Cigarette Smoking in Relation to Depression: Historical Trends From the Stirling County Study
Abstract
OBJECTIVE: Building on findings about the prevalence and incidence of depression over a 40-year period, the authors provide data on trends in cigarette smoking and associations with depression. METHOD: Data come from interviews with adult population samples (1952, 1970, and 1992) and followed cohorts (1952–1970 and 1970–1992). Logistic regression models and survival regressions were used to analyze the data. RESULTS: The associations between smoking and depression were small and nonsignificant in 1952 and 1970. In 1992, however, the odds that a smoker would be depressed were three times the odds that a nonsmoker would be depressed. The interaction between smoking and study year was significant, indicating that the association was limited to the most recent sample. In the cohort analysis, smoking at baseline did not predict the onset of depression, but subjects who became depressed were more likely to start or continue smoking and less likely to quit than those who never had a depression. CONCLUSIONS: In terms of population trends, the association between depression and cigarette smoking became prominent as the use of tobacco declined because of awareness of the risks involved. The findings about individuals followed over time suggest that those who became depressed were more involved with nicotine than those who never had a depression. The authors discuss hypotheses involving “self-medication,” risk-taking, and changes in the social climate but conclude that the relationships between smoking and depression are probably multiple and complex.
Cigarette smoking became common during the 20th century; many men smoked by the time of World War I, and many women were smoking by World War II (1). The Surgeon General’s 1964 report on lung cancer and smoking was followed by steadily increasing information about the health hazards of smoking (2, 3). General monitoring of time trends and correlates has indicated that more men than women smoke, more younger than older people, and, although overall rates have decreased, the decline is more marked among men than women (4, 5).
By the 1980s, research had begun to show that there was a high rate of cigarette smoking among psychiatric patients (6). Since then, studies using both cross-sectional and follow-up data have examined relationships between smoking and psychiatric disorders, especially depression (7–10).
A common hypothesis (referred to as the “self-medication” hypothesis) focusses on the chemical properties of nicotine and suggests that smoking may reduce dysphoria (11, 12). Another hypothesis suggests that common genetic factors may predispose to both smoking and depression (13, 14). It has also been observed that smoking is among several risk-taking behaviors associated with depression (15, 16).
Where time trends in the association between smoking and psychiatric disorders are concerned, evidence is sparse. One study, for example, has suggested that the association between smoking and nicotine dependence is increasing (17); younger cohorts were found to have a higher ratio of nicotine dependence to smoking than older cohorts. There do not appear to be any reports on historical trends in the associations between smoking and depression, however. In this paper, we investigate such time trends, drawing on evidence from a long-term psychiatric epidemiologic investigation.
Known as the Stirling County Study, the investigation provides a 40-year perspective that makes it possible to observe the associations between depression and smoking over a historical period when use of nicotine increased and then declined. Through repeated cross-sectional surveys, the study gives information about population trends in the prevalence of both smoking and depression as well as trends in their association. Through cohort follow-up investigations, the Stirling County Study provides data on trends exhibited by individuals in terms of initiation, cessation, and continuation of smoking and how these patterns relate to depression.
Method
Site
Data have been gathered in a county in Atlantic Canada with a population of about 20,000 (18, 19). The site was typically rural at the beginning of the study, but major changes have occurred. Service and information industries have burgeoned; women have become a large part of the labor force; educational levels have increased; the media has exerted strong influence; racial tension has increased; and use of drugs and criminal activity have increased. Decreases have occurred in religious activity, marital stability, and family size. Thus, the area exhibits most of the social trends that characterize North American society generally (20–22).
To assess the degree to which psychiatric findings about this population are similar or different from those of other areas, the depression portions of the National Institute of Mental Health Diagnostic Interview Schedule (23) were included in the interviews carried out in the most recent wave of data gathering. The 1-month prevalence of major depressive episodes was 2.6% (21), which is similar to the 2.2% found in the Epidemiologic Catchment Area (ECA) program (24, 25) and the 2.3% found in the Edmonton Psychiatric Epidemiology Study (26). The lifetime rates were also comparable: 7.9% in Stirling County (21), 6.3% in the ECA program (24, 25), and 8.6% in Edmonton (26). Thus, where depression is concerned, the population of Stirling County is like many other populations in North America.
Study Design, Completeness, Interview Procedures
Data for this report derive from three adult population samples selected in 1952, 1970, and 1992 as well as from survivors of the 1952 sample who were reinterviewed in the 1970 survey period (cohort 1) and survivors of the 1970 sample reinterviewed in the 1992 survey period (cohort 2) (Table 1). Completion rates from both types of investigations ranged from 82% to 92%. Sampling procedures, concerned with adequate representation of the demographic profile of the county, have been described in detail elsewhere (20–22).
Subjects were visited in their homes by trained interviewers. The purpose of the study and the nature of the interview were explained verbally, and a written description of the study along with the director’s name and her telephone number was provided when a subject expressed willingness to be interviewed. These procedures have been approved by the Human Research Committee of the Massachusetts General Hospital and by other committees concerned with the ethical protection of human subjects in both the United States and Canada.
Cigarette Smoking
Smoking habits were assessed by two questions. The first, “Do you smoke? Would you say ‘a lot,’ ‘some,’ or ‘not at all’?” was followed by a question about the amount and kind of smoking as “more than 20 cigarettes per day,” “20 or fewer cigarettes,” or “only cigars or pipes.” This study excludes cigars and pipes, and the two levels of daily cigarette smoking are labeled as “heavy” and “moderate.”
In the two earlier samples, among the people who smoked more than 20 cigarettes a day, most (92% in 1952 and 93% in 1970) indicated that they smoked a lot. In 1992, the proportion had dropped to 80%. Nevertheless, the division between heavy and moderate smoking seemed to be meaningful to most smokers.
The information about cigarette smoking is limited to customary daily use at the time of interview. It does not include past history, and subjects were not asked for dates of smoking onset and/or cessation.
Depression
The identification of depression involved the application of procedures called DPAX, where the DP stands for depression and the AX for anxiety (27, 28). In this article, we deal only with depression and build on reports about its prevalence and incidence over the 40-year period (21, 29). The DPAX procedures are implemented by computerized algorithms, and the definition of depression involves dysphoric mood as the essential feature; disturbances of sleep, appetite, and energy as associated symptoms; a duration of at least 1 month; and impairment in everyday functioning. Chronic and acute forms are not differentiated, and thus the definition can be regarded as similar to a combination of major depressive episode and dysthymia.
Over the years of the study, the vernacular for describing depressed mood has changed. The idiom of “being in poor spirits” was commonly used at the beginning of the study but declined in frequency. Idioms such as “feeling low and hopeless” and “wondering if anything is worthwhile” became more customary. The methods used for time trends have been adjusted for sensitivity to such changes (21, 28).
The DPAX findings indicated that the current prevalence of depression in each year of study was about 5% (Table 1). In 1992 a change in distribution was observed, occasioned by the fact that women younger than 45 years exhibited a twofold increase that was counterbalanced by small diminutions among older men and women (21). The incidence of depression remained stable at approximately 4 per 1,000 (29).
Statistical Methods
Analysis of cross-sectional time trends used multivariate logistic regression in SAS PROC GENMOD (30). For assessing trends in smoking, three analyses were conducted: the prevalence of heavy smoking, the prevalence of moderate smoking, and the prevalence of both levels combined. In each, the comparison group was subjects who did not smoke. Three predictor variables were used: age (<45 and ≥45), gender, and study year.
For analysis of trends in the relationships between smoking and depression, current depression was the outcome variable and four predictor variables were used: age, gender, study year (1952, 1970, and 1992), and current daily smoking (no cigarette smoking, moderate smoking, and heavy smoking).
Because we were especially interested in time trends, the main model tested included the interaction of smoking and study year. In addition, models were fitted that included all other pairwise interactions. To investigate possible higher-order interactions, the analysis was repeated, stratified by gender and then stratified by age.
Results of the logistic regression models are presented in terms of odds ratios with 95% confidence intervals. The odds ratios were adjusted so that, in each year of study, the reference category consisted of depressed nonsmokers.
Where the cohorts were concerned, standard life-table methods were used to calculate incidence rates for depression among subjects who were at risk for a first-ever depression (29, 31). The effects of age, gender, smoking status at baseline, and cohort interval (1952–1970 compared with 1970–1992) were statistically assessed by using survival regressions implemented in log linear analysis (32). In addition, the incidence of depression was related to the different patterns of tobacco use (continuing to be a nonsmoker as well as starting, continuing, or quitting smoking) over the time interval. Individuals who became depressed were compared with those who never had a depression by using relative risk with 95% confidence intervals.
Results
Our first analysis concerned population smoking trends. Table 2 shows prevalence rates by year, gender, and age. Analysis of all those who smoked (combining both heavy and moderate levels) indicated that the main effects of year, gender, and age as well as the interactions with year and gender and with year and age were all significant at the level of p<0.0001. Smoking increased between 1952 and 1970 and decreased by 1992. Men were significantly more likely to smoke than women, but this difference attenuated over time. Similarly, more younger people smoked than older people, and this difference also reduced over time.
By 1992, moderate smoking had declined among both men and women. This was achieved by a sharp drop between 1970 and 1992 for men while the drop-off among women followed an increase. Men displayed a stable prevalence of heavy smoking at just over 20%, but heavy smoking increased among women (2% in 1952, 4% in 1970, and 11% in 1992). The increase of heavy smoking was somewhat more pronounced for younger women (2% in 1952, 5% in 1970, and 17% in 1992).
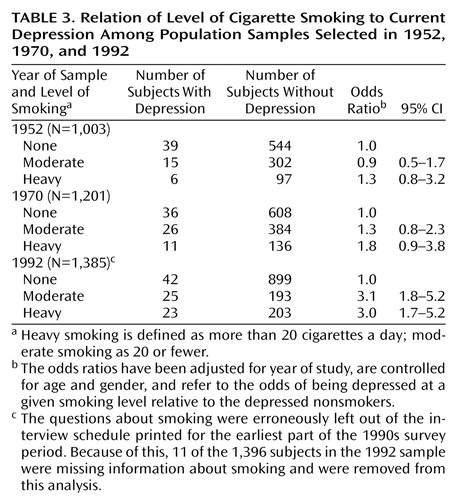
In regard to the associations between depression and smoking in the three samples, logistic regression indicated that smoking and study year exhibited a significant interaction (χ2=10.2, df=4, p=0.04). The other pairwise interactions were not significant and were not used in the estimation of odds ratios. In 1952 and 1970, the associations between depression and smoking were not significant, but in 1992 they were strong and significant. Table 3 shows that in the most recent sample the odds that a smoker would be depressed were three times the odds that a nonsmoker would be depressed. When stratified by age, the results were similar. When stratified by gender, the analysis suggested that the association had been present in 1970 for men but not at so strong a level as in 1992.
For individuals followed over time, we investigated the general patterns of change and stability in smoking. Because smoking was more common among younger subjects and because the prevalence of smoking declined after 1970, many subjects who were smoking at the beginning of the intervals were not smoking at the end. Such cessation increased over time (33% of the smokers in cohort 1 and 54% of the smokers in cohort 2 quit). Concomitantly, only a few of these adults started smoking, and this proportion decreased over time from 10% in cohort 1 to 4% in cohort 2. The patterns of starting and stopping tended to be similar for men and women, but older people were more likely to quit and less likely to start than younger people.
With regard to studying whether depression preceded smoking as might be disclosed by following individuals, we were unable to test whether depression at baseline predicted subsequent initiation of smoking. This was because smoking was so common in 1952 and 1970 that the cohorts were nearly halved when limited to those at risk and because so few adults started smoking that in cohort 1 there were only two depressed subjects who later became smokers and in cohort 2 none did so.
With regard to studying whether smoking preceded depression, we found that smoking at baseline was not related to the subsequent incidence of depression. In cohort 1 the average annual incidence of depression among smokers was 4.5 per 1,000; among nonsmokers it was 4.6 per 1,000. In cohort 2, comparable figures were 3.8 and 3.5.
Given the historical trend toward smoking cessation, it was possible that some of the subjects who became depressed had already quit smoking before the onset of depression. This possibility led us to use information about all types of changes and continuities in smoking practices. We found that subjects who became depressed were more likely to begin or continue smoking and less likely to quit than those who never became depressed (Table 4). Although the associations were modest, the same general pattern pertained in both cohorts. In cohort 2, subjects who became depressed were nearly four times more likely to start smoking at some point in the interval than those who were never depressed.
Discussion
This investigation began when cigarette smoking was very common and increasing, and it extended through the period when tobacco use was declining. The samples of 1952 and 1970 were studied before evidence began to appear in the psychiatric literature indicating an association between having a psychiatric disorder and using nicotine. The main finding from this study is that a significant association between depression and smoking did not appear until 1992, when the most recent sample was selected.
It was only when smoking was becoming nonnormative that a strong and positive association with depression appeared. Studies of other forms of substance use and abuse have suggested that there may be a relationship between the commonness of use and the degree to which it is associated with deviance or psychopathology (33, 34). For example, fewer drug use problems seem to occur in inner cities where heroin is commonly used, and more alcohol use problems may be found in cultural areas where abstemiousness is the norm (33). Although such illustrations point up cross-sectional differences by geographic locales, there is also some evidence about changing relationships over time. For example, as cocaine use has become more widespread its association with affective disorder appears to have declined (34). Where tobacco use is concerned, our finding about the emergence of a strong association with depression when cigarette smoking was becoming less prevalent can be compared to evidence of a stronger relationship between smoking and the psychopathology of nicotine dependence in recent than in early birth cohorts (17).
Following cohorts of individuals over time is a useful way to investigate whether depression tends to precede smoking or smoking to precede depression. Our analysis of “depression first and smoking later” was hampered by the fact that quitting was much more common than starting to smoke. Where “smoking first and depression later” was concerned, our evidence was negative. Given the trend toward cessation, however, it is possible that subjects who became depressed had already quit smoking.
Given these factors, our main finding about what happened over time among individuals comes from using all patterns of smoking change and continuity. This finding indicates that subjects who became depressed were more likely to continue smoking, to initiate smoking, and not to quit than those who never became depressed. The finding also suggests that subjects who became depressed were more involved with nicotine than those who were never depressed.
The Stirling County Study has several strengths for addressing the topic of this report. Among them are time-depth and the combination of repeated cross-sectional surveys with cohort follow-up of individuals. In addition, the definition of depression is explicit and quite congruent with contemporary criteria. The measurement of time trends in depression has benefited from attention to consistency of methods while making adjustments for changes in the vernacular for expressing depressed mood.
A limitation is that the Stirling County Study concerns adults, but there is strong evidence that smoking begins among adolescents and that trends among them differ from the trends for adults (35). There are also several features of smoking practices that it would have been useful to explore through each individual’s history, but the data are limited to behavior at the time of interview.
It is very likely that the general decline in smoking prevalence was related to the markedly increased public awareness of health hazards of smoking. Given the numerous warnings and prohibitions on smoking that have come into effect, it is probable that everyone was aware of the dangers by the 1990s. Because of this, the knowledge about the risks needs to be considered in interpreting the findings.
If the self-medication hypothesis is correct, it is plausible that the positive effect of nicotine in diminishing dysphoric feelings might have been so strong that depressed subjects would smoke in spite of knowledge about the negative effects. They would resist quitting and would be more likely to start or continue to use tobacco. Support for the self-medication hypothesis would be strengthened if a dose response were found. Although not clear-cut, our findings are not inconsistent with such a response; it was suggested in 1970 when the association was beginning to be observed, especially among men. Further, although the odds for moderate and heavy smoking were similar in 1992, they had quite wide confidence intervals.
Another possible mechanism relates to the fact that depression may incline its sufferers to take risks of many kinds because they feel that life is not worthwhile. Thus, awareness of the risks associated with smoking may not have reduced the incentive to smoke. It is notable that some other recent studies have indicated that depression is associated with many risky behaviors, including use of chemical substances and poor attention to health care (15, 16).
The hypotheses about self-medication and risk-taking flow from the view that depression leads to smoking rather than that smoking leads to depression. In this study, we found no positive association between previous smoking and subsequent depression. Further, the evidence that subjects who became depressed were more involved with tobacco than those who had never been depressed seems to give greater weight to the view that there is something about depression inclining its sufferers to use tobacco than that there is something about smoking engendering depression.
It would seem unwise, nevertheless, to rule out the possibility that smoking might be among the antecedent factors associated with the development of depression. One reason for caution is that both depression and heavy smoking were found to have increased among younger women in the 1992 sample. Other studies have also pointed to increasing rates of depression and have suggested that the increase seems to have appeared among subjects born after World War II (36, 37). All of the younger women in our 1992 sample had been born after that war (21).
The fact that both heavy smoking and depression increased among this particular segment of the population raises questions about whether the social changes that have particularly affected women over the last half of the 20th century are relevant to the increase in depression. Over this period, acceptability for women to smoke went along with acceptability to work outside of the home, to use the pill, to drink, to divorce, and to compete with men in many spheres. The consequences of these changes were probably variable: some were advantageous and others created a climate that may have put larger numbers of women at risk for depression.
The smoking trends among men were different from those among women, and the association with depression started earlier for men. The fact that the associations between depression and smoking were general in 1992 rather than being limited to a particular segment of the population suggests that the relationships may be multifaceted and not easily reducible to just one or two main factors.
The portions of the Stirling County Study following individuals through time have thus far indicated that depression is an extremely grave disorder, carrying a risk of chronicity, progressive disability, and premature death (38, 39). The adverse consequences of nicotine use are well-known. Compared with other drugs, cigarettes are the most persistently used (40). When depression and smoking coexist, the quality and quantity of life are doubly assaulted.
 |
 |
 |
 |
Received July 31, 2002; revision received Feb. 4, 2003; accepted Feb. 22, 2003. From the Department of Psychiatry, Massachusetts General Hospital, Harvard Medical School; the Department of Mathematics, Smith College; and the Department of Biostatistics and the Department of Epidemiology, Harvard School of Public Health, Boston. Address reprint requests to Dr. Murphy, Massachusetts General Hospital, Department of Psychiatry, Rm. 10028, 149 13th St., Charlestown, MA 02129-2000; [email protected] (e-mail). Supported by NIMH grant MH-39576 (Dr. Murphy). The authors thank Patricia Merritt, Ellen Krystofik, and Barbara Burns for field management and data processing and Barbara Burns for literature review.
1. Walsh DC, Sorenson G, Leonard L: Gender, health and cigarette smoking, in Society and Health. Edited by Amick BC, Levine S, Tarlov A. New York, Oxford University Press, 1995, pp 131–171Google Scholar
2. United States Department of Health, Education and Welfare: Surgeon General’s Report on Smoking and Health. Washington, DC, US Public Health Service, 1964Google Scholar
3. World Health Organization: Smoking and Its Effects on Health: Technical Report Series Number 568. Geneva, WHO, 1975Google Scholar
4. Escobedo LG, Anda RF, Smith PF, Remington PL, Mast EE: Sociodemographic characteristics of cigarette smoking initiation in the United States: implications for smoking prevention policy. JAMA 1990; 264:1550–1555Crossref, Medline, Google Scholar
5. Ferrence RG: Sex differences in cigarette smoking in Canada, 1900–1978: a reconstructed cohort study. Can J Public Health 1988;79:160–165Google Scholar
6. Hughes JR, Hatsukami DK, Mitchell JE, Dahlgren LA: Prevalence of smoking among psychiatric outpatients. Am J Psychiatry 1986; 143:993–997Link, Google Scholar
7. Frerichs RR, Aneshensel CS, Clark VA, Yokopenic P: Smoking and depression: a community survey. Am J Public Health 1981; 71:637–640Crossref, Medline, Google Scholar
8. Anda RF, Williamson DF, Escobedo L, Mast EE, Giovino GA, Remington PL: Depression and the dynamics of smoking: a national perspective. JAMA 1990; 264:1541–1545Crossref, Medline, Google Scholar
9. Breslau N, Peterson EL, Schultz LR, Chilcoat HD, Andreski P: Major depression and stages of smoking: a longitudinal investigation. Arch Gen Psychiatry 1998; 55:161–166Crossref, Medline, Google Scholar
10. Patten CA, Gillin C, Golshan S, Wolter TD, Rapaport M, Kelsoe J: Relationship of mood disturbance to cigarette smoking status among 252 patients with a current mood disorder. J Clin Psychiatry 2001; 62:319–324Crossref, Medline, Google Scholar
11. Glassman AH, Helzer JE, Covey LS, Cottler LB, Stetner F, Tipp JE, Johnson J: Smoking, smoking cessation, and major depression. JAMA 1990; 264:1546–1549Crossref, Medline, Google Scholar
12. Khantzian EJ: The self-medication hypothesis of substance use disorders: a reconsideration and recent applications. Harv Rev Psychiatry 1997; 4:231–244Crossref, Medline, Google Scholar
13. Kendler KS, Neale MC, Maclean CJ, Heath AC, Eaves LJ, Kessler RC: Smoking and major depression: a causal analysis. Arch Gen Psychiatry 1993; 50:36–43Crossref, Medline, Google Scholar
14. Dierker LC, Avenevoli S, Stolar M, Merikangas KR: Smoking and depression: an examination of mechanisms of comorbidity. Am J Psychiatry 2002; 159:947–953Link, Google Scholar
15. Hanna EZ, Yi HY, Dufour MC, Whitmore CC: The relationship of early-onset regular smoking to alcohol use, depression, illicit drug use, and other risky behaviors during early adolescence: results from the Youth Supplement to the Third National Health and Nutrition Examination Survey. J Subst Abuse 2001; 13:265–282Crossref, Medline, Google Scholar
16. Allgower AN, Wardle J, Steptoe A: Depressive symptoms, social support, and personal health behaviors in young men and women. Health Psychol 2001; 20:223–227Crossref, Medline, Google Scholar
17. Breslau N, Johnson EO, Hiripi E, Kessler R: Nicotine dependence in the United States: prevalence, trends, and smoking persistence. Arch Gen Psychiatry 2001; 58:810–816Crossref, Medline, Google Scholar
18. Leighton AH: My Name Is Legion: The Stirling County Study of Psychiatric Disorder and Sociocultural Environment, vol 1. New York, Basic Books, 1959Google Scholar
19. Murphy JM: The Stirling County Study: then and now. Int Rev Psychiatry 1994; 6(special issue):329–348Google Scholar
20. Murphy JM, Sobol AM, Neff RK, Olivier DC, Leighton AH: Stability of prevalence: depression and anxiety disorders. Arch Gen Psychiatry 1984; 41:990–997Crossref, Medline, Google Scholar
21. Murphy JM, Monson RR, Laird NM, Sobol AM, Leighton AH: A forty-year perspective on the prevalence of depression from the Stirling County Study. Arch Gen Psychiatry 2000; 57:209–215Crossref, Medline, Google Scholar
22. Murphy JM, Olivier DC, Monson RR, Sobol AM, Federman EB, Leighton AH: Depression and anxiety in relation to social status: a prospective epidemiologic study. Arch Gen Psychiatry 1991; 48:223–229Crossref, Medline, Google Scholar
23. Robins LN, Helzer JE, Croughan J, Ratcliff KS: The National Institute of Mental Health Diagnostic Interview Schedule: its history, characteristics, and validity. Arch Gen Psychiatry 1981; 38:381–389Crossref, Medline, Google Scholar
24. Regier DA, Boyd JH, Burke JD Jr, Rae DS, Myers JK, Kramer M, Robins LN, George LK, Karno M, Locke BZ: One-month prevalence of mental disorders in the United States: based on five Epidemiologic Catchment Area sites. Arch Gen Psychiatry 1988; 45:977–986Crossref, Medline, Google Scholar
25. Weissman MM, Bruce ML, Leaf PJ, Florio LP, Holzer C: Affective disorders, in Psychiatric Disorders in America: The Epidemiologic Catchment Area Study. Edited by Robins LN, Regier DA. New York, Free Press, 1991, pp 53–80Google Scholar
26. Bland RC, Newman SC, Orn H (eds): Epidemiology of Psychiatric Disorders in Edmonton. Acta Psychiatr Scand Suppl 1988; 338Google Scholar
27. Murphy JM, Neff RK, Sobol AM, Rice JX, Olivier DC: Computer diagnosis of depression and anxiety: the Stirling County Study. Psychol Med 1985; 15:99–112Crossref, Medline, Google Scholar
28. Murphy JM, Monson RR, Laird NM, Sobol AM, Leighton AH: Identifying depression and anxiety in a forty-year epidemiologic investigation: the Stirling County Study. Int J Methods Psychiatr Res 1998; 7:89–109Crossref, Google Scholar
29. Murphy JM, Laird NM, Monson RR, Sobol AM, Leighton AH: Incidence of depression in the Stirling County Study: historical and comparative perspectives. Psychol Med 2000; 30:505–514Crossref, Medline, Google Scholar
30. Hosmer DW, Lemeshow S: Applied Logistic Regression, 2nd ed. New York, John Wiley & Sons, 2000Google Scholar
31. Anderson A, Auguier A, Hauck WW, Oakes D, Vandaele W, Weisberg HI: Statistical Methods for Comparative Studies. New York, John Wiley & Sons, 1980Google Scholar
32. Laird NM, Olivier DC: Covariance analysis of censored survival data using log linear analysis techniques. J Am Stat Assoc 1981; 76:231–240Crossref, Google Scholar
33. Robins LN: Detecting individual factors in substance abuse problems, in The Nature of Alcohol and Drug Related Problems. Edited by Lader M, Edwards G, Drummond DC. New York, Oxford University Press, 1992, pp 133–150Google Scholar
34. Weiss RD, Mirin SM, Griffin ML, Michael JL: Psychopathology in cocaine abusers: changing trends. J Nerv Ment Dis 1988; 176:719–725Crossref, Medline, Google Scholar
35. Robins LN: The natural history of substance use as a guide to setting drug policy (editorial). Am J Public Health 1995; 85:12–13Crossref, Medline, Google Scholar
36. Klerman GL, Weissman MM: Increasing rates of depression. JAMA 1989; 261:2229–2235Crossref, Medline, Google Scholar
37. Kessler RC, McGonagle KA, Nelson CB, Hughes M, Swartz M, Blazer DG: Sex and depression in the National Comorbidity Survey II: cohort effects. J Affect Disord 1994; 30:15–26Crossref, Medline, Google Scholar
38. Murphy JM, Olivier DC, Sobol AM, Monson RR, Leighton AH: Diagnosis and outcome: depression and anxiety in a general population. Psychol Med 1986; 16:117–126Crossref, Medline, Google Scholar
39. Murphy JM, Monson RR, Olivier DC, Sobol AM, Leighton AH: Affective disorders and mortality: a general population study. Arch Gen Psychiatry 1987; 44:473–480Crossref, Medline, Google Scholar
40. Chen K, Kandel DB: The natural history of drug use from adolescence to the mid-thirties in a general population sample. Am J Public Health 1995; 85:41–47Crossref, Medline, Google Scholar



