Extensions of Errorless Learning for Social Problem-Solving Deficits in Schizophrenia
Abstract
OBJECTIVE: There is a clear need to develop psychosocial rehabilitation methods that compensate for neurocognitive deficits common to persons with severe and persistent mental illness. Errorless learning, a compensatory training intervention, has been successful in teaching entry-level job tasks. However, errorless learning’s applicability to broader, more complex functions is unknown. The present study tested the extension of errorless learning for deficits in social problem-solving skills in patients with schizophrenia. METHOD: Sixty clinically stable outpatients with schizophrenia or schizoaffective disorder were stratified by gender and level of memory impairment before being randomly assigned to one of two training programs: errorless learning or symptom management. Groups were matched for training time, format and structure of training, and types of teaching aids used. Social problem-solving ability, measured by the Assessment of Interpersonal Problem-Solving Skills, was assessed at baseline, within 2 days of training completion, and after 3 months. Dependent measures were the scores for the receiving, processing, and sending skills areas from the Assessment of Interpersonal Problem-Solving Skills. RESULTS: A repeated-measures analysis of covariance was conducted for each dependent measure with baseline Assessment of Interpersonal Problem-Solving Skills score entered as a covariate. For all three skills, there was a significant training group effect favoring errorless learning. Durability of errorless learning training effects extended to the 3-month follow-up assessment for processing and sending skills but not receiving skills. CONCLUSIONS: Results support the extension of errorless learning to complex functions such as social problem-solving skills in the rehabilitation of persons with schizophrenia.
More than 60 studies have provided empirical support for a relationship between neurocognition and community functioning among persons with schizophrenia (1). These findings emphasize the role of neurocognition, more than psychotic symptoms, in cross-sectional and prospective links to functional outcome. The neurocognitive functions most frequently implicated involve learning and memory, attention, and reasoning and problem-solving abilities. Despite this extensive knowledge base, few efforts have attempted to apply this knowledge to develop more effective rehabilitation interventions for persons with schizophrenia (2).
Errorless learning is a training approach designed to compensate for impairments in neurocognition that impede or restrict skill acquisition. Errorless learning is based on a theoretically and empirically driven model, which proposes that learning occurring in the absence of errors is stronger and more durable. First introduced as an alternative to trial-and-error learning (3), errorless learning has been used extensively with the developmentally disabled and other neurologically impaired groups to teach new skills and curb maladaptive behavior (4–7). However, applications of errorless learning to schizophrenia patients have only appeared recently (8, 9).
Among the neurocognitive disturbances common to schizophrenia, impairments in learning may be the most severe (10–12). Patient performance on tasks involving learning and recall of word lists and short passages is typically poorer compared with normal subjects (13, 14), and their performance is marked by perseverative and intrusion errors (15). Performance is also compromised by problems in the ability to self-correct (i.e., using feedback to correct past mistakes and guide subsequent behavior), a disturbance prevalent in both neurocognitive test performance and clinical behavior (16, 17). It is likely that a psychosocial intervention that bypasses problems associated with error commission would hold promise for persons with schizophrenia.
Errorless learning has four components. 1) The to-be-learned task is broken down into component parts. 2) Training begins on simple tasks that have a high likelihood of success. 3) Training proceeds through hierarchically ordered exercises in which the tasks are gradually made more difficult. High levels of proficiency are achieved at each level by using multiple instructional aids (e.g., prompts, visual cues, guided instruction). 4) Performance within each component is overlearned through repetitive, successful practice and a rich schedule of positive reinforcement. Errorless learning shares methodological features with other rehabilitation training approaches (e.g., cognitive rehabilitation training, behavioral shaping) (18–20), but it differs conceptually in its view of the significance of errors on learning and differs methodologically by inclusion of training procedures specifically tailored to prevent mistakes from occurring.
The application of errorless learning to psychiatric patients has relied on an extensive literature on developmental disabilities. From this literature, errorless learning has been shown to be a successful teaching approach for children with severe cognitive impairment. However, its extensions to broader aspects of human behavior have been limited. Two of the more prominent criticisms of errorless learning include 1) that it is geared for training on simple tasks but not complex ones, and 2) that training success is tied to improvement on the trained-on task and, with few exceptions, does not extend to other similar tasks (21). Although these limitations have been uncovered with developmental disabilities, it is not known whether the same problems apply to schizophrenia. A previous effort from our lab demonstrated that errorless learning could be successfully applied to teaching entry-level job tasks in a group of schizophrenia and schizoaffective disorder outpatients, but the aforementioned limitations were not tested (9). The tasks in that study were relatively simple, and training took place on the to-be-learned task. For the present study, our aims were twofold: 1) develop a set of errorless learning training procedures for highly complex functions (social problem-solving skills), and 2) design the training procedures so that skills learned could be applied in different situations. The primary goal was to see if we could overcome the limitations of errorless learning that would be necessary to address if this training method is to have a place in the rehabilitation of persons with schizophrenia.
Method
Subjects
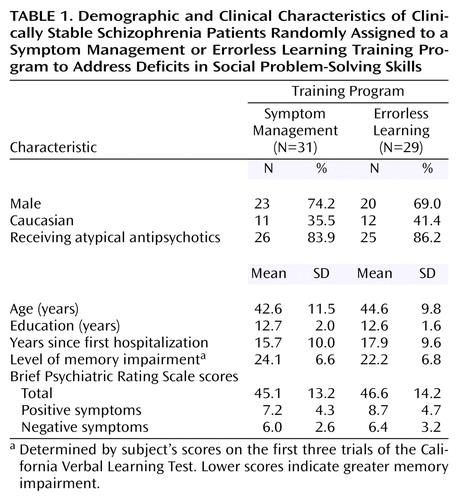
Sixty subjects from the VA Greater Los Angeles Healthcare Center and the San Fernando Mental Health Center who met DSM-IV criteria for schizophrenia or schizoaffective disorder participated. Psychiatric diagnosis was determined following administration of the Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition (SCID-P) (22) by an interviewer trained to use the SCID-P by the Diagnosis and Psychopathology Unit of the UCLA Clinical Research Center for the Study of Schizophrenia. A minimum kappa of 0.75 for rating the presence of psychotic and mood items is required for certification. Subjects were clinically stable outpatients (no psychiatric hospitalizations in the past 6 months, same antipsychotic medication for past 3 months). Exclusion criteria were evidence of current or past neurological disorder (e.g., epilepsy), mental retardation, or substance dependence within the past 3 months. Antipsychotic medication type and dose were not controlled in the study but were left to the discretion of the subjects’ treating physician. Table 1 presents the characteristics of the subjects. After complete description of the study to subjects, written informed consent was obtained.
Procedure
Gender and memory status are variables associated with differential performance levels on measures of social skill and problem-solving ability (23, 24) To ensure baseline equivalency, subjects were stratified on these variables before being randomly assigned to their training group (errorless learning or symptom management). Level of memory impairment (high versus low) was determined by subjects’ scores on the first three trials of the California Verbal Learning Test (25). On the basis of previous data with a similar sample (26), a dividing score of 22.5 was selected. For each subject, a slip of paper denoting group assignment was kept in a sealed envelope until baseline assessments were completed and classification according to stratified variables was determined. To ensure proportional assignment within cells, a separate set of randomization numbers was used for each of the four classification cells (i.e., male/high memory impairment; female/high memory impairment; male/low memory impairment; female/low memory impairment). Thus, for every 10 subjects per cell there was a 50:50 chance of assignment to errorless learning versus symptom management.
The groups were equated for total training time, group structure and format, and types of instructional aids used. Training, in groups of six to eight subjects with one instructor and two assistants, took place over 6 hours, split over 2 days. For both groups, training included didactic and videotape instruction, modeling and social reinforcement, role-play exercises, and in-class written assignments. To ensure that these procedures were implemented consistently, a fidelity checklist was completed during each session noting their use.
Social problem-solving ability was assessed at baseline (prior to group assignment), 0–2 days after training, and 3 months later with the Assessment of Interpersonal Problem-Solving Skills. This instrument is a measure of social problem-solving ability well-validated in studies of schizophrenia (27, 28). It includes videotape presentations of 13 scenes involving various social situations. Ten of the scenes depict a social conflict (e.g., roommate disagreements, being ignored by a store clerk); three do not. Subjects’ skills are assessed in three areas: 1) receiving (i.e., identifying the presence/absence of a problem), 2) processing (i.e., generating a solution), and 3) sending (i.e., demonstrating the solution via role-play). The test requires 45–60 minutes administration time. Subject responses were recorded via verbatim transcripts; the role-play exercises were videotaped. Transcripts and videotapes were scored by two raters blind to group assignment and time of administration.
The principal investigator’s training of those scoring the Assessment of Interpersonal Problem-Solving Skills involved didactic instruction and practice scoring until competency, set at a kappa of 0.90, was established. Interrater reliability with the principal investigator after training yielded kappas of 0.96 and 0.93. These levels compare with previous reports of Assessment of Interpersonal Problem-Solving Skills interrater reliability (29). Psychiatric symptoms, using the 24-item Brief Psychiatric Rating Scale (30), were assessed within 2 weeks before training by an interviewer trained to a minimum intraclass correlation coefficient of 0.80 by the Diagnosis and Psychopathology Unit of the UCLA Clinical Research Center for the Study of Schizophrenia. Following training, participants evaluated the enthusiasm and knowledge of the primary trainer (S.M.) by completing a 10-point Likert scale. Fifty-two of the 60 subjects were available for retest at the 3-month follow-up assessment. Five from the symptom management group and three from the errorless learning group were unavailable.
Errorless Learning
On the basis of previous conceptual models of social problem-solving skills (31, 32), three skill areas were selected as targets for training: 1) identifying the presence/absence of a problem (receiving skills), 2) generating an appropriate solution (processing skills), and 3) effectively enacting the solution (sending skills).
Following traditional errorless learning procedures, errors were minimized during training by beginning on simpler exercises associated with a high likelihood for success and gradually transitioning to more complex ones. Within each skill area, training proceeded in the following way. The trainer provided instruction about the to-be-learned skill, the target behavior or skill was modeled (via the primary trainer or an in-house-developed training videotape), subjects repeatedly practiced performing the skill with the aid of cues or prompts, and then subjects performed the skill with aids removed. The repeated practice of skills was done to automate performance and minimize the occurrence of errors during fading procedures when the cues/prompts were gradually removed. All to-be-learned skills were trained under a rich schedule of social reinforcement. Scenes from the training videotape differed from those on the Assessment of Interpersonal Problem-Solving Skills so that assessment of training outcome required applying learned skills to a set of different social problems (i.e., stimulus generalization). Because of the desire to include scenes that represented problems common to patients and relevant to their daily lives, there was some overlap in broader themes (e.g., problems at doctor’s office). Mastery within each skill area was defined as three in a row correct by all persons in the group. Approximately 2 hours of training were devoted to each skill area.
Receiving skills
Training began with identification of key elements (participants, what they were doing, and where the interaction was taking place) in a variety of social scenes presented on the videotape. First, the primary trainer modeled and then subjects practiced identification of key elements. Training then proceeded to identifying goals and obstacles within each scene and tying these to an operational definition for a social problem (i.e., problem=goal plus obstacle). For example, in a lunchroom scene, a man leaves his seat to get a soda only to find someone sitting in his place when he returns. The goal was identified as getting the seat back; the obstacle being that another person is sitting there. Several scenes with and without social problems were viewed until mastery was established.
Processing skills
For this area, we proposed that many social problems could be resolved using one of three basic solutions: 1) clarifying communication, 2) perspective taking, or 3) seeking help from a higher authority. Clarifying communication involved repeating or more clearly stating the initial request. Perspective taking involved either saying something to convey an understanding of the other person’s perspective or trying to get the other person to understand one’s own perspective. The last solution was to get outside help in those situations when unable to resolve the conflict easily by oneself. The primary trainer explained the types of solutions, providing simple definitions, often as sound bites, to make them easier to understand and remember (e.g., definition for perspective taking=“put self in their shoes”). The primary trainer and actors on the tape modeled solutions to problems. Afterward, subjects practiced selecting and describing the solutions they would use to solve the problems presented on the videotape. Subjects were trained to use all three solutions and to use another solution if the one they initially selected did not solve the problem.
Sending skills
Training for the final skill was divided into verbal and nonverbal components. For the verbal component, the primary trainer modeled and then subjects practiced generating statements based on the three proposed solutions previously learned. Early in training, the task was presented as a sentence completion exercise. Subjects were provided the first few words and then asked to complete the remainder of the sentence. The assistants and primary trainer examined subjects’ written statements and modifications were made if necessary. Subjects then read aloud their written response before the group. During pilot observations, subjects tended to get off track, say inappropriate things, or say too much despite having appropriate responses modeled for them immediately beforehand. The procedures for this study were developed to enhance the amount of structure and thus curb the commission of errors when speaking aloud.
For the nonverbal subcomponent, the primary trainer modeled and subjects practiced the use of appropriate eye contact, body posture, hand gestures, voice volume, prosody, and rate of speech. Pre-scripted neutral phrases were used for training nonverbal behavior (e.g., “The man walked his dog down the street.”). After mastery was established for the verbal and nonverbal components, subjects practiced and established mastery in the use of the two together through a series of role-play exercises based on scenes from the videotape.
Symptom Management
Training procedures for the Symptom Management module of the UCLA Social and Independent Living Skills series (33) followed standard guidelines for implementation of the instructional material. Training activities included didactic and videotape instruction, modeling and social reinforcement, written in-class assignments, and role-play exercises. Training for this module has a strong problem-solving emphasis. Subjects are taught to identify problems associated with the management of their illness and to formulate interpersonal solutions to effectively cope with them. For example, in “Identifying Warning Signs of Relapse,” subjects practice problem-solving a situation in which a relative thinks the subject’s irritability is a warning sign (i.e., precursor to symptom exacerbation), but the subject doesn’t think so. Problem-solving follows a multistep method in which subjects identify and define the problem (receiving skills), generate a list of possible alternatives and weigh the advantages/disadvantages of each (processing skills), and then select the best one and demonstrate it via role-play (sending skills).
Subjects’ Evaluation of Trainer
As differential training effects could be, in part, due to group differences in level of satisfaction with training, this potential confounding variable was measured immediately after training by asking the subjects to complete a 10-point Likert scale (1=extremely negative; 10=extremely positive). Questions about the trainer’s enthusiasm and knowledge of course material were asked. To enhance objectivity, the forms were completed in the primary trainer’s absence.
Data Analyses
Initially, contrasts were conducted on demographic, chronicity, and symptom measures to examine possible group differences at the time of training. Correlational analyses were performed to examine the relationship between symptoms and baseline social problem-solving ability for the two training groups. For the primary analyses, the three dependent measures from the Assessment of Interpersonal Problem-Solving Skills were analyzed separately by using the SAS mixed model procedure with a two-by-two (group [errorless learning versus symptom management] by time [immediately after training versus 3-month follow-up assessment]) repeated-measures analysis of covariance (34). The SAS mixed model procedure uses maximum probability likelihood to estimate the parameters of the analysis of variance and does not require complete cases. The baseline Assessment of Interpersonal Problem-Solving Skills score was entered as a covariate. In addition, entry of positive or negative symptom severity was evaluated as an additional covariate depending on the presence of a significant relationship between symptom severity and baseline Assessment of Interpersonal Problem-Solving Skills performance. Efficacy was assessed by examining group effects, durability by time, and interaction effects. Between-group contrasts were conducted on subjects’ ratings of the primary trainer.
Results
There were no differences between groups on any of the demographic or chronicity measures, and the groups were also comparable in their severity of symptoms as assessed during a 2-week window prior to training (range=1–13 days). No significant correlations were found between positive symptoms and baseline performance for any of the three skills areas of the Assessment of Interpersonal Problem-Solving Skills (all p>0. 50), but there was a significant negative correlation between severity of negative symptoms and baseline processing skills (r=–0.28, df=58, p<0.03) and sending skills (r=–0.36, df=58, p<0.005).
Receiving Skills
A significant effect of training group was revealed (F=5.46, df=1, 54, p<0.03), but there were no time or interaction effects. The errorless learning group showed better overall performance than the symptom management group; performance levels of both groups remained relatively stable over the 3-month follow-up period. Between-group contrasts at the two time points revealed a significant difference in favor of the errorless learning group at the end of training (t=–2.34, df=49, p=0.007) that was weaker and nonsignificant at the 3-month follow-up assessment.
Processing Skills
A significant group effect was revealed (Figure 1), but there were no time or interaction effects. The errorless learning group showed better overall performance than the symptom management group; performance levels of both groups remained relatively stable at the time of the 3-month follow-up assessment. Between-group contrasts at the two time points revealed a significant difference in favor of the errorless learning group at the end of training (t=–2.75, df=49, p=0.008) that remained significant at the 3-month follow-up assessment (t=–2.26, df=49, p<0.03).
Sending Skills
A significant group effect was revealed (F=9.83, df=1, 54, p=0.003). While there was a tendency for time to have an effect (p=0.11), there was no interaction effect. The errorless learning group showed better overall performance than the symptom management group and the performance levels of both groups showed a modest drop at the 3-month follow-up assessment. Between-group contrasts at the two time points revealed a significant difference in favor of the errorless learning group at the end of training (t=–3.83, df=49, p=0.0004) that remained significant at the 3-month follow-up assessment (t=–2.04, df=49, p<0.05).
Trainer Evaluation
The symptom management and errorless learning groups were highly comparable in their high ratings of the primary trainer’s enthusiasm (mean=9.06 [SD=1.46] and 9.34 [SD=1.01], respectively; t=–0.86, df=58, p=0.39) and knowledge of course material (mean=9.35 [SD=1.38] and 9.24 [SD=1.38]; t=0.32, df=58, p=0.75). The vast majority of subjects, regardless of group, perceived the trainer as enthusiastic and knowledgeable.
Discussion
The present study tested the extension of errorless learning to a complex rehabilitation target, social problem-solving skills, in a group of clinically stable schizophrenia and schizoaffective disorder outpatients. Guided by a background developmental literature that defined the strengths and weaknesses of errorless learning, previous applications in schizophrenia have been limited to training on tasks that are relatively simple and free of generalization demands (e.g., entry-level job tasks). Attempts to apply errorless learning to complex functions such as social problem-solving skills have been missing, mainly due to practical concerns (e.g., length of training time, tediousness of procedures) and a low expectation for success. In this study, these challenges were met by 1) focusing training on three functions central to social problem-solving skills, 2) simplifying and reducing the number of solutions, and 3) designing training so that skills learned could be easily applied to different social situations. The results showed that errorless learning training yielded improvement in all three skill areas (receiving, processing, and sending), and the gains were maintained up to 3 months later without further intervention.
It is important to note that the study’s main finding is that errorless learning can be applied to complex behaviors. No claims can be made on the basis of these data about the superiority of errorless learning over other training methods for this particular skill. For this initial exploration of errorless learning, we opted to include a comparison training condition that would serve as a reasonable control for general training effects and one that would mirror the types of functions targeted for training in the errorless learning condition. Training in the symptom management module addresses receiving, processing, and sending skills involved in patients’ abilities to solve problems related to the management of their illness. Although many of the problems require interpersonal solutions, this module was not selected to be a competitive training intervention. As a logical first step in testing the extension of errorless learning in schizophrenia patient rehabilitation, we thought it necessary to test the feasibility of the application prior to testing errorless learning against other competitive training methods specifically designed for social problem-solving skills.
On the basis of our experience with errorless learning, it is helpful to consider the types of cognitive processing difficulties common to persons with schizophrenia when designing training procedures. Initially, procedures are piloted to determine closeness to an “errorless” training experience for subjects. Piloting also reveals which processing difficulties patients typically experience and clarifies which procedures require adjustment. For example, for training of processing skills we avoided asking subjects to generate multiple alternative solutions and weigh their advantages and disadvantages, a common problem-solving approach in the social skills training modules. Patients have difficulties with this method when problems are complex or involve numerous solution alternatives. This may be due to the putative burden placed on working memory and executive processes. Instead, for the purpose of this study we generated three basic solutions for patients to use that could be applied to a wide variety of social problems. This approach reduced the amount of information to be held on-line and lessened the burden on cognitive resources to filter relevant from irrelevant information and weigh the relative value of multiple solution alternatives.
The mechanism by which errorless learning works is not fully understood. Previously, we proposed that errorless learning compensates for neurocognitive deficits in schizophrenia by reducing the demands on explicit memory and simultaneously increasing the demands on implicit memory. The emphasis on automating stimulus-response connections in errorless learning suggests prominent involvement of implicit memory processes. However, at this point there is little empirical evidence to support this proposal (35). Data from a previous study in our lab support the idea that errorless learning reduces demands on explicit memory in learning entry-level job tasks (36), but there is little evidence that errorless learning increases involvement of implicit memory.
The second study hypothesis concerning durability of training effects was largely supported. There were no time or interaction effects that would indicate a significant drop in performance for the errorless learning group, and for two of the three skill areas the group effect favoring errorless learning was maintained at the 3-month follow-up assessment. The automation of learned skills, which minimizes the commission of posttraining mistakes and the need to self-correct, may be a key factor in maintaining stable levels of performance over time. These findings are similar to those found in an earlier study of errorless learning with the Wisconsin Card Sorting Test (37) in which there were no statistically significant drops in performance 4 weeks after training.
The present study attempted to address a number of methodological problems common to interpretation of intervention effects at this stage of testing. To address potential confounds of gender and level of memory impairment, subjects were stratified by these variables before being randomly assigned to a group. Both groups were run in small group format with six to eight subjects, one primary trainer (S.M.), and two assistants. Both groups received 6 hours total training time, split over 2 days. The material covered in both groups was taught using the same instructional tools (e.g., role-play exercises, viewing of videotapes, etc.). To address the possibility that the trainer was more engaging and enthusiastic in the errorless learning group, subjects in both groups evaluated the primary trainer immediately after training. Finally, to guard against rater bias in scoring of the study’s primary outcome measure, all Assessment of Interpersonal Problem-Solving Skills records were scored by two raters blind to group assignment and order of test administration.
In conclusion, the findings support the extension of errorless learning to more complex rehabilitation targets. Given these results, the logical next step would be to test errorless learning versus a competitive training approach specifically designed for social problem-solving skills. In keeping with the translational trajectory of this program of research, we hope to be able to extend applications of errorless learning from simple, discrete work tasks to more complex rehabilitation targets and ultimately move from the tightly controlled atmosphere of the laboratory to community mental health and vocational rehabilitation settings. The vision is to extend errorless learning applications to a wide range of skills and then examine whether change on these component skills leads to changes in broader aspects of work functioning, social functioning, and quality of life. Although few psychiatric rehabilitation programs currently use errorless learning or other compensatory approaches, these findings support continued testing of the approach in schizophrenia.
 |
Presented in part at the 42nd annual meeting of the American College of Neuropsychopharmacology, San Juan, Puerto Rico, Dec. 7–11, 2003. Received Feb. 17, 2004; revision received April 28, 2004; accepted May 17, 2004. From the Department of Psychiatry and Biobehavioral Sciences, UCLA Neuropsychiatric Institute and Hospital, Los Angeles; the Department of Veterans Affairs VISN 22 Mental Illness Research Education and Clinical Center; and the San Fernando Mental Health Center, Mission Hills, Calif. Address correspondence and reprint requests to Dr. Kern, VA Greater Los Angeles Healthcare System (MIRECC 210 A), 11301 Wilshire Blvd., Los Angeles, CA 90073; [email protected] (e-mail). This project was supported by a Stanley Medical Research Institute grant. In-kind support was provided by the UCLA Clinical Research Center for the Study of Schizophrenia (R.P. Liberman, principal investigator), the Department of Veterans Affairs VISN 22 Mental Illness Research Education and Clinical Center, and the San Fernando Mental Health Center. The authors thank Stacy Belkonen, Anita Herrera, M.S., Jay Pope, M.A., Scott Symington, M.A., and Katie Kogler for their collective efforts in training and data collection. The authors also thank Sun Hwang, M.S., for data analyses, the patients and staff of the San Fernando and VA Greater Los Angeles Healthcare Centers for their participation and support, and the Media Department at Pasadena Community College for editing the training videotape.
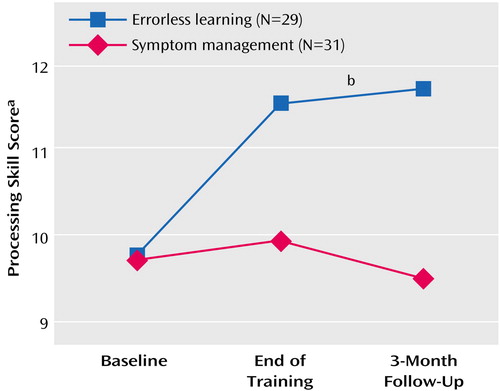
Figure 1. Processing Skill Scores Over Time Among Clinically Stable Schizophrenia Patients Randomly Assigned to a Symptom Management or Errorless Learning Training Program to Address Deficits in Social Problem-Solving Skills
aMeasure of subject’s ability to generate an appropriate solution to a problematic social situation, presented as part of the Assessment of Interpersonal Problem-Solving Skills.
bSignificant group effect (F=8.13, df=1, 54, p=0.006).
1. Green MF, Kern RS, Braff DL, Mintz J: Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the “right stuff”? Schizophr Bull 2000; 26:119–136Crossref, Medline, Google Scholar
2. Velligan DI, Bow-Thomas CC, Huntzinger C, Ritch J, Ledbetter N, Prihoda TJ, Miller AL: Randomized controlled trial of the use of compensatory strategies to enhance adaptive functioning in outpatients with schizophrenia. Am J Psychiatry 2000; 157:1317–1323Link, Google Scholar
3. Terrace HS: Errorless transfer of a discrimination across two continua. J Exp Anal Behav 1963; 6:223–232Crossref, Medline, Google Scholar
4. Ducharme JM, Lucas H, Pontes E: Errorless embedding in the reduction of severe maladaptive behavior during interactive and learning tasks. Behav Ther 1994; 25:489–501Crossref, Google Scholar
5. Lancioni GE, Smeets PM: Procedures and parameters of errorless discrimination training with developmentally impaired individuals. Int Rev Res Ment Retard 1986; 14:135–164Crossref, Google Scholar
6. Tailby R, Haslam C: An investigation of errorless learning in memory-impaired patients: improving the technique and clarifying theory. Neuropsychologia 2003; 41:1230–1240Crossref, Medline, Google Scholar
7. Evans JJ, Wilson BA, Schuwi U, Andrade J, Baddeley A, Bruna O, Canavan T, Della Sala S, Green R, Laaksonen R, Lorenzi L, Taussik I: A comparison of “errorless” and “trial-and-error” learning methods for teaching individuals with acquired memory deficits. Neuropsychological Rehabilitation 2000; 10:67–101Crossref, Google Scholar
8. O’Carroll RE, Russell HH, Lawrie SM, Johnstone EC: Errorless learning and the cognitive rehabilitation of memory-impaired schizophrenic patients. Psychol Med 1999; 29:105–112Crossref, Medline, Google Scholar
9. Kern RS, Liberman RP, Kopelowicz A, Mintz J, Green MF: Applications of errorless learning or improving work performance in persons with schizophrenia. Am J Psychiatry 2002; 159:1921–1926Link, Google Scholar
10. Saykin AJ, Gur RC, Gur RE, Mozley PD, Mozley LH, Resnick SM, Kester DB, Stafiniak P: Neuropsychological function in schizophrenia: selective impairment in memory and learning. Arch Gen Psychiatry 1991; 48:618–624Crossref, Medline, Google Scholar
11. Heinrichs RW, Zakzanis KK: Neurocognitive deficit in schizophrenia: a quantitative review of the evidence. Neuropsychology 1998; 12:426–445Crossref, Medline, Google Scholar
12. Aleman A, Hijman R, de Haan EHF, Kahn RS: Memory impairment in schizophrenia: a meta-analysis. Am J Psychiatry 1999; 156:1358–1366Abstract, Google Scholar
13. Gold JM, Rehkemper G, Binks SW III, Carpenter CJ, Fleming K, Goldberg TE, Weinberger DR: Learning and forgetting in schizophrenia. J Abnorm Psychol 2000; 109:534–538Crossref, Medline, Google Scholar
14. Heaton R, Paulsen JS, McAdams LA, Kuck J, Zisook S, Braff D, Harris MJ, Jeste DV: Neuropsychological deficits in schizophrenics. Arch Gen Psychiatry 1994; 51:469–476Crossref, Medline, Google Scholar
15. Paulsen JS, Heaton RK, Sadek JR, Perry W, Delis DC, Braff D, Kuck J, Zisook S, Jeste DV: The nature of learning and memory impairments in schizophrenia. J Int Neuropsychol Soc 1995; 1:88–99Crossref, Medline, Google Scholar
16. Goldberg TE, Weinberger DR, Berman KF, Pliskin NH, Podd MH: Further evidence for dementia of the prefrontal type in schizophrenia? a controlled study of teaching the Wisconsin Card Sorting Test. Arch Gen Psychiatry 1987; 44:1008–1014Crossref, Medline, Google Scholar
17. Weinberger DR, Aloia MS, Goldberg TE, Berman KF: The frontal lobes and schizophrenia. J Neuropsychiatry 1994; 6:419–427Crossref, Medline, Google Scholar
18. Bell M, Gryson G, Greig T, Corcoran C, Wexler BE: Neurocognitive enhancement therapy with work therapy: effects on neuropsychological test performance. Arch Gen Psychiatry 2001; 58:763–768Crossref, Medline, Google Scholar
19. Medalia A, Revheim H, Casey M: Remediation of memory disorders in schizophrenia. Psychol Med 2003; 30:1451–1459Crossref, Google Scholar
20. Silverstein SM, Pierce DL, Saytes M, Hems L, Schenkel L, Streaker N: Behavioral treatment of attentional dysfunction in chronic, treatment-refractory schizophrenia. Psychiatr Q 1998; 69:95–105Crossref, Medline, Google Scholar
21. Jones RSP, Eayrs CB: The use of errorless learning procedures in teaching people with a learning disability: a critical review. Ment Handicap Res 1992; 5:204–212Crossref, Google Scholar
22. First MB, Spitzer RL, Gibbon M, Williams JBW: Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition (SCID-P), version 2. New York, New York State Psychiatric Institute, Biometrics Research, 1996Google Scholar
23. Addington J, Addington D: Neurocognitive and social functioning in schizophrenia. Schizophr Bull 1999; 25:173–182Crossref, Medline, Google Scholar
24. Mueser KT, Bellack AS, Morrison RL, Wade JH: Gender, social competence, and symptomatology in schizophrenia: a longitudinal analysis. J Abnorm Psychol 1990; 99:138–147Crossref, Medline, Google Scholar
25. Delis DC, Kramer JH, Kaplan E, Ober BA: California Verbal Learning Test Manual. San Antonio, Tex, Psychological Corp, 1987Google Scholar
26. Kern RS, Green MF, Mintz J, Liberman RP: Does “errorless learning” compensate for neurocognitive impairments in the work rehabilitation of schizophrenia patients? Psychol Med 2003; 33:433–442Crossref, Medline, Google Scholar
27. Donahoe CP, Carter MJ, Bloem WD, Hirsch GL, Laasi N, Wallace CJ: Assessment of interpersonal problem-solving skills. Psychiatry 1990; 53:329–339Crossref, Medline, Google Scholar
28. Bowen L, Wallace CJ, Glynn SM, Nuechterlein KH, Lutzker JR, Kuehnel TG: Schizophrenic individuals cognitive functioning and performance in interpersonal interactions and skills training research. J Psychiatr Res 1994; 28:289–301Crossref, Medline, Google Scholar
29. Toomey R, Wallace CJ, Corrigan PW, Schuldberg D, Green MF: Social processing correlates of nonverbal social perception in schizophrenia. Psychiatry 1997; 60:292–300Crossref, Medline, Google Scholar
30. Lukoff D, Nuechterlein K, Ventura J: Manual for the Expanded Brief Psychiatric Rating Scale. Schizophr Bull 1986; 12:594–602Google Scholar
31. Bellack AS, Sayers M, Mueser KT, Bennett M: An evaluation of social problem solving in schizophrenia. J Abnorm Psychol 1994; 103:371–378Crossref, Medline, Google Scholar
32. Mueser KT, Bellack AS: Social skills and social functioning, in Handbook of Social Functioning in Schizophrenia. Edited by Mueser KT, Tarrier N. Boston, Allyn & Bacon, 1998, pp 79–96Google Scholar
33. Liberman RP, Wallace CJ, Blackwell G, Eckman TA, Vaccaro JV, Kuehnel TG: Innovations in skills training for the seriously mentally ill: the UCLA Social and Independent Living Skills Modules. Innovations & Research 1993; 2:43–60Google Scholar
34. SAS Version 6.12. Cary, NC, SAS Institute, 1990Google Scholar
35. Hunkin NM, Squires EJ, Parkin AJ, Tidy JA: Are the benefits of errorless learning dependent on implicit memory? Neuropsychologia 1998; 36:25–36Crossref, Medline, Google Scholar
36. Sergi MJ, Kern RS, Mintz J, Green MF: How useful are learning potential assessments in predicting rehabilitation outcome in schizophrenia? Schizophr Bull (in press)Google Scholar
37. Kern RS, Wallace CJ, Hellman SG, Womack L, Green MF: A training procedure for remediating WCST deficits in chronic psychotic patients: an adaption of errorless learning principles. J Psychiatr Res 1996; 30:283–294Crossref, Medline, Google Scholar



