalized for a mental disorder, involuntary reasons for separation were significantly more common. Mental disorders were strongly associated with medical separations that involved disability determinations for conditions originating on active duty (χ2=48.02, df=1, p<0.0001). Mental disorder hospitalizations were also significantly associated with another category of medical separation involving conditions that preexisted joining military service (χ2=616.14, df=1, p<0.0001).
Other involuntary reasons for separation that were significantly more common among those hospitalized for mental disorders compared with those hospitalized for other medical conditions included misconduct and other legal problems, personality disorders, alcohol and drug rehabilitation failure, unauthorized absence from work, failure to meet physical fitness or weight requirements, and unsatisfactory performance during entry-level training (χ2=14.60–1154.75, df=1, p≤0.001). Entry-level training separations are separations that occur in the first 6 months of service usually due to failure to meet performance standards or problems adjusting to military training.
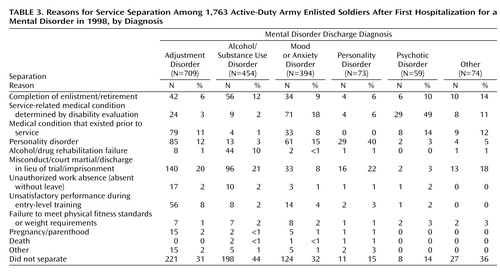
Among the 1,763 service members hospitalized for a mental disorder, 709 (40%) had a primary discharge diagnosis of an adjustment disorder, 454 (26%) had an alcohol/substance use disorder, 394 (22%) had a mood/anxiety disorder, 73 (4%) had a personality disorder, 59 (3%) had a psychotic disorder, and 74 (4%) had another mental disorder diagnosis. Table 3 shows the reasons for separation for each of these diagnostic categories.
Data on service separations were compared with the official electronic records from the administrative database of the Army Physical Disability Agency, which were available through December 2000. This database records the results of all disability evaluations, which are based on the evaluations of clinicians and reviewers who determine the level of occupational impairment and the percent disability. The separation records showed excellent correlation with the disability database. Of the 145 soldiers in group 1 and the 531 in group 3 coded as having a service-related medical separation, 143 (98.6%) and 529 (99.6%), respectively, had a record of a disability evaluation in the Army Physical Disability database. Of all remaining 3,919 separations in group 1 and group 3 not coded as a service-related medical discharge, only 161 (4%) had a record of receiving a disability evaluation in the database. In addition, there was a high correlation between the primary hospital discharge diagnosis and the diagnosis code used in the disability record under the Department of Veterans Affairs System for Rating Disabilities. Among the 143 persons with mental disorder hospitalizations, 102 (71%) had a primary disability diagnosis of a mental disorder, 27 (19%) were coded as having a musculoskeletal disability, five (4%) as having a neurological condition, and eight (5%) as having another disability diagnosis or no code listed. Among the 529 persons hospitalized for reasons other than a mental disorder, only 14 (3%) received a mental disorder disability diagnosis. Overall, mental disorders were the second leading category of disability in the Army, with musculoskeletal conditions being the most common category. Of the 143 persons with mental disorder hospitalizations, 86 (60%) were rated as having 30% or greater disability compared to 165 (31%) of the 529 persons with other types of disability diagnoses (χ2=41.81, df=1, p<0.0001).
Discussion
This study confirmed previous findings demonstrating the considerable occupational morbidity attributable to mental disorders in the U.S. military (8). The study provides new data on the reasons for service separation and the association of mental disorders with disability. The attrition rate within 6 months following hospitalization for a mental disorder was 45% compared with 11% following hospitalization for any other illness category, and multivariate analyses that controlled for demographic variables confirmed the strong association with attrition. In addition, this study showed that having a secondary mental disorder diagnosis also conferred an increased risk of attrition (27% at 6 months).
This is the first study to correlate hospitalizations for mental disorders with military separations and disability using additional administrative databases. Mental disorder hospitalizations were significantly associated with service-related medical disability separations. Overall, 8% of soldiers hospitalized for mental disorders received a medical separation compared with 4% of those hospitalized for other medical conditions, and the level of disability awarded was significantly higher among those with mental disorders compared with persons treated for other conditions. In the military, 30% disability has particular significance because this generally entitles a service member with less than 20 years of service to retirement benefits (15). In aggregate, these findings add to the growing literature documenting the disabling, chronic, and costly nature of mental disorders compared with other medical conditions (1–7, 16).
Mental disorder hospitalizations were significantly associated with a variety of other involuntary separation categories. Not surprisingly, mental disorder hospitalizations were associated with separations due to personality disorders and alcohol rehabilitation failure, both of which involve behaviors that are not considered conducive to further service if they continue after appropriate counseling or treatment. It is also not surprising that there was an association between mental disorder hospitalizations and separations due to misconduct and other legal problems. However, the magnitude of this association was unexpected. Overall, 17% of all soldiers hospitalized for mental disorders were involuntarily separated due to misconduct and other legal problems, accounting for one-quarter of all separations among these soldiers. These types of separations include serious offenses involving criminal behavior, use of illegal drugs (routinely checked through random urine testing throughout a service member’s career), or a repetitive pattern of lesser offenses (15). Also, mental disorders were significantly associated with unauthorized absences and training separations (which include failure to adjust to the military or unsatisfactory performance during the initial 6-month training period), also reflected in the high rate of hospitalizations related to adjustment disorders. Regarding mental disorder diagnoses, psychotic, mood, and anxiety disorders were much more likely to be associated with a medical discharge and disability, whereas substance use disorders, adjustment disorders, and personality disorders were more often associated with other types of involuntary separations.
Further work is needed to understand these associations. However, it appears clear that in many cases the occupational impact of mental disorders, as defined by the utilization of inpatient psychiatric services and attrition, is mediated by conduct, antisocial, and related behavioral problems. These data complement other research demonstrating the marked occupational and social impact of impulse control and personality disorders (17, 18), as well as data from the recent National Comorbidity Survey in which impulse control disorders were found to be one of the three leading causes of comorbidity in depressed persons (6). The Army predominantly consists of young men (87%), a population at high risk for health risk behaviors, including alcohol/drug abuse and conduct problems. With universal access to mental health services and a social environment in which service members often live and work together, these behavioral problems may intersect with psychiatric inpatient services differently than they do in civilian populations. Criteria for psychiatric hospitalization are similar in military and civilian settings (particularly threat to self or others). However, in the military there may be a higher likelihood of initially involving mental health services rather than law enforcement for behavioral control of misconduct such as aggression or substance abuse. There are also potential differences in diagnostic practices between military and civilian settings. In civilian settings, insurance will not likely reimburse for adjustment disorder diagnoses, whereas military health care providers do not have the same constraints in assigning diagnoses. This raises a number of questions about the influence that the practice environment may have on diagnostic prescribing, a topic that is beyond the scope of this study but one that has received attention in the literature (19, 20) and is being researched further (9).
Although the military is a unique occupational environment, the data have important implications for measuring the burden of mental disorders in the general population. Without the behavioral health care interface, it is likely that the occupational impact of mental disorders often goes unrecognized in civilian settings. For example, behaviors related to adjustment disorders, personality disorders, alcohol abuse, or misconduct may lead to resignation or rapid termination from a civilian job setting, whereas in the military these problems may involve mental health referral, counseling, and rehabilitation efforts before culminating in involuntary separation. Despite the high proportion of hospitalizations labeled as adjustment disorders and the link with behavioral problems such as misconduct, recent comparisons with National Hospital Discharge Survey data suggest that the overall rate of psychiatric hospitalizations in the military is comparable to the rate in civilian populations (9, 21), further supporting the generalizability of our findings.
Another important finding in this study was the association between mental disorders and medical separations in which there was evidence that the condition existed prior to service. These can occur when a medical condition that would normally disqualify someone from service is not detected during the entry medical evaluation but is discovered sometime during the first 6 months of service. The fact that these separations were significantly higher among those with mental disorders (8%) than among those with other conditions (<1%) speaks to the many problems inherent in screening applicants for mental disorders prior to coming into service (22).
The principal limitation of this study was the reliance on administrative data systems to assess the reasons for service separation. However, there are good data on the validity and usefulness of automated health care utilization data in the military (8, 9, 12, 23, 24). Also, the very high correlation that we found between different administrative data systems supports the validity of these data. Another limitation is that this study focused exclusively on persons who were hospitalized, representing a very small proportion of the total number of people with mental disorders in the population. Additional research involving the ambulatory health care data systems is needed to characterize the full occupational burden of mental disorders in the military.
 |
 |
 |
Received Oct. 1, 2003; revisions received Jan. 9, 2004, and March 22, 2004; accepted May 10, 2004. From the Department of Psychiatry and Behavioral Sciences, Division of Neuropsychiatry, Walter Reed Army Institute of Research; the U.S. Army Research Institute of Environmental Medicine, Total Army Injury and Health Outcomes Database Project, Natick, Mass.; Social Sectors Development Strategies, Inc., Natick, Mass.; and the Health Policy and Services Directorate, Headquarters, U.S. Army Medical Command, Fort Sam Houston, Tex. Address correspondence and reprint requests to Dr. Hoge, Walter Reed Army Institute of Research, 503 Robert Grant Ave., Silver Spring, MD 20910; [email protected] (e-mail). The views expressed are those of the authors and do not reflect the official position of the Department of the Army, the Department of Defense, the U.S. Government, or any of the institutional affiliations listed above.
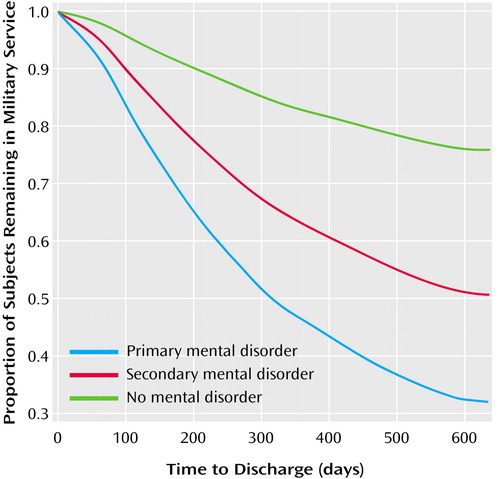
Figure 1. Service Attrition Among Active-Duty Army Enlisted Soldiers After First Hospitalization in 1998, by Discharge Diagnosisa
aSurvival curves are adjusted for demographic variables (age, gender, rank, education, marital status, and race).
1. Wells KB, Stewart A, Hays RD, Burnam MA, Rogers W, Daniels M, Berry S, Greenfield S, Ware J: The functioning and well-being of depressed patients: results from the Medical Outcomes Study. JAMA 1989; 262:914–919Crossref, Medline, Google Scholar
2. Hays RD, Wells KB, Sherbourne CD, Rogers W, Spritzer K: Functioning and well-being outcomes of patients with depression compared with chronic general medical illness. Arch Gen Psychiatry 1995; 52:11–19Crossref, Medline, Google Scholar
3. Wells KB, Sherbourne CD: Functioning and utility for current health of patients with depression or chronic medical conditions in managed, primary care practices. Arch Gen Psychiatry 1999; 56:897–904Crossref, Medline, Google Scholar
4. Johnson J, Weissman MM, Klerman GL: Service utilization and social morbidity associated with depressive symptoms in the community. JAMA 1992; 267:1478–1483Crossref, Medline, Google Scholar
5. Kessler RC, Frank RG: The impact of psychiatric disorders on work loss days. Psychol Med 1997; 27:861–873Crossref, Medline, Google Scholar
6. Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Rush AJ, Walters EE, Wang PS: The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA 2003; 289:3095–3105Crossref, Medline, Google Scholar
7. Narrow WE, Regier DA, Rae DS, Mandersheid RW, Locke BZ: Use of services by persons with mental and addictive disorders: findings from the National Institute of Mental Health Epidemiologic Catchment Area program. Arch Gen Psychiatry 1993; 50:95–107Crossref, Medline, Google Scholar
8. Hoge CW, Lesikar SE, Guevara R, Lange J, Brundage JF, Engel CC, Messer SC, Orman DT: Mental disorders among US military personnel in the 1990s: association with high levels of health care utilization and early military attrition. Am J Psychiatry 2002; 159:1576–1583Link, Google Scholar
9. Garvey-Wilson AL, Hoge CW, Messer SC, Lesikar SE, Eaton KM: Diagnoses in behavioral health clinics: impact on perceived burden of mental health, in 2003 Annual Meeting New Research Program and Abstracts. Washington, DC, American Psychiatric Association, 2003, number 53Google Scholar
10. Hoge CW, Messer SC, Engel CC, Krauss M, Amoroso P, Ryan MAK, Orman DT: Priorities for psychiatric research in the US military: an epidemiological approach. Mil Med 2003; 168:182–185Crossref, Medline, Google Scholar
11. Amoroso PJ, Yore MM, Weyandt B, Jones BH: Total Army Injury and Health Outcomes Database: a model comprehensive research database. Mil Med 1999; 164(suppl 8):1–36Google Scholar
12. Miller M, Hemenway D, Bell NS, Yore MM, Amoroso PJ: Cigarettes and suicide: a prospective study of 300,000 male active duty Army soldiers. Am J Epidemiol 2000; 151:1060–1063Crossref, Medline, Google Scholar
13. Army Regulation 70–25: Research and Development: Use of Volunteers as Subjects of Research. Washington, DC, US Department of the Army, Jan 25, 1990Google Scholar
14. Code of Federal Regulations, Title 45, Public Welfare, Part 46: Protection of Human Subjects (45 CFR 46). Washington, DC, Department of Health and Human Services, National Institutes of Health, 1991Google Scholar
15. Army Regulation 635–40: Physical Evaluation for Retention, Retirement, or Separation. Washington, DC, US Department of the Army, Aug 15, 1990Google Scholar
16. Ormel J, VonKorff M, Ustun B, Pini S, Korten A, Oldehinkel T: Common mental disorders and disability across cultures: results from the WHO collaborative study on psychological problems in general health care. JAMA 1994; 272:1741–1748Crossref, Medline, Google Scholar
17. Black DW: Bad Boys, Bad Men: Confronting Antisocial Personality Disorder. New York, Oxford University Press, 1999Google Scholar
18. Gunderson EKE, Hourani LL: The epidemiology of personality disorders in the US Navy. Mil Med 2003; 168:575–582Crossref, Medline, Google Scholar
19. Wynia MK, Cummins DS, VanGeest JB, Wilson IB: Physician manipulation of reimbursement rules for patients: between a rock and a hard place. JAMA 2000; 283:1858–1865Crossref, Medline, Google Scholar
20. Freeman VG, Rathore SS, Weinfurt KP, Schulman KA, Sulmasy DP: Lying for patients: physician deception of third-party payers. Arch Intern Med 1999; 159:2263–2270Crossref, Medline, Google Scholar
21. Kozak LJ, Hall MJ, Owings MF: National Hospital Discharge Survey: 2000 annual summary with detailed diagnosis and procedure data. Vital Health Stat 13 2002; 153:1–194Medline, Google Scholar
22. Jones E, Hyams KC, Wessely S: Screening for vulnerability to psychological disorders in the military: an historical survey. J Med Screen 2003; 10:40–46Crossref, Medline, Google Scholar
23. Dlugosz LJ, Hocter WJ, Kaiser KS, Knoke JD, Heller JM, Hamid NA, Reed RJ, Kendler KS, Gray GC: Risk factors for mental disorder hospitalization after the Persian Gulf War: US Armed Forces, June 1, 1991-September 30, 1993. J Clin Epidemiol 1999; 52:1267–1278Crossref, Medline, Google Scholar
24. Bell NS, Williams JO, Senier L, Strowman SR, Amoroso PJ: The reliability and validity of the self-reported drinking measures in the Army’s Health Risk Appraisal Survey. Alcohol Clin Exp Res 2003; 27:826–834Crossref, Medline, Google Scholar



