Posttraumatic Stress Disorder and Health-Related Quality of Life in Long-Term Survivors of Acute Respiratory Distress Syndrome
Abstract
OBJECTIVE: Intensive care often means exposure to physical and psychological stress, with long-lasting emotional sequelae for most patients. Psychiatric morbidity and negative effects on health-related quality of life were assessed in long-term survivors of acute respiratory distress syndrome. METHOD: Forty-six long-term survivors were enrolled in a psychiatric follow-up study. All patients had received standard, protocol-driven treatment during intensive care. The median follow-up time was 8 years after treatment. DSM-IV was used for psychiatric diagnosis. Psychological tests were performed to measure posttraumatic stress symptoms; depression; state anxiety; somatization; symptoms regarding concentration, attention, and short-term memory; social support; and health-related quality of life. RESULTS: At time of discharge, 20 of the patients suffered from posttraumaatic stress disorder (PTSD) and four from sub-PTSD. At follow-up, 11 patients continued to suffer from PTSD and eight from sub-PTSD. The patients with PTSD demonstrated a pronounced tendency for somatization and state anxiety. Among the groups with PTSD, sub-PTSD, and no PTSD, there were no statistically significant differences regarding social support and symptoms of cognitive dysfunction. Those with PTSD showed major impairments in some dimensions of health-related quality of life, whereas those without PTSD had scores that were in the range of the general population. Except for duration of stay on the intensive care unit, neither age, gender, sociodemographic variables, premorbid psychopathology, nor initial severity of illness discriminated between the groups. CONCLUSIONS: Long-term survivors of acute respiratory distress syndrome seem to face a major risk of PTSD and major impairments in health-related quality of life in the long term.
Intensive care treatment exposes patients to enormous stresses. These result from a life-threatening physical situation on one hand and from necessary intensive medical procedures on the other (1). To date, there are relatively few findings available about the psychological long-term effects and later health-related quality of life of former intensive care patients.
From an etiological point of view, patients with acute respiratory distress syndrome form a heterogeneous group. Acute respiratory distress syndrome can result from various disorders (e.g., trauma, pneumonia, sepsis) (2). The threat to the normal matter-of-factness of breathing, dependency on supportive apparatus, and the enormously impaired ability to communicate during intubation are central aspects of these patients’ frightening experiences.
In the first retrospective study (median follow-up time after intensive care treatment=6 years, range=1–10 years), survivors of acute respiratory distress syndrome showed an increased rate of posttraumatic stress symptoms detected by a self-questionnaire in comparison to several comparison groups (acute respiratory distress syndrome, 27.5%; surgery, 11.9%; United Nations soldiers from Cambodia, 1.3%) (3). The patients with acute respiratory distress syndrome and posttraumatic symptoms had pronounced impairments in psychosocial dimensions of health-related quality of life (3).
The current study aimed to establish the presence of posttraumatic stress disorder (PTSD) with the Structured Clinical Interview for DSM-IV (SCID) and to search for an association regarding PTSD diagnostic status with other psychopathologically relevant and psychosocial dimensions.
Method
Subjects
Forty-six patients (22 women and 24 men) were enrolled in a psychiatric follow-up study. All patients had suffered from acute respiratory distress syndrome for various medical reasons and had been treated according to a standardized treatment protocol in the intensive care unit of the Department of Anesthesiology at Grosshadern University Hospital (1985–1995). Acute respiratory distress syndrome was defined according to the criteria of the American-European Consensus Conference on acute respiratory distress syndrome (4). All 46 patients had already participated in the first retrospective study (3).
The 80 patients in the original study group included 92% of all eligible long-term survivors of acute respiratory distress syndrome during the treatment period (3). Reasons for nonparticipation at the follow-up were that the subjects were no longer traceable (N=17), they had died in the meantime (N=2), they were too somatically ill (N=5), they refused to participate (N=4), or no complete data set was available (N=6). There was no significant difference between the participating and nonparticipating patients regarding their intensive care baseline data (Table 1). The median follow-up time of this follow-up study was 8 years after the intensive care treatment (range=3–13 years).
All patients were examined by two experienced psychiatrists who had no knowledge about the medical baseline data or the scores obtained in the self-questionnaires about posttraumatic stress symptoms (with the Posttraumatic Stress Syndrome 10-Questions Inventory) during the first retrospective study. Clinical assessment with the SCID was made after the patients had completed psychological testing and the various self-rating scales were administered by a graduate medical student. The observer-rated Montgomery-Åsberg Depression Rating Scale was administered by the psychiatrist after administration of the SCID.
Psychiatric Diagnosis
A structured clinical interview (SCID) was conducted to establish a DSM-IV diagnosis of PTSD for the time before and after acute respiratory distress syndrome. In order to assess any previous exposure to traumatic experiences, the SCID included a question regarding events or items from the patients’ past that would indicate a psychological trauma of clinical or subclinical significance regarding possible symptoms of PTSD (part of the SCID life chart). Further psychiatric evaluation by a psychiatrist and a SCID assessment were performed at the time of discharge from intensive care. Similar assessments were also performed for the time interval between discharge of the patient from the intensive care unit and the initial follow-up study. Further and final assessments were performed between the initial study and the current follow-up study.
While mental disorders other than PTSD were coded only when DSM-IV criteria were met fully, in the case of PTSD, the symptoms were segregated between having complete PTSD and a subthreshold disorder (sub-PTSD). For subthreshold PTSD, two of the three criteria, criterion B (intrusive recollections or thoughts), criterion C (avoidance symptoms), and criterion D (autonomic hyperactivity), had to be fulfilled. Criterion A (trauma) was homogeneously defined as acute respiratory distress syndrome, which included intensive medical care. The temporal criterion E and criterion F regarding a relevant subjective or psychosocial negative effect had to be present for both full-fledged PTSD as well as for subthreshold PTSD.
In order to quantify the interrater agreement between both examiners, 15 randomly selected patients were examined by both psychiatrists with the SCID according to DSM-IV criteria for PTSD. Kappa statistics were calculated (5). There were discrepancies among three patients. Kappa for PTSD was 0.82; for sub-PTSD, it was 0.76.
Assessments
The Posttraumatic Stress Syndrome 10-Questions Inventory (6) is a self-administered questionnaire that measures the current presence of specific PTSD symptoms that approximate those on the DSM-III PTSD symptom list. Patients are required to rate the presence of each symptom during the past 7 days and its severity on a scale from 1 (never) to 7 (always). A total score >35 is associated with a high probability that the diagnostic criteria for PTSD are fulfilled (6). The reliability coefficient (Cronbach’s alpha) for all 10 items on the Posttraumatic Stress Syndrome 10-Questions Inventory was 0.91 in our first study population (3).
The Montgomery-Åsberg Depression Rating Scale (7) is an observer rating scale that records depressive symptoms. Ten depression items are rated between 0 and 6, according to their intensity. A German version is available (8). The interrater reliability is high (7). The median score on the Montgomery-Åsberg Depression Rating Scale for the patients with major depression is 30 (9).
The State-Trait Anxiety Inventory X1 is a self-assessment questionnaire that measures the amount of anxiety in a current situation. It contains 20 anxiety items with an intensity rated between 1 (not at all) and 4 (very). The minimal score is 20; the maximum score 80 (10). A German version is available (11). In contrast to the State-Trait Anxiety Inventory X2, which measures trait anxiety and has a high retest reliability, the retest reliability of the State-Trait Anxiety Inventory X1 is usually lower (r=0.34).
The Screening for Somatoform Disorders (12), by Rief et al., is a self-questionnaire that contains the symptoms of somatization disorder in items 1 to 35, as they are listed in DSM-III-R. Cronbach’s alpha is high (0.87).
The Syndrom-Kurztest (13) registers deficits in cognitive performance. Nine subtests measure symptoms of attention, concentration, and memory. An English version of the Syndrom-Kurztest is available (14). Cronbach’s alpha is high (0.86). The raw values obtained from the nine subtests can be shown as a norm value according to age group. Norm values ≥5 are clinically relevant. The maximum score is 27.
The Self-Assessment Questionnaire on Social Support (15) contains 19 items that measure dimensions of cognitive, emotional, and practical support. A German version is available (16). The items are scaled between 0 (never) and 4 (always), according to a frequency dimension. Greater scores indicate increasingly favorable social support.
The Medical Outcomes Study 36-item Short-Form Health Survey (17) was used to assess health-related quality of life. It is based on eight concepts of health: physical function, physical role function, pain, general health, vitality, social function, emotional function, and mental health. A total score is calculated for the eight dimensions and ranges from 0 to 100, in which higher values indicate a more favorable quality of life. For the purposes of orientation, a Short-Form Health Survey physical sum score and mental sum score can be calculated. Cronbach’s alpha reliability coefficients for the Short-Form Health Survey dimensions lie between 0.85 and 0.99. A validated German version is available (18). For purposes of comparison, standard values for the Short-Form Health Survey can be obtained from an extensive database of volunteers (N=3,000) from the West German population.
Data Analysis
All statistical calculations were performed by using the SPSS statistical package (SPSS, Chicago). Nonparametric tests were used because the majority of psychometric data presented in this study were not normally distributed. Mann-Whitney U test results were calculated to compare two independent groups. Kruskal-Wallis analysis of variance on the ranks test was employed to compare more than two independent groups. When tests of normality failed, Dunn’s method was applied as a post hoc test after analysis of variance on ranks tests for paired comparisons. Differences with a probability value of p<0.01 were considered significant. Discrete variables were compared between the groups with Fisher’s exact test. All values are given as medians and ranges between the 25th and 75th percentiles.
The study was approved by the ethics committee of the medical faculty of Ludwig-Maximilians-University of Munich. The personal data were coded in accordance with German law. After complete description of the study to the patients, written informed consent was obtained.
Results
Psychiatric Diagnosis
Only three patients fulfilled criteria for a mental disorder according to DSM-IV. Two had major depression and one had alcohol abuse before experiencing acute respiratory distress syndrome. Signs of an earlier posttraumatic stress syndrome (e.g., PTSD) could not be determined in any of the patients.
At the time of dismissal from the intensive care unit or hospital, 43.5% of the patients (20 of 46) had PTSD, according to the SCID, and 8.7% (four of 46) had sub-PTSD. At the time of the follow-up evaluation, i.e., an average of 8 years after intensive care, 23.9% (11 of 46) continued to suffer from full-blown PTSD, and 17.4% (eight of 46) had sub-PTSD. None of the patients who had shown posttraumatic symptoms at the time of dismissal developed delayed PTSD.
In the patients with PTSD, psychiatric comorbidity according to the SCID could be determined at follow-up: two with major depression, one with an eating disorder (bulimia), one with alcohol abuse, and 11 with undifferentiated somatoform disorder. In the patients with sub-PTSD (N=4) and without PTSD (N=1), there were five cases of undifferentiated somatoform disorder (Fisher’s exact test: χ2=27.11, df=1, p=0.0003).
Psychological Assessments
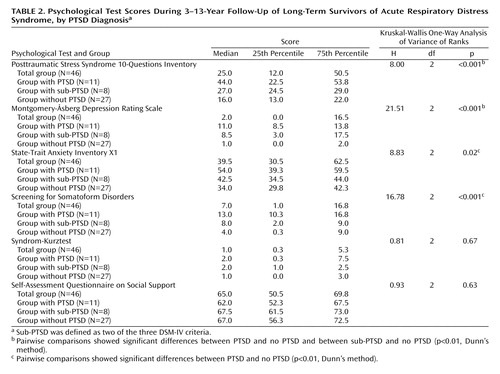
The results of the Posttraumatic Stress Syndrome 10-Questions Inventory self-questionnaire seemed to discriminate well with respect to the diagnostic status of PTSD, according to DSM-IV (Kruskal-Wallis H=18.00, df=2, p<0.001) (Table 2). The scores of both the PTSD group and the sub-PTSD group were significantly different from those of the group without PTSD (p<0.01, Dunn’s method). The average Posttraumatic Stress Syndrome 10-Questions Inventory value of 44.0 in the PTSD group was well above the cutoff score of 35 reported in the literature.
Although the depression scores on the Montgomery-Åsberg Depression Rating Scale demonstrated statistically significant differences among the subgroups (PTSD, sub-PTSD, no PTSD), in terms of clinical relevance, however, they indicated only minor degrees of depressed mood. This was confirmed by the fact that, in addition, only two patients fulfilled the diagnostic criteria for depressive disorder.
There were statistically significant differences between the subgroups in respect to the amount of situational anxiety in the State-Trait Anxiety Inventory X1. The patients with PTSD significantly differed from the patients without PTSD (p<0.01, Dunn’s method). However, it should be noted that none of the patients fulfilled all of the criteria for an anxiety disorder according to DSM-IV.
The patients with a DSM-IV diagnosis of PTSD showed a marked tendency toward somatization. Their average score on the Screening for Somatoform Disorders was in the range that characterizes patients with somatoform disorders, according to the literature. There were significant differences between the groups. Only the pairwise comparison between the group with PTSD and the group without PTSD differed significantly (p<0.01, Dunn’s method).
There were no indications in any of the patient groups for relevant losses in cognitive function as evaluated by psychological tests. The average scores on the Syndrom-Kurztest fell well under the cutoff point of 5. However, four patients (two with PTSD, one with sub-PTSD, one with no PTSD) with respective scores of 7, 9, 11, and 16 demonstrated signs of a mild or moderately severe disturbance of cognitive functions. There were no statistically significant differences among the patient groups with respect to the degree of available social support.
Patients with complete PTSD showed the most serious losses with respect to their health-related quality of life in the following Short-Form Health Survey dimensions (Table 3): general health, social function, and mental health. The scores of the patients without PTSD were within the range for the general population (18). All absolute scores from the patients with sub-PTSD were located near the median. However, only the paired comparison between the groups with PTSD and without PTSD demonstrated statistically significant differences (p<0.01, Dunn’s method).
None of the variables (age, sex, sociodemographic or premorbid psychopathology) discriminated between the subgroups (PTSD, sub-PTSD, or no PTSD). With respect to the severity of the somatic disorder at the start of intensive medical care, neither the Acute Physiology and Chronic Health Evaluation (APACHE II) (4) nor the Lung Injury Score (4) discriminated between the subgroups. The duration of the stay in the intensive care unit correlated significantly with the risk for PTSD (patients with PTSD: median=70 days; patients with sub-PTSD: median=27.5 days; patients with no PTSD: median=27.5 days) (Kruskal-Wallis H=7.37, df=2, p<0.04).
Discussion
In our view, this study represents the first evaluation of long-term survivors of acute respiratory distress syndrome with a structured clinical interview that allows diagnosis according to DSM-IV. At the follow-up evaluation, i.e., a median of 8 years after treatment in the intensive care unit, 23.9% (N=11) of the patients were still suffering from PTSD and 17.4% (N=8) from sub-PTSD. It was remarkable that the symptoms of PTSD could already be determined upon dismissal from the intensive care unit. At this early time point, 43.5% (N=20) of the patients with acute respiratory distress syndrome fulfilled the diagnostic criteria for PTSD and 8.7% (N=4) for sub-PTSD.
In order to properly evaluate the prevalence of PTSD in our group, one must keep in mind that it refers to a group that already had shown signs of increased posttraumatic stress symptoms in a first follow-up study 2 years earlier (3). From an epidemiological perspective, the U.S. National Comorbidity Survey estimated a 7.8% lifetime prevalence of DSM-III-R PTSD (5.0% for men and 10.4% for women) for the U.S. population ages 15–55 years (19). Roughly one-third of the subjects with PTSD did not recover. This rate of chronic PTSD seems to be somewhat comparable to our findings. In a representative community sample of German adolescents and young adults ages 14–24 years, the prevalence rates for PTSD were significantly lower (1% for men and 2.2% for women) (20). Unfortunately, we know of no German epidemiological study that includes an estimation of PTSD rates for the full age range used in the u.s. study.
Posttraumatic symptoms resulting from severe somatic disorders and necessary medical treatment procedures are easily overlooked in the overall treatment plan (21). If one compares the frequency of PTSD symptoms after other severe disorders, such as, e.g., 8.0% and 5.5% for myocardial infarction (22, 23), 32% for cardiac arrest (24), 22% for burns (25), 4% for cancer (26), and 18.8% for a coronary bypass operation (27), a high frequency of PTSD immediately after the illness and a persistent tendency during the further treatment course were conspicuous in our group with acute respiratory distress syndrome.
Psychopathological Dimensions in Assessments
Chronic courses of PTSD are often marked by a high degree of psychiatric comorbidity (28). At follow-up, a further psychiatric disorder in addition to PTSD could be determined by the SCID in four patients, if one put aside the diagnostic category of undifferentiated somatoform disorder.
In psychological assessments, the PTSD subgroup did distinguish itself with significantly higher scores on the psychopathological dimensions of depressive mood (the Montgomery-Åsberg Depression Rating Scale), situational anxiety (the State-Trait Anxiety Inventory X1), and somatization (the Screening for Somatoform Disorders). However, only the greater situational anxiety and increased tendency to somatization appeared to be clinically relevant. The vast majority of the patients with acute respiratory distress syndrome demonstrated good cognitive performance on the Syndrom-Kurztest. This should be regarded as an important result in long-term development when one considers the severity of the somatic disorder and the regularly increased occurrence of critical cerebral complications during the intensive medical care of these patients (29).
Psychosocial Support and Health-Related Quality of Life
During the interim psychosocial adaptation, the various patient subgroups could all receive comparably positive emotional, cognitive, and pragmatic social support (the Self-Assessment Questionnaire on Social Support). With regard to health-related quality of life, on the whole, the results found in the earlier study were replicated (3). The American study from Weinert et al. (30), which was clinically and methodologically comparable to our earlier study, also showed similar findings with respect to the quality of life of patients subsequent to intensive medical treatment of a respiratory disorder. The diagnostic status of PTSD at follow-up was associated with significantly more unfavorable values in the most important psychosocial dimensions of the Short-Form Health Survey. In contrast, there was no statistical association with the dimensions of the Short-Form Health Survey, which depicts physical functioning more closely (physical function, pain).
Possible Risk Variables for PTSD
An analysis of a data set available at the time of intensive medical care showed that neither age, sex, nor sociodemographic variables were significantly different between the patient subgroups. This was also true for possible premorbid psychopathology, as retrospectively assessed by the SCID. In this respect, our overall patient group had to be rated as largely inconspicuous in its premorbid status in comparison to the frequencies of psychiatric disorders found for the general German population (31). Major traumatizing events before the appearance of acute respiratory distress syndrome could not be elicited in any case; only three patients reported on car accidents of a mild to moderate intensity. Nor were there any major traumatic events found during the follow-up period.
The severity of acute respiratory distress syndrome rated with the APACHE II and the Lung Injury Score at the start of intensive medical care also could not discriminate significantly between the subgroups. This may have been the expression of a ceiling effect, however. In comparison to the patients in the study by Weinert et al. (30), our patients with acute respiratory distress syndrome seemed to represent an extremely ill group. This was accompanied by a longer treatment duration in the intensive care unit. The number of days spent in the intensive care unit, again, was significantly associated with PTSD diagnostic status. This finding seems to need more attention in a prospective study design.
The Process of Traumatization
Of course, possible traumatic factors contributing to the pathogenesis of PTSD in patients with acute respiratory distress syndrome can be discussed only tentatively from a retrospective point of view. The initial phase of illness in patients with acute respiratory distress syndrome is characterized by acute respiratory distress with an immediate threat of death by suffocation, initiating extreme organismal stress reactions (32). High doses of exogenous catecholamines are often needed to support circulatory system functions. This may contribute to a further escalation of physiological stress reactions.
Besides the continuous mechanical ventilation of the patient, note that the initial and middle phases of treatment in an intensive care unit require deep analgesic sedation. All of our patients with acute respiratory distress syndrome had Ramsey Sedation Scores corresponding to a condition of general anesthesia (3). This makes subjective experiences of traumatic events improbable, but they cannot be ruled out definitively (33).
In our view, weaning from mechanical ventilation represents a decisive phase for the subjective perception of trauma in patients with acute respiratory distress syndrome. The patient must be at least partially awake and cooperative during this process (34). This means that a certain degree of consciousness appears unavoidable during a stressful stage of treatment of acute respiratory distress syndrome. Besides pharmacology-related withdrawal syndromes (not registered, however, in our study), which can contribute to deliria and conditions of massive anxiety, the main experience for the patient with acute respiratory distress is the threatened respiration without further mechanical support, or a feeling of suffocation. This destructive experience is potentiated by the continued limited ability to communicate and the lack of possibilities to flee.
A close association between anxiety disorders, especially panic disorder, and comorbid respiratory disorders is being discussed widely (35, 36). There are indications for a specific association between panic disorder and a history of traumatic experiences of suffocation (37). According to Klein’s prominent hypothesis (38), panic disorder may be related to a false suffocation alarm due to an abnormally sensitive reactivity of the medullary chemoreceptor system to increasing arterial carbon dioxide. This corresponds exactly to the real pathophysiological conditions during acute respiratory distress syndrome. So far, there are only a few observations about an association between respiratory dysfunction and PTSD (39, 40, 41). This relationship appears to be much more evident in patients with acute respiratory distress syndrome, since the often prolonged duration of this condition is an extreme threat to respiration.
Limitations of the Study
Our study has been conducted retrospectively. The period of observation covers many years since the patients had received intensive care treatment originally. The follow-up rate was only 58%, and a recall bias might also have significantly lowered the reporting of any psychiatric symptoms before and after acute respiratory distress syndrome. Our patient group was not randomly selected and, in addition, involved a patient population that already showed signs of increased posttraumatic stress reaction in a previous study. The observed actual rate of PTSD can be seen only in relative terms. The same caution should be exercised in the interpretation of any possible risk variables. In a retrospective analysis, any observed correlation could be considered of hypothetical importance, only requiring further validation in a controlled prospective study.
Nevertheless, in conclusion, long-term survivors of acute respiratory distress syndrome seem to face a major risk of PTSD and impairments in health-related quality of life.
 |
 |
 |
Received July 20, 1999; revisions received Nov. 20, 2000, June 26, 2001, and April 23, 2003; accepted May 2, 2003. From the Department of Psychiatry, Karl-Franzens-University; and the Department of Anaesthesiology and the Department of Psychiatry, Ludwig-Maximilians-University of Munich, Germany. Address reprint requests to Dr. Kapfhammer, Department of Psychiatry of the Karl-Franzens-University of Graz, Auenbruggerplatz 31, A-8036 Graz, Austria; [email protected] (e-mail). Supported by a grant from the Eli Lilly International Foundation.
1. Shuster JL, Stern TA: Intensive care units, in Textbook of Consultation-Liaison Psychiatry. Edited by Rundell JR, Wise MG. Washington, DC, American Psychiatric Press, 1996, pp 782–802Google Scholar
2. Ware LB, Matthay MA: The acute respiratory distress syndrome. N Engl J Med 2000; 342:1334–1349Crossref, Medline, Google Scholar
3. Schelling G, Stoll C, Haller M, Briegel J, Manert W, Hummel T, Lenhart A, Heyduck M, Polasek J, Meier M, Preuß U, Bullinger M, Schüffel W, Peter K: Health-related quality of life and posttraumatic stress disorder in survivors of the acute respiratory distress syndrome. Crit Care Med 1998; 26:651–659Crossref, Medline, Google Scholar
4. Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, Legall JR, Morris A, Spragg R: The American-European Consensus Conference on acute respiratory distress syndrome: definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med 1994; 149:818–824Crossref, Medline, Google Scholar
5. Altman DG: Practical Statistics for Medical Research. London, Chapman & Hall, 1991Google Scholar
6. Weisaeth L: Torture of a Norwegian ship’s crew: the torture, stress reactions and psychiatric aftereffects. Acta Psychiatr Scand Suppl 1989; 355:63–72Crossref, Medline, Google Scholar
7. Montgomery SA, Åsberg M: A new depression scale designed to be sensitive to change. Br J Psychiatry 1979; 134:382–389Crossref, Medline, Google Scholar
8. Schmidtke A, Fleckenstein P, Moises W, Beckmann H: Untersuchungen zur Reliabilität und Validität einer deutschen Version der Montgomery-Åsberg Depression-Rating Scale (MADRS). Schweiz Arch Neurol Psychiatrie 1988; 139:51–65Medline, Google Scholar
9. Maier W, Philipp M: Comparative analysis of observer depression scales. Acta Psychiatr Scand 1985; 72:239–245Crossref, Medline, Google Scholar
10. Spielberger CD, Gorsuch RL, Lushene RD: STAI Manual. Palo Alto, Calif, Consulting Psychologists Press, 1970Google Scholar
11. Laux L, Glanzmann P, Schaffner P, Spielberger CD: Das State-Trait Angstinventar. Theoretische Grundlagen und Handanweisung. Weinheim, Germany, Beltz, 1981Google Scholar
12. Rief W, Schaefer S, Fichter M: SOMS—ein Screening-Verfahren zur Identifizierung von Personen mit somatoformen Störungen. Diagnostica 1992; 38:228–241Google Scholar
13. Erzigkeit H: SKT: Ein Kurztest zur Erfassung von Gedächtnis- und Aufmerksamkeitsstörungen: Manual. Weinheim, Germany, Beltz 1989Google Scholar
14. Overall JE, Schaltenbrand R: The SKT neuropsychological test battery. J Geriatr Psychiatry Neurol 1992; 5:220–227Crossref, Medline, Google Scholar
15. Donald CA, Ware JE: The measurement of social support. Res Community Ment Health 1984; 4:325–370Google Scholar
16. Kirchberger J, Bullinger M: Der Social Support Fragebogen. Göttingen, Germany, Hogrefe, 2004Google Scholar
17. Ware JE, Snow KK, Kosinski M, Gandek B: SF-36 Health Survey Manual and Interpretation Guide. Boston, Health Institute, 1993Google Scholar
18. Bullinger M, Kirchberger J: SF-36 Fragebogen zum Gesundheitszustand. Göttingen, Germany, Hogrefe, 1998Google Scholar
19. Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB: Post-traumatic stress disorder in the community. Arch Gen Psychiatry 1998; 55:626–632Crossref, Medline, Google Scholar
20. Perkonigg A, Kessler RC, Storz S, Wittchen HU: Traumatic events and post-traumatic stress disorder in the community: prevalence, risk factors and comorbidity. Acta Psychiatr Scand 2000; 101:46–59Crossref, Medline, Google Scholar
21. Mayou RA, Smith KA: Posttraumatic symptoms following medical illness and treatment. J Psychosom Res 1997; 43:121–123Crossref, Medline, Google Scholar
22. Doerfler LA, Pbert L, DeCosimo D: Symptoms of posttraumatic stress disorder following myocardial infarction and coronary bypass surgery. Gen Hosp Psychiatry 1994; 16:193–199Crossref, Medline, Google Scholar
23. Van Driel RC, Op den Velde W: Myocardial infarction and posttraumatic stress disorder. J Trauma Stress 1995; 8:151–159Crossref, Medline, Google Scholar
24. Ladwig K-H, Schoefinius A, Dammann G, Danner R, Gürtler R, Herrmann R: Long-acting psychotraumatic properties of a cardiac arrest experience. Am J Psychiatry 1999; 156:912–919Link, Google Scholar
25. Roca RP, Spence RJ, Munster AM: Posttraumatic adaptation and distress among adult burn survivors. Am J Psychiatry 1992; 149:1234–1238Link, Google Scholar
26. Alter CL, Pelcovitz D, Axelrod A, Goldenberg B, Harris H, Meyers B, Grobois B, Mandel F, Septimus A, Kaplan S: Identification of PTSD in cancer survivors. Psychosomatics 1996; 37:137–143Crossref, Medline, Google Scholar
27. Stoll C, Schelling G, Goetz A, Kilger E, Bayer A, Kapfhammer HP, Rothenhäusler HB, Kreuzer E, Reichert B, Peter K: Health-related quality of life and post-traumatic stress disorder in patients after cardiac surgery and intensive care treatment. J Cardiovasc Thorac Surgery 2000; 120:505–512Crossref, Medline, Google Scholar
28. Deering CG, Glover SG, Ready D, Eddleman HC, Alarcon RD: Unique patterns of comorbidity in post-traumatic stress disorder from different sources of trauma. Compr Psychiatry 1996; 37:336–346Crossref, Medline, Google Scholar
29. Eidelman LA, Putterman D, Putterman C: The spectrum of septic encephalopathy: definitions, etiologies, and mortalities. JAMA 1996; 14:470–473Crossref, Google Scholar
30. Weinert C, Gross CR, Kangas JR, Bury CR, Marinelli WA: Health-related quality of life after acute lung injury. Am J Respir Crit Care Med 1997; 156:1120–1128Crossref, Medline, Google Scholar
31. Fichter MM, Narrow WE, Roper MT, Rehm J, Elton M, Rae DS, Locke BZ, Regier DA: Prevalence of mental illness in Germany and the United States: comparison of the Upper Bavarian Study and the Epidemiologic Catchment Area Program. J Nerv Ment Dis 1996; 184:598–606Crossref, Medline, Google Scholar
32. McEwen BS: Protective and damaging effects of stress mediators. N Engl J Med 1998; 338:171–179Crossref, Medline, Google Scholar
33. Osterman JE, van der Kolk B: Awareness during anaesthesia and posttraumatic stress disorder. Gen Hosp Psychiatry 1998; 20:274–281Crossref, Medline, Google Scholar
34. Weinberger SE, Weiss JW: Weaning from ventilatory support. N Engl J Med 1995; 332:388–389Crossref, Medline, Google Scholar
35. Smoller JW, Simon NM, Pollack MH, Kradin R, Stern T: Anxiety in patients with pulmonary disease: comorbidity and treatment. Semin Clin Neuropsychiatry 1999; 4:84–97Medline, Google Scholar
36. Verburg K, Griez E, Meijer J, Pols H: Respiratory disorders as a possible predisposing factor for panic disorder. J Affect Disord 1995; 33:129–134Crossref, Medline, Google Scholar
37. Bouwer C, Stein DJ: Association of panic disorder with a history of traumatic suffocation. Am J Psychiatry 1997; 154:1566–1570Link, Google Scholar
38. Klein DF: False suffocation alarms, spontaneous panics, and related conditions: an integrated hypothesis. Arch Gen Psychiatry 1993; 50:306–317Crossref, Medline, Google Scholar
39. Gavin LA, Roesler TA: Posttraumatic distress in children and families after intubation. Pediatr Emerg Care 1997; 13:222–224Crossref, Medline, Google Scholar
40. Obhu S, Yamashina A, Takasu N, Yamaguchi T, Murai T, Nakano K, Matsui Y, Mikami R, Sakurai K, Hinohara S: Sarin poisoning on Tokyo subway. South Med J 1997; 90:587–593Crossref, Medline, Google Scholar
41. Youakim JM, Doghramji K, Schutte SL: Posttraumatic stress disorder and obstructive sleep apnea syndrome. Psychosomatics 1998; 39:168–171Crossref, Medline, Google Scholar



